Complementary and Alternative Medicine Use and Latina Breast Cancer Survivors’ Symptoms and Functioning
Abstract
:1. Introduction
1.1. Current Literature
1.2. Gaps in the Literature and Study Purpose
2. Materials and Methods
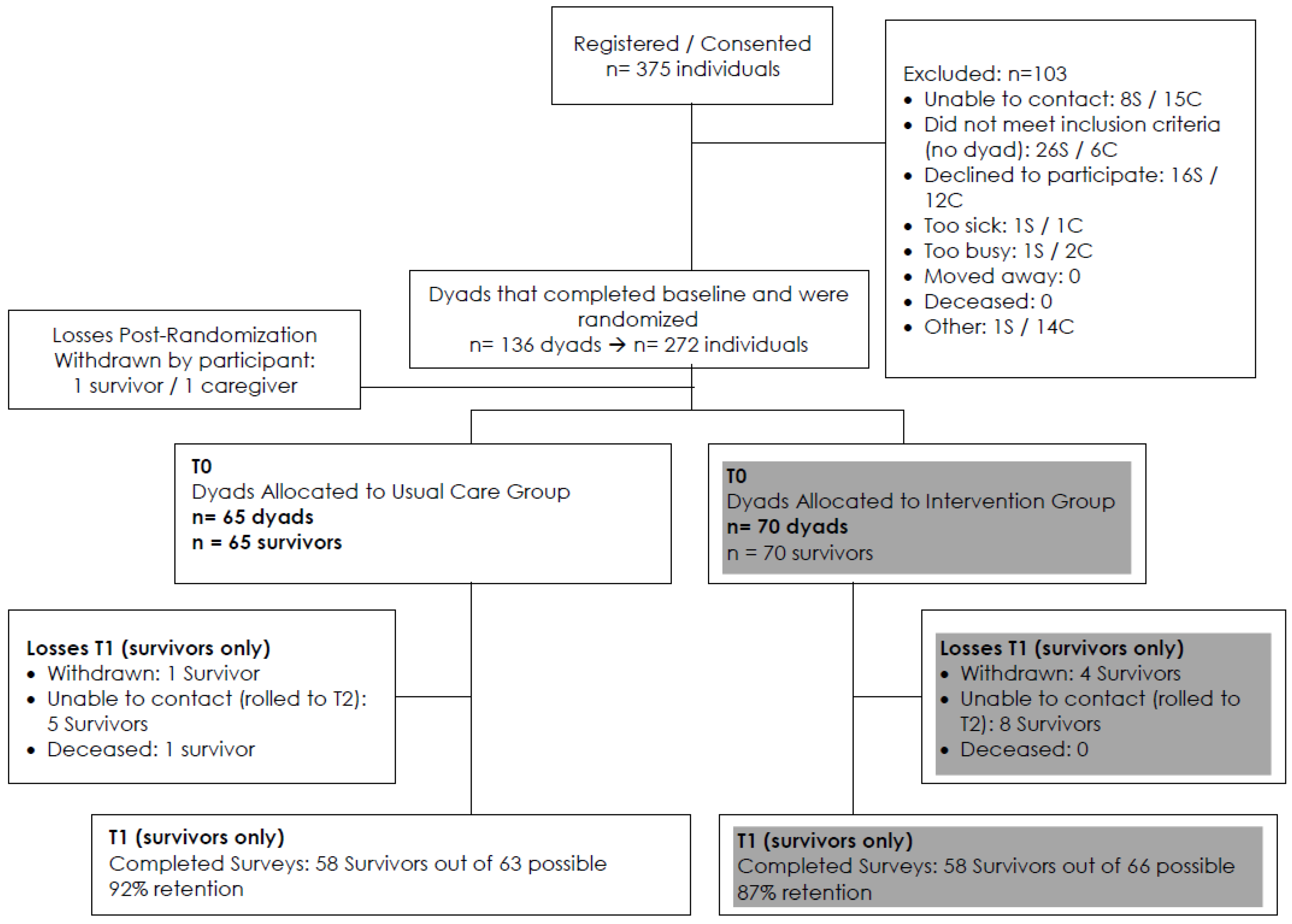
2.1. Participants
2.2. Procedures
2.2.1. Participating Organizations
2.3. Measures
2.3.1. Demographic and Clinical Variables
2.3.2. Patient-Reported Symptoms and Function
2.3.3. CAM Activities Questionnaire
2.3.4. Devotional and Spiritual Practices
2.4. Statistical Analyses
3. Results
3.1. Sample Characteristics
3.1.1. Demographics
3.1.2. CAM Activities
3.1.3. Devotional and Spiritual Practices
3.2. Baseline Cross-Sectional Analysis
3.2.1. Physical Function
3.2.2. Satisfaction with Participation in Social Roles
3.2.3. Emotional Distress: Anxiety
3.2.4. Emotional Distress: Depression
3.2.5. Fatigue
3.3. Longitudinal Analysis
3.3.1. Physical Function
3.3.2. Satisfaction with Participation in Social Roles
3.3.3. Emotional Distress: Anxiety
3.3.4. Emotional Distress: Depression
3.3.5. Fatigue
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- National Center for Complementary and Integrative Health (NCCIH); National Institutes of Health. Complementary, Alternative, or Integrative Health: What’s in a Name? Available online: https://nccih.nih.gov/health/integrative-health#cvsa (accessed on 6 July 2016).
- Brown, C.M.; Barner, J.C.; Richards, K.M.; Bohman, T.M. Patterns of complementary and alternative medicine use in African Americans. J Altern. Complement. Med. 2007, 13, 751–758. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.M.; Lin, S.S.; Wrensch, M.R.; Adler, S.R.; Eisenberg, D. Alternative therapies used by women with breast cancer in four ethnic populations. J. Natl. Cancer Inst. 2000, 92, 42–47. [Google Scholar] [CrossRef] [PubMed]
- Tippens, K.; Marsman, K.; Zwickey, H. Is prayer CAM? J. Altern. Complement. Med. 2009, 15, 435–438. [Google Scholar] [CrossRef] [PubMed]
- Gansler, T.; Kaw, C.; Crammer, C.; Smith, T. A population-based study of prevalence of complementary methods use by cancer survivors: A report from the American Cancer Society’s studies of cancer survivors. Cancer 2008, 113, 1048–1057. [Google Scholar] [CrossRef] [PubMed]
- Greenlee, H.; Kwan, M.L.; Ergas, I.J.; Sherman, K.J.; Krathwohl, S.E.; Bonnell, C.; Lee, M.M.; Kushi, L.H. Complementary and alternative therapy use before and after breast cancer diagnosis: The Pathways Study. Breast Cancer Res. Treat. 2009, 117, 653–665. [Google Scholar] [CrossRef] [PubMed]
- Matsuno, R.K.; Pagano, I.S.; Maskarinec, G.; Issell, B.F.; Gotay, C.C. Complementary and alternative medicine use and breast cancer prognosis: A pooled analysis of four population-based studies of breast cancer survivors. J. Womens Health 2012, 21, 1252–1258. [Google Scholar] [CrossRef] [PubMed]
- Culos-Reed, S.N.; Mackenzie, M.J.; Sohl, S.J.; Jesse, M.T.; Zahavich, A.N.; Danhauer, S.C. Yoga & cancer interventions: A review of the clinical significance of patient reported outcomes for cancer survivors. Evid. Based Complement. Alternat. Med. 2012. [Google Scholar] [CrossRef]
- Moadel, A.B.; Shah, C.; Wylie-Rosett, J.; Harris, M.S.; Patel, S.R.; Hall, C.B.; Sparano, J.A. Randomized controlled trial of yoga among a multiethnic sample of breast cancer patients: Effects on quality of life. J. Clin. Oncol. 2007, 25, 4387–4395. [Google Scholar] [CrossRef] [PubMed]
- Johannsen, M.; O’Connor, M.; O’Toole, M.S.; Jensen, A.B.; Hojris, I.; Zachariae, R. Efficacy of mindfulness-based cognitive therapy on late post-treatment pain in women treated for primary breast cancer: A randomized controlled trial. J. Clin. Oncol. 2016, 34, 3390–3399. [Google Scholar] [CrossRef] [PubMed]
- Wanchai, A.; Armer, J.M.; Stewart, B.R. Complementary and alternative medicine use among women with breast cancer: A systematic review. Clin. J. Oncol. Nurs. 2010, 14, E45–E55. [Google Scholar] [CrossRef] [PubMed]
- Brown, A. U.S. Hispanic and Asian Populations Growing, but for Different Reasons; Pew Research Center: Washington, DC, USA, 2014; Available online: http://www.pewresearch.org/fact-tank/2014/06/26/u-s-hispanic-and-asian-populations-growing-but-for-different-reasons/ (accessed on 6 July 2016).
- Owens, B.; Dirksen, S.R. Review and critique of the literature of complementary and alternative therapy use among Hispanic/Latino women with breast cancer. Clin. J. Oncol. Nurs. 2004, 8, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Owens, B. A test of the self-help model and use of complementary and alternative medicine among Hispanic women during treatment for breast cancer. Oncol. Nurs. Forum. 2007, 34, E42–E50. [Google Scholar] [CrossRef] [PubMed]
- Owens, B.; Jackson, M.; Berndt, A. Complementary therapy used by Hispanic women during treatment for breast cancer. J. Holist. Nurs. 2009, 27, 167–176. [Google Scholar] [CrossRef] [PubMed]
- Ashing-Giwa, K.T.; Padilla, G.V.; Bohorquez, D.E.; Tejero, J.S.; Garcia, M. Understanding the breast cancer experience of Latina women. J Psychosoc. Oncol. 2006, 24, 19–52. [Google Scholar] [CrossRef] [PubMed]
- Canada, A.L.; Murphy, P.E.; Fitchett, G.; Stein, K. Re-examining the contributions of faith, meaning, and peace to quality of life: A report from the American Cancer Society’s Studies of Cancer Survivors-II (SCS-II). Ann. Behav. Med. 2016, 50, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Gesselman, A.N.; Bigatti, S.M.; Garcia, J.R.; Coe, K.; Cella, D.; Champion, V.L. Spirituality, emotional distress, and post-traumatic growth in breast cancer survivors and their partners: An actor-partner interdependence modeling approach. Psychooncology 2016. [Google Scholar] [CrossRef] [PubMed]
- Mao, J.J.; Farrar, J.T.; Xie, S.X.; Bowman, M.A.; Armstrong, K. Use of complementary and alternative medicine and prayer among a national sample of cancer survivors compared to other populations without cancer. Complement. Ther. Med. 2007, 15, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Wildes, K.A.; Miller, A.R.; de Majors, S.S.; Ramirez, A.G. The religiosity/spirituality of Latina breast cancer survivors and influence on health-related quality of life. Psychooncology 2009, 18, 831–840. [Google Scholar] [CrossRef] [PubMed]
- Alferi, S.M.; Antoni, M.H.; Ironson, G.; Kilbourn, K.M.; Carver, C.S. Factors predicting the use of complementary therapies in a multi-ethnic sample of early-stage breast cancer patients. J. Am. Med. Womens Assoc. 2001, 56, 120–123, 126. [Google Scholar] [PubMed]
- Ernst, E. Complementary and alternative medicine (CAM) and cancer: The kind face of complementary medicine. Int. J. Surg. 2009, 7, 499–500. [Google Scholar] [CrossRef] [PubMed]
- Snyder, C.F.; Herman, J.M.; White, S.M.; Luber, B.S.; Blackford, A.L.; Carducci, M.A.; Wu, A.W. When using patient-reported outcomes in clinical practice, the measure matters: A randomized controlled trial. J. Oncol. Pract. 2014, 10, e299–e306. [Google Scholar] [CrossRef] [PubMed]
- Rush, C.L.; Darling, M.; Elliott, M.G.; Febus-Sampayo, I.; Kuo, C.; Munoz, J.; Duron, Y.; Torres, M.; Galvan, C.C.; Gonzalez, F.; et al. Engaging Latina cancer survivors, their caregivers, and community partners in a randomized controlled trial: Nueva Vida intervention. Qual. Life Res. 2015, 24, 1107–1118. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Cella, D.; Yount, S.; Rothrock, N.; Gershon, R.; Cook, K.; Reeve, B.; Ader, D.; Fries, J.F.; Bruce, B.; Rose, M. The Patient-Reported Outcomes Measurement Information System (PROMIS): Progress of an NIH Roadmap cooperative group during its first two years. Med. Care 2007, 45, S3–S11. [Google Scholar] [CrossRef] [PubMed]
- DeWalt, D.A.; Rothrock, N.; Yount, S.; Stone, A.A. Evaluation of item candidates: The PROMIS qualitative item review. Med. Care 2007, 45, S12–S21. [Google Scholar] [CrossRef] [PubMed]
- Reeve, B.B.; Hays, R.D.; Bjorner, J.B.; Cook, K.F.; Crane, P.K.; Teresi, J.A.; Thissen, D.; Revicki, D.A.; Weiss, D.J.; Hambleton, R.K.; et al. Psychometric evaluation and calibration of health-related quality of life item banks: Plans for the Patient-Reported Outcomes Measurement Information System (PROMIS). Med. Care 2007, 45, S22–S31. [Google Scholar] [CrossRef] [PubMed]
- Cella, D.; Gershon, R.; Bass, M.; Rothrock, N. Assessment Center. Available online: https://www.assessmentcenter.net/ (accessed on 6 July 2016).
- Liu, H.; Cella, D.; Gershon, R.; Shen, J.; Morales, L.S.; Riley, W.; Hays, R.D. Representativeness of the Patient-Reported Outcomes Measurement Information System Internet panel. J. Clin. Epidemiol. 2010, 63, 1169–1178. [Google Scholar] [CrossRef] [PubMed]
- Bock, R.D.; Mislevy, R.J. Adaptive EAP estimation of ability in a microcomputer environment. Appl. Psychol. Meas. 1982, 6, 431–444. [Google Scholar] [CrossRef]
- Jensen, R.E.; Moinpour, C.M.; Keegan, T.H.; Cress, R.D.; Wu, X.C.; Paddock, L.E.; Stroup, A.M.; Potosky, A.L. The Measuring Your Health study: Leveraging community-based cancer registry recruitment to establish a large, diverse cohort of cancer survivors for analyses of measurement equivalance and validity of the Patient Reported Outcomes Measurement Information System® (PROMIS®) short form items. Psychol. Test. Assess. Model. 2016, 58, 99–117. [Google Scholar]
- Cella, D.; Riley, W.; Stone, A.; Rothrock, N.; Reeve, B.; Yount, S.; Amtmann, D.; Bode, R.; Buysse, D.; Choi, S.; et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J. Clin. Epidemiol. 2010, 63, 1179–1194. [Google Scholar] [CrossRef] [PubMed]
- Cook, K.F.; Jensen, S.E.; Schalet, B.D.; Beaumont, J.L.; Amtmann, D.; Czajkowski, S.; DeWalt, D.A.; Fries, J.F.; Pilkonis, P.A.; Reeve, B.B.; et al. PROMIS measures of pain, fatigue, negative affect, physical function, and social function demonstrated clinical validity across a range of chronic conditions. J. Clin. Epidemiol. 2016, 73, 89–102. [Google Scholar] [CrossRef] [PubMed]
- Rothrock, N.E.; Hays, R.D.; Spritzer, K.; Yount, S.E.; Riley, W.; Cella, D. Relative to the general US population, chronic diseases are associated with poorer health-related quality of life as measured by the Patient-Reported Outcomes Measurement Information System (PROMIS). J. Clin. Epidemiol. 2010, 63, 1195–1204. [Google Scholar] [CrossRef] [PubMed]
- Jensen, R.E.; Potosky, A.L.; Reeve, B.B.; Hahn, E.; Cella, D.; Fries, J.; Smith, A.W.; Keegan, T.H.; Wu, X.C.; Paddock, L.; et al. Validation of the PROMIS physical function measures in a diverse US population-based cohort of cancer patients. Qual. Life Res. 2015, 24, 2333–2344. [Google Scholar] [CrossRef] [PubMed]
- Yost, K.J.; Eton, D.T.; Garcia, S.F.; Cella, D. Minimally important differences were estimated for six Patient-Reported Outcomes Measurement Information System-Cancer scales in advanced-stage cancer patients. J. Clin. Epidemiol. 2011, 64, 507–516. [Google Scholar] [CrossRef] [PubMed]
- Canada, A.L.; Fitchett, G.; Murphy, P.E.; Stein, K.; Portier, K.; Crammer, C.; Peterman, A.H. Racial/ethnic differences in spiritual well-being among cancer survivors. J. Behav. Med. 2013, 36, 441–453. [Google Scholar] [CrossRef] [PubMed]
- Levine, E.G.; Aviv, C.; Yoo, G.; Ewing, C.; Au, A. The benefits of prayer on mood and well-being of breast cancer survivors. Support. Care Cancer 2009, 17, 295–306. [Google Scholar] [CrossRef] [PubMed]
- Prince, P.; Mitchell, S.A.; Wehrlen, L.; Childs, R.; Savani, B.; Yang, L.; Bevans, M. Spiritual well-being in Hispanic and non-Hispanic survivors of allogeneic hematopoietic stem cell transplantation. J. Psychosoc. Oncol. 2015, 33, 635–654. [Google Scholar] [CrossRef] [PubMed]
- Bai, M.; Lazenby, M. A systematic review of associations between spiritual well-being and quality of life at the scale and factor levels in studies among patients with cancer. J. Palliat. Med. 2015, 18, 286–298. [Google Scholar] [CrossRef] [PubMed]
- Winger, J.G.; Adams, R.N.; Mosher, C.E. Relations of meaning in life and sense of coherence to distress in cancer patients: A meta-analysis. Psychooncology 2016, 25, 2–10. [Google Scholar] [CrossRef] [PubMed]
- DiGianni, L.M.; Garber, J.E.; Winer, E.P. Complementary and alternative medicine use among women with breast cancer. J. Clin. Oncol. 2002, 20, 34S–38S. [Google Scholar] [PubMed]
| Baseline and Follow-Up Measures | Selected Sample Questions |
|---|---|
| Demographics and Clinical | Education, income, insurance, breast cancer stage, age, time since diagnosis, employment, marital status. |
| PROMIS Emotional Distress: Anxiety (6a) | My worries overwhelmed me. |
| PROMIS Emotional Distress: Depression (6a) | I felt hopeless. |
| PROMIS Physical Function (6b) | Are you able to do chores such as vacuuming or yard work? |
| PROMIS Fatigue (6a) | I have trouble starting things because I am tired. |
| PROMIS Satisfaction with Participation in Social Roles(6a) | I am satisfied with my ability to meet the needs of those who depend on me. |
CAM Activities Questionnaire
| Do you practice any complementary and alternative medicine (for example, yoga, massage, meditation, herbal / dietary practices)? If yes, how often? If yes, please describe: |
| Spirituality/Devotional Practices | Do you currently have spirituality or devotional practices? If yes, how often? |
| Baseline | Baseline | Follow-Up | ||||
|---|---|---|---|---|---|---|
| All | (UC Only) | (UC Only) | ||||
| N | % | n | % | n | % | |
| All | 136 | 100 | 65 | 100 | 58 | 100 |
| Time Since Dx (in Years) | Mean ± SD | Mean ± SD | Mean ± SD | |||
| 132 | 3.31 ± 4.60 | 64 | 3.23 ± 4.21 | 57 | 3.42 ± 4.40 | |
| Survey Language | ||||||
| English | 10 | 7 | 5 | 8 | 3 | 5 |
| Spanish | 126 | 93 | 60 | 92 | 55 | 95 |
| Race | ||||||
| Black or African American | 8 | 6 | 5 | 8 | 5 | 9 |
| White or Caucasian | 39 | 29 | 17 | 26 | 15 | 26 |
| More than One Race | 59 | 43 | 31 | 48 | 29 | 50 |
| Don’t Know/Unsure/Prefer Not to Answer | 30 | 22 | 12 | 18 | 9 | 16 |
| Marital Status | ||||||
| Single/Separated/Divorced/Widowed | 59 | 43 | 27 | 42 | 22 | 38 |
| Married/Living with a Partner | 77 | 57 | 38 | 58 | 36 | 62 |
| Age at Diagnosis | ||||||
| <50 | 75 | 55 | 36 | 55 | 33 | 57 |
| 50+ | 61 | 45 | 29 | 45 | 25 | 43 |
| Age at Survey Completion | ||||||
| Missing | 2 | 1 | 1 | 2 | 1 | 2 |
| <50 | 52 | 38 | 26 | 40 | 23 | 40 |
| 50+ | 82 | 60 | 38 | 58 | 34 | 59 |
| Stage | ||||||
| Stage 0/I/Unknown | 96 | 71 | 48 | 74 | 46 | 79 |
| Stage II | 22 | 16 | 9 | 14 | 7 | 12 |
| Stage III/IV | 18 | 13 | 8 | 12 | 5 | 9 |
| Education | ||||||
| ≤High school diploma, or GED | 84 | 62 | 37 | 57 | 34 | 59 |
| >High school | 52 | 38 | 28 | 43 | 24 | 41 |
| Employment | ||||||
| Working | 44 | 32 | 20 | 31 | 20 | 34 |
| Not working | 92 | 68 | 45 | 69 | 38 | 66 |
| Income | ||||||
| <$30,000 (includes prefer not to answer/unsure n = 43) | 105 | 77 | 51 | 78 | 45 | 78 |
| >$30,000 | 31 | 23 | 14 | 22 | 13 | 22 |
| Insurance | ||||||
| Group Insurance/Private/Non-government | 27 | 20 | 14 | 22 | 13 | 22 |
| Government (includes Don’t know/Unsure n = (26) | 109 | 80 | 51 | 78 | 45 | 78 |
| Years in the US | ||||||
| Missing | 5 | 4 | 2 | 3 | 2 | 3 |
| 1–10 years | 22 | 16 | 12 | 18 | 11 | 19 |
| 11+ years | 109 | 80 | 51 | 78 | 45 | 78 |
| Surgery | ||||||
| No | 34 | 25 | 16 | 25 | 14 | 24 |
| Yes, Any surgery | 102 | 75 | 49 | 75 | 44 | 76 |
| Yes, Mastectomy | 71 | 52 | 27 | 42 | 19 | 41 |
| Yes, Lumpectomy | 30 | 22 | 15 | 23 | 9 | 20 |
| Chemotherapy | ||||||
| No | 61 | 45 | 26 | 40 | 25 | 43 |
| Yes | 75 | 55 | 39 | 60 | 33 | 57 |
| Hormonal Therapy | ||||||
| No | 84 | 62 | 40 | 62 | 35 | 60 |
| Yes | 52 | 38 | 25 | 38 | 23 | 40 |
| Radiation Therapy | ||||||
| No | 75 | 55 | 35 | 54 | 31 | 53 |
| Yes | 61 | 45 | 30 | 46 | 27 | 47 |
| Complementary & Alternative Medicine Use Baseline | ||||||
| Yes, CAM, Overall | 47 | 35 | 24 | 37 | 21 | 36 |
| CAM Overall, One or more times per week | 22 | 16 | 11 | 17 | 9 | 16 |
| CAM Overall, < One or more times/month | 25 | 18 | 13 | 20 | 12 | 21 |
| Yes, CAM, Yoga/Meditation/Massages/Herbal Supplements | 43 | 32 | 21 | 32 | 18 | 31 |
| Devotional and Spiritual Practices Baseline | ||||||
| Yes, Devotional/Spiritual Practices, Overall | 109 | 80 | 54 | 83 | 49 | 84 |
| D/S * Overall, 1 or more times/week | 86 | 63 | 41 | 63 | 36 | 62 |
| D/S Overall, <One or more times/month | 23 | 17 | 13 | 20 | 13 | 22 |
| Yes, Church | 95 | 70 | 44 | 68 | 40 | 69 |
| Yes, Prayer/Religious Groups/Bible Study | 30 | 22 | 18 | 28 | 16 | 28 |
| Complementary & Alternative Medicine and Devotional/Spiritual Practices (Post Intervention) | ||||||
| Yes, CAM, Overall | 18 | 28 | 22 | 38 | ||
| Yes, CAM, Yoga/Meditation/Massages/Herbal Supplements | 17 | 26 | 20 | 34 | ||
| Yes, Devotional/Spiritual Practices, Overall | 37 | 57 | 47 | 81 | ||
| Yes, Church | 33 | 51 | 43 | 74 | ||
| Yes, Prayer/Prayer or Religious Groups/Bible Study | 10 | 15 | 15 | 26 | ||
| Symptoms and Functioning | Baseline | Baseline | Follow-Up | |||
| All | (UC Only) | (UC Only) | ||||
| Baseline Physical Functioning Mean ± SD | 44.28 ± 9.34 | 44.33 ± 9.64 | 44.71± 9.91 | |||
| Baseline Satisfaction with Social Roles Mean ± SD | 48.35 ± 7.65 | 48.99 ± 7.71 | 49.39 ± 6.95 | |||
| Baseline Anxiety Mean ± SD | 53.63 ± 11.55 | 52.94 ± 9.95 | 52.31 ± 9.60 | |||
| Baseline Depression Mean ± SD | 49.83 ± 10.97 | 48.22 ± 9.52 | 47.80 ± 9.30 | |||
| Baseline Fatigue Mean ± SD | 51.41 ± 12.6 | 49.57 ± 11.99 | 49.19 ± 11.71 | |||
| QOL Outcomes | Baseline | Follow-up |
|---|---|---|
| Physical Function | CAM: β = 3.48, p < 0.05 | Baseline CAM β = 3.48, p < 0.05 |
| D/S *: p > 0.05 | Baseline D/S: p > 0.05 | |
| Satisfaction with Social Roles | CAM: p > 0.05 | Baseline CAM: p > 0.05 |
| D/S: p > 0.05 | Baseline D/S: p > 0.05 | |
| Anxiety | CAM: p > 0.05 | Baseline CAM: p > 0.05 |
| D/S: p > 0.05 | Baseline D/S: β = 6.48, p < 0.05 | |
| Depression | CAM: β = −5.49, p < 0.01 | Baseline CAM: p > 0.05 |
| D/S: p > 0.05 | Baseline D/S: β = 7.69, p < 0.05 | |
| Fatigue | CAM: p > 0.05 | Baseline CAM: p > 0.05 |
| D/S: p > 0.05 | Baseline D/S β = −7.12, p < 0.05 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rush, C.L.; Lobo, T.; Serrano, A.; Blasini, M.; Campos, C.; Graves, K.D. Complementary and Alternative Medicine Use and Latina Breast Cancer Survivors’ Symptoms and Functioning. Healthcare 2016, 4, 80. https://doi.org/10.3390/healthcare4040080
Rush CL, Lobo T, Serrano A, Blasini M, Campos C, Graves KD. Complementary and Alternative Medicine Use and Latina Breast Cancer Survivors’ Symptoms and Functioning. Healthcare. 2016; 4(4):80. https://doi.org/10.3390/healthcare4040080
Chicago/Turabian StyleRush, Christina L., Tania Lobo, Adriana Serrano, Maxie Blasini, Claudia Campos, and Kristi D. Graves. 2016. "Complementary and Alternative Medicine Use and Latina Breast Cancer Survivors’ Symptoms and Functioning" Healthcare 4, no. 4: 80. https://doi.org/10.3390/healthcare4040080
APA StyleRush, C. L., Lobo, T., Serrano, A., Blasini, M., Campos, C., & Graves, K. D. (2016). Complementary and Alternative Medicine Use and Latina Breast Cancer Survivors’ Symptoms and Functioning. Healthcare, 4(4), 80. https://doi.org/10.3390/healthcare4040080





