Last Aid Course. An Education For All Citizens and an Ingredient of Compassionate Communities
Abstract
1. Introduction
2. Materials and Methods
3. Findings
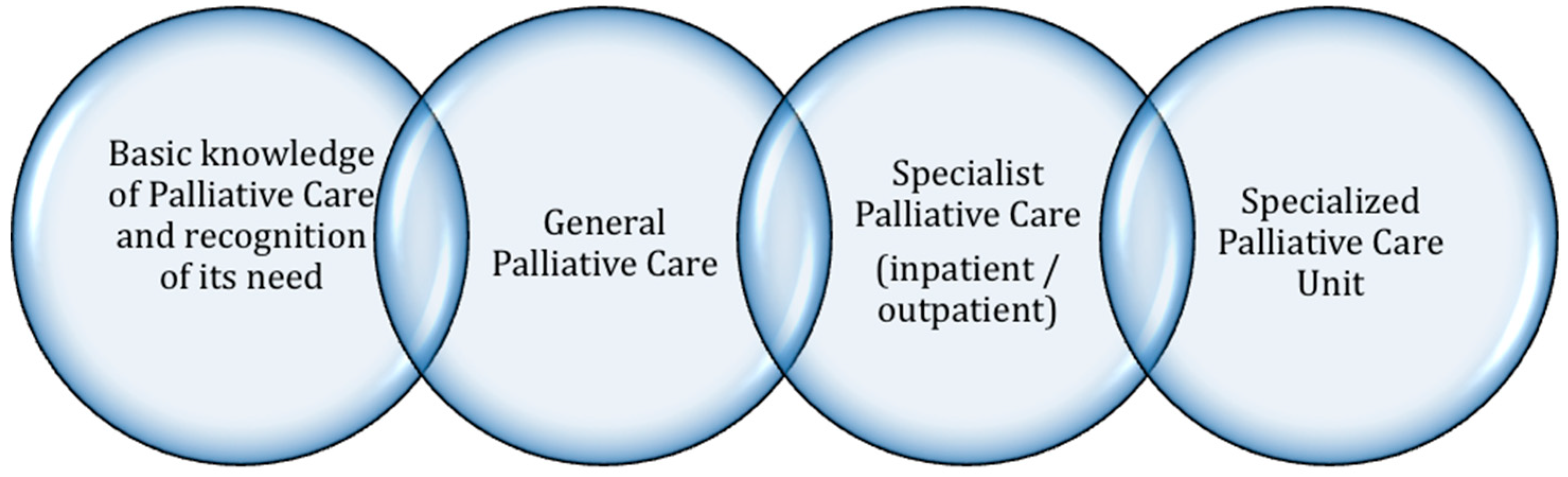
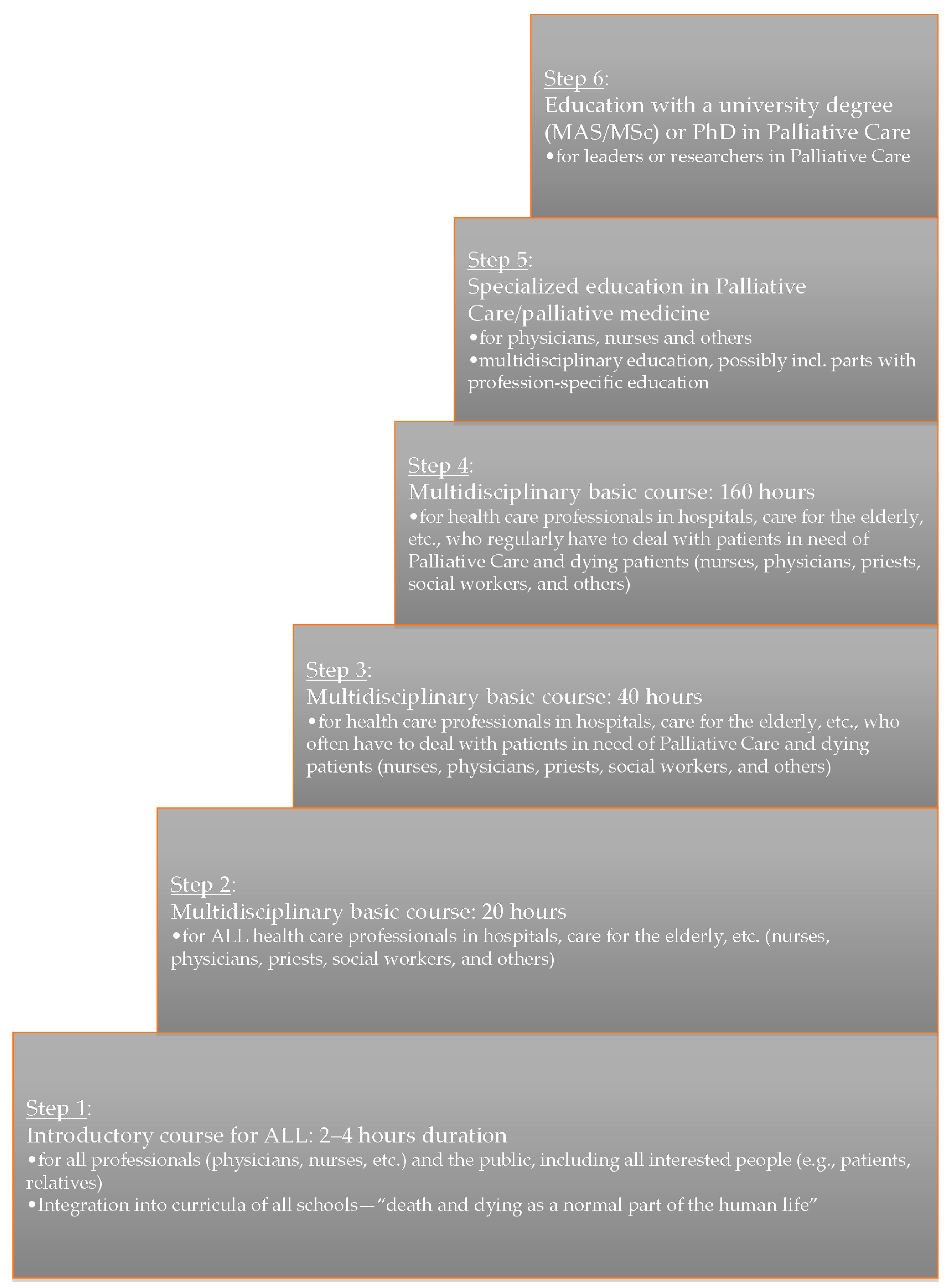
3.1. Palliative Care Education for the Public
3.2. Compassionate Communities
- Attitudes toward death, dying, loss and care;
- Social, cultural, and historical influences on death and dying;
- Mortality and society;
- Death and dying in healthcare;
- End-of-life issues and decisions;
- Facing death—living with life-threatening illness;
- Last rites: funerals and body disposition;
- Death in the lives of children and adolescents;
- Death in the lives of adults;
- Beyond death/after life;
- The path ahead: personal and social choices.
3.3. Development and Implementation of Last Aid Courses
- Germany;
- Denmark;
- Austria;
- Switzerland;
- Lithuania;
- Slovenia;
- Scotland;
- Estonia;
- Latvia.
- If I only had known that before it would have helped me when my aunt died.
- I appreciate the natural way to deal with the topics death and dying.
- Lively and easy although the topic is complicated.
- I have no suggestion that could improve the course.
- Clear and structured.
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
| Module nr. | Topic | Course Content |
|---|---|---|
| Module 1 | Dying as a normal part of life |
|
| Module 2 | Planning ahead |
|
| Module 3 | Relieving suffering |
|
| Module 4 | Final goodbyes |
|
References
- Ferri, C.P.; Prince, M.; Brayne, C.; Brodaty, H.; Fratiglioni, L.; Ganguli, M.; Hall, K.; Hasegawa, K.; Hendrie, H.; Huang, Y.; et al. Alzheimer’s Disease International. Global prevalence of dementia: A Delphi consensus study. Lancet 2005, 366, 2112–2117. [Google Scholar] [CrossRef]
- Clegg, A.; Young, J.; Iliffe, S.; Rikkert, M.O.; Rockwood, K. Frailty in elderly people. Lancet 2013, 381, 752–762. [Google Scholar] [CrossRef]
- Chrismon Spezial, Das Evangelische Magazin zum Reformationstag 2014, im Auftrag der Evangelischen Kirche in Deutschlang (EKD), Was wir Glauben. Religion ist Privatsache? Prominente Protestanten Sprechen über Gott. Available online: http://static.evangelisch.de/get/?daid=jwhRNMB8FaGErjJle8tHi0fL00081222&dfid=download (accessed on 5 November 2018).
- Gomes, B.; Higginson, I.J.; Calanzani, N.; Cohen, J.; Deliens, L.; Daveson, B.A.; Bechinger-English, D.; Bausewein, C.; Ferreira, P.L.; Toscani, F.; et al. Preferences for place of death if faced with advanced cancer: A population survey in England, Flanders, Germany, Italy, The Netherlands, Portugal and Spain. Ann. Oncol. 2012, 23, 2006–2015. [Google Scholar] [CrossRef] [PubMed]
- Gágyor, I.; Himmel, W.; Pierau, A.; Chenot, J.F. Dying at home or in the hospital? An observational study in German general practice. Eur. J. Gen. Pract. 2016, 22, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Kozlov, E.; McDarby, M.; Reid, M.C.; Carpenter, B.D. Knowledge of Palliative Care Among Community-Dwelling Adults. Am. J. Hosp. Palliat. Care 2018, 35, 647–651. [Google Scholar] [CrossRef]
- Partridge, A.H.; Seah, D.S.; King, T.; Leighl, N.B.; Hauke, R.; Wollins, D.S.; Von Roenn, J.H. Developing a service model that integrates palliative care throughout cancer care: The time is now. J. Clin. Oncol. 2014, 32, 3330–3336. [Google Scholar] [CrossRef]
- Bollig, G. Palliative Care für alte und Demente Menschen Lernen und Lehren; LIT-Verlag: Berlin, Germany, 2010; Available online: http://www.lit-verlag.de/isbn/3-643-90058-6 (accessed on 5 November 2018).
- Singer, P.A.; Wolfson, M. The best places to die. Br. Med. J. 2003, 327, 173–174. [Google Scholar] [CrossRef]
- Edwards, S.B.; Olson, K.; Koop, P.M.; Northcott, H.C. Patient and family caregiver decision making in the context of advanced cancer. Cancer Nurs. 2012, 35, 178–186. [Google Scholar] [CrossRef]
- Dellon, E.P.; Helms, S.W.; Hailey, C.E.; Shay, R.; Carney, S.D.; Schmidt, H.J.; Brown, D.E.; Prieur, M.G. Exploring knowledge and perceptions of palliative care to inform integration of palliative care education into cystic fibrosis care. Pediatr. Pulmonol. 2018, 53, 1218–1224. [Google Scholar] [CrossRef]
- Boucher, N.A.; Bull, J.H.; Cross, S.H.; Kirby, C.; Davis, J.K.; Taylor, D.H., Jr. Patient, Caregiver and Taxpayer Knowledge of Palliative Care and Views on a Model of Community-Based Palliative Care. J. Pain Symptom Manag. 2018, 56, 951–956. [Google Scholar] [CrossRef]
- McIlfatrick, S.; Noble, H.; McCorry, N.K.; Roulston, A.; Hasson, F.; McLaughlin, D.; Johnston, G.; Rutherford, L.; Payne, C.; Kernohan, G.; et al. Exploring public awareness and perceptions of palliative care: A qualitative study. Palliat. Med. 2014, 28, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Shalev, A.; Phongtankuel, V.; Reid, M.C.; Czaja, S.J.; Dignam, R.; Baughn, R.; Newmark, M.; Prigerson, H.G.; Teresi, J.; Adelman, R.D. Home Hospice Caregivers’ Perceived Information Needs. Am. J. Hosp. Palliat. Care 2018. [Google Scholar] [CrossRef] [PubMed]
- Prabhu, A.V.; Crihalmeanu, T.; Hansberry, D.R.; Agarwal, N.; Glaser, C.; Clump, D.A.; Heron, D.E.; Beriwal, S. Online palliative care and oncology patient education resources through Google: Do they meet national health literacy recommendations? Pract. Radiat. Oncol. 2017, 7, 306–310. [Google Scholar] [CrossRef] [PubMed]
- Hudson, P.; Quinn, K.; Kristjanson, L.; Thomas, T.; Braithwaite, M.; Fisher, J.; Cockayne, M. Evaluation of a psycho-educational group programme for family caregivers in home-based palliative care. Palliat. Med. 2008, 22, 270–280. [Google Scholar] [CrossRef] [PubMed]
- Hudson, P.; Thomas, T.; Quinn, K.; Cockayne, M.; Braithwaite, M. Teaching family carers about home-based palliative care: final results from a group education program. J. Pain Symptom Manag. 2009, 38, 299–308. [Google Scholar] [CrossRef] [PubMed]
- Death Cafe. Available online: http://deathcafe.com (accessed on 5 November 2018).
- Death Chat—Talking about Death and Dying Remains One of the Biggest Taboos within Most Communities. Available online: http://www.stchristophers.org.uk/social-programme/death-chat (accessed on 5 November 2018).
- Noonan, K. Death Literacy—Developing a Tool to Measure the Social Impact of Public Health Initiatives. Ann. Palliat. Med. 2018, 7 (Suppl. 1), AB007. [Google Scholar] [CrossRef] [PubMed]
- Kellehear, A. Compassionate communities: End-of-life care as everyone’s responsibility. Q. J. Med. 2013, 106, 1071–1075. [Google Scholar] [CrossRef]
- Kellehear, A. Compassionate Cities: Public Health and End-of-Life Care; Routledge: Oxfordshire, UK, 2005. [Google Scholar]
- Librada Flores, S.; Herrera Molina, E.; Boceta Osuna, J.; Mota Vargas, R.; Nabal Vicuña, M. All with You: A new method for developing compassionate communities—Experiences in Spain and Latin-America. Ann. Palliat. Med. 2018, 7 (Suppl. 2), S15–S31. [Google Scholar] [CrossRef]
- Gómez-Batiste, X.; Mateu, S.; Serra-Jofre, S.; Molas, M.; Mir-Roca, S.; Amblàs, J.; Costa, X.; Lasmarías, C.; Serrarols, M.; Solà-Serrabou, A.; et al. Compassionate communities: design and preliminary results of the experience of Vic (Barcelona, Spain) caring city. Ann. Palliat. Med. 2018, 7 (Suppl. 2), S32–S41. [Google Scholar] [CrossRef]
- Grindrod, A.; Rumbold, B. Healthy End of Life Project (HELP): A progress report on implementing community guidance on public health palliative care initiatives in Australia. Ann. Palliat. Med. 2018, 7 (Suppl. 2), S73–S83. [Google Scholar] [CrossRef]
- Krakowiak, P.; Deka, R.; Janowicz, A. Solidarity and compassion—Prisoners as hospice volunteers in Poland. Ann. Palliat. Med. 2018, 7 (Suppl. 2), S109–S117. [Google Scholar] [CrossRef] [PubMed]
- Tompkins, B. Compassionate Communities in Canada: It is everyoner´s responsibility. Ann. Palliat. Med. 2018, 7 (Suppl. 2), S118–S129. [Google Scholar] [CrossRef]
- Hospiz Macht Schule. Available online: https://www.hospizmachtschule.de (accessed on 5 November 2018).
- McLoughlin, K. Compassionate Communities Project Evaluation Report. Report 2013. Available online: https://www.researchgate.net/publication/281465213_Compassionate_Communities_Project_Evaluation_Report (accessed on 5 November 2018).
- Bollig, G. The “Chain of Palliative care“ and the “public knowledge approach“—New concepts for introduction of Palliative Care to the public. In Proceedings of the Posterpresentation 11th Congress of the European Association for Palliative Care, Vienna, Austria, 7–10 May 2009. [Google Scholar]
- Wegleitner, K.; Heller, A.; Bollig, G.; Völkel, M.; Gröschel, C.; Wild, M.; Appel, E.; Gruber, W. “Leben und Helfen bis zuletzt“—Übers Sterben reden—ein Curriculum, um mit BürgerInnen vorsorgend über das Leben und Sterben ins Gespräch zu kommen. In Zu Hause sterben—der Tod hält sich nicht an Dienstpläne; Klaus, W., Katharina, H., Andreas, H., Eds.; Hospizverlag: Ludwigsburg, Germany, 2012. [Google Scholar]
- Last Aid International. Available online: www.lastaid.info (accessed on 5 November 2018).
- Bollig, G.; Kuklau, N. Sistehjelpskurset! Et kurs for folk flest om død og omsorg ved livets slutt, palliasjon. Omsorg 2015, 2, 66–71. [Google Scholar]
- Bollig, G.; Kuklau, N. Der Letzte Hilfe Kurs—ein Angebot zur Verbesserung der allgemeinen ambulanten Palliativversorgung durch Information und Befähigung von Bürgerinnen und Bürgern. Zeitschrift für Palliativmedizin 2015, 16, 210–216. [Google Scholar] [CrossRef]
- Bollig, G.; Heller, A. The last aid course—A simple and effective concept to teach the public about palliative care and to enhance the public discussion about death and dying. Austin Palliat Care 2016, 1, 1010. [Google Scholar]
- Bollig, G. The Public Knowledge Approach as educational concept for bringing Palliative Care to the public. In Proceedings of the International Palliative Care Network Conference 2012; online conference. Available online: https://palliativecarenetwork.com/ (accessed on 20 January 2018).
- Bollig, G. Der Letzte Hilfe Kurs—Eine sorgende Gemeinschaft braucht Allgemeinwissen über Palliativversorgung und Palliative Care. Praxis Palliative Care 2015, 26, 36–39. [Google Scholar]
- Startsocial. Available online: https://startsocial.de (accessed on 5 November 2018).
- Bollig, G. Sistehjelpskurs. Liv til dagene. Lecture Norsk landskonferanse i Stavanger. Sep. 2016. (In Norwegian)
- Bollig, G. Letzte Hilfe. In Palliative Care für alte und Demente Menschen Lernen und Lehren; Lecture 11; Fachtagung Palliative Geriatrie Berlin Sep.: Berlin, Germany, 2016. [Google Scholar]
- Bollig, G. The Last Aid Course—Teaching the Public About Palliative Care. In Proceedings of the Lecture 21st International Congress on Palliative Care, Montréal, QC, Canada, 18–21 October 2016. [Google Scholar]
- Bollig, G. Was alle Menschen über Palliative Care Wissen Sollten; Lecture 10; Bremer Kongress für Palliativmedizin: Bremen, Germany, March 2017. [Google Scholar]
- Bollig, G. The “Last Aid” Course—An Approach to Promoting Public Discussion, Awareness and Education. Lecture SPPC Annual Conference 2017: Making the Best of Hard Times. Sep 2017 Edinburgh. Available online: https://www.youtube.com/watch?v=0mAAIXH2xPY (accessed on 5 November 2018).
- Bollig, G.; Heller, A.; Völkel, M. Letzte Hilfe—Umsorgen von Schwer Erkrankten und Sterbenden Menschen am Lebensende. Hospizverlag Ludwigsburg: Germany, 2016. Available online: http://www.hospiz-verlag.de/produkt/letzte-hilfe/ (accessed on 5 November 2018).
- Bollig, G.; Frank, S.; Kastberg, I.; Bachmann, K.H. Sidstehjælp. Munksgaard, Copenhagen 2018. Available online: http://munksgaard.dk/Sygepleje/Sidstehjælp/9788762818064 (accessed on 5 November 2018).
- Martins Pereira, S.; Araújo, J.; Hernández-Marrero, P. Towards a public health approach for palliative care: An action-research study focused on engaging a local community and educating teenagers. BMC Palliat. Care 2018, 17, 89. [Google Scholar] [CrossRef] [PubMed]
- Ferris, F.D.; von Gunten, C.F.; Emanuel, L.L. Knowledge: Insufficient for Change. J. Palliat. Med. 2001, 4, 145–147. [Google Scholar] [CrossRef]
- Faber, H. Sidstehjælp i et samfundspsykologisk perspektiv. Specialist opgave i klinisk samfundspsykolog. Unpublished work. 2017. [Google Scholar]
- EAPC White Paper on Palliative Care Education. Available online: https://www.eapcnet.eu/publications/Education/EAPCWhitepaperoneducation (accessed on 5 November 2018).
- Bollig, G. A six-step approach to education in Palliative Care for ALL. In Proceedings of the Posterpresentation Congress of the European Association for Palliative Care, Vienna, Austria, 7–10 May 2009. [Google Scholar]
- O’Connor, M.; Abbott, J.A.; Recoche, K. Getting the message across: Does the use of drama aid education in palliative care? Adv. Health Sci. Educ. Theory Pract. 2012, 17, 195–201. [Google Scholar]
- EUPCA Participants 2017–2019. Georg Bollig. Available online: https://www.eupca.eu/participants-2017-2019/ (accessed on 5 November 2018).
- Mueller, E.; Bollig, G.; Becker, G.; Boehlke, C. Lessons learned from introducing “Last-Aid” courses at a university hospital in Germany. In Proceedings of the 16th World Congress of the European Association for Palliative Care, Berlin, Germany, 23–25 May 2019. [Google Scholar]
- Bollig, G.; Mainzer, K.; Fiedler, H.; Barra, F.; Pothmann, R. A New Last Aid Course for Kids from 8–14 Years—A Pilot-test. In Proceedings of the 16th World Congress of the European Association for Palliative Care, Berlin, Germany, 23–25 May 2019. [Google Scholar]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bollig, G.; Brandt, F.; Ciurlionis, M.; Knopf, B. Last Aid Course. An Education For All Citizens and an Ingredient of Compassionate Communities. Healthcare 2019, 7, 19. https://doi.org/10.3390/healthcare7010019
Bollig G, Brandt F, Ciurlionis M, Knopf B. Last Aid Course. An Education For All Citizens and an Ingredient of Compassionate Communities. Healthcare. 2019; 7(1):19. https://doi.org/10.3390/healthcare7010019
Chicago/Turabian StyleBollig, Georg, Frans Brandt, Marius Ciurlionis, and Boris Knopf. 2019. "Last Aid Course. An Education For All Citizens and an Ingredient of Compassionate Communities" Healthcare 7, no. 1: 19. https://doi.org/10.3390/healthcare7010019
APA StyleBollig, G., Brandt, F., Ciurlionis, M., & Knopf, B. (2019). Last Aid Course. An Education For All Citizens and an Ingredient of Compassionate Communities. Healthcare, 7(1), 19. https://doi.org/10.3390/healthcare7010019




