Impact of Time-Varying Treatment Exposures on the Risk of Venous Thromboembolism in Multiple Myeloma
Abstract
:1. Introduction
2. Methods
2.1. Data Source and Study Sample
2.2. Subject Characteristics
2.3. Outcome Events
2.4. Statistical Analysis
2.4.1. Model #1—Competing Risks Survival Analysis
2.4.2. Model #2—Case-Time-Control Analysis
2.4.3. Model #3—Time-Varying Cox Proportional Hazard Models
3. Results
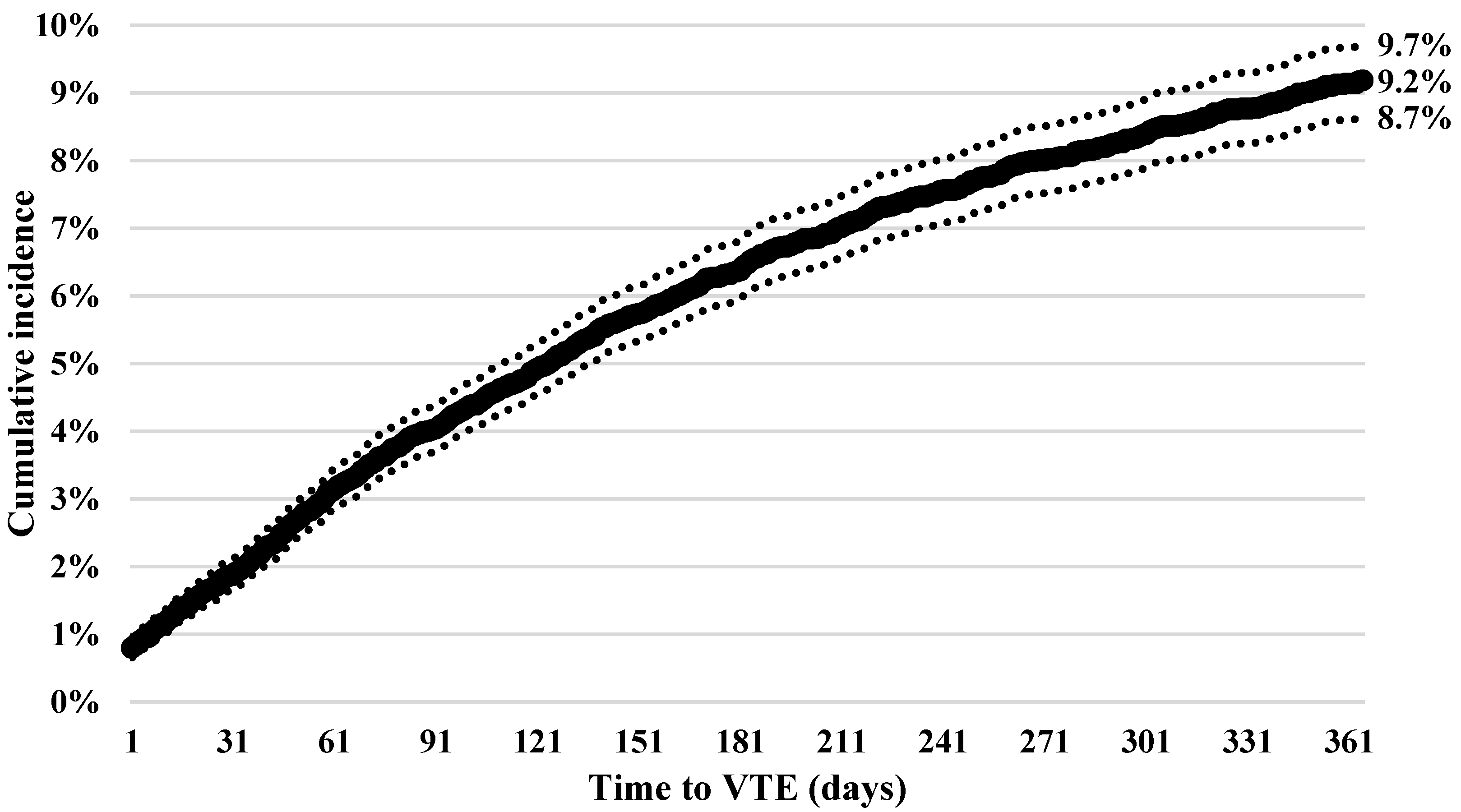
3.1. Incidence of Thrombosis
3.2. Competing Risk Model Results
3.3. Case-Time-Control Model
3.4. 90-Day Time-Varying Exposure Model
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Cronin-Fenton, D.P.; Sondergaard, F.; Pedersen, L.A.; Fryzek, J.P.; Cetin, K.; Acquavella, J.; Baron, J.A.; Sørensen, H.T. Hospitalisation for venous thromboembolism in cancer patients and the general population: A population-based cohort study in Denmark, 1997–2006. Br. J. Cancer 2010, 103, 947–953. [Google Scholar] [CrossRef] [PubMed]
- Srkalovic, G.; Cameron, M.G.; Rybicki, L.; Deitcher, S.R.; Kattke-Marchant, K.; Hussein, M.A. Monoclonal gammopathy of undetermined significance and multiple myeloma are associated with an increased incidence of venothromboembolic disease. Cancer 2004, 101, 558–566. [Google Scholar] [CrossRef] [PubMed]
- Zamagni, E.; Brioli, A.; Tacchetti, P.; Zannetti, B.; Pantani, L.; Cavo, M. Multiple myeloma, venous thromboembolism, and treatment-related risk of thrombosis. Semin. Thromb. Hemost. 2011, 37, 209–219. [Google Scholar] [CrossRef] [PubMed]
- Lip, G.Y.; Chin, B.S.; Blann, A.D. Cancer and the prothrombotic state. Lancet. Oncol. 2002, 3, 27–34. [Google Scholar] [CrossRef]
- Khorana, A.A.; Dalal, M.; Lin, J.; Connolly, G.C. Incidence and predictors of venous thromboembolism (VTE) among ambulatory high-risk cancer patients undergoing chemotherapy in the United States. Cancer 2013, 119, 648–655. [Google Scholar] [CrossRef] [PubMed]
- Zangari, M.; Anaissie, E.; Barlogie, B.; Badros, A.; Desikan, R.; Gopal, A.V.; Morris, C.; Toor, A.; Siegel, E.; Fink, L.; et al. Increased risk of deep-vein thrombosis in patients with multiple myeloma receiving thalidomide and chemotherapy. Blood 2001, 98, 1614–1615. [Google Scholar] [CrossRef] [PubMed]
- Zangari, M.; Siegel, E.; Barlogie, B.; Anaissie, E.; Saghafifar, F.; Fassas, A.; Morris, C.; Fink, L.; Tricot, G. Thrombogenic activity of doxorubicin in myeloma patients receiving thalidomide: Implications for therapy. Blood 2002, 100, 1168–1171. [Google Scholar] [CrossRef] [PubMed]
- Bennett, C.L.; Angelotta, C.; Yarnold, P.R.; Evens, A.M.; Zonder, J.A.; Raisch, D.W.; Richardson, P. Thalidomide- and lenalidomide-associated thromboembolism among patients with cancer. JAMA 2006, 296, 2558–2560. [Google Scholar] [CrossRef] [PubMed]
- Leleu, X.; Rodon, P.; Hulin, C.; Daley, L.; Dauriac, C.; Hacini, M.; Decaux, O.; Eisemann, J.C.; Fitoussi, O.; Lioure, B.; et al. MELISSE, a large multicentric observational study to determine risk factors of venous thromboembolism in patients with multiple myeloma treated with immunomodulatory drugs. Thromb. Haemost. 2013, 110, 844–851. [Google Scholar] [CrossRef] [PubMed]
- Carrier, M.; Le Gal, G.; Tay, J.; Wu, C.; Lee, A.Y. Rates of venous thromboembolism in multiple myeloma patients undergoing immunomodulatory therapy with thalidomide or lenalidomide: A systematic review and meta-analysis. J. Thromb. Haemost. 2011, 9, 653–663. [Google Scholar] [CrossRef] [PubMed]
- Zangari, M.; Fink, L.; Zhan, F.; Tricot, G. Low venous thromboembolic risk with bortezomib in multiple myeloma and potential protective effect with thalidomide/lenalidomide-based therapy: Review of data from phase 3 trials and studies of novel combination regimens. Clin. Lymphoma Myeloma Leuk. 2011, 11, 228–236. [Google Scholar] [CrossRef] [PubMed]
- Bennett, C.L.; Silver, S.M.; Djulbegovic, B.; Samaras, A.T.; Blau, C.A.; Gleason, K.J.; Barnato, S.E.; Elverman, K.M.; Courtney, D.M.; McKoy, J.M.; et al. Venous thromboembolism and mortality associated with recombinant erythropoietin and darbepoetin administration for the treatment of cancer-associated anemia. JAMA 2008, 299, 914–924. [Google Scholar] [CrossRef] [PubMed]
- Khorana, A.A.; Francis, C.W.; Culakova, E.; Lyman, G.H. Risk factors for chemotherapy-associated venous thromboembolism in a prospective observational study. Cancer 2005, 104, 2822–2829. [Google Scholar] [CrossRef] [PubMed]
- Lippi, G.; Franchini, M.; Favaloro, E.J. Thrombotic complications of erythropoiesis-stimulating agents. Semin. Thromb. Hemost. 2010, 36, 537–549. [Google Scholar] [CrossRef] [PubMed]
- Wun, T.; White, R.H. Venous thromboembolism (VTE) in patients with cancer: Epidemiology and risk factors. Cancer Investig. 2009, 27 (Suppl. 1), 63–74. [Google Scholar] [CrossRef] [PubMed]
- Beckers, M.M.; Ruven, H.J.; Seldenrijk, C.A.; Prins, M.H.; Biesma, D.H. Risk of thrombosis and infections of central venous catheters and totally implanted access ports in patients treated for cancer. Thromb. Res. 2010, 125, 318–321. [Google Scholar] [CrossRef] [PubMed]
- Shivakumar, S.P.; Anderson, D.R.; Couban, S. Catheter-associated thrombosis in patients with malignancy. J. Clin. Oncol. 2009, 27, 4858–4864. [Google Scholar] [CrossRef] [PubMed]
- Esmon, C.T. Does inflammation contribute to thrombotic events? Haemostasis 2000, 30 (Suppl. 2), 34–40. [Google Scholar] [CrossRef] [PubMed]
- Lyman, G.H.; Khorana, A.A.; Kuderer, N.M.; Lee, A.Y.; Arcelus, J.I.; Balaban, E.P.; Clarke, J.M.; Flowers, C.R.; Francis, C.W.; Gates, L.E.; et al. Venous thromboembolism prophylaxis and treatment in patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J. Clin. Oncol. 2013, 31, 2189–2204. [Google Scholar] [CrossRef] [PubMed]
- Anderson, K.C.; Alsina, M.; Atanackovic, D.; Biermann, J.S.; Chandler, J.C.; Costello, C.; Djulbegovic, B.; Fung, H.C.; Gasparetto, C.; Godby, K.; et al. Multiple Myeloma, Version 2.2016. J. Natl. Compr. Cancer Netw. 2015, 13, 1398–1435. [Google Scholar]
- Kristinsson, S.Y.; Fears, T.R.; Gridley, G.; Turesson, I.; Mellqvist, U.H.; Bjorkholm, M.; Landgren, O. Deep vein thrombosis after monoclonal gammopathy of undetermined significance and multiple myeloma. Blood 2008, 112, 3582–3586. [Google Scholar] [CrossRef] [PubMed]
- Quan, H.; Sundararajan, V.; Halfon, P.; Fong, A.; Burnand, B.; Luthi, J.C.; Saunders, L.D.; Beck, C.A.; Feasby, T.E.; Ghali, W.A. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med. Care 2005, 43, 1130–1139. [Google Scholar] [CrossRef] [PubMed]
- Sanfilippo, K.M.; Wang, T.; Gage, B.F.; Liu, W.; Carson, K.R. Improving accuracy of International Classification of Diseases codes for venous thromboembolism in administrative data. Thromb. Res. 2015, 135, 616–620. [Google Scholar] [CrossRef] [PubMed]
- White, R.H.; Garcia, M.; Sadeghi, B.; Tancredi, D.J.; Zrelak, P.; Cuny, J.; Sama, P.; Gammon, H.; Schmaltz, S.; Romano, P.S. Evaluation of the predictive value of ICD-9-CM coded administrative data for venous thromboembolism in the United States. Thromb. Res. 2010, 126, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Zhan, C.; Battles, J.; Chiang, Y.P.; Hunt, D. The validity of ICD-9-CM codes in identifying postoperative deep vein thrombosis and pulmonary embolism. Jt. Comm. J. Qual. Patient Saf. 2007, 33, 326–331. [Google Scholar] [CrossRef]
- Brown, J.D.; Adams, V.R. Incidence and Risk Factors of Thromboembolism with Multiple Myeloma in the Presence of Death as a Competing Risk: An Empirical Comparison of Statistical Methodologies. Healthcare 2016, 4. [Google Scholar] [CrossRef] [PubMed]
- Ay, C.; Posch, F.; Kaider, A.; Zielinski, C.; Pabinger, I. Estimating risk of venous thromboembolism in patients with cancer in the presence of competing mortality. J. Thromb. Haemost. 2014, 13, 390–397. [Google Scholar] [CrossRef] [PubMed]
- Lund, J.L.; Ostgard, L.S.; Prandoni, P.; Sorensen, H.T.; de Nully Brown, P. Incidence, determinants and the transient impact of cancer treatments on venous thromboembolism risk among lymphoma patients in Denmark. Thromb. Res. 2015, 136, 917–923. [Google Scholar] [CrossRef] [PubMed]
- Suissa, S. The case-time-control design: Further assumptions and conditions. Epidemiology 1998, 9, 441–445. [Google Scholar] [CrossRef] [PubMed]
- Blom, J.W.; Vanderschoot, J.P.; Oostindier, M.J.; Osanto, S.; van der Meer, F.J.; Rosendaal, F.R. Incidence of venous thrombosis in a large cohort of 66,329 cancer patients: Results of a record linkage study. J. Thromb. Haemost. 2006, 4, 529–535. [Google Scholar] [CrossRef] [PubMed]
- Menon, S.P.; Rajkumar, S.V.; Lacy, M.; Falco, P.; Palumbo, A. Thromboembolic events with lenalidomide-based therapy for multiple myeloma. Cancer 2008, 112, 1522–1528. [Google Scholar] [CrossRef] [PubMed]
- Mahindra, A.; Laubach, J.; Raje, N.; Munshi, N.; Richardson, P.G.; Anderson, K. Latest advances and current challenges in the treatment of multiple myeloma. Nat. Rev. Clin. Oncol. 2012, 9, 135–143. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.K.; Rajkumar, S.V.; Dispenzieri, A.; Lacy, M.Q.; Hayman, S.R.; Buadi, F.K.; Zeldenrust, S.R.; Dingli, D.; Russell, S.J.; Lust, J.A.; et al. Improved survival in multiple myeloma and the impact of novel therapies. Blood 2008, 111, 2516–2520. [Google Scholar] [CrossRef] [PubMed]
- Palumbo, A.; Cavo, M.; Bringhen, S.; Zamagni, E.; Romano, A.; Patriarca, F.; Rossi, D.; Gentilini, F.; Crippa, C.; Galli, M.; et al. Aspirin, warfarin, or enoxaparin thromboprophylaxis in patients with multiple myeloma treated with thalidomide: A phase III, open-label, randomized trial. J. Clin. Oncol. 2011, 29, 986–993. [Google Scholar] [CrossRef] [PubMed]
- Larocca, A.; Cavallo, F.; Bringhen, S.; Di Raimondo, F.; Falanga, A.; Evangelista, A.; Cavalli, M.; Stanevsky, A.; Corradini, P.; Pezzatti, S.; et al. Aspirin or enoxaparin thromboprophylaxis for patients with newly diagnosed multiple myeloma treated with lenalidomide. Blood 2012, 119, 933–939. [Google Scholar] [CrossRef] [PubMed]
- Khorana, A.A.; Dalal, M.R.; Lin, J.; Connolly, G.C. Health care costs associated with venous thromboembolism in selected high-risk ambulatory patients with solid tumors undergoing chemotherapy in the United States. Clin. Outcomes Res. 2013, 5, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.Y. Anticoagulation in the treatment of established venous thromboembolism in patients with cancer. J. Clin. Oncol. 2009, 27, 4895–4901. [Google Scholar] [CrossRef] [PubMed]
- Lyman, G.H.; Bohlke, K.; Khorana, A.A.; Kuderer, N.M.; Lee, A.Y.; Arcelus, J.I.; Balaban, E.P.; Clarke, J.M.; Flowers, C.R.; Francis, C.W.; et al. Venous Thromboembolism Prophylaxis and Treatment in Patients with Cancer: American Society of Clinical Oncology Clinical Practice Guideline Update 2014. J. Clin. Oncol. 2015, 33, 2189–2204. [Google Scholar]
- Schneeweiss, S.; Avorn, J. A review of uses of health care utilization databases for epidemiologic research on therapeutics. J. Clin. Epidemiol. 2005, 58, 323–337. [Google Scholar] [CrossRef] [PubMed]
- Zhan, C.; Miller, M.R. Administrative data based patient safety research: A critical review. Qual. Saf. Health Care 2003, 12 (Suppl. 2), ii58–ii63. [Google Scholar] [CrossRef] [PubMed]
- Tamariz, L.; Harkins, T.; Nair, V. A systematic review of validated methods for identifying venous thromboembolism using administrative and claims data. Pharmacoepidemiol. Drug Saf. 2012, 21 (Suppl. 1), 154–162. [Google Scholar] [CrossRef] [PubMed]
| Overall Cohort N = 13,700 | ||
|---|---|---|
| N | % | |
| Age | Mean 63.9 | SD 13.7 |
| 18–34 | 283 | 2.1 |
| 35–64 | 7389 | 53.9 |
| 65–74 | 2648 | 19.3 |
| 75+ | 3380 | 24.7 |
| Gender | ||
| Male | 6625 | 48.4 |
| Female | 7075 | 51.6 |
| Charlson Comorbidity Index | Mean 1.1 | SD 1.5 |
| 0 | 6892 | 50.3 |
| 1–2 | 4758 | 34.7 |
| 3–4 | 1476 | 10.8 |
| 5+ | 574 | 4.2 |
| Comorbidity | ||
| MI | 251 | 1.8 |
| CHF | 933 | 6.8 |
| PVD | 841 | 6.1 |
| Dementia | 123 | 0.9 |
| COPD | 1817 | 13.3 |
| Rheumatism | 734 | 5.4 |
| PUD | 134 | 1.0 |
| Mild liver disease | 551 | 4.0 |
| Diabetes | 2814 | 20.5 |
| Diabetes w/complications | 755 | 5.5 |
| Paralysis | 68 | 0.5 |
| Renal disease | 1826 | 13.3 |
| Severe liver disease | 45 | 0.3 |
| CVD | 910 | 6.6 |
| HIV/AIDS | 30 | 0.2 |
| Hypertension | 6466 | 47.2 |
| CHD | 1725 | 12.6 |
| Lipids | 4260 | 31.1 |
| Anemia | 3727 | 27.2 |
| Covariate | sHR | 95% Confidence Interval | |
|---|---|---|---|
| Age | |||
| 18–34 | Ref. | Ref. | Ref. |
| 35–64 * | 1.7 | 1.0 | 3.0 |
| 65–74 * | 1.9 | 1.1 | 3.2 |
| 75+ | 1.6 | 0.9 | 2.7 |
| Gender | |||
| Male | Ref. | Ref. | Ref. |
| Female * | 0.7 | 0.7 | 0.8 |
| Charlson Comorbidity Index | |||
| 0 | Ref. | Ref. | Ref. |
| 1–2 | 1.0 | 0.5 | 2.1 |
| 3–4 | 0.8 | 0.5 | 1.3 |
| 5+ | 1.0 | 0.8 | 1.2 |
| Comorbidities | |||
| MI | 0.9 | 0.6 | 1.4 |
| CHF * | 1.7 | 1.4 | 2.1 |
| PVD | 1.2 | 0.9 | 1.5 |
| Dementia | 1.2 | 0.7 | 2.1 |
| COPD | 0.9 | 0.8 | 1.1 |
| Rheumatism | 0.9 | 0.6 | 1.2 |
| PUD | 0.8 | 0.5 | 1.5 |
| Mild liver disease | 0.8 | 0.5 | 1.1 |
| Diabetes | 1.0 | 0.8 | 1.2 |
| Diabetes with complications | 1.1 | 0.8 | 1.5 |
| Paralysis | 1.4 | 0.8 | 2.5 |
| Renal disease | 1.0 | 0.8 | 1.3 |
| Severe liver disease | 1.1 | 0.4 | 3.0 |
| CVD | 1.0 | 0.8 | 1.3 |
| Hypertension * | 1.2 | 1.0 | 1.3 |
| CHD | 1.0 | 0.8 | 1.1 |
| Lipids | 1.0 | 0.9 | 1.1 |
| Anemia | 0.9 | 0.8 | 1.1 |
| Treatment/Exposure | Cases Exposure | Controls Exposure | CTC Adjusted Odds Ratio | ||||
|---|---|---|---|---|---|---|---|
| Hazard N (%) | Comparison N (%) | Hazard N (%) | Comparison N (%) | Point Estimate | 95% CI | ||
| Thalidomide and derivatives | 119 (23.7) | 107 (21.3) | 147 (8.5) | 153 (8.8) | 1.61 | 1.11 | 2.33 |
| Proteasome inhibitors | 108 (21.5) | 121 (24.1) | 140 (8.1) | 180 (10.4) | 0.65 | 0.35 | 1.22 |
| Steroids | 126 (25.1) | 135 (26.9) | 178 (10.3) | 198 (11.4) | 1.58 | 0.95 | 2.65 |
| Cytotoxic chemotherapy | 46 (9.2) | 56 (11.2) | 99 (5.7) | 82 (4.7) | 0.44 | 0.31 | 0.63 |
| Stem cell transplant | 28 (5.6) | 11 (2.2) | 15 (0.9) | 18 (1.0) | 3.76 | 3.07 | 4.61 |
| Hospitalization | 65 (13.0) | 58 (11.6) | 70 (4.0) | 75 (4.3) | 1.24 | 1.15 | 1.35 |
| Colony stimulating factors | 20 (4.0) | 22 (4.4) | 44 (2.5) | 34 (2.0) | 0.48 | 0.33 | 0.70 |
| Central venous catheters | 57 (11.4) | 23 (4.6) | 42 (2.4) | 38 (2.2) | 2.56 | 2.28 | 2.87 |
| Erythropoietin-stimulating agents | 44 (8.8) | 27 (5.4) | 47 (2.7) | 47 (2.7) | 3.82 | 2.55 | 5.70 |
| Infection | 74 (14.7) | 45 (9.0) | 90 (5.2) | 87 (5.0) | 2.51 | 1.95 | 3.24 |
| Time-Varying Exposures | HR | 95% CI | HR | 95% CI | HR | 95% CI | HR | 95% CI | HR | 95% CI | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | Treated | Treated + Anticoagulation | Treated – Anticoagulation | Untreated | |||||||||||
| Thalidomide derivatives | 1.38 | 1.06 | 1.79 | 1.29 | 0.97 | 1.72 | 1.07 | 0.62 | 1.85 | 1.58 | 1.13 | 2.22 | -- | -- | -- |
| Proteasome Inhibitors | 0.80 | 0.51 | 1.26 | 0.73 | 0.46 | 1.16 | 1.93 | 0.74 | 5.06 | 0.52 | 0.31 | 0.89 | -- | -- | -- |
| Steroids | 1.54 | 1.21 | 1.96 | 2.18 | 1.60 | 2.95 | 2.81 | 1.43 | 5.55 | 2.05 | 1.45 | 2.90 | -- | -- | -- |
| Cytotoxic chemotherapy | 1.15 | 0.76 | 1.73 | 1.37 | 0.89 | 2.10 | 0.80 | 0.31 | 2.07 | 1.61 | 0.99 | 2.61 | -- | -- | -- |
| Infections | 2.29 | 1.80 | 2.92 | 1.88 | 1.28 | 2.77 | 1.42 | 0.49 | 4.13 | 1.84 | 1.21 | 2.79 | 2.15 | 1.55 | 2.98 |
| Erythropoiesis-stimulating agents | 1.03 | 0.64 | 1.67 | 1.08 | 0.63 | 1.87 | 1.09 | 0.37 | 3.20 | 1.33 | 0.71 | 2.49 | * | * | * |
| Colony stimulating factors | 0.93 | 0.43 | 1.99 | 1.09 | 0.50 | 2.39 | 2.28 | 0.47 | 10.94 | 0.93 | 0.37 | 2.33 | * | * | * |
| Stem cell transplant | 2.40 | 0.99 | 5.83 | 2.74 | 1.11 | 6.72 | * | * | * | 3.74 | 1.51 | 9.27 | -- | -- | -- |
| Central venous catheters | 2.02 | 1.65 | 2.49 | 1.51 | 1.14 | 2.01 | 1.42 | 0.79 | 2.57 | 1.60 | 1.16 | 2.22 | 3.00 | 2.24 | 4.11 |
| Hospitalization | 8.90 | 7.26 | 10.92 | 7.16 | 5.40 | 9.50 | 1.50 | 0.78 | 2.90 | 12.02 | 8.57 | 16.84 | 15.72 | 11.52 | 21.44 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brown, J.D.; Adams, V.R.; Moga, D.C. Impact of Time-Varying Treatment Exposures on the Risk of Venous Thromboembolism in Multiple Myeloma. Healthcare 2016, 4, 93. https://doi.org/10.3390/healthcare4040093
Brown JD, Adams VR, Moga DC. Impact of Time-Varying Treatment Exposures on the Risk of Venous Thromboembolism in Multiple Myeloma. Healthcare. 2016; 4(4):93. https://doi.org/10.3390/healthcare4040093
Chicago/Turabian StyleBrown, Joshua D., Val R. Adams, and Daniela C. Moga. 2016. "Impact of Time-Varying Treatment Exposures on the Risk of Venous Thromboembolism in Multiple Myeloma" Healthcare 4, no. 4: 93. https://doi.org/10.3390/healthcare4040093
APA StyleBrown, J. D., Adams, V. R., & Moga, D. C. (2016). Impact of Time-Varying Treatment Exposures on the Risk of Venous Thromboembolism in Multiple Myeloma. Healthcare, 4(4), 93. https://doi.org/10.3390/healthcare4040093






