A Cross-Sectional Evaluation of Caregiver Burden in Schizophrenia Care: Findings from Western Saudi Arabia with Policy Implications for Preventive Mental Healthcare
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Description
2.2. Sampling Procedures
2.3. Data Collection Steps
2.4. Data Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. Mental Health. Available online: https://www.who.int/health-topics/mental-health#tab=tab_1 (accessed on 28 November 2024).
- GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry 2022, 9, 137–150. [Google Scholar] [CrossRef]
- Solmi, M.; Seitidis, G.; Mavridis, D.; Correll, C.U.; Dragioti, E.; Guimond, S.; Tuominen, L.; Dargél, A.; Carvalho, A.F.; Fornaro, M.; et al. Incidence, prevalence, and global burden of schizophrenia-data, with critical appraisal, from the Global Burden of Disease (GBD) 2019. Mol. Psychiatry 2023, 28, 5319–5327. [Google Scholar] [CrossRef] [PubMed]
- Świtaj, P.; Anczewska, M.; Chrostek, A.; Sabariego, C.; Cieza, A.; Bickenbach, J.; Chatterji, S. Disability and schizophrenia: A systematic review of experienced psychosocial difficulties. BMC Psychiatry 2012, 12, 193. [Google Scholar] [CrossRef] [PubMed]
- WHO. Schizophrenia. Available online: https://www.who.int/news-room/fact-sheets/detail/schizophrenia (accessed on 10 May 2025).
- Hany, M.; Rehman, B.; Rizvi, A.; Chapman, J. Schizophrenia. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- NIMH. Schizophrenia. Available online: https://www.nimh.nih.gov/health/statistics/schizophrenia (accessed on 22 November 2024).
- Hajebi, A.; Naserbakht, M.; Minoletti, A. Burden experienced by caregivers of schizophrenia patients and its related factors. Med. J. Islam. Repub. Iran 2019, 33, 54. [Google Scholar] [CrossRef] [PubMed]
- Peng, M.M.; Ma, Z.; Ran, M.S. Family caregiving and chronic illness management in schizophrenia: Positive and negative aspects of caregiving. BMC Psychol. 2022, 10, 83. [Google Scholar] [CrossRef]
- Liu, Z.; Heffernan, C.; Tan, J. Caregiver burden: A concept analysis. Int. J. Nurs. Sci. 2020, 7, 438–445. [Google Scholar] [CrossRef]
- Karambelas, G.J.; Filia, K.; Byrne, L.K.; Allott, K.A.; Jayasinghe, A.; Cotton, S.M. A systematic review comparing caregiver burden and psychological functioning in caregivers of individuals with schizophrenia spectrum disorders and bipolar disorders. BMC Psychiatry 2022, 22, 422. [Google Scholar] [CrossRef]
- Cham, C.Q.; Ibrahim, N.; Siau, C.S.; Kalaman, C.R.; Ho, M.C.; Yahya, A.N.; Visvalingam, U.; Roslan, S.; Abd Rahman, F.N.; Lee, K.W. Caregiver Burden among Caregivers of Patients with Mental Illness: A Systematic Review and Meta-Analysis. Healthcare 2022, 10, 2423. [Google Scholar] [CrossRef]
- Strunoiu, L.M.; Strunoiu, C.M.; Chirita, A.L.; Pirlog, M.C.; Tica, A.A. Factors that Impact Caregivers of Patients with Schizophrenia. Curr. Health Sci. J. 2019, 45, 301–310. [Google Scholar] [CrossRef]
- Kaya, Y.; Öz, F. Global social functioning of patients with schizophrenia and care burden of caregiving relatives. J. Psychiatr. Nurs. 2019, 10, 28–38. [Google Scholar]
- Tamizi, Z.; Fallahi-Khoshknab, M.; Dalvandi, A.; Mohammadi-Shahboulaghi, F.; Mohammadi, E.; Bakhshi, E. Caregiving burden in family caregivers of patients with schizophrenia: A qualitative study. J. Educ. Health Promot. 2020, 9, 12. [Google Scholar] [CrossRef] [PubMed]
- Gagiu, C.; Dionisie, V.; Manea, M.C.; Covaliu, A.; Vlad, A.D.; Tupu, A.E.; Manea, M. Quality of Life in Caregivers of Patients with Schizophrenia: A Systematic Review of the Impact of Sociodemographic, Clinical, and Psychological Factors. Behav. Sci. 2025, 15, 684. [Google Scholar] [CrossRef] [PubMed]
- Sharif, L.; Basri, S.; Alsahafi, F.; Altaylouni, M.; Albugumi, S.; Banakhar, M.; Mahsoon, A.; Alasmee, N.; Wright, R.J. An Exploration of Family Caregiver Experiences of Burden and Coping While Caring for People with Mental Disorders in Saudi Arabia-A Qualitative Study. Int. J. Environ. Res. Public Health 2020, 17, 6405. [Google Scholar] [CrossRef]
- Almulla, H.; Aljaloud, O.; Almulla, H.; Nasser, S. Caregiver burden, perceived stress, and social support among parents of chronically Ill children in Saudi Arabia. BMC Nurs. 2024, 23, 811. [Google Scholar] [CrossRef]
- Al-Subaie, A.S.; Al-Habeeb, A.; Altwaijri, Y.A. Overview of the Saudi National Mental Health Survey. Int. J. Methods Psychiatr. Res. 2020, 29, e1835. [Google Scholar] [CrossRef]
- Carlisle, J. Mental health law in Saudi Arabia. BJPsych. Int. 2018, 15, 17–19. [Google Scholar] [CrossRef]
- AlFattani, A.; Bilal, L.; Saad, S.Y.; Naseem, M.T.; Hyder, S.; Alhabib, A.; Alsubaie, A.; Altwaijri, Y. Effect of perceived stigma on work and social roles among individuals with mental health disorders in Saudi Arabia: Findings from a national survey. Ann. Gen. Psychiatry 2023, 22, 54. [Google Scholar] [CrossRef]
- Alamer, M.; Alsaad, A.; Al-Ghareeb, M.; Almomatten, A.; Alaethan, M.; AlAmeer, M.A. Mental Stigma Among Al-Ahsa Population in Saudi Arabia. Cureus 2021, 13, e19710. [Google Scholar] [CrossRef]
- Alyafei, A.H.; Alqunaibet, T.; Mansour, H.; Ali, A.; Billings, J. The experiences of family caregivers of people with severe mental illness in the Middle East: A systematic review and meta-synthesis of qualitative data. PLoS ONE 2021, 16, e0254351. [Google Scholar] [CrossRef]
- Sampogna, G.; Brohan, E.; Luciano, M.; Chowdhary, N.; Fiorillo, A. Psychosocial interventions for carers of people with severe mental and substance use disorders: A systematic review and meta-analysis. Eur. Psychiatry 2023, 66, e98. [Google Scholar] [CrossRef]
- Kojima, Y.; Yamada, S.; Kamijima, K.; Kogushi, K.; Ikeda, S. Burden in caregivers of patients with schizophrenia, depression, dementia, and stroke in Japan: Comparative analysis of quality of life, work productivity, and qualitative caregiving burden. BMC Psychiatry 2024, 24, 591. [Google Scholar] [CrossRef]
- Rahmani, F.; Roshangar, F.; Gholizadeh, L.; Asghari, E. Caregiver burden and the associated factors in the family caregivers of patients with schizophrenia. Nurs. Open 2022, 9, 1995–2002. [Google Scholar] [CrossRef] [PubMed]
- Ali, S.; Tallent, J.; Sambrook, H.; MacInnes, D.; Kinane, C. Effectiveness of psychological interventions for carers of patients with severe mental illness (SMI): A systematic review. BMJ Open 2024, 14, e086149. [Google Scholar] [CrossRef] [PubMed]
- Sharif, L.; Al-Zahrani, M.S.; Alanzi, F.R.; Mahsoon, A.; Sharif, K.; Al-Qubali, S.A.; Wright, R.J.; El-Ashry, A.M. Effectiveness of Psychoeducation via Telenursing on Reducing Caregiver Burden Among Caregivers for Patients with Schizophrenia in Saudi Arabia: A Quasi-Experimental Study. Healthcare 2025, 13, 1922. [Google Scholar] [CrossRef]
- Chou, K.R.; Liu, S.Y.; Chu, H. The effects of support groups on caregivers of patients with schizophrenia. Int. J. Nurs. Stud. 2002, 39, 713–722. [Google Scholar] [CrossRef]
- O’Neill, B. Sample size determination with a pilot study. PLoS ONE 2022, 17, e0262804. [Google Scholar] [CrossRef]
- Naing, L.; Nordin, R.B.; Abdul Rahman, H.; Naing, Y.T. Sample size calculation for prevalence studies using Scalex and ScalaR calculators. BMC Med. Res. Methodol. 2022, 22, 209. [Google Scholar] [CrossRef]
- Tsang, S.; Royse, C.F.; Terkawi, A.S. Guidelines for developing, translating, and validating a questionnaire in perioperative and pain medicine. Saudi J. Anaesth. 2017, 11, S80–S89. [Google Scholar] [CrossRef]
- Wisconsin Alzheimer’s Institute. Zarit Burden Interview Assessing Caregiver Burden. Available online: https://wai.wisc.edu/wp-content/uploads/sites/1129/2021/11/Zarit-Caregiver-Burden-Assessment-Instruments.pdf (accessed on 2 March 2025).
- Zarit, S.H.; Reever, K.E.; Bach-Peterson, J. Relatives of the Impaired Elderly: Correlates of Feelings of Burden. Gerontologist 1980, 20, 649–655. [Google Scholar] [CrossRef]
- Kadam, K.S.; Unnithan, V.B.; Mane, M.R.; Angane, A.Y. Brewing Caregiver Burden: Indian Insights into Alcohol Use Disorder. Indian J. Soc. Psychiatry 2020, 36, 236–242. [Google Scholar] [CrossRef]
- Elmståhl, S.; Dahlrup, B.; Ekström, H.; Nordell, E. The association between medical diagnosis and caregiver burden: A cross-sectional study of recipients of informal support and caregivers from the general population study ‘Good Aging in Skåne’, Sweden. Aging Clin. Exp. Res. 2018, 30, 1023–1032. [Google Scholar] [CrossRef]
- Eze, N.C.; Ezeugwu, C.G.; Eze, R.N.; Soronnadi, C.N.; Orji, C.J.; Chime, O.H. Caregiving Burden and Coping Strategies Among Informal Caregivers of Cancer Patients in Nigeria: From Duty to Distress. Int. J. Public Health 2025, 70, 1607735. [Google Scholar] [CrossRef]
- Broxson, J.; Feliciano, L. Understanding the Impacts of Caregiver Stress. Prof. Case Manag. 2020, 25, 213–219. [Google Scholar] [CrossRef] [PubMed]
- Oleas Rodríguez, D.A.; Yong Peña, C.; Garza Olivares, X.; Teixeira Filho, F.S.; Lucero Córdova, J.E.; Salas Naranjo, A.J. Emotional Coping Strategies for Informal Caregivers of Hospitalized Patients: A Study of Distress and Overload. Psychol. Res. Behav. Manag. 2024, 17, 725–734. [Google Scholar] [CrossRef]
- Wang, X.; Chen, Q.; Yang, M. Effect of caregivers’ expressed emotion on the care burden and rehospitalization rate of schizophrenia. Patient Prefer. Adherence 2017, 11, 1505–1511. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.Y.; Pohlig, R.; Habermann, B. Impacts of Perceived Choice on Physical Strain, Emotional Stress and Health among Caregivers. West. J. Nurs. Res. 2023, 45, 826–832. [Google Scholar] [CrossRef] [PubMed]
- Kamil, S.H.; Velligan, D.I. Caregivers of individuals with schizophrenia: Who are they and what are their challenges? Curr. Opin. Psychiatry 2019, 32, 157–163. [Google Scholar] [CrossRef]
- Addo, R.; Agyemang, S.A.; Tozan, Y.; Nonvignon, J. Economic burden of caregiving for persons with severe mental illness in sub-Saharan Africa: A systematic review. PLoS ONE 2018, 13, e0199830. [Google Scholar] [CrossRef]
- Al-Awad, F. Perceived Burden and Quality of Life in Caregivers of Patients with Schizophrenia in Saudi Arabia’s Eastern Province: A Cross-sectional Study. Clin. Pract. Epidemiol. Ment. Health 2024, 20, e17450179314013. [Google Scholar] [CrossRef]
- Issac, A.; Nayak, S.G.; Yesodharan, R.; Sequira, L. Needs, challenges, and coping strategies among primary caregivers of schizophrenia patient: A systematic review & meta-synthesis. Arch. Psychiatr. Nurs. 2022, 41, 317–332. [Google Scholar] [CrossRef]
- Stanley, S.; Balakrishnan, S. Family Caregiving in Schizophrenia: Do stress, social support and resilience influence life satisfaction?-A quantitative study from India. Soc. Work. Ment. Health 2023, 21, 67–85. [Google Scholar] [CrossRef]
- Wang, Y.Z.; Meng, X.D.; Zhang, T.M.; Weng, X.; Li, M.; Luo, W.; Huang, Y.; Thornicroft, G.; Ran, M.S. Affiliate stigma and caregiving burden among family caregivers of persons with schizophrenia in rural China. Int. J. Soc. Psychiatry 2023, 69, 1024–1032. [Google Scholar] [CrossRef]
- Ong, H.C.; Ibrahim, N.; Wahab, S. Psychological distress, perceived stigma, and coping among caregivers of patients with schizophrenia. Psychol. Res. Behav. Manag. 2016, 9, 211–218. [Google Scholar] [CrossRef] [PubMed]
- Alhumaidan, N.I.; Alotaibi, T.A.; Aloufi, K.S.; Althobaiti, A.A.; Althobaiti, N.S.A.; Althobaiti, K.; Almutiri, W.A.; Alhaqbani, K.; Alboqami, T.; Albeheiri, L.; et al. Barriers to Seeking Mental Health Help in Saudi Arabia: A Systematic Review. Cureus 2024, 16, e60363. [Google Scholar] [CrossRef] [PubMed]
- Phillips, R.; Durkin, M.; Engward, H.; Cable, G.; Iancu, M. The impact of caring for family members with mental illnesses on the caregiver: A scoping review. Health Promot. Int. 2023, 38, daac049. [Google Scholar] [CrossRef]
- Gilsenan, J.; Gorman, C.; Shevlin, M. Explaining caregiver burden in a large sample of UK dementia caregivers: The role of contextual factors, behavioural problems, psychological resilience, and anticipatory grief. Aging Ment. Health 2023, 27, 1274–1281. [Google Scholar] [CrossRef]
- Grover, S.; Sarkar, S.; Naskar, C.; Kamal, N. Caregiver burden as perceived by caregivers of patients with schizophrenia: A meta-analysis of Indian studies. Asian J. Psychiatry 2025, 106, 104421. [Google Scholar] [CrossRef]
- Mital, A.K.; Sabnis, S.G.; Kulkarni, V.V. Caregiver Burden in Medical versus Psychiatric Patients: A Cross-sectional Comparative Study. Indian J. Psychol. Med. 2017, 39, 777–784. [Google Scholar] [CrossRef]
- Ampalam, P.; Gunturu, S.; Padma, V. A comparative study of caregiver burden in psychiatric illness and chronic medical illness. Indian J. Psychiatry 2012, 54, 239–243. [Google Scholar] [CrossRef]
- Shamsaei, F.; Cheraghi, F.; Bashirian, S. Burden on Family Caregivers Caring for Patients with Schizophrenia. Iran. J. Psychiatry 2015, 10, 239–245. [Google Scholar]
| Characteristics | Frequency | Percentage |
|---|---|---|
| Patients’ characteristics | ||
| Age | ||
| Less than 20 years | 105 | 31.8 |
| 20 to 40 years | 141 | 42.7 |
| More than 40 years | 84 | 25.5 |
| Gender | ||
| Female | 136 | 41.2 |
| Male | 194 | 58.8 |
| Duration since diagnosis | ||
| Less than 2 years | 101 | 30.6 |
| 2 to 5 years | 136 | 41.2 |
| More than 5 years | 93 | 28.2 |
| Caregivers’ characteristics | ||
| Age | ||
| Less than 40 years | 110 | 33.3 |
| 40 to 50 years | 138 | 41.8 |
| More than 50 years | 82 | 24.8 |
| Gender | ||
| Female | 179 | 54.2 |
| Male | 151 | 45.8 |
| Education level | ||
| Up to high school | 101 | 30.7 |
| Bachelor’s degree | 101 | 30.6 |
| Postgraduate degree | 128 | 38.7 |
| Occupation | ||
| Private | 98 | 29.7 |
| Government | 130 | 39.4 |
| Unemployed | 64 | 19.4 |
| Retired | 38 | 11.5 |
| Monthly income | ||
| Less than 5000 SAR | 100 | 30.3 |
| 5000 to 7000 SAR | 134 | 40.6 |
| More than 7000 SAR | 96 | 29.1 |
| Perceived social support | ||
| No support | 122 | 37.0 |
| Some support | 110 | 33.3 |
| Enough support | 98 | 29.7 |
| Relationship with the patients | ||
| Extended family (Uncles, aunts, etc.) | 30 | 9.1 |
| Siblings | 54 | 16.4 |
| Spouse | 82 | 24.8 |
| Adult children caring for parents | 77 | 23.3 |
| Parents | 87 | 26.4 |
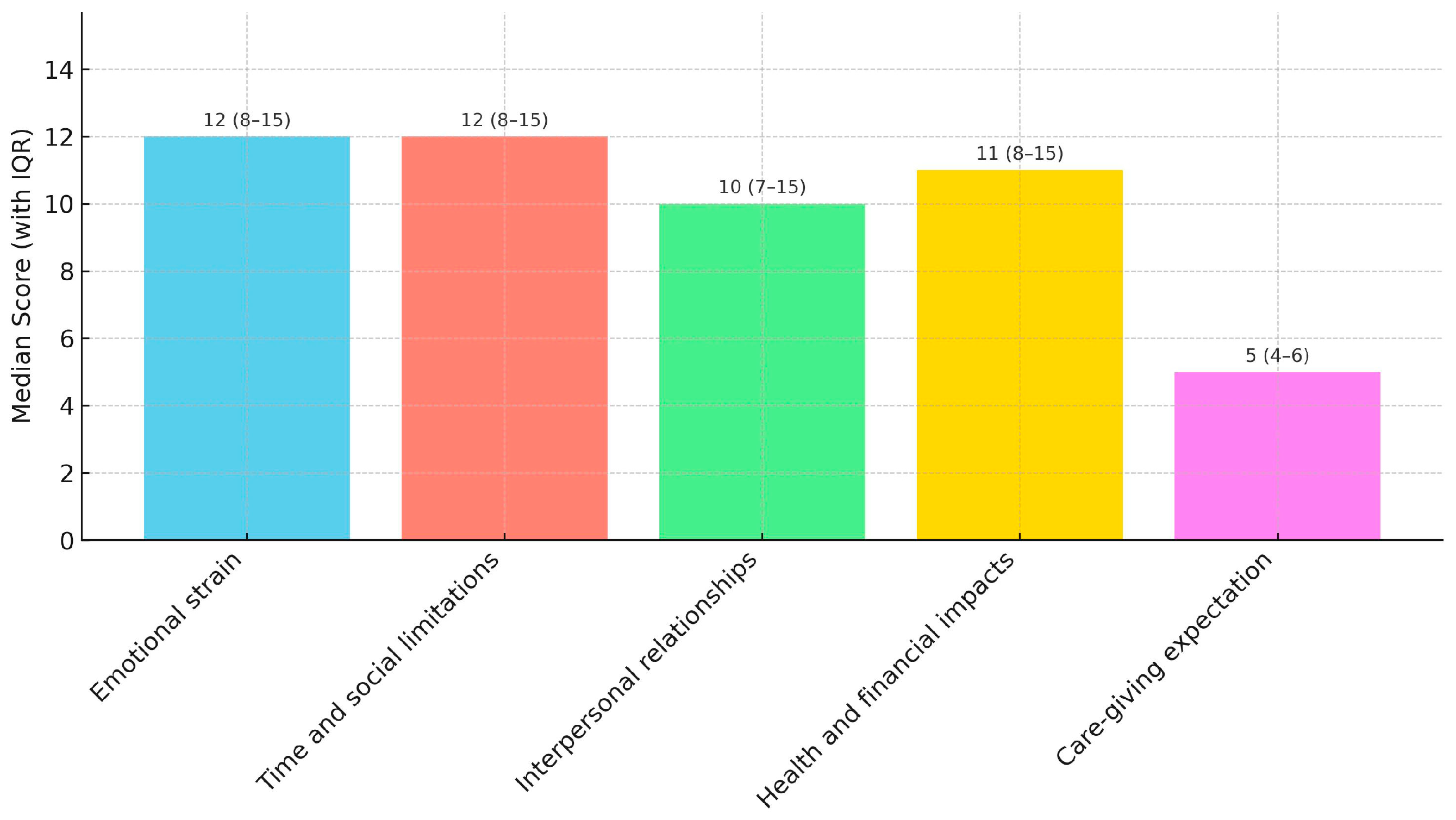
| Domains | Mean ± SD | Median (IQR) |
|---|---|---|
| Emotional strain | 11.52 ± 4.3 | 12 (8–15) |
| Time and social limitations | 11.29 ± 5.07 | 12 (8–15) |
| Interpersonal relationships and dependency | 10.51 ± 4.95 | 10 (7–15) |
| Health and financial impacts | 11.08 ± 5.08 | 11 (8–15) |
| Care-giving expectation | 4.79 ± 2.14 | 5 (4–6) |
| Total | 49.18 ± 17.33 | 57 (40–60) |
| Variables | Frequency | Emotional Strain | Time and Social Limitations | Interpersonal Relationships and Dependency | Health and Financial Impacts | Care Giving Expectation | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean Rank | p Value | Mean Rank | p Value | Mean Rank | p Value | Mean Rank | p Value | Mean Rank | p Value | ||
| Patients’ characteristics | |||||||||||
| Age | 0.727 | 0.198 | 0.385 | 0.606 | 0.820 | ||||||
| Less than 20 years | 105 | 169.77 | 175.27 | 169.04 | 172.20 | 165.51 | |||||
| 20 to 40 years | 141 | 160.70 | 154.72 | 157.47 | 159.98 | 162.44 | |||||
| More than 40 years | 84 | 168.21 | 171.38 | 174.55 | 166.39 | 170.62 | |||||
| Gender | 0.376 | 0.629 | 0.796 | 0.988 | 0.676 | ||||||
| Female | 136 | 159.96 | 168.53 | 163.89 | 165.40 | 162.91 | |||||
| Male | 194 | 169.38 | 163.38 | 166.63 | 165.57 | 167.32 | |||||
| Duration since diagnosis | 0.404 | 0.132 | 0.379 | 0.822 | 0.695 | ||||||
| Less than 2 years | 101 | 168.07 | 172.92 | 165.08 | 169.88 | 167.12 | |||||
| 2 to 5 years | 136 | 157.57 | 152.98 | 158.45 | 162.07 | 160.53 | |||||
| More than 5 years | 93 | 174.30 | 175.76 | 176.27 | 165.76 | 171.01 | |||||
| Caregivers’ characteristics | |||||||||||
| Age | 0.935 | 0.731 | 0.338 | 0.390 | 0.011 | ||||||
| Less than 40 years | 110 | 163.57 | 160.67 | 155.37 | 155.74 | 150.10 | |||||
| 40 to 50 years | 138 | 167.74 | 165.69 | 167.69 | 168.47 | 168.68 | |||||
| More than 50 years | 82 | 164.33 | 171.66 | 171.66 | 173.59 | 180.82 | |||||
| Gender | 0.114 | 0.759 | 0.585 | 0.607 | 0.872 | ||||||
| Female | 179 | 173.10 | 166.97 | 162.87 | 167.97 | 164.73 | |||||
| Male | 151 | 156.49 | 163.75 | 168.61 | 162.57 | 166.41 | |||||
| Education level | 0.132 | 0.365 | 0.454 | 0.516 | 0.992 | ||||||
| Up to high school | 101 | 166.93 | 176.53 | 173.81 | 167.90 | 163.23 | |||||
| Bachelor’s degree | 101 | 174.33 | 162.56 | 162.56 | 156.28 | 165.22 | |||||
| Postgraduate degree | 128 | 152.71 | 157.44 | 157.44 | 167.76 | 166.60 | |||||
| Occupation | 0.756 | 0.012 | 0.222 | 0.279 | 0.516 | ||||||
| Private | 98 | 157.05 | 146.88 | 149.64 | 153.14 | 158.12 | |||||
| Government | 130 | 168.28 | 172.38 | 169.43 | 164.64 | 167.14 | |||||
| Unemployed | 64 | 168.18 | 167.06 | 171.95 | 182.30 | 162.14 | |||||
| Retired | 38 | 173.26 | 187.37 | 182.09 | 172.01 | 184.57 | |||||
| Monthly income | 0.507 | 0.388 | 0.176 | 0.158 | 0.138 | ||||||
| Less than 5000 SAR | 100 | 174.69 | 169.44 | 169.73 | 164.61 | 161.06 | |||||
| 5000 to 7000 SAR | 134 | 160.72 | 156.97 | 154.17 | 155.71 | 157.40 | |||||
| More than 7000 SAR | 96 | 162.61 | 173.31 | 176.91 | 180.09 | 181.43 | |||||
| Perceived social support | 0.571 | 0.722 | 0.713 | 0.702 | 0.388 | ||||||
| No support | 122 | 160.15 | 160.29 | 171.01 | 170.98 | 172.13 | |||||
| Some support | 110 | 173.08 | 170.21 | 163.29 | 163.85 | 167.56 | |||||
| Enough support | 98 | 163.66 | 166.70 | 161.12 | 160.52 | 154.93 | |||||
| Variable | Frequency | Percentage |
|---|---|---|
| No burden | 59 | 17.9 |
| Mild burden | 85 | 25.8 |
| Moderate burden | 115 | 34.8 |
| Severe burden | 71 | 21.5 |
| Variables | Total (n = 330) | No/Mild (n = 144) | Moderate/Severe (n = 186) | Adjusted OR (95% CI) | p-Value |
|---|---|---|---|---|---|
| Patients’ characteristics | |||||
| Age | |||||
| Less than 20 years | 105 | 42 | 63 | Ref | |
| 20 to 40 years | 141 | 68 | 73 | 1.21 (0.54–2.59) | 0.789 |
| More than 40 years | 84 | 34 | 50 | 2.60 (0.38–1.11) | 0.116 |
| Gender | |||||
| Female | 136 | 59 | 77 | Ref | |
| Male | 194 | 85 | 109 | 1.01 (0.65–1.58) | 0.938 |
| Duration since diagnosis | |||||
| Less than 2 years | 101 | 41 | 60 | Ref | |
| 2 to 5 years | 136 | 67 | 69 | 0.92 (0.52–1.64) | 0.924 |
| More than 5 years | 93 | 36 | 57 | 0.65 (0.38–1.11) | 0.650 |
| Caregivers’ characteristics | |||||
| Age | |||||
| Less than 40 years | 110 | 54 | 56 | Ref | |
| 40 to 50 years | 138 | 57 | 81 | 0.70 (0.39–1.25) | 0.224 |
| 51 and above years | 82 | 33 | 49 | 0.96 (0.55–1.67) | 0.877 |
| Gender | |||||
| Female | 179 | 77 | 102 | Ref | |
| Male | 151 | 67 | 84 | 1.06 (0.68–1.65) | 0.805 |
| Education level | |||||
| No formal education | |||||
| Up to high school | 101 | 40 | 61 | Ref | |
| Bachelor’s degree | 101 | 42 | 59 | 1.29 (0.74–2.25) | 0.372 |
| Postgraduate degree | 128 | 62 | 66 | 1.32 (0.78–2.23) | 0.301 |
| Occupation | |||||
| Private | 98 | 50 | 48 | Ref | |
| Government | 130 | 57 | 73 | 0.39 (0.28–0.61) | 0.022 |
| Unemployed | 64 | 26 | 38 | 0.52 (0.23–1.14) | 0.103 |
| Retired | 38 | 11 | 27 | 0.59 (0.25–1.41) | 0.238 |
| Monthly income | |||||
| Less than 5000 SAR | 100 | 39 | 61 | Ref | |
| 5000 to 7000 SAR | 134 | 70 | 64 | 0.89 (0.50–1.60) | 0.714 |
| More than 7000 SAR | 96 | 35 | 61 | 0.53 (0.31–0.70) | 0.018 |
| Social Support | |||||
| No support | 122 | 51 | 71 | Ref | |
| Some support | 110 | 47 | 63 | 1.23 (0.72–2.10) | 0.446 |
| Enough support | 98 | 46 | 52 | 1.19 (0.69–2.05) | 0.542 |
| Relationship with the patients | |||||
| Extended family (Uncles, aunts, etc.) | 30 | 15 | 15 | Ref | |
| Siblings | 54 | 20 | 34 | 1.12 (0.49–2.57) | 0.786 |
| Spouse | 82 | 30 | 52 | 1.91 (0.95–3.82) | 0.068 |
| Adult children caring for parents | 77 | 33 | 44 | 1.95 (1.05–3.60) | 0.034 |
| Parents | 87 | 46 | 41 | 1.49 (0.81–2.77) | 0.201 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Thirunavukkarasu, A.; Zawawi, E.M. A Cross-Sectional Evaluation of Caregiver Burden in Schizophrenia Care: Findings from Western Saudi Arabia with Policy Implications for Preventive Mental Healthcare. Healthcare 2026, 14, 55. https://doi.org/10.3390/healthcare14010055
Thirunavukkarasu A, Zawawi EM. A Cross-Sectional Evaluation of Caregiver Burden in Schizophrenia Care: Findings from Western Saudi Arabia with Policy Implications for Preventive Mental Healthcare. Healthcare. 2026; 14(1):55. https://doi.org/10.3390/healthcare14010055
Chicago/Turabian StyleThirunavukkarasu, Ashokkumar, and Ebtehal Mobarak Zawawi. 2026. "A Cross-Sectional Evaluation of Caregiver Burden in Schizophrenia Care: Findings from Western Saudi Arabia with Policy Implications for Preventive Mental Healthcare" Healthcare 14, no. 1: 55. https://doi.org/10.3390/healthcare14010055
APA StyleThirunavukkarasu, A., & Zawawi, E. M. (2026). A Cross-Sectional Evaluation of Caregiver Burden in Schizophrenia Care: Findings from Western Saudi Arabia with Policy Implications for Preventive Mental Healthcare. Healthcare, 14(1), 55. https://doi.org/10.3390/healthcare14010055





