Unveiling the Mental Health of Postpartum Women During and After COVID-19: Analysis of Two Population-Based National Maternity Surveys in Romania (2020–2025)
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Sample Description
- Mothers aged 18–50 years, who gave birth during the SARS-CoV-2 pandemic or the post-pandemic period;
- Women who had given birth within the year prior to completing the survey;
- No history of psychiatric disorders;
- No history of peripartum depression in previous pregnancies;
- No past diagnosis or incidents of COVID-19 infection in the past year;
- Women who expressed interest in the topic and provided informed consent to participate in the study.
- Women currently using or with a history of psychotropic medication use;
- Women with high-risk pregnancies, including conditions such as preeclampsia, pregnancy-induced hypertension, gestational diabetes mellitus, intrauterine growth restriction, chronic diseases, chromosomal abnormalities, or known fetal anomalies;
- Women with a history of psychiatric disorders or mental health issues.
2.2. Ethical Declarations
2.3. Edinburgh Postnatal Depression Scale Questionnaire
2.4. Statistical Assessment
3. Results
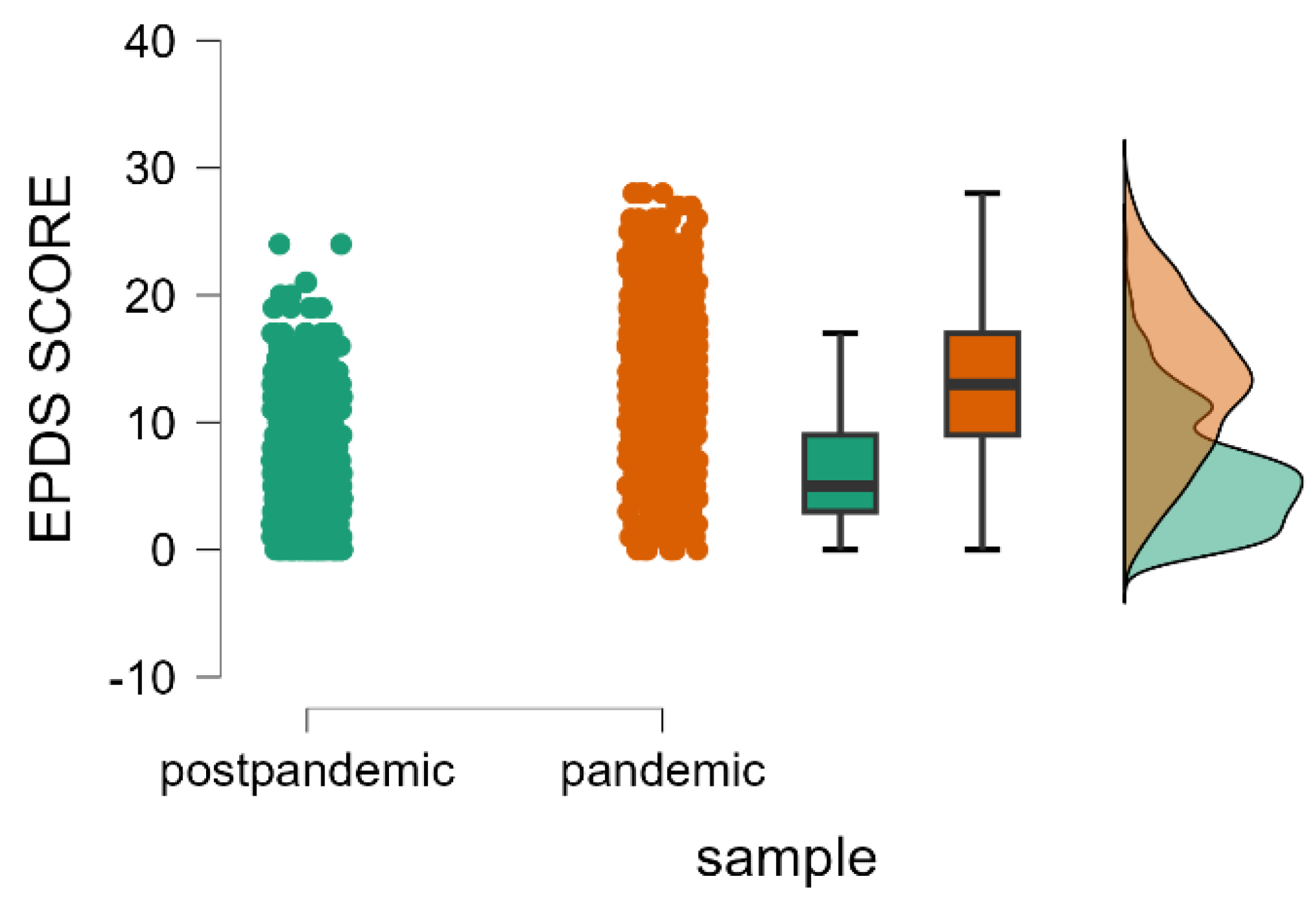
3.1. Prevalence of Postpartum Depression in the 2020–2023 and 2023–2025 Surveys
3.2. Factors Associated with Postnatal Depression
4. Discussion
4.1. Implications and Interpretation of Research Findings
4.2. Summary of Main Findings
4.3. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PPD | Postpartum depression |
| EPDS | Edinburgh Postnatal Depression Scale |
| SARS-CoV-2 | Severe acute respiratory syndrome coronavirus 2 |
| DSM-5 | The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition |
| DSM-5-TR | Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision |
| HIV | Human Immunodeficiency Virus |
| AIDS | Acquired Immunodeficiency Syndrome |
References
- O’Hara, M.W. Postpartum Depression: What We Know. J. Clin. Psychol. 2009, 65, 1258–1269. [Google Scholar] [CrossRef] [PubMed]
- Serati, M.; Redaelli, M.; Buoli, M.; Altamura, A.C. Perinatal Major Depression Biomarkers: A Systematic Review. J. Affect. Disord. 2016, 193, 391–404. [Google Scholar] [CrossRef] [PubMed]
- Sharma, R.; Bansal, P.; Saini, L.; Sharma, N.; Dhingra, R. Zuranolone, a Neuroactive Drug, Used in the Treatment of Postpartum Depression by Modulation of GABAA Receptors. Pharmacol. Biochem. Behav. 2024, 238, 173734. [Google Scholar] [CrossRef]
- Liu, X.; Wang, S.; Wang, G. Prevalence and Risk Factors of Postpartum Depression in Women: A Systematic Review and Meta-Analysis. J. Clin. Nurs. 2022, 31, 2665–2677. [Google Scholar] [CrossRef]
- Couto, T.C.e; Brancaglion, M.Y.M.; Alvim-Soares, A.; Moreira, L.; Garcia, F.D.; Nicolato, R.; Aguiar, R.A.L.P.; Leite, H.V.; Corrêa, H. Postpartum Depression: A Systematic Review of the Genetics Involved. World J. Psychiatry 2015, 5, 103–111. [Google Scholar] [CrossRef]
- Hahn-Holbrook, J.; Cornwell-Hinrichs, T.; Anaya, I. Economic and Health Predictors of National Postpartum Depression Prevalence: A Systematic Review, Meta-Analysis, and Meta-Regression of 291 Studies from 56 Countries. Front. Psychiatry 2017, 8, 248. [Google Scholar] [CrossRef] [PubMed]
- Slomian, J.; Honvo, G.; Emonts, P.; Reginster, J.-Y.; Bruyère, O. Consequences of Maternal Postpartum Depression: A Systematic Review of Maternal and Infant Outcomes. Womens Health 2019, 15, 1745506519844044. [Google Scholar] [CrossRef]
- Harrison, S.; Quigley, M.A.; Fellmeth, G.; Stein, A.; Alderdice, F. The Impact of the COVID-19 Pandemic on Postnatal Depression: Analysis of Three Population-Based National Maternity Surveys in England (2014–2020). Lancet Reg. Health-Eur. 2023, 30, 100654. [Google Scholar] [CrossRef]
- Wyszynski, D.F.; Hernandez-Diaz, S.; Gordon-Dseagu, V.; Ramiro, N.; Basu, A.; Kim, H.H.; Koenen, K.C. Frequency and Source of Worries in an International Sample of Pregnant and Postpartum Women during the COVID-19 Pandemic. BMC Pregnancy Childbirth 2021, 21, 768. [Google Scholar] [CrossRef]
- Siegel, M.R.; Lumbreras-Marquez, M.I.; James, K.; McBay, B.R.; Gray, K.J.; Schantz-Dunn, J.; Diouf, K.; Goldfarb, I.T. Perceptions and Attitudes toward COVID-19 Vaccination among Pregnant and Postpartum Individuals. Am. J. Perinatol. 2022, 29, 1489–1495. [Google Scholar] [CrossRef]
- Caparros-Gonzalez, R.A.; Alderdice, F. The COVID-19 Pandemic and Perinatal Mental Health. J. Reprod. Infant Psychol. 2020, 38, 223–225. [Google Scholar] [CrossRef] [PubMed]
- Rocca-Ihenacho, L.; Alonso, C. Where Do Women Birth during a Pandemic? Changing Perspectives on Safe Motherhood during the COVID-19 Pandemic. J. Glob. Health Sci. 2020, 2, e4. [Google Scholar] [CrossRef]
- Silverio, S.A.; De Backer, K.; Easter, A.; von Dadelszen, P.; Magee, L.A.; Sandall, J. Women’s Experiences of Maternity Service Reconfiguration during the COVID-19 Pandemic: A Qualitative Investigation. Midwifery 2021, 102, 103116. [Google Scholar] [CrossRef]
- Chmielewska, B.; Barratt, I.; Townsend, R.; Kalafat, E.; van der Meulen, J.; Gurol-Urganci, I.; O’Brien, P.; Morris, E.; Draycott, T.; Thangaratinam, S.; et al. Effects of the COVID-19 Pandemic on Maternal and Perinatal Outcomes: A Systematic Review and Meta-Analysis. Lancet Glob. Health 2021, 9, e759–e772. [Google Scholar] [CrossRef] [PubMed]
- Shuman, C.J.; Peahl, A.F.; Pareddy, N.; Morgan, M.E.; Chiangong, J.; Veliz, P.T.; Dalton, V.K. Postpartum Depression and Associated Risk Factors during the COVID-19 Pandemic. BMC Res. Notes 2022, 15, 102. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A Flexible Statistical Power Analysis Program for the Social, Behavioral, and Biomedical Sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of Postnatal Depression. Development of the 10-Item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 1987, 150, 782–786. [Google Scholar] [CrossRef]
- Lebel, C.; MacKinnon, A.; Bagshawe, M.; Tomfohr-Madsen, L.; Giesbrecht, G. Elevated Depression and Anxiety Symptoms among Pregnant Individuals during the COVID-19 Pandemic. J. Affect. Disord. 2020, 277, 5–13. [Google Scholar] [CrossRef]
- Matsumura, K.; Hamazaki, K.; Tsuchida, A.; Kasamatsu, H.; Inadera, H. Factor Structure of the Edinburgh Postnatal Depression Scale in the Japan Environment and Children’s Study. Sci. Rep. 2020, 10, 11647. [Google Scholar] [CrossRef]
- Bergant, A.M.; Nguyen, T.; Heim, K.; Ulmer, H.; Dapunt, O. German language version and validation of the Edinburgh postnatal depression scale. Dtsch. Med. Wochenschr. 1998, 123, 35–40. [Google Scholar] [CrossRef]
- Vivilaki, V.G.; Dafermos, V.; Kogevinas, M.; Bitsios, P.; Lionis, C. The Edinburgh Postnatal Depression Scale: Translation and Validation for a Greek Sample. BMC Public Health 2009, 9, 329. [Google Scholar] [CrossRef] [PubMed]
- Wallis, A.; Fernandez, R.; Florin, O.; Cherecheş, R.; Zlati, A.; Dungy, C. Validation of a Romanian Scale to Detect Antenatal Depression. Cent. Eur. J. Med. 2012, 7, 216–223. [Google Scholar] [CrossRef]
- Levis, B.; Negeri, Z.; Sun, Y.; Benedetti, A.; Thombs, B.D.; DEPRESsion Screening Data (DEPRESSD) EPDS Group. Accuracy of the Edinburgh Postnatal Depression Scale (EPDS) for Screening to Detect Major Depression among Pregnant and Postpartum Women: Systematic Review and Meta-Analysis of Individual Participant Data. Br. Med. J. 2020, 371, m4022. [Google Scholar] [CrossRef]
- Shrestha, S.D.; Pradhan, R.; Tran, T.D.; Gualano, R.C.; Fisher, J.R.W. Reliability and Validity of the Edinburgh Postnatal Depression Scale (EPDS) for Detecting Perinatal Common Mental Disorders (PCMDs) among Women in Low-and Lower-Middle-Income Countries: A Systematic Review. BMC Pregnancy Childbirth 2016, 16, 72. [Google Scholar] [CrossRef]
- JASP Team. JASP, Version 0.19.3. [Computer Software]. JASP Team: Amsterdam, The Netherlands, 2024. Available online: https://Jasp-Stats.Org/ (accessed on 6 March 2025).
- Ciolac, L.; Craina, M.L.; Enatescu, V.R.; Tudor, A.; Bernad, E.S.; Nitu, R.; Hogea, L.; Boscu, L.; Bernad, B.-C.; Timircan, M.O.; et al. The Impact of the COVID-19 Pandemic on Depressive Disorder with Postpartum Onset: A Cross-Sectional Study. Healthcare 2023, 11, 2857. [Google Scholar] [CrossRef]
- Yan, H.; Ding, Y.; Guo, W. Mental Health of Pregnant and Postpartum Women During the Coronavirus Disease 2019 Pandemic: A Systematic Review and Meta-Analysis. Front. Psychol. 2020, 11, 617001. [Google Scholar] [CrossRef]
- Iyengar, U.; Jaiprakash, B.; Haitsuka, H.; Kim, S. One Year into the Pandemic: A Systematic Review of Perinatal Mental Health Outcomes During COVID-19. Front. Psychiatry 2021, 12, 674194. [Google Scholar] [CrossRef] [PubMed]
- Hessami, K.; Romanelli, C.; Chiurazzi, M.; Cozzolino, M. COVID-19 Pandemic and Maternal Mental Health: A Systematic Review and Meta-Analysis. J. Matern. Fetal Neonatal Med. 2022, 35, 4014–4021. [Google Scholar] [CrossRef]
- Shorey, S.Y.; Ng, E.D.; Chee, C.Y.I. Anxiety and Depressive Symptoms of Women in the Perinatal Period during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Scand. J. Public Health 2021, 49, 730–740. [Google Scholar] [CrossRef]
- Wang, Z.; Liu, J.; Shuai, H.; Cai, Z.; Fu, X.; Liu, Y.; Xiao, X.; Zhang, W.; Krabbendam, E.; Liu, S.; et al. Mapping Global Prevalence of Depression among Postpartum Women. Transl. Psychiatry 2021, 11, 543. [Google Scholar] [CrossRef]
- Usmani, S.; Greca, E.; Javed, S.; Sharath, M.; Sarfraz, Z.; Sarfraz, A.; Salari, S.W.; Hussaini, S.S.; Mohammadi, A.; Chellapuram, N.; et al. Risk Factors for Postpartum Depression During COVID-19 Pandemic: A Systematic Literature Review. J. Prim. Care Community Health 2021, 12, 21501327211059348. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, S. Psychological Status of Postpartum Women under the COVID-19 Pandemic in Japan. J. Matern.-Fetal Neonatal Med. 2022, 35, 1798–1800. [Google Scholar] [CrossRef]
- Pariente, G.; Broder, O.W.; Sheiner, E.; Battat, T.L.; Mazor, E.; Salem, S.Y.; Kosef, T.; Wainstock, T. Risk for Probable Post-Partum Depression among Women during the COVID-19 Pandemic. Arch. Womens Ment. Health 2020, 23, 767–773. [Google Scholar] [CrossRef]
- Kuipers, Y.J.; Bleijenbergh, R.; Van den Branden, L.; van Gils, Y.; Rimaux, S.; Brosens, C.; Claerbout, A.; Mestdagh, E. Psychological Health of Pregnant and Postpartum Women before and during the COVID-19 Pandemic. PLoS ONE 2022, 17, e0267042. [Google Scholar] [CrossRef]
- Zanardo, V.; Manghina, V.; Giliberti, L.; Vettore, M.; Severino, L.; Straface, G. Psychological Impact of COVID-19 Quarantine Measures in Northeastern Italy on Mothers in the Immediate Postpartum Period. Int. J. Gynaecol. Obstet. 2020, 150, 184–188. [Google Scholar] [CrossRef]
- Zhang, C.X.W.; Okeke, J.C.; Levitan, R.D.; Murphy, K.E.; Foshay, K.; Lye, S.J.; Knight, J.A.; Matthews, S.G. Evaluating Depression and Anxiety throughout Pregnancy and after Birth: Impact of the COVID-19 Pandemic. Am. J. Obstet. Gynecol. MFM 2022, 4, 100605. [Google Scholar] [CrossRef] [PubMed]
- Perez, A.; Göbel, A.; Stuhrmann, L.Y.; Schepanski, S.; Singer, D.; Bindt, C.; Mudra, S. Born Under COVID-19 Pandemic Conditions: Infant Regulatory Problems and Maternal Mental Health at 7 Months Postpartum. Front. Psychol. 2022, 12, 805543. [Google Scholar] [CrossRef]
- Dadi, A.F.; Miller, E.R.; Mwanri, L. Postnatal Depression and Its Association with Adverse Infant Health Outcomes in Low- and Middle-Income Countries: A Systematic Review and Meta-Analysis. BMC Pregnancy Childbirth 2020, 20, 416. [Google Scholar] [CrossRef]
- Chen, J.; Cross, W.M.; Plummer, V.; Lam, L.; Tang, S. A Systematic Review of Prevalence and Risk Factors of Postpartum Depression in Chinese Immigrant Women. Women Birth 2019, 32, 487–492. [Google Scholar] [CrossRef]
- Perzow, S.E.D.; Hennessey, E.-M.P.; Hoffman, M.C.; Grote, N.K.; Davis, E.P.; Hankin, B.L. Mental Health of Pregnant and Postpartum Women in Response to the COVID-19 Pandemic. J. Affect. Disord. Rep. 2021, 4, 100123. [Google Scholar] [CrossRef]
- Davenport, M.H.; Meyer, S.; Meah, V.L.; Strynadka, M.C.; Khurana, R. Moms Are Not OK: COVID-19 and Maternal Mental Health. Front. Glob. Womens Health 2020, 1, 561147. [Google Scholar] [CrossRef] [PubMed]
- Stojanov, J.; Stankovic, M.; Zikic, O.; Stankovic, M.; Stojanov, A. The Risk for Nonpsychotic Postpartum Mood and Anxiety Disorders during the COVID-19 Pandemic. Int. J. Psychiatry Med. 2021, 56, 228–239. [Google Scholar] [CrossRef] [PubMed]
- Bradshaw, H.; Riddle, J.N.; Salimgaraev, R.; Zhaunova, L.; Payne, J.L. Risk Factors Associated with Postpartum Depressive Symptoms: A Multinational Study. J. Affect. Disord. 2022, 301, 345–351. [Google Scholar] [CrossRef]
- Dira, I.K.P.A.; Wahyuni, A.A.S. Prevalensi dan Faktor Risiko Depresi Postpartum di Kota Denpasar Menggunakan Edinburgh Postnatal Depression Scale. E-J. Med. Udayana 2016, 5, 1–5. [Google Scholar]
- Coca, K.P.; Chien, L.-Y.; Lee, E.Y.; de Prima Souza, A.C.; Hong, S.A.; Chang, Y.-S. Factors Associated with Postpartum Depression Symptoms among Postpartum Women in Five Countries during the COVID-19 Pandemic: An Online Cross-Sectional Study. BMC Psychiatry 2023, 23, 171. [Google Scholar] [CrossRef]
- Matsumura, K.; Hamazaki, K.; Tsuchida, A.; Kasamatsu, H.; Inadera, H.; Japan Environment and Children’s Study (JECS) Group. Education Level and Risk of Postpartum Depression: Results from the Japan Environment and Children’s Study (JECS). BMC Psychiatry 2019, 19, 419. [Google Scholar] [CrossRef]
- Villegas, L.; McKay, K.; Dennis, C.-L.; Ross, L.E. Postpartum Depression among Rural Women from Developed and Developing Countries: A Systematic Review. J. Rural Health 2011, 27, 278–288. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Dee, V. Sociodemographic and Obstetric Factors Related to Symptoms of Postpartum Depression in Hispanic Women in Rural California. J. Obstet. Gynecol. Neonatal Nurs. 2018, 47, 23–31. [Google Scholar] [CrossRef]
- Mollard, E.; Hudson, D.B.; Ford, A.; Pullen, C. An Integrative Review of Postpartum Depression in Rural U.S. Communities. Arch. Psychiatr. Nurs 2016, 30, 418–424. [Google Scholar] [CrossRef]
- Xu, H.; Ding, Y.; Ma, Y.; Xin, X.; Zhang, D. Cesarean Section and Risk of Postpartum Depression: A Meta-Analysis. J. Psychosom. Res 2017, 97, 118–126. [Google Scholar] [CrossRef]
- Simionescu, A.A.; Horobet, A.; Erika, M.; Belascu, L. Who Indicates Caesarean Section in Romania? A Cross-Sectional Survey in Tertiary Level Maternity on Childbirth Patients and Doctors’ Profiles. 2020. Available online: https://www.researchgate.net/publication/346375529_Who_indicates_Caesarean_section_in_Romania_A_cross-sectional_survey_in_tertiary_level_maternity_on_childbirth_patients_and_doctors’_profiles (accessed on 10 April 2025).
- Simionescu, A.A.; Erika, M. Caesarean Birth in Romania: Safe Motherhood Between Ethical, Medical and Statistical Arguments. Maedica 2017, 12, 5–12. [Google Scholar]
- Winkler-Dworak, M.; Zeman, K.; Sobotka, T. Birth Rate Decline in the Later Phase of the COVID-19 Pandemic: The Role of Policy Interventions, Vaccination Programmes, and Economic Uncertainty. Hum. Reprod. Open 2024, 2024, hoae052. [Google Scholar] [CrossRef] [PubMed]
- Allen, M.O.T.; Rhoades, G.K.; Mazzoni, S.E. Individual-Oriented Relationship Education and Postpartum Depression: The Impact of the MotherWise Program. Couple Fam. Psychol. Res. Pract. 2024, 13, 263–275. [Google Scholar] [CrossRef]
- Mousa, O.; Al Sabati, S.Y.; Al Khars, F. Postpartum Depression: Neglected Issue in Maternal Health. Int. J. Nurs. Educ. 2023, 15, 72–77. [Google Scholar] [CrossRef]
- Feldman, N.; Perret, S. Digital Mental Health for Postpartum Women: Perils, Pitfalls, and Promise. Npj Digit. Med. 2023, 6, 11. Available online: https://www.nature.com/articles/s41746-023-00756-4 (accessed on 3 March 2025). [CrossRef]
- Browning, H.S. Impact of COVID-19 Healthcare Policies on Postpartum Depression. Master’s Thesis, Rhode Island College, Providence, RI, USA, 2023. [Google Scholar]
- Luca, D.L.; Margiotta, C.; Staatz, C.; Garlow, E.; Christensen, A.; Zivin, K. Financial Toll of Untreated Perinatal Mood and Anxiety Disorders Among 2017 Births in the United States. Am. J. Public Health 2020, 110, 888–896. [Google Scholar] [CrossRef]
- Overview|Antenatal and Postnatal Mental Health: Clinical Management and Service Guidance|Guidance|NICE. Available online: https://www.nice.org.uk/guidance/cg192 (accessed on 2 March 2025).
| Association Variables | Sample | p Value | ||
|---|---|---|---|---|
| COVID-19 Pandemic Period (n = 860) | Post-Pandemic Period (n = 860) | |||
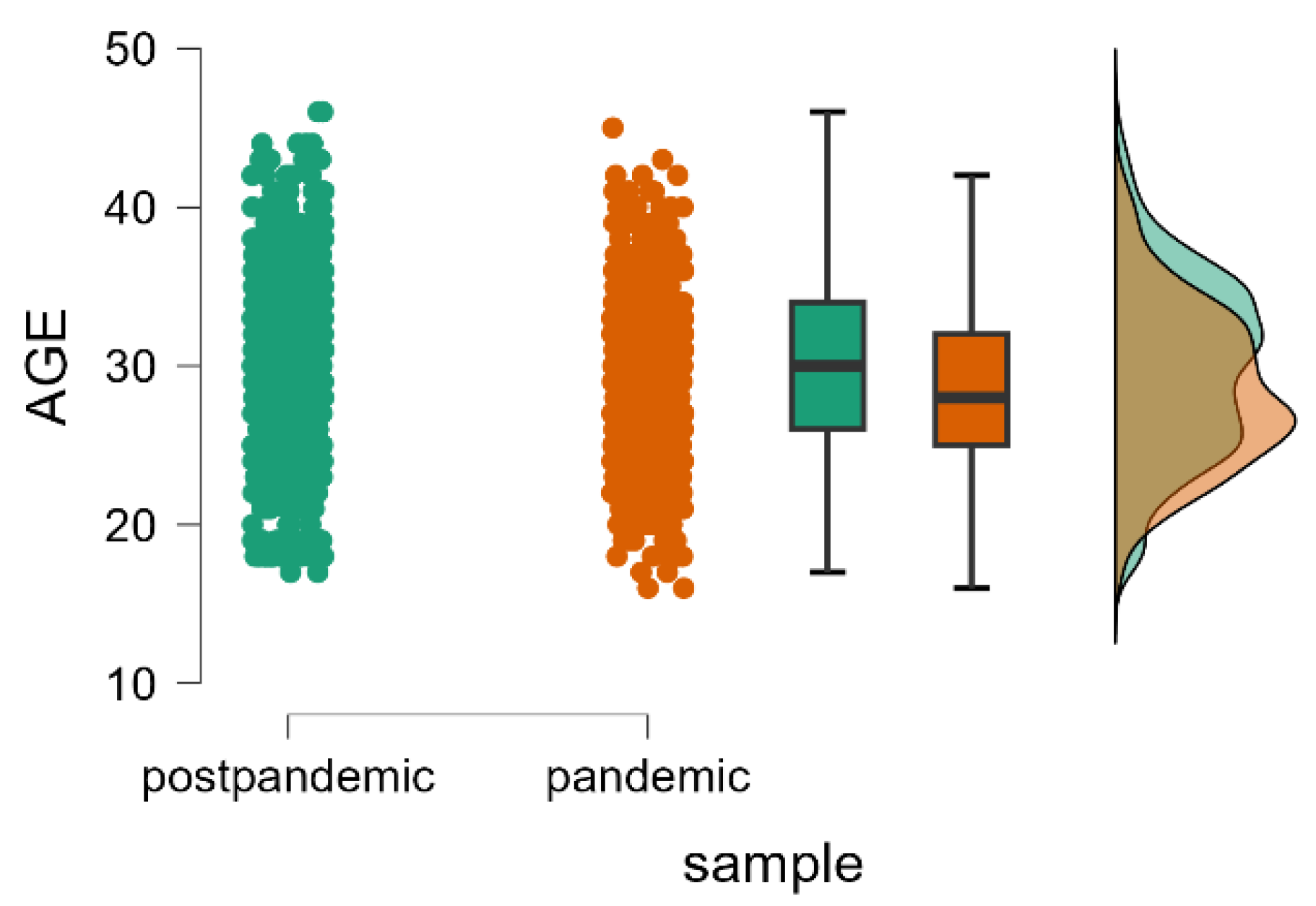
| Age Mean ± SD Median (Q1–Q3) | 28.45 ± 5.18 28 (25–32) | 30.06 ± 5.62 30 (26–34) | <0.001 * | |
| EPDS score Mean ± SD Median (Q1–Q3) | 13.06 ± 6.01 13 (9–17) | 6.12 ± 4.56 5 (3–9) | <0.001 * | |
| Postpartum depressive disorder n (%) | Major postpartum depressive disorder | 466 (54.186%) | 87 (10.116%) | <0.001 * |
| Minor postpartum depressive disorder | 134 (15.581%) | 94 (10.930%) | 0.006 * | |
| Without postpartum depressive disorder | 260 (30.233%) | 679 (78.954%) | <0.001 * | |
| Marital status n (%) | Married | 746 (86.744%) | 703 (81.744%) | 0.005 * |
| Cohabiting | 98 (11.395%) | 89 (10.349%) | 0.536 | |
| Divorced | 0 (0%) | 24 (2.791%) | <0.001 * | |
| Single | 16 (1.860%) | 44 (5.116%) | <0.001 * | |
| Area of residence n (%) | Urban | 598 (69.535%) | 468 (54.419%) | <0.001 * |
| Rural | 262 (30.465%) | 392 (45.581%) | ||
| Level of education n (%) | Higher education | 509 (59.186%) | 447 (51.977%) | 0.003 * |
| High school graduate | 277 (32.209%) | 266 (30.930%) | 0.604 | |
| Vocational school | 0 (0%) | 56 (6.512%) | <0.001 * | |
| Middle school | 74 (8.605%) | 55 (6.395%) | 0.099 | |
| Primary education | 0 (0%) | 36 (4.186%) | <0.001 * | |
| Socio-economic conditions n (%) | Very good standard of living | 167 (19.419%) | 228 (26.512%) | <0.001 * |
| Good standard of living | 507 (58.953%) | 503 (58.488%) | 0.883 | |
| Satisfactory conditions | 160 (18.605%) | 125 (14.535%) | 0.027 * | |
| Poor living conditions | 26 (3.023%) | 4 (0.465%) | <0.001 * | |
| Workplace hazard n (%) | High | 72 (8.372%) | 40 (4.651%) | 0.002 * |
| Medium | 195 (22.674%) | 139 (16.163%) | <0.001 * | |
| Low | 593 (68.953%) | 681 (79.186%) | <0.001 * | |
| Health status n (%) | Good | 683 (79.419%) | 809 (94.070%) | <0.001 * |
| Satisfactory | 168 (19.535%) | 51 (5.930%) | <0.001 * | |
| Poor | 9 (1.047%) | 0 (0%) | 0.023 * | |
| Parity n (%) | Primiparous | 561 (65.232%) | 417 (48.488%) | <0.001 * |
| Secundiparous | 242 (28.139%) | 300 (34.883%) | 0.003 * | |
| Tertiparous | 45 (5.232%) | 92 (10.697%) | <0.001 * | |
| Quadriparous | 11 (1.279%) | 30 (3.4883%) | 0.005 * | |
| Multiparous (5+) | 1 (0.116%) | 21 (2.4418%) | <0.001 * | |
| Number of miscarriages in their personal obstetric history n (%) | No miscarriage | 689 (80.116%) | 700 (81.395%) | 0.534 |
| 1 miscarriage | 130 (15.116%) | 117 (13.604%) | 0.413 | |
| 2 miscarriages | 34 (3.953%) | 18 (2.093%) | 0.030 * | |
| 3 miscarriages | 5 (0.581%) | 19 (2.209%) | 0.008 * | |
| 4 miscarriages | 2 (0.232%) | 6 (0.697%) | 0.235 | |
| Number of abortions performed upon request in their personal obstetric history n (%) | No abortion on request | 750 (87.209%) | 755 (87.790%) | 0.766 |
| 1 abortion on request | 77 (8.953%) | 83 (9.651%) | 0.703 | |
| 2 abortions on request | 23 (2.674%) | 10 (1.162%) | 0.032 * | |
| 3 abortions on request | 8 (0.930%) | 8 (0.930%) | 0.851 | |
| 4 abortions on request | 0 (0%) | 4 (0.465%) | 0.130 | |
| 5 abortions on request | 2 (0.232%) | 0 (0%) | 0.583 | |
| Method of achieving pregnancy n (%) | Naturally | 824 (95.813%) | 848 (98.604%) | <0.001 * |
| In vitro fertilization | 10 (1.162%) | 8 (0.930%) | 0.812 | |
| With previous treatment | 26 (3.023%) | 4 (0.465%) | <0.001 * | |
| Type of birth n (%) | Cesarean section | 262 (30.465%) | 392 (45.581%) | 0.016 * |
| Vaginal delivery | 598 (69.534%) | 468 (54.418%) | ||
| Association Variables | Type of Birth | p Value | Postpartum Depression | p Value | |||
|---|---|---|---|---|---|---|---|
| Cesarean Section | Vaginal Delivery | Absence | Presence | ||||
| Depressive disorder | Without | 128 (25.80%) | 132 (36.30%) | 0.0012 * | |||
| Minor | 78 (15.70%) | 56 (15.40%) | 0.98 | ------------ | |||
| Major | 290 (58.50%) | 176 (48.40%) | 0.0041 * | ||||
| Marital status | Married | 441 (88.90%) | 305 (83.80%) | 0.0382 * | 229 (88.10%) | 517 (86.17%) | 0.511 |
| Cohabiting | 41 (8.30%) | 57 (15.70%) | 0.0011 * | 26 (10.00%) | 72 (12.00%) | 0.465 | |
| Single | 14 (2.80%) | 2 (0.50%) | 0.026 * | 5 (1.90%) | 11 (1.83%) | 0.837 | |
| Education level | Less than high school | 24 (4.80%) | 50 (13.70%) | <0.001 * | 24 (9.20%) | 50 (8.30%) | 0.764 |
| High school graduate | 160 (32.30%) | 117 (32.10%) | 0.991 | 67 (25.8%) | 210 (35.00%) | 0.010 * | |
| Higher education | 312 (62.90%) | 197 (54.10%) | 0.012 * | 169 (65.00%) | 340 (56.70%) | 0.028 * | |
| Socio-economic conditions | Good | 290 (58.50%) | 217 (59.60%) | 0.799 | 157 (60.40%) | 350 (58.30%) | 0.617 |
| Very good | 111 (22.40%) | 56 (15.40%) | 0.013 * | 60 (23.10%) | 107 (17.80%) | 0.087 | |
| Poor | 10 (2.00%) | 16 (4.40%) | 0.067 | 4 (1.50%) | 22 (3.70%) | 0.131 | |
| Satisfactory | 85 (17.10%) | 75 (20.60%) | 0.224 | 39 (15.00%) | 121 (20.20%) | 0.088 | |
| Health status | Good | 386 (77.80%) | 297 (81.60%) | 0.202 | 232 (89.20%) | 451 (75.20%) | <0.001 * |
| Poor | 6 (1.20%) | 3 (0.80%) | 0.816 | 1 (0.40%) | 8 (1.30%) | 0.404 | |
| Fair | 104 (21.00%) | 64 (17.60%) | 0.248 | 27 (10.40%) | 141 (23.50%) | <0.001 * | |
| Association Variables | Type of Birth | p Value | Postpartum Depression | p Value | |||
|---|---|---|---|---|---|---|---|
| Cesarean Section (545) | Vaginal Delivery (315) | Absence (679) | Presence (181) | ||||
| Depressive disorder | Without | 428 (78.50%) | 251 (79.70%) | 0.104 | |||
| Minor | 54 (9.90%) | 40 (12.70%) | ------------ | ||||
| Major | 63 (11.60%) | 24 (7.60%) | |||||
| Marital status | Married | 454 (83.30%) | 249 (79.00%) | 0.362 | 565 (83.20%) | 138 (76.20%) | 0.146 |
| Cohabiting | 53 (9.70%) | 36 (11.40%) | 66 (9.70%) | 23 (12.70%) | |||
| Divorced | 12 (2.20%) | 12 (3.8%) | 18 (2.70%) | 6 (3.30%) | |||
| Single | 26 (4.80%) | 18 (5.70%) | 30 (4.40%) | 14 (7.70%) | |||
| Education level | Primary education | 14 (2.60%) | 22 (7.00%) | 0.004 * | 28 (4.10%) | 8 (4.40%) | 0.947 |
| Middle school | 35 (6.4%) | 20 (6.30%) | 0.930 | 30 (4.40%) | 25 (13.80%) | <0.001 * | |
| Vocational school | 32 (5.9%) | 24 (7.60%) | 0.409 | 44 (6.50%) | 12 (6.60%) | 0.904 | |
| High school graduate | 168 (30.80%) | 98 (31.10%) | 0.988 | 218 (32.10%) | 48 (26.50%) | 0.174 | |
| Higher education | 296 (54.30%) | 151 (47.90%) | 0.082 | 359 (52.90%) | 88 (48.60%) | 0.345 | |
| Workplace Hazard | High | 28 (5.10%) | 12 (3.80%) | 0.671 | 28 (4.10%) | 12 (6.60%) | 0.339 |
| Low | 429 (78.70%) | 252 (80.00%) | 539 (79.40%) | 142 (78.50%) | |||
| Medium | 88 (16.10%) | 51 (16.20%) | 112 (16.50%) | 27 (14.90%) | |||
| Socio-economic conditions | Good | 345 (63.30%) | 158 (50.20%) | <0.001 * | 404 (59.50%) | 99 (54.70%) | 0.280 |
| Very good | 131 (24.00%) | 97 (30.80%) | 0.036 * | 188 (27.70%) | 40 (22.10%) | 0.155 | |
| Poor | 2 (0.40%) | 2 (0.60%) | 0.917 | 2 (0.30%) | 2 (1.10%) | 0.431 | |
| Satisfactory | 67 (12.30%) | 58 (18.40%) | 0.019 * | 85 (12.50%) | 40 (22.10%) | 0.002 * | |
| Health status | Good | 508 (93.20%) | 301 (95.60%) | 0.104 | 644 (94.80%) | 165 (91.20%) | 0.075 |
| Satisfactory | 37 (6.80%) | 14 (4.40%) | 35 (5.20%) | 16 (8.80%) | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ciolac, L.; Nițu, D.-R.; Bernad, E.S.; Gluhovschi, A.; Popa, D.-I.; Toc, T.; Tudor, A.; Maghiari, A.-L.; Craina, M.L. Unveiling the Mental Health of Postpartum Women During and After COVID-19: Analysis of Two Population-Based National Maternity Surveys in Romania (2020–2025). Healthcare 2025, 13, 911. https://doi.org/10.3390/healthcare13080911
Ciolac L, Nițu D-R, Bernad ES, Gluhovschi A, Popa D-I, Toc T, Tudor A, Maghiari A-L, Craina ML. Unveiling the Mental Health of Postpartum Women During and After COVID-19: Analysis of Two Population-Based National Maternity Surveys in Romania (2020–2025). Healthcare. 2025; 13(8):911. https://doi.org/10.3390/healthcare13080911
Chicago/Turabian StyleCiolac, Livia, Dumitru-Răzvan Nițu, Elena Silvia Bernad, Adrian Gluhovschi, Daian-Ionel Popa, Teodora Toc, Anca Tudor, Anca-Laura Maghiari, and Marius Lucian Craina. 2025. "Unveiling the Mental Health of Postpartum Women During and After COVID-19: Analysis of Two Population-Based National Maternity Surveys in Romania (2020–2025)" Healthcare 13, no. 8: 911. https://doi.org/10.3390/healthcare13080911
APA StyleCiolac, L., Nițu, D.-R., Bernad, E. S., Gluhovschi, A., Popa, D.-I., Toc, T., Tudor, A., Maghiari, A.-L., & Craina, M. L. (2025). Unveiling the Mental Health of Postpartum Women During and After COVID-19: Analysis of Two Population-Based National Maternity Surveys in Romania (2020–2025). Healthcare, 13(8), 911. https://doi.org/10.3390/healthcare13080911







