Abstract
Background/Objectives: HIV-related stigma and fear among healthcare professionals represent significant barriers to effective patient care, contributing to delayed diagnosis and suboptimal treatment for people living with HIV (PLHIV). Although these issues have been studied in various settings, there is a lack of evidence on how they manifest among general practitionersin Colombia—a key group in the healthcare system. This study investigated the prevalence of stigma and fear among Colombian general practitioners and identified associated factors. Methods: A cross-sectional, observational study was conducted between February and May 2024, using a self-administered online survey targeting general practitioners. A validated 28-question instrument adapted from the Health Policy Project assessed fear, stigma, and related factors. Results: Among 579 participants, 68.6% exhibited low fear levels; however, specific clinical tasks, such as taking blood samples, elicited greater concern. Stigmatizing beliefs—such as associating HIV with irresponsible behavior—were reported by 25% of participants. Prior training in HIV care was inversely associated with stigma (OR = 0.681; 95% CI: 0.489–0.949), while older age and heterosexual orientation correlated with higher stigma levels. Conclusions: Despite generally low levels of fear and stigma, gaps in HIV-related training among physicians highlight the need for targeted educational initiatives. Promoting comprehensive HIV education in medical curricula and continuing professional development can reduce stigma, enhance confidence in care, and foster a more inclusive healthcare environment.
1. Introduction
Since the emergence of the human immunodeficiency virus (HIV) epidemic, widespread misconceptions regarding its transmission and the lived experiences of people living with HIV/AIDS (PLWHA) have fueled persistent stigma and discrimination [1,2]. HIV infection poses one of the greatest public health challenges globally due to its high transmissibility, continued growth, impact on morbidity and mortality, and the associated costs to the health system that further exacerbate the problem.
Healthcare professionals, particularly physicians, play a pivotal role in HIV prevention, diagnosis, and treatment. They are central to promoting early detection, educating patients on risk factors, and ensuring access to screening and care services [3]. Prejudices and stereotypes held by health professionals can influence the quality of care provided to PLWHA by discouraging them from seeking medical care. Stigma and discrimination among health workers have been documented in several countries across different regions of the world [4,5,6,7,8]. These attitudes result in underdiagnosis, poor adherence to treatment, and, ultimately, higher morbidity and mortality [9,10].
In addition to these clinical consequences, stigma from healthcare providers also affects the mental health of PLWHA, who experience higher rates of depression, social isolation, and suicidal ideation compared to the general population [11]. For instance, individuals in Serbia have reported that the most profound stigma they face originates from the healthcare sector itself [12]. Stigma within health services thus constitutes a critical barrier to both accessing and delivering effective HIV care [13].
Several studies have identified contributing factors to these stigmatizing attitudes among healthcare providers, including limited training in HIV care, unfounded fears of occupational exposure, moral or religious beliefs, and systemic gaps in education regarding HIV transmission and management [14,15,16,17]. These factors have led healthcare providers to spend less time with PLWH compared to other patients and to avoid physical contact during routine medical examinations [1,2,13,18,19,20]. The identification and recognition of stigma by healthcare workers are crucial strategies in the fight against HIV. Stigmatizing attitudes from key actors, such as healthcare providers, represent significant barriers to the well-being and quality of life of patients [4,5].
Despite the growing body of international literature on this topic, there is a notable lack of recent, empirical data from Colombia. National data indicate ongoing challenges in the HIV care cascade: in 2023, only 43.5% of newly diagnosed HIV cases in Colombia were identified in early stages, and only 68.35% of PLWHA reached an undetectable viral load, placing the country below global UNAIDS targets [21]. Given these gaps, a better understanding of physician-related stigma is essential to improve national HIV responses.
Despite the fundamental role of health workers in HIV management, this topic has not been widely explored in Colombia. This study aims to investigate the stigma and discrimination among general practitioners in Colombia towards HIV infection using a nationwide cross-sectional survey.
2. Materials and Methods
2.1. Study Design and Setting
This cross-sectional, observational study was conducted using a self-administered online survey targeting general practitioners in Colombia between February and May 2024. Colombia, a Latin American country, is bordered by the Pacific Ocean and shares borders with Ecuador, Peru, Brazil, Venezuela, and Panama, regions that have significant cultural influences [22]. According to the Colombian Ministry of Health, approximately 126,279 physicians were practicing in 2022, of whom 94,892 were general practitioners (75.1%) [23].
2.2. Population and Sample
The study population consisted of general practitioners residing in Colombia, defined as individuals holding a university degree in medicine who had not pursued or completed postgraduate specialization studies.
Based on a 2022 estimate of 94,892 general practitioners [23], the sample size was calculated using a 95% confidence level, a 5% margin of error, and a 50% response probability. The minimum required sample was 383 participants, determined using a standard formula for survey populations [24]:
A non-probabilistic convenience sampling method was employed using the “Google Forms” platform. Participation was voluntary, and only responses from those who provided informed consent were included.
The Selection of Participants Was Based on the Following Criteria
Inclusion criteria: (1) being a general practitioner as defined above, (2) residing in Colombia at the time of the survey, and (3) accepting the informed consent before beginning the questionnaire. Exclusion criteria: (1) having completed or currently pursuing postgraduate medical specialization, (2) not residing in Colombia, or (3) declining to provide informed consent.
2.3. Questionnaire Development and Measurement
The study used a 28-question, self-administered online questionnaire adapted from the “Measuring HIV Stigma and Discrimination among People Working in Health Facilities” tool developed by the Health Policy Project [25]. The questionnaire was designed to evaluate fear and stigma related to HIV among general practitioners in Colombia.
The validation of the tool occurred in two stages. First, a public health expert reviewed the questionnaire for accuracy. Subsequently, a pilot test was conducted with 30 general practitioners, who provided feedback on comprehension and wording. Based on this, the final questionnaire in Spanish was structured into seven sections:
- Informed Consent;
- Sociodemographic Data (6 questions);
- Specialized Training on HIV (4 questions);
- Fear of HIV Infection (4 questions);
- Stigma and Discrimination Towards People Living with HIV (PLHIV) (6 questions);
- Stereotypes and Prejudices (7 questions).
2.4. Variables
The questionnaire collected a range of variables, including demographic data (e.g., sex, age, sexual orientation, workplace, and work experience). Additionally, it captured information on specialized training related to PLHIV, which encompassed training on HIV-specific care, infection control, care for key populations, and stigma and discrimination.
Using the framework of the Health Policy Project questionnaire and interpretation indicators proposed by UNAIDS, the instrument was designed as a 28-item, self-administered survey comprising closed-ended questions. Most items used four-point Likert-type scales (e.g., “not worried” to “very worried” or “strongly disagree” to “strongly agree”) to assess levels of fear, stigma, and attitudes toward PLHIV.
Fear of infection was assessed through four items evaluating participants’ emotional responses during specific work-related activities involving PLHIV. These were classified as noninvasive (e.g., touching clothes, taking temperature) or invasive (e.g., drawing blood, dressing wounds), based on infection risk. Participants who indicated worry on at least one invasive item were categorized as having a high level of fear [26].
Stigma and discrimination were assessed using items designed to detect stigmatizing beliefs and behaviors. Participants were classified as showing high stigma if they agreed with at least one stigmatizing statement. Additional items addressed manifestations of stigma, such as the use of unnecessary precautions (e.g., always wearing gloves for history-taking) and stereotypes about the behavior or morality of PLHIV.
Physicians’ attitudes toward key populations—including people who inject drugs, men who have sex with men, and sex workers—were also explored through items measuring willingness to provide care and personal comfort levels.
2.5. Data Collection and Management
Data collection was conducted using the online platform Google Forms, with participants accessing the survey through a unique link disseminated via social media channels, including Instagram and WhatsApp. The survey preamble provided an overview of the study objectives, reinforced the importance of confidentiality, and included a request for informed consent. Participants were required to agree to an electronic Participation Agreement before proceeding, ensuring anonymity throughout the process.
To ensure data integrity, all responses were subjected to a rigorous quality control process. This included verifying eligibility and consistency of responses, and identifying entries with implausible age ranges, indiscriminate selection of response options, duplicate submissions, or those that included only demographic data. Out of the 657 responses initially received, a total of 78 were excluded: 28 did not meet the selection criteria, 16 presented implausible age ranges, 17 showed indiscriminate selection of all options, 6 were identified as duplicates, and 11 included only demographic data. Ultimately, 579 valid responses were retained for inclusion in the final analysis.
2.6. Ethical Statement
This study adhered to the ethical principles established by the Declaration of Helsinki and complied with the protocols approved by the Ethics Committee of the Institute of Medical Diagnostics (IDIME) S.A. No personal, identifiable, high-risk, or sensitive information was collected during the study. All participants provided informed consent, ensuring full compliance with ethical research standards.
2.7. Statistical Analysis
Descriptive statistics were applied to analyze categorical variables, with frequencies and percentages calculated for each response. To explore the association between demographic, professional, and training characteristics and fear of HIV infection or stigma toward PLHIV, a logistic regression model was employed. Results were expressed as odds ratios (ORs) with 95% confidence intervals (CIs). Statistical significance was determined using a two-tailed approach, with a threshold of p < 0.05. All analyses were conducted using IBM SPSS Statistics for Windows, version 26.0 (IBM, Chicago, IL, USA).
3. Results
3.1. Sociodemographic and Professional Characteristics
A total of 579 general practitioners were included in the study. The majority were women (64.1%, n = 371), and 53.2% were aged between 27 and 59 years. Most participants identified as heterosexual (87.0%, n = 504). Regarding professional experience, 50.1% (n = 290) worked in outpatient services, and 45.4% (n = 262) reported having between one and five years of work experience. Only 11.9% (n = 69) had prior experience working in services specialized for people living with HIV (PLHIV), while 27.6% (n = 160) reported knowing someone close to them with an HIV diagnosis (Table 1).

Table 1.
Sociodemographic and professional characteristics of the physicians participating in the study.
3.2. Previous Training for PLHIV
The analysis of previous training related to the care of PLHIV revealed that the highest proportion of training was associated with caring for PLHIV (55.8%), followed by training in infection control and universal precautions (47.8%). However, significant gaps in training were noted, particularly concerning key populations, where 80.5% of participants reported a lack of training. Similarly, 72.5% reported no training on stigma or discrimination toward PLHIV (Figure 1).
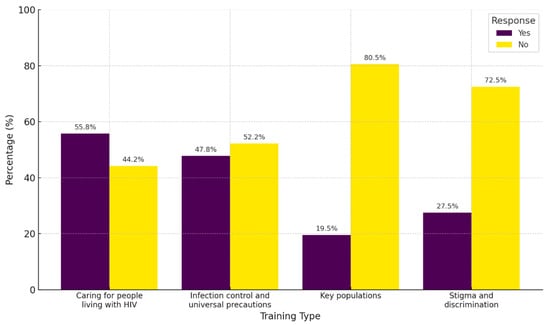
Figure 1.
Health care training for PLHIV and key populations.
3.3. Fear of HIV Infection
Fear of infection was assessed using four questions, with the highest level of fear identified in tasks such as taking blood samples from patients living with HIV (9.2% reported being very worried, 19.5% reported being worried). This was followed by applying bandages to a wound of a PLHIV (4.8% very worried, 9.8% worried). Activities eliciting the least fear included taking the temperature of a PLHIV (98.3% reported no concern) and touching their clothing (95.2% reported no concern) (Figure 2). Overall, the global evaluation showed that most participants exhibited minimal fear (65.6%, n = 397).
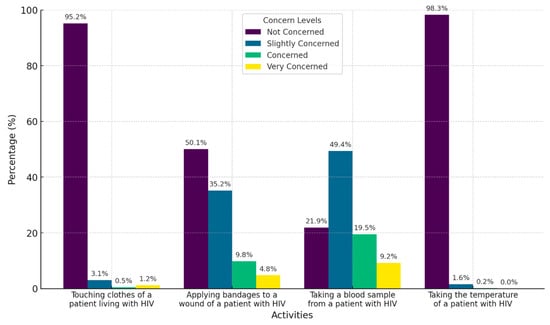
Figure 2.
Characterization of Colombian physicians’ fear of HIV infection.
3.4. Factors Associated with Fear of HIV Infection
Among the sociodemographic factors studied, advanced age (27–59 years) was negatively associated with a high level of fear of infection (OR = 0.701; 95% CI: 0.493–0.998). Additionally, knowing someone close to them with an HIV diagnosis was also negatively associated with high fear (OR = 0.622; 95% CI: 0.411–0.941). Work characteristics further revealed that increased professional experience reduced the likelihood of high fear levels. Physicians with 5–10 years of work experience (OR = 0.517; 95% CI: 0.295–0.906) and those with over 10 years of experience (OR = 0.505; 95% CI: 0.274–0.931) exhibited significantly lower levels of fear (Table 2).

Table 2.
Factors associated with fear of HIV infection among Colombian physicians.
3.5. Stereotypes and Prejudices Toward PLWH
The evaluation of stereotypes and prejudices among physicians revealed that unnecessary precautions were relatively common. The most frequently reported behaviors included implementing special measures during care for PLHIV that were not applied to other patients (28.0%) and consistently using gloves throughout the care process, including during activities like taking a patient’s history or performing a physical examination (23%). In contrast, avoiding physical contact with PLHIV was the least reported behavior, with 97.0% of participants denying this practice (Figure 3).
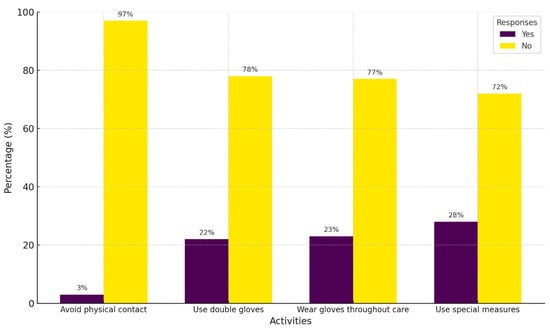
Figure 3.
Characterization of the self-reported use of unnecessary precautions for HIV infection.
Regarding physicians’ willingness and comfort in providing care to key populations, very little rejection was observed. Fewer than 2% of participants expressed strong agreement with preferring not to provide services to key populations. However, slightly higher reluctance was observed in relation to people who inject illicit drugs, with 7% of participants agreeing that they would prefer not to provide care to this group (Figure 4).
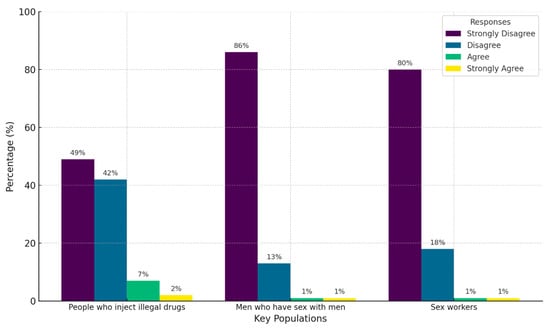
Figure 4.
Characterization of physicians’ willingness and comfort in providing care to key populations.
3.6. Stigma Among Physicians Toward PLWH
The evaluation of stigma and prejudice revealed that most participants disagreed with stigmatizing statements. Specifically, 90% of respondents disagreed with the notion that PLWH should feel ashamed of themselves, and 82% rejected the idea that HIV is a punishment for bad behavior. However, 25% of participants agreed with the statement that people who contract HIV do so because they engage in irresponsible behavior. Additionally, 51% of respondents fully agreed that women living with HIV should be allowed to have children if they wish (Figure 5). In addition, the global assessment of stigma levels indicated that the majority of participating physicians (56.8%, n = 329) exhibited a low level of stigma toward PLWH, while 43.2% (n = 250) were classified as having a high level of stigma.
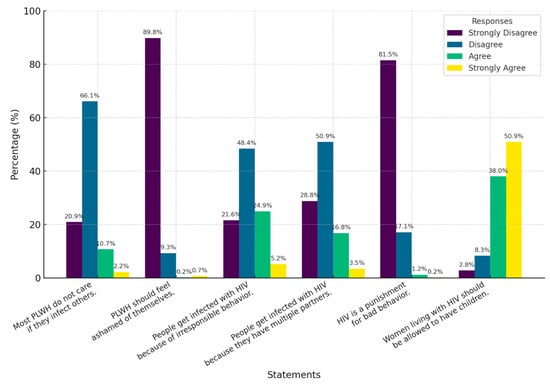
Figure 5.
Characterization of the stigma of physicians towards PLWH.
3.7. Factors Associated with Stigma Toward PLWH
Analysis of demographic variables showed that physicians aged between 27 and 59 years were significantly more likely to exhibit high levels of stigma toward PLWH (OR = 1.66; 95% CI: 1.206–2.356). Similarly, heterosexual participants were more likely to report high stigma levels (OR = 1.853; 95% CI: 1.100–3.120). In terms of professional characteristics, greater work experience was associated with higher stigma levels, particularly among physicians with 10 or more years of professional practice (OR = 2.145; 95% CI: 1.220–3.770). In contrast, previous training in caring for PLWH was the only factor associated with lower stigma levels, showing a negative association (OR = 0.681; 95% CI: 0.489–0.949) (Table 3).

Table 3.
Factors associated with stigma towards PLWH among physicians.
4. Discussion
This study explored fear and stigma related to HIV infection among Colombian physicians, particularly in the context of their interactions with PLHIV. Several studies have employed the same standardized tool developed by the Health Policy Project to assess stigma among healthcare personnel in diverse contexts—including China, Thailand, and multi-country field trials across Africa, Asia, and the Caribbean—supporting the instrument’s cross-cultural applicability and reinforcing the comparability of our findings [27,28].
The sample was predominantly composed of female physicians, mirroring national trends of increasing female representation in medicine and medical training programs in Colombia and the broader Latin American region [29,30,31,32]. Most participants were young physicians aged 20 to 26 years, with limited professional experience of one to five years, likely influenced by the study’s reliance on self-reported electronic questionnaires, which are more accessible to younger populations. Additionally, 87% of participants identified as heterosexual, a pattern consistent with other studies among healthcare professionals [33,34].
A striking finding was the lack of specific training among more than 70% of physicians regarding the care of PLHIV and key populations. This is consistent with previous studies, such as Aziz M. et al., where 62% of surveyed physicians reported insufficient training on stigma-related issues, and Koseoglu Ornek et al., who found that 86% lacked specific education on HIV [2,20]. These results underscore an urgent need for academic and public health institutions in Colombia to prioritize HIV-focused training in medical curricula.
Regarding fear of HIV infection, 68.6% of participants reported low levels of fear, a smaller proportion compared to studies conducted in countries such as Indonesia and Yemen [35,36]. However, certain activities, such as applying bandages or taking blood samples from PLHIV, elicited higher levels of concern. These findings highlight the need to reinforce training on universal precaution practices, not only to protect healthcare workers but also to mitigate irrational fears. Moreover, the negative association between knowing someone diagnosed with HIV and fear supports the role of personal interactions in demystifying the disease and fostering positive attitudes, as observed in studies conducted in sub-Saharan Africa [19]. In addition, older age (27 to 59 years) and greater professional experience (five years or more) were also associated with reduced fear of HIV infection. This suggests that accumulated experience contributes to greater confidence in prevention measures and a more accurate understanding of HIV transmission routes. Similar findings in Egypt showed higher prejudice and fear among less experienced physicians [2]. The findings also revealed that some physicians adopted excessive protective measures, such as consistent glove use during non-invasive tasks. These practices reflect persistent misconceptions about HIV transmission, as standard universal precautions—such as hand hygiene, the use of gloves when in contact with blood or body fluids, and the safe handling of sharps—are sufficient for safely providing care to PLHIV [37]. Reinforcing these evidence-based hygiene practices may help reduce fear-driven and stigma-reinforcing behaviors within healthcare settings.
While the majority of physicians demonstrated low levels of stigma, approximately 20% agreed with stigmatizing beliefs, such as the idea that HIV is a consequence of irresponsible behavior or having multiple sexual partners. These beliefs oversimplify the multifaceted social, structural, and biological factors contributing to HIV transmission and risk perpetuating stigmas that can negatively impact patient care. Factors such as older age (27 to 59 years) and heterosexual orientation were associated with higher levels of stigma, consistent with studies showing that heterosexual individuals often display higher stigma rates [38,39]. These results may reflect cultural and generational norms, including the association of HIV with morally questionable behaviors, exacerbated by limited training on sexual diversity and insufficient knowledge of the structural drivers of HIV transmission. Addressing these cultural biases and promoting evidence-based education are critical to reducing stigma in these groups.
Training emerged as the only factor negatively associated with stigma toward PLHIV, reinforcing the pivotal role of education in reducing both fear and stigma, even among specialized groups like physicians. This finding aligns with systematic reviews by Okpua NC et al. and studies by Shahar E et al., which emphasize the effectiveness of educational programs in managing HIV-related stigma [6,40]. The high proportion of Colombian physicians untrained in caring for PLHIV and key populations [7] highlights modifiable factors that can be addressed through targeted interventions. Promoting ongoing training can create a stigma-free healthcare environment, with physicians playing a leading role in dismantling barriers to equitable care [8]. Beyond raising awareness, continuing education can challenge underlying attitudes that perpetuate stigma and discrimination, paving the way for a more inclusive and professional healthcare system [41,42].
Limitations
This study provides valuable insights into fear and stigma toward HIV among Colombian general practitioners, yet several limitations should be considered when interpreting the findings. One notable limitation is the use of non-probability convenience sampling and online data collection, which may introduce selection and response biases, potentially excluding participants with limited access to electronic devices or the internet. To mitigate these challenges, a recruitment strategy was implemented, leveraging multiple dissemination channels, including medical associations, to reach a broader and more diverse sample.
Although the questionnaire was adapted from a validated standardized tool developed by the Health Policy Project, it was not revalidated psychometrically within the Colombian context. While a pilot test was conducted to ensure comprehension and cultural relevance, the absence of a formal validation process in this population constitutes a methodological limitation.
Additionally, the use of a closed-ended questionnaire limits the ability to capture nuanced attitudes or explanations behind certain responses, potentially constraining the depth of insight into physicians’ beliefs and behaviors.
Reliance on self-reported responses also poses a risk of recall bias or social desirability bias. To address this, the survey emphasized confidentiality and anonymity, employed neutral language, and highlighted the importance of honest responses to participants. These measures were designed to minimize biases and enhance the reliability and validity of the collected data.
5. Conclusions
This study found that most participants exhibited low levels of fear and stigma toward PLHIV. However, a substantial proportion of physicians lacked specialized training in caring for PLHIV and key populations, emphasizing the urgent need for targeted educational initiatives in medical curricula and continuing professional development.
Academic training emerged as the strongest factor associated with reduced stigma, underscoring its transformative role in shaping positive attitudes and fostering a more inclusive healthcare environment. These findings highlight the critical importance of integrating comprehensive HIV education into medical training programs to address stigma effectively.
Additionally, demographic and professional factors such as age, work experience, and personal familiarity with someone diagnosed with HIV were linked to lower levels of fear. This suggests that exposure and practical experience significantly contribute to reducing unfounded concerns and promoting confidence in managing HIV-related care. Conversely, stigmatizing beliefs were more prevalent among heterosexual and older physicians, reflecting underlying cultural and generational biases that require targeted intervention.
Author Contributions
Conceptualization, V.L.-G. and J.S.I.-C.; methodology, J.S.I.-C.; software, V.L.-G., J.P.M.R., J.S.C., W.D.G. and E.D.C.; validation, J.S.I.-C.; formal analysis, J.S.I.-C.; investigation, V.L.-G., J.P.M.R., J.S.C., W.D.G. and E.D.C.; resources, V.L.-G., J.P.M.R., J.S.C. and W.D.G.; data curation, J.S.I.-C.; writing—original draft preparation, V.L.-G., J.P.M.R., J.S.C., W.D.G. and E.D.C.; writing—review and editing, J.S.I.-C.; visualization, J.S.I.-C.; supervision, J.S.I.-C.; project administration, V.L.-G. and J.S.I.-C.; funding acquisition, J.S.I.-C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Committee of the Institute of Medical Diagnostics (IDIME) S.A. (approval code ID-GGLEG-GU-01-F01 on 6 December 2023). Additionally, this work is derived from a thesis project for the Master’s Program in Permanent Training on HIV Infection XIII at the Universidad Rey Juan Carlos and the Ministry of Health, Madrid.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| HIV | Human immunodeficiency virus |
| PLWHA | People living with HIV/AIDS |
| PLHIV | People living with HIV |
| CI | Confidence interval |
| OR | Odds ratio |
| UNAIDS | Joint United Nations Programme on HIV/AIDS |
References
- Smith, M.K.; Xu, R.H.; Hunt, S.L.; Wei, C.; Tucker, J.D.; Tang, W.; Luo, D.; Xue, H.; Wang, C.; Yang, L.; et al. Combating HIV Stigma in Low- and Middle-Income Healthcare Settings: A Scoping Review. J. Int. AIDS Soc. 2020, 23, e25553. [Google Scholar] [CrossRef] [PubMed]
- Aziz, M.M.; Abdelrheem, S.S.; Mohammed, H.M. Stigma and Discrimination Against People Living with HIV by Health Care Providers in Egypt. BMC Health Serv. Res. 2023, 23, 663. [Google Scholar] [CrossRef] [PubMed]
- Mendez, A.D.; Neelamegam, M.; Griner, S.B. Health Care Provider Discussions Regarding HIV/Sexually Transmitted Infection Risk Factors and Associations with HIV/Sexually Transmitted Infection Screening Among Men. Arch. Sex. Behav. 2023, 52, 2111–2121. [Google Scholar] [CrossRef] [PubMed]
- Mohammadifirouzeh, M.; Oh, K.M.; Tanner, S. HIV Stigma Reduction Interventions Among Health Care Providers and Students in Different Countries: A Systematic Review. Curr. HIV Res. 2022, 20, 20–31. [Google Scholar] [CrossRef]
- Baldwin, A.; Sileo, K.M.; Huynh, T.A.; Olfers, A.; Woo, C.J.; Greene, S.L.; Casillas, G.L.; Taylor, B.S. Applying the Health Stigma and Discrimination Framework to Assess HIV Stigma among Health Care Professionals: A Mixed Methods, Community-Based Participatory Research Study. J. Health Care Poor Underserved 2022, 33, 950–972. [Google Scholar] [CrossRef]
- Okpua, N.C.; Godwin, C.A. Healthcare Providers in Nigerian Hospitals and HIV-Related Stigma: A Systematic Review. J. Commun. Healthc. 2023, 16, 170–179. [Google Scholar] [CrossRef]
- Spence, A.B.; Wang, C.; Michel, K.; Ocampo, J.M.; Kharfen, M.; Merenstein, D.; Goparaju, L.; Kassaye, S. HIV Related Stigma among Healthcare Providers: Opportunities for Education and Training. J. Int. Assoc. Provid. AIDS Care 2022, 21, 23259582221114797. [Google Scholar] [CrossRef]
- Nyblade, L.; Mbuya-Brown, R.J.; Ezekiel, M.J.; Addo, N.A.; Sabasaba, A.N.; Atuahene, K.; Kiwia, P.; Gyamera, E.; Akyoo, W.O.; Vormawor, R.; et al. A Total Facility Approach to Reducing HIV Stigma in Health Facilities: Implementation Process and Lessons Learned. AIDS 2020, 34 (Suppl. S1), S93–S102. [Google Scholar] [CrossRef]
- Vetrova, M.V.; Cheng, D.M.; Bendiks, S.; Gnatienko, N.; Lloyd-Travaglini, C.; Jiang, W.; Luoma, J.; Blokhina, E.; Krupitsky, E.; Lioznov, D.; et al. HIV and Substance Use Stigma, Intersectional Stigma and Healthcare Among HIV-Positive PWID in Russia. AIDS Behav. 2021, 25, 2815–2826. [Google Scholar] [CrossRef]
- Khumalo, G.E.; Lutge, E.E.; Naidoo, P.; Mashamba-Thompson, T.P. Barriers and Facilitators of Rendering HIV Services by Community Health Workers in Sub-Saharan Africa: A Meta-Synthesis. Fam. Med. Community Health 2021, 9, e000958. [Google Scholar] [CrossRef]
- Knippler, E.T.; Martinez, A.J.; Amiri, I.; Madundo, K.; Mmbaga, B.T.; Goldston, D.B.; Relf, M.V.; Knettel, B.A. Challenges and Opportunities for Improving Mental Health Care and Preventing Suicide Among People Living with HIV: Perspectives of Mental Health Professionals in Tanzania. PLoS Glob. Public. Health 2024, 4, e0002762. [Google Scholar] [CrossRef] [PubMed]
- Cousins, S. HIV in Serbia: Stigma and a stagnant HIV response. Lancet HIV 2018, 5, e343–e344. [Google Scholar] [CrossRef]
- Rivera-Díaz, M.; Varas-Díaz, N.; Reyes-Estrada, M.; Coriano, D.; Ortiz, N.; Padilla, M. Mobile technology as a potential tool in research on stigma associated with HIV/AIDS among medical students. Rev. Puertorriquena Psicol. 2019, 30, 60–68. [Google Scholar] [PubMed]
- Yin, Y.; Chen, A.C.-C.; Wan, S.; Chen, H. Factors Associated With HIV-Related Stigma Toward People Living With HIV Among Nurses in Liangshan Yi Autonomous Prefecture, China: A Cross-Sectional Study. Front. Psychiatry 2021, 12, 714597. [Google Scholar] [CrossRef]
- Geter, A.; Herron, A.R.; Sutton, M.Y. HIV-Related Stigma by Healthcare Providers in the United States: A Systematic Review. AIDS Patient Care STDS 2018, 32, 418–424. [Google Scholar] [CrossRef]
- Shrestha, P.W.; Visudtibhan, P.J.; Kiertiburanakul, S. Factors Associated With HIV-Related Stigma Among Healthcare Providers at a University Hospital in Nepal. J. Int. Assoc. Provid. AIDS Care 2024, 23, 23259582241282583. [Google Scholar] [CrossRef]
- Fauk, N.K.; Ward, P.R.; Hawke, K.; Mwanri, L. HIV Stigma and Discrimination: Perspectives and Personal Experiences of Healthcare Providers in Yogyakarta and Belu, Indonesia. Front. Med. 2021, 8, 625787. [Google Scholar] [CrossRef]
- Shah, S.; Elgalib, A.; Al-Wahaibi, A.; Al-Fori, M.; Raju, P.; Al-Skaiti, M.; Al-Mashani, H.N.; Duthade, K.; Omaar, I.; Muqeetullah, M.; et al. Knowledge, Attitudes and Practices Related to HIV Stigma and Discrimination Among Healthcare Workers in Oman. Sultan Qaboos Univ. Med. J. 2020, 20, e29–e36. [Google Scholar] [CrossRef]
- Du, H.; Chi, P.; Li, X. High HIV Prevalence Predicts Less HIV Stigma: A Cross-National Investigation. AIDS Care 2018, 30, 714–721. [Google Scholar] [CrossRef]
- Koseoglu Ornek, O.; Tabak, F.; Mete, B. Stigma in Hospital: An Examination of Beliefs and Attitudes Towards HIV/AIDS Patients, Istanbul. AIDS Care 2020, 32, 1045–1051. [Google Scholar] [CrossRef]
- Jiménez Forero, L.A. Casos de VIH: Una Tendencia en Aumento en el Marco del Aseguramiento en Colombia 2023. Available online: https://cuentadealtocosto.org/vih/dia-mundial-de-respuesta-al-vih-2023/ (accessed on 17 January 2025).
- Cano Blandón, R. Las fronteras en Colombia: Su origen, evolución, pérdida e importancia en las Relaciones Internacionales. Rev. Ciudad. Estados Y Política 2022, 9, 4. [Google Scholar] [CrossRef]
- Ministerio de Salud y Protección Social ¿Se Necesitan más Médicos Especialistas en Colombia? Available online: https://www.periodicoelpulso.com.co/301-octubre-2023/generales-2.php (accessed on 17 January 2025).
- Daniel, W.W.; Cross, C.L. Biostatistics: A Foundation for Analysis in the Health Sciences, 10th ed.; John Wiley & Sons: New York, NY, USA, 2013; Volume 1, ISBN 978-1-119-28237-2. [Google Scholar]
- Health Policy Project Midiendo Estigma Y Discriminación Hacia el VIH Entre Personas que Trabajan en Facilidades de Salud 2015. Available online: https://www.healthpolicyproject.com/pubs/49_SpanishStandardizedBriefQuestionnairersion.pdf (accessed on 17 January 2025).
- Joint United Nations Programme on HIV/AIDS the Indicators for Global AIDS Monitoring (GAM). Available online: https://indicatorregistry.unaids.org/ (accessed on 17 January 2025).
- Yuan, L.; Peng, X.; Wu, D.; Chen, S.; Tang, W.; Wang, H.; Zhou, J. Stigma Toward People Living with HIV Among Healthcare Providers in Midwifery Hospitals in Shenzhen, China from 2020 to 2023. Sci. Rep. 2025, 15, 6677. [Google Scholar] [CrossRef] [PubMed]
- Nyblade, L.; Jain, A.; Benkirane, M.; Li, L.; Lohiniva, A.-L.; McLean, R.; Turan, J.M.; Varas-Díaz, N.; Cintrón-Bou, F.; Guan, J.; et al. A Brief, Standardized Tool for Measuring HIV-Related Stigma Among Health Facility Staff: Results of Field Testing in China, Dominica, Egypt, Kenya, Puerto Rico and St. Christopher & Nevis. J. Int. AIDS Soc. 2013, 16, 18718. [Google Scholar] [CrossRef]
- Loaiza-Guevara, V.; Acosta, M.A.G.; Álvarez, A.V.A.; Martínez, V.A.; Montoya, M.C.M.; Ramírez, A.A.; Izquierdo-Condoy, J.S. Exploring Psychosocial Factors Influencing Sexually Transmitted Infection Intention Testing Among Medical Students: A Cross-Sectional Study in Two Universities. Front. Public. Health 2024, 12, 1407070. [Google Scholar] [CrossRef]
- Izquierdo-Condoy, J.S.; Simbaña-Rivera, K.; Nati-Castillo, H.A.; Cassa Macedo, A.; Cardozo Espínola, C.D.; Vidal Barazorda, G.M.; Palazuelos-Guzmán, I.; Trejo García, B.; Carrington, S.J.; Ortiz-Prado, E. How Much Do Latin American Medical Students Know About Radiology? Latin-American Multicenter Cross-Sectional Study. Med. Educ. Online 2023, 28, 2173044. [Google Scholar] [CrossRef]
- Izquierdo-Condoy, J.S.; Paz, C.; Nati-Castillo, H.A.; Gollini-Mihalopoulos, R.; Aveiro-Róbalo, T.R.; Paucar, J.R.V.; Mamami, S.E.L.; Caicedo, J.F.; Loaiza-Guevara, V.; Mejía, D.C.; et al. Impact of Mobile Phone Usage on Sleep Quality Among Medical Students Across Latin America: Multicenter Cross-Sectional Study. J. Med. Internet Res. 2025, 27, e60630. [Google Scholar] [CrossRef]
- Izquierdo-Condoy, J.S.; Arias-Intriago, M.; Nati-Castillo, H.A.; Gollini-Mihalopoulos, R.; Cardozo-Espínola, C.D.; Loaiza-Guevara, V.; Dalel-Gómez, W.; Villamil, J.; Suárez-Sangucho, I.A.; Morales-Lapo, E.; et al. Exploring Smartphone Use and Its Applicability in Academic Training of Medical Students in Latin America: A Multicenter Cross-Sectional Study. BMC Med. Educ. 2024, 24, 1401. [Google Scholar] [CrossRef]
- Petroll, A.E.; Mosack, K.E. Physician Awareness of Sexual Orientation and Preventive Health Recommendations to Men Who Have Sex With Men. Sex. Transm. Dis. 2011, 38, 63–67. [Google Scholar] [CrossRef]
- Dagostini, C.M.; Bicca, Y.D.A.; Ramos, M.B.; Busnello, S.; Gionedis, M.C.; Contini, N.; Falavigna, A. Patients’ Preferences Regarding Physicians’ Gender: A Clinical Center Cross-Sectional Study. Sao Paulo Med. J. 2022, 140, 134–143. [Google Scholar] [CrossRef]
- Langi, G.G.; Rahadi, A.; Praptoraharjo, I.; Ahmad, R.A. HIV-Related Stigma and Discrimination Among Health Care Workers During Early Program Decentralization in Rural District Gunungkidul, Indonesia: A Cross-Sectional Study. BMC Health Serv. Res. 2022, 22, 356. [Google Scholar] [CrossRef]
- Attal, B.A.; Al-Rowaishan, K.M.; Akeel, A.A.; AlAmmar, F.K. HIV Stigma in the Teaching Hospitals in Sana’a, Yemen: A Conflict and Low-Resource Setting. BMC Public. Health 2021, 21, 1793. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention Infection Control Standard Precautions for All Patient Care. Available online: https://www.cdc.gov/infection-control/hcp/basics/standard-precautions.html (accessed on 5 April 2025).
- Gázquez-López, M.; Álvarez-Serrano, M.A.; Martín-Salvador, A.; Pérez-Morente, M.Á.; García-García, I.; González-García, A.; Martínez-García, E. Attitudes Towards People Living with HIV/AIDS Through the EAPVVS-E: A Descriptive Analysis in Nursing Students. Nurse Educ. Today 2025, 144, 106418. [Google Scholar] [CrossRef] [PubMed]
- Gruszczyńska, E.; Rzeszutek, M. HIV/AIDS Stigma Accumulation Among People Living with HIV: A Role of General and Relative Minority Status. Sci. Rep. 2023, 13, 10709. [Google Scholar] [CrossRef] [PubMed]
- Shahar, E.; Maor, C.; Moshe-Eilon, Y. Medical Personnel Knowledge and Stigmatic Attitude Toward HIV Patients in a High-Income Country. AIDS Care 2020, 32, 1023–1029. [Google Scholar] [CrossRef]
- Anderson, J.; Fenton, K. HIV Related Stigma: A Dangerous Roadblock. BMJ 2022, 379, o2989. [Google Scholar] [CrossRef]
- Rana, B.K.; Sarfraz, M.; Reza, T.E.; Emmanuel, F. A Cross-Sectional Study to Assess HIV/AIDS-Related Stigma and Its Drivers Among Dental Healthcare Providers in Islamabad, Pakistan. Cureus 2023, 15, e46769. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).