Evaluating the Wasfaty E-Prescribing Platform Against Best Practices for Computerized Provider Order Entry
Abstract
1. Introduction
2. Methods
2.1. Study Design and Data Collection
2.2. An Overview of E-Prescribing Systems in Different Countries
2.3. E-Prescribing Functional Characteristics Used to Assess the Wasfaty Program Compliance
- Patient identification and data access—ensuring that relevant demographic information is readily available.
- Current medications and medication history—enabling prescribers to access a comprehensive list of a patient’s current and past medications.
- Medication selection—assisting in the selection of appropriate medications based on entered diagnoses and the patient’s medical background.
- Alerts and communications—providing alerts that inform prescribers about potential contraindications and guiding them towards optimal medication choices based on individual patient data.
- Patient education—supplying necessary information to patients on the proper administration of prescribed medications.
- Data transmission and storage—allowing prescribers to directly transmit prescriptions to the patient’s preferred pharmacy.
- Monitoring and renewals—ensuring that the system notifies prescribers if a prescription or its refill has not been dispensed.
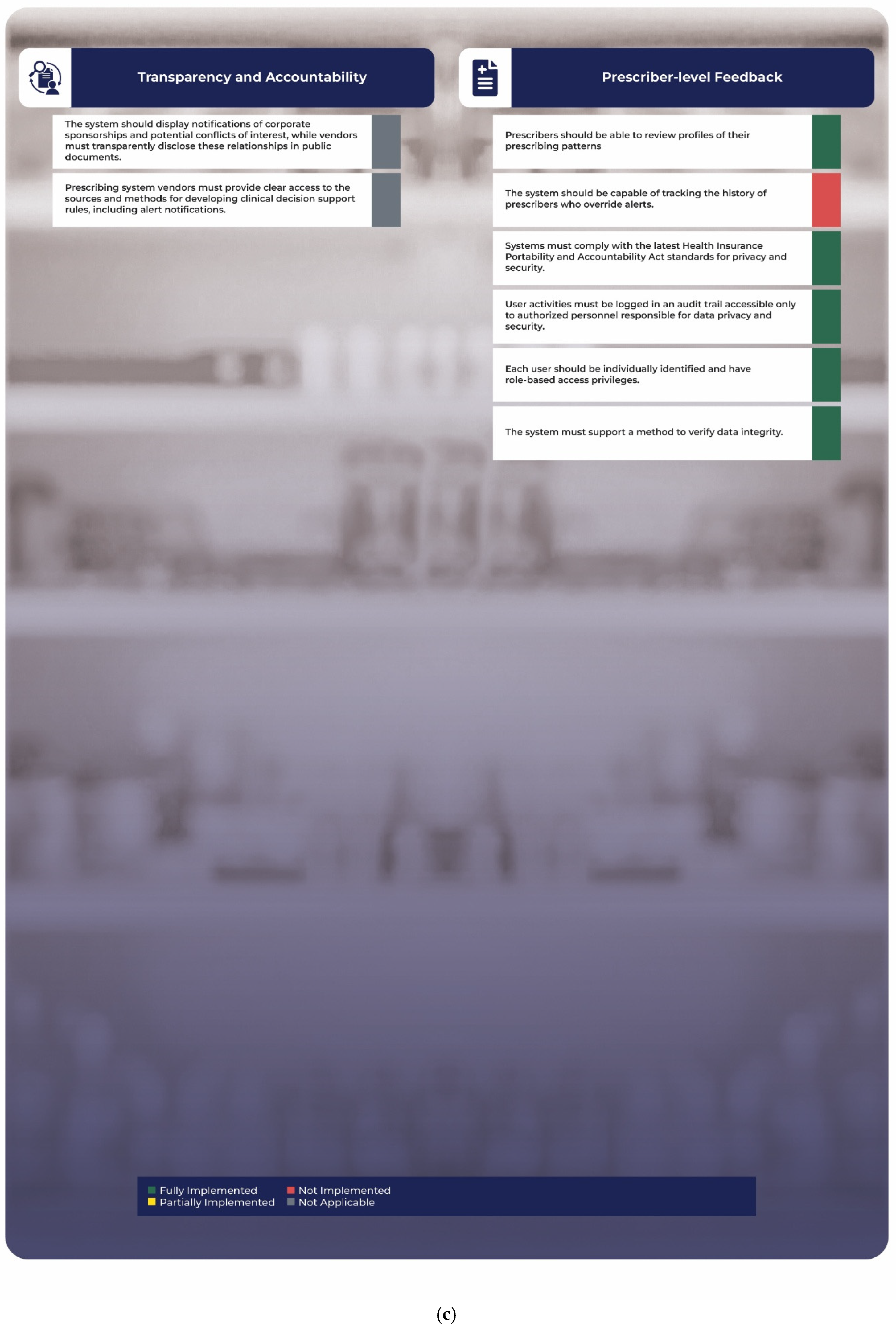
- Transparency and accountability—disclosing clear and transparent procedures regarding how clinical decision support rules are formulated.
- Prescriber-level feedback—providing prescribers with insights to review their own prescribing patterns.
- Security and confidentiality—supporting adherence to regulations designed to protect patient privacy and maintain the confidentiality of health information.
2.4. Statistical Analysis
3. Results
3.1. Patient Identification and Data Access
3.2. Current Medications/Medication History
3.3. Medication Selection
3.4. Alerts and Other Messages to Prescribers
3.5. Patient Education
3.6. Data Transmission and Storage
3.7. Monitoring and Renewals
3.8. Transparency and Accountability
3.9. Prescriber-Level Feedback
4. Discussion
Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ruutiainen, H.; Holmström, A.R.; Kunnola, E.; Kuitunen, S. Use of Computerized Physician Order Entry with Clinical Decision Support to Prevent Dose Errors in Pediatric Medication Orders: A Systematic Review. Paediatr. Drugs 2024, 26, 127–143. [Google Scholar] [CrossRef]
- Uslu, A.; Stausberg, J. Value of the Electronic Medical Record for Hospital Care: Update From the Literature. J. Med. Internet Res. 2021, 23, e26323. [Google Scholar] [CrossRef] [PubMed]
- Kebodeaux, C.D. Prescription and over-the-counter medication record integration: A holistic patient-centered approach. J. Am. Pharm. Assoc. 2019, 59, S13–S17. [Google Scholar] [CrossRef] [PubMed]
- Vejdani, M.; Varmaghani, M.; Meraji, M.; Jamali, J.; Hooshmand, E.; Vafaee-Najar, A. Electronic prescription system requirements: A scoping review. BMC Med. Inform. Decis. Mak. 2022, 22, 231. [Google Scholar] [CrossRef]
- Jõgi, R.; Timonen, J.; Saastamoinen, L.; Laius, O.; Volmer, D. Implementation of European Cross-border Electronic Prescription and Electronic Dispensing Service: Cross-sectional Survey. J. Med. Internet Res. 2023, 25, e42453. [Google Scholar] [CrossRef] [PubMed]
- Esmaeil Zadeh, P.; Tremblay, M.C. A review of the literature and proposed classification on e-prescribing: Functions, assimilation stages, benefits, concerns, and risks. Res. Social. Adm. Pharm. 2016, 12, 1–19. [Google Scholar] [CrossRef]
- Forrester, S.H.; Hepp, Z.; Roth, J.A.; Wirtz, H.S.; Devine, E.B. Cost-effectiveness of a computerized provider order entry system in improving medication safety ambulatory care. Value Health 2014, 17, 340–349. [Google Scholar] [CrossRef]
- Vermeulen, K.M.; van Doormaal, J.E.; Zaal, R.J.; Mol, P.G.; Lenderink, A.W.; Haaijer-Ruskamp, F.M.; Kosterink, J.G.; van den Bemt, P.M. Cost-effectiveness of an electronic medication ordering system (CPOE/CDSS) in hospitalized patients. Int. J. Med. Inform. 2014, 83, 572–580. [Google Scholar] [CrossRef]
- Osmani, F.; Arab-Zozani, M.; Shahali, Z.; Lotfi, F. Evaluation of the effectiveness of electronic prescription in reducing medical and medical errors (systematic review study). In Annales Pharmaceutiques Françaises; Elsevier: Amsterdam, The Netherlands, 2023; pp. 433–445. [Google Scholar]
- Kauppinen, H.; Ahonen, R.; Timonen, J. The impact of electronic prescriptions on medication safety in Finnish community pharmacies: A survey of pharmacists. Int. J. Med. Inform. 2017, 100, 56–62. [Google Scholar] [CrossRef]
- Bilgener, E.; Bulut, S. Evaluation of electronic prescriptions in Turkey: A community pharmacy perspective. Health Policy Technol. 2021, 10, 52–59. [Google Scholar] [CrossRef]
- Aldughayfiq, B.; Sampalli, S. Digital health in physicians’ and pharmacists’ office: A comparative study of e-prescription systems’ architecture and digital security in eight countries. Omics 2021, 25, 102–122. [Google Scholar] [CrossRef] [PubMed]
- Alayed, T.M.; Alrumeh, A.S.; Alkanhal, I.A.; Alhuthil, R.T. Impact of Privatization on Healthcare System: A Systematic Review. Saudi J. Med. Med. Sci. 2024, 12, 125–133. [Google Scholar] [CrossRef]
- Goodair, B.; Reeves, A. The effect of health-care privatisation on the quality of care. Lancet Public Health 2024, 9, e199–e206. [Google Scholar] [CrossRef] [PubMed]
- Alsubahi, N.; Pavlova, M.; Alzahrani, A.A.; Ahmad, A.; Groot, W. Healthcare Quality from the Perspective of Patients in Gulf Cooperation Council Countries: A Systematic Literature Review. Healthcare 2024, 12, 315. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, S.; Mok, D.; Leenen, L. Transformation of health care and the new model of care in Saudi Arabia: Kingdom’s Vision 2030. J. Med. Life 2021, 14, 347–354. [Google Scholar] [CrossRef]
- Alshammari, T.M.; Alsubait, S.I.; Alenzi, K.A.; Almalki, Z.S. Estimating the potential economic impact of the Wasfaty program on costs of antidiabetic treatment: An initiative for the digital transformation of health. Saudi Pharm. J. 2023, 31, 1029–1035. [Google Scholar] [CrossRef]
- Alsahali, S.; Almutairi, G.; Aedh, R.; Alanezi, S.; Almutairi, H.; Anaam, M.; Alshammari, M.; Alhabib, A.; Alowayed, A.; Abdulsalim, S. Perceptions of Community Pharmacists toward the National E-Prescribing Service (Wasfaty) and Exploring the Benefits and Challenges of the Service: A Descriptive Study from Qassim Region, Saudi Arabia. Pharmacy 2023, 11, 152. [Google Scholar] [CrossRef]
- Almaghaslah, D.; Alsayari, A.; Almaghaslah, S.; Alsanna, H. Patients’ Satisfaction with E-Prescribing (Wasfaty) in Saudi Arabia: A Survey of Country-Level Implementation. Healthcare 2022, 10, 806. [Google Scholar] [CrossRef]
- Wang, C.J.; Marken, R.S.; Meili, R.C.; Straus, J.B.; Landman, A.B.; Bell, D.S. Functional Characteristics of Commercial Ambulatory Electronic Prescribing Systems: A Field Study. J. Am. Med. Inform. Assoc. 2005, 12, 346–356. [Google Scholar] [CrossRef]
- Lapane, K.L.; Rosen, R.K.; Dubé, C. Perceptions of e-prescribing efficiencies and inefficiencies in ambulatory care. Int. J. Med. Inform. 2011, 80, 39–46. [Google Scholar] [CrossRef]
- Hibberd, R.; Cornford, T.; Lichtner, V.; Venters, W.; Barber, N. England’s Electronic Prescription Service: Infrastructure in an Institutional Setting. In Information Infrastructures within European Health Care: Working with the Installed Base; Springer: Cham, Switzerland, 2017; pp. 109–128. [Google Scholar]
- Bell, D.S.; Marken, R.S.; Meili, R.C.; Wang, C.J.; Rosen, M.; Brook, R.H.; Panel, R.E.P.E.A. Recommendations For Comparing Electronic Prescribing Systems: Results Of An Expert Consensus Process: Guidance to help early adopters and policymakers select the systems most likely to benefit patients. Health Aff. 2004, 23, W4-305–W304-317. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Anatomical Therapeutic Chemical (ATC) Classification; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Odukoya, O.K.; Chui, M.A. E-prescribing: A focused review and new approach to addressing safety in pharmacies and primary care. Res. Social. Adm. Pharm. 2013, 9, 996–1003. [Google Scholar] [CrossRef]
- Scott, I.A.; Pillans, P.I.; Barras, M.; Morris, C. Using EMR-enabled computerized decision support systems to reduce prescribing of potentially inappropriate medications: A narrative review. Ther. Adv. Drug Saf. 2018, 9, 559–573. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.; Kim, C.K.; Kang, J.; Park, J.M.; Park, T.H.; Lee, K.B.; Lee, S.J.; Cho, Y.J.; Ko, J.; Seo, J.; et al. A Novel Computerized Clinical Decision Support System for Treating Thrombolysis in Patients with Acute Ischemic Stroke. J. Stroke 2015, 17, 199–209. [Google Scholar] [CrossRef]
- Sun, M.-C.; Chan, J.-A. A clinical decision support tool to screen health records for contraindications to stroke thrombolysis–a pilot study. BMC Med. Inform. Decis. Mak. 2015, 15, 105. [Google Scholar] [CrossRef][Green Version]
- Loh, S.; Wijaya, K.; Rogers, M.; Asghari-Jafarabadi, M.; Wojnar, R. A clinical decision support tool for improving venous thromboembolism risk assessment and thromboprophylaxis prescribing compliance within an electronic medication management system: A retrospective observational study. Int. J. Clin. Pharm. 2025, 1–9. [Google Scholar] [CrossRef]
- Horsky, J.; Drucker, E.A.; Ramelson, H.Z. Accuracy and Completeness of Clinical Coding Using ICD-10 for Ambulatory Visits. AMIA Annu. Symp. Proc. 2017, 2017, 912–920. [Google Scholar] [PubMed]
- Almanaa, M. Impact of Computerized Physician Order Entry (CPOE) Coupled With Clinical Decision Support (CDS) on Radiologic Services. Cureus 2024, 16, e69470. [Google Scholar] [CrossRef]
- Li, L.; Foer, D.; Hallisey, R.K.; Hanson, C.; McKee, A.E.; Zuccotti, G.; Mort, E.A.; Sequist, T.D.; Kaufman, N.E.; Seguin, C.M.; et al. Improving Allergy Documentation: A Retrospective Electronic Health Record System-Wide Patient Safety Initiative. J. Patient Saf. 2022, 18, e108–e114. [Google Scholar] [CrossRef]
- Márquez-Contreras, E.; López García-Ramos, L.; Martell-Claros, N.; Gil-Guillen, V.F.; Márquez-Rivero, S.; Pérez-López, E.; Garrido-Lopez, M.A.; Farauste, C.; López-Pineda, A.; Casado-Martinez, J.J.; et al. Validation of the electronic prescription as a method for measuring treatment adherence in hypertension. Patient Educ. Couns. 2018, 101, 1654–1660. [Google Scholar] [CrossRef]



| Variable | Male (n = 612) | Female (n = 755) | p-Value | All Patients (n = 1367) |
|---|---|---|---|---|
| Age (years) | 55.65 ± 20.48 | 52.99 ± 19.44 | 0.0011 | 54.19 ± 19.95 |
| Weight (kg) | 75.45 ± 20.43 | 73.39 ± 18.80 | 0.0042 | 74.32 ± 19.57 |
| Age in Years | Percent (%) | Number of Males | Weight for Male (Mean ± SD) | Number of Females | Weight for Female (Mean ± SD) |
|---|---|---|---|---|---|
| 1 to <5 | 1.46 | 11 | 25.55 ± 30.3 | 9 | 15.00 ± 6.40 |
| 5 to ≤10 | 2.27 | 14 | 23.79 ± 5.69 | 17 | 28.21 ± 12.90 |
| >10 to ≤15 | 2.71 | 21 | 39.95 ± 13.60 | 16 | 49.88 ± 17.11 |
| >15 to ≤20 | 2.27 | 12 | 58.83 ± 28.22 | 19 | 58.37 ± 17.89 |
| >20 to ≤25 | 3.07 | 14 | 69.29 ± 29.03 | 28 | 64.75 ± 18.92 |
| >25 to ≤30 | 6.22 | 29 | 77.93 ± 20.72 | 56 | 68.57 ± 13.95 |
| >30 to ≤35 | 9.14 | 49 | 90.80 ± 18.64 | 76 | 77,53 ± 18.85 |
| >35 to ≤40 | 15.22 | 84 | 80.89 ± 16.97 | 124 | 79.68 ± 16.68 |
| >40 to ≤45 | 27.36 | 163 | 80.73 ± 12.51 | 211 | 78.09 ± 14.14 |
| >45 | 30.29 | 215 | 76.20 ± 11.88 | 199 | 75.33 ± 13.62 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alkathiri, S.; Alothman, R.; Ata, S.; Alruthia, Y. Evaluating the Wasfaty E-Prescribing Platform Against Best Practices for Computerized Provider Order Entry. Healthcare 2025, 13, 946. https://doi.org/10.3390/healthcare13080946
Alkathiri S, Alothman R, Ata S, Alruthia Y. Evaluating the Wasfaty E-Prescribing Platform Against Best Practices for Computerized Provider Order Entry. Healthcare. 2025; 13(8):946. https://doi.org/10.3390/healthcare13080946
Chicago/Turabian StyleAlkathiri, Saba, Razan Alothman, Sondus Ata, and Yazed Alruthia. 2025. "Evaluating the Wasfaty E-Prescribing Platform Against Best Practices for Computerized Provider Order Entry" Healthcare 13, no. 8: 946. https://doi.org/10.3390/healthcare13080946
APA StyleAlkathiri, S., Alothman, R., Ata, S., & Alruthia, Y. (2025). Evaluating the Wasfaty E-Prescribing Platform Against Best Practices for Computerized Provider Order Entry. Healthcare, 13(8), 946. https://doi.org/10.3390/healthcare13080946







