Impact of Pharmacist Educational Intervention on Costs of Medication with Improved Clinical Outcomes for Diabetic Patients in Various Tertiary Care Hospitals in Malaysia: A Randomized Controlled Trial
Abstract
1. Introduction
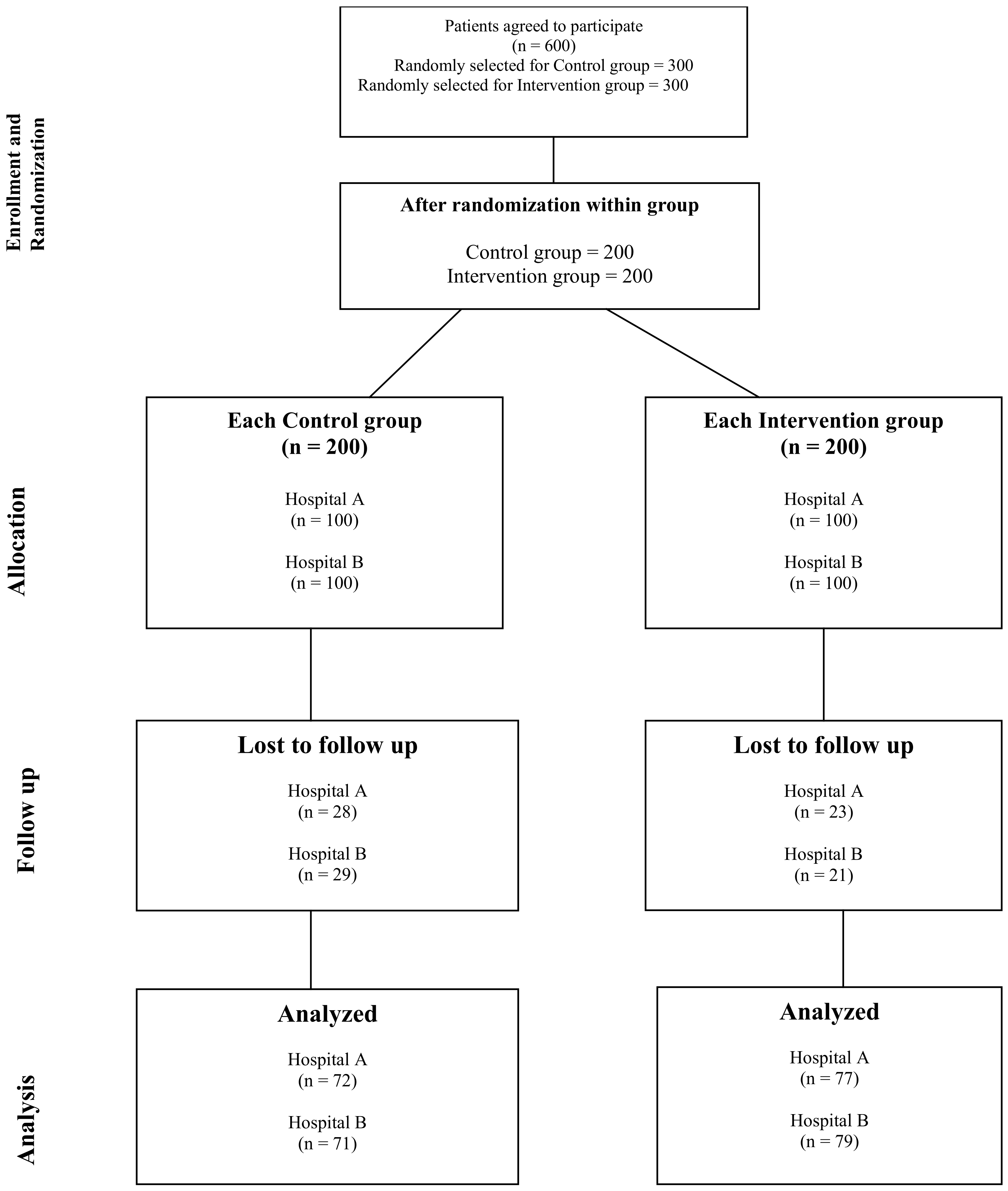
2. Methodology
2.1. Study Design
2.2. Study Population and Study Approvals
2.3. Procedure and Randomization
2.4. Data Collection and Data Management
2.5. Validation of Tools for Data Collection
2.6. Data Requisite for Study Tool
2.7. Statistical Analysis
2.8. Confidentiality and Data Security
3. Results
3.1. Clinical Outcome Measurements
3.2. Cost of Medication Measure
| Parameters | Cost for 3 Months Mean ± SD CG (N = 143) | Difference from Baseline Price | Cost for 3 Months Mean ± SD IG (N = 156) | Difference from Baseline Price | t-Statistic (df) | p-Value |
|---|---|---|---|---|---|---|
| Insulin | MYR 918.62 ± 230.43 | MYR +154.72 | MYR 811.94 ± 165.69 | MYR +28.93 | 4.62 (1, 297) | <0.001 |
| Oral antidiabetics | MYR 87.03 ± 52.43 | MYR +38.32 | MYR 56.37 ± 27.67 | MYR +7.62 | 6.39 (1, 297) | <0.001 |
| Diabetic comorbidities | MYR 85.20 ± 10.26 | MYR +6.4 | MYR 80.75 ± 6.05 | MYR +1.87 | 4.60 (1, 297) | <0.001 |
| Diabetic complications | MYR 379.84 ± 39.80 | MYR +29.63 | MYR 359.37 ± 33.21 | MYR +11.88 | 4.84 (1, 297) | <0.001 |
| Multivitamins and minerals | MYR 18.44 ± 4.77 | MYR +2.59 | MYR 14.88 ± 2.06 | MYR −0.37 | 8.47 (1, 297) | <0.001 |
| NSAIDs | MYR 3.23 ± 0.97 | MYR +0.55 | MYR 2.21 ± 0.80 | MYR −0.38 | 9.90 (1, 297) | <0.001 |
| Others | MYR 26.72 ± 6.48 | MYR +3.86 | MYR 19.88 ± 3.73 | MYR −2.22 | 11.29 (1, 297) | <0.001 |
4. Discussion
4.1. Impact on Glycated Hemoglobin (HbA1c)
4.2. Medication Costs and Analysis
4.3. Comparison with Previous Studies
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Pharmacists Association. Pharmacists’ Impact on Patient Safety. 2016. Available online: https://www.pharmacist.com/Portals/0/PDFS/Practice/PharmacistsImpactonPatientSafety_Web.pdf?ver=dYeAzwlN3-PG9eSkMMsV-A%3D%3D (accessed on 25 March 2025).
- Polonsky, W.H.; Henry, R.R. Poor medication adherence in type 2 diabetes: Recognizing the scope of the problem and its key contributors. Patient Prefer. Adherence 2016, 10, 1299–1306. [Google Scholar] [CrossRef]
- Jeong, S.; Lee, M.; Ji, E. Effect of pharmaceutical care interventions on glycemic control in patients with diabetes: A systematic review and meta-analysis. Ther. Clin. Risk Manag. 2018, 14, 1813–1829. [Google Scholar] [CrossRef]
- Marín-Peñalver, J.J.; Martín-Timón, I.; Sevillano-Collantes, C.; del Cañizo-Gómez, F.J. Update on the treatment of type 2 diabetes mellitus. World J. Diabetes 2016, 7, 354. [Google Scholar] [CrossRef]
- Iqbal, M.; Khan, A.; Syed Sulaiman, S.A. A Review of Pharmacist-led Interventions on Diabetes Outcomes: An Observational Analysis to Explore Diabetes Care Opportunities for Pharmacists. J. Pharm. Bioallied Sci. 2019, 11, 299. [Google Scholar] [CrossRef]
- CPG Malaysia. Clinical Practice Guidelines Management of Type 2 Diabetes Mellitus, 6th ed.; CPG Malaysia: Kuala Lumpur, Malaysia, 2020. Available online: https://www.moh.gov.my/moh/resources/Penerbitan/CPG/Endocrine/QR_T2DM_6th_Edition_QR_Guide_Digital.pdf (accessed on 9 April 2025).
- Khan, M.A.B.; Hashim, M.J.; King, J.K.; Govender, R.D.; Mustafa, H.; Al Kaabi, J. Epidemiology of Type 2 Diabetes—Global Burden of Disease and Forecasted Trends. J. Epidemiol. Glob. Health 2020, 10, 107–111. [Google Scholar] [CrossRef]
- Paz-Pacheco, E. Diabetes Clinical Practice Guidelines (CPGs) for the ASEAN region: Country Initiatives for Collectively Enhanced Diabetes Care in the Region. J. ASEAN Fed. Endocr. Soc. 2011, 26, 36. [Google Scholar] [CrossRef]
- Zheng, Y.; Ley, S.H.; Hu, F.B. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat. Rev. Endocrinol. 2017, 14, 88–98. [Google Scholar] [CrossRef]
- Ha, K.H.; Kim, D.J. Current status of managing diabetes mellitus in Korea. Korean J. Intern. Med. 2016, 31, 845. [Google Scholar] [CrossRef]
- Liebl, A.; Khunti, K.; Orozco-Beltran, D.; Yale, J.F. Health economic evaluation of type 2 diabetes mellitus: A clinical practice focused review. Clin. Med. Insights Endocrinol. Diabetes 2015, 8, 13–19. [Google Scholar] [CrossRef]
- Religioni, U.; Barrios-Rodríguez, R.; Requena, P.; Borowska, M.; Ostrowski, J. Enhancing Therapy Adherence: Impact on Clinical Outcomes, Healthcare Costs, and Patient Quality of Life. Medicina 2025, 61, 153. [Google Scholar] [CrossRef]
- Boehme, M.W.J.; Buechele, G.; Frankenhauser-Mannuss, J.; Mueller, J.; Lump, D.; Boehm, B.O.; Rothenbacher, D. Prevalence, incidence, and concomitant co-morbidities of type 2 diabetes mellitus in South Western Germany—A retrospective cohort and case-control study in claims data of a large statutory health insurance. BMC Public Health 2015, 15, 855. [Google Scholar] [CrossRef]
- Long, A.N.; Dagogo-Jack, S. Comorbidities of diabetes and hypertension: Mechanisms and approach to target organ protection. J. Clin. Hypertens. 2011, 13, 244–251. [Google Scholar] [CrossRef]
- Massi-Benedetti, M. The cost of diabetes Type II in Europe. The CODE-2 study: Preface. Diabetologia 2002, 45, S1–S4. [Google Scholar] [CrossRef]
- Stratton, I.M.; Adler, A.I.; Neil, H.A.W.; Matthews, D.R.; Manley, S.E.; Cull, C.A.; Hadden, D.; Turner, R.C.; Holman, R.R. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): Prospective observational study. Br. Med. J. 2000, 321, 405–412. [Google Scholar] [CrossRef]
- Zhang, P.; Zhang, X.; Brown, J.; Vistisen, D.; Sicree, R.; Shaw, J.; Nichols, G. Global healthcare expenditure on diabetes for 2010 and 2030. Diabetes Res. Clin. Pract. 2010, 87, 293–301. [Google Scholar] [CrossRef]
- Sharifa Ezat, W.P.; Azimatun, N.A.; Amrizal, M.N.; Saperi, B.S. Economic burden of diabetic care in Government Health Facilities in Selangor. J. Community Health 2009, 15, 17–26. Available online: https://journalarticle.ukm.my/273/1/1.pdf (accessed on 25 March 2025).
- Mustapha, F.I.; Azmi, S.; Manaf, M.R.A.; Hussein, Z.; Mahir, N.J.N.; Ismail, F.; Aizuddin, A.N.; Goh, A. What are the direct medical costs of managing type 2 diabetes mellitus in Malaysia? Med. J. Malays. 2017, 72, 271–277. Available online: https://www.e-mjm.org/2017/v72n5/medical-cost-of-diabetes.pdf (accessed on 25 March 2025).
- Pharmaceutical Services Program. Diabetes Medication Therapy Adherence Clinic Protocol, 3rd ed.; Pharmaceutical Services Program: Petaling Jaya, Malaysia, 2022. Available online: https://pharmacy.moh.gov.my/en/documents/diabetes-medication-therapy-adherence-clinic-protocol-third-edition-2022.html (accessed on 25 March 2025).
- Seidu, S.; Cos, X.; Brunton, S.; Harris, S.B.; Jansson, S.P.O.; Mata-Cases, M.; Neijens, A.M.J.; Topsever, P.; Khunti, K. 2022 update to the position statement by Primary Care Diabetes Europe: A disease state approach to the pharmacological management of type 2 diabetes in primary care. Prim. Care Diabetes 2022, 16, 223–244. [Google Scholar] [CrossRef]
- Iqbal, M.Z.; Alqahtani, S.S.; Mubarak, N.; Shahid, S.; Mohammed, R.; Mustafa, A.; Khan, A.H.; Iqbal, M.S. The influence of pharmacist-led collaborative care on clinical outcomes in type 2 diabetes mellitus: A multicenter randomized control trial. Front. Public Health 2024, 12, 1323102. [Google Scholar] [CrossRef]
- Butt, M.; Mhd Ali, A.; Bakry, M.M.; Mustafa, N. Impact of a pharmacist-led diabetes mellitus intervention on HbA1c, medication adherence, and quality of life: A randomized controlled study. Saudi Pharm. J. 2016, 24, 40–48. [Google Scholar] [CrossRef]
- Lim, P.C.; Lim, K.; Embee, Z.C.; Hassali, M.A.; Thiagarajan, A.; Khan, T.M. Study investigating the impact of pharmacist involvement on the outcomes of diabetes medication therapy adherence program Malaysia. Pak. J. Pharm. Sci. 2016, 29, 595–601. Available online: https://pubmed.ncbi.nlm.nih.gov/27087103/ (accessed on 25 March 2025).
- Jarab, A.S.; Alqudah, S.G.; Mukattash, T.L.; Shattat, G.; Al-Qirim, T. Randomized controlled trial of clinical pharmacy management of patients with type 2 diabetes in an outpatient diabetes clinic in Jordan. J. Manag. Care Pharm. 2012, 18, 516–526. [Google Scholar] [CrossRef]
- Phumipamorn, S.; Pongwecharak, J.; Soorapan, S.; Pattharachayakul, S. Effects of the pharmacist’s input on glycaemic control and cardiovascular risks in Muslim diabetes. Prim. Care Diabetes 2008, 2, 31–37. [Google Scholar] [CrossRef]
- Abdullah, M.J.; Tew, M.M.; Tan, P.H.; Koh, J.H.; Osman, N.M.; Chan, H.K. Pharmacist-managed Diabetes Clinic in Malaysia—Does the Number of Follow-up Visits Really Matter? J. Pharm. Pract. Community Med. 2018, 4, 55–59. [Google Scholar] [CrossRef]
- You, L.X.; Selvadurai, S.; Yee, C.K.; Noh, N.B.; Bao, G.; Joyce, T.; Hamdi, A. Impact of Pharmacist-Managed Diabetes Medication Therapy Adherence Clinic (DMTAC) in Government Health Clinics. Malays. J. Pharm. Sci. 2015, 13, 43–51. Available online: http://web.usm.my/mjps/mjps13012015/mjps13012015_4.pdf (accessed on 25 March 2025).
- Mehani, R.; Sharma, P. Cost variation analysis of oral anti-diabetic drugs. Int. J. Basic Clin. Pharmacol. 2018, 7, 1709. [Google Scholar] [CrossRef]
- Wang, Y.; Yeo, Q.Q.; Ko, Y. Economic evaluations of pharmacist-managed services in people with diabetes mellitus: A systematic review. Diabet. Med. 2016, 33, 421–427. [Google Scholar] [CrossRef]
- Dussa, K.; Parimalakrishnan, S.; Vishnuvardhanrao, M.; Sahay, R. Impact of pharmaceutical care on economic, clinical, and humanistic outcomes in type 2 diabetes mellitus patients. J. Chem. Pharm. Sci. 2017, 10, 29–38. Available online: https://jchps.com/specialissues/2017%20Special%20Issue%2010/6_333.pdf (accessed on 25 March 2025).
- Maeng, D.D.; Graham, J.; Bogart, M.; Hao, J.; Wright, E.A. Impact of a pharmacist-led diabetes management on outcomes, utilization, and cost. Clinicoecon. Outcomes Res. CEOR 2018, 10, 551–562. [Google Scholar] [CrossRef]
- Cranor, C.; Bunting, B.; Christensen, D. The Asheville Project: Long-term clinical and economic outcomes of a community pharmacy diabetes care program. J. Am. Pharm. Assoc. 2003, 43, 173–184. [Google Scholar] [CrossRef]
- Fox, D.; Ried, L.D.; Klein, G.E.; Myers, W.; Foli, K. A medication therapy management program’s impact on low-density lipoprotein cholesterol goal attainment in Medicare Part D patients with diabetes. J. Am. Pharm. Assoc. JAPhA 2009, 49, 192–199. [Google Scholar] [CrossRef] [PubMed]
- Romanelli, R.J.; Leahy, A.; Jukes, T.; Ishisaka, D.Y. Pharmacist-led medication management program within a patient-centered medical home. Am. J. Health-Syst. Pharm. 2015, 72, 453–459. [Google Scholar] [CrossRef]
| Variables | Frequency | p-Value | ||
|---|---|---|---|---|
| ** CG n (%) | ** IG n (%) | |||
| Hospital Name | 0.819 * | |||
| Hospital A | 71 (48.6) | 75 (51.4) | ||
| Hospital B | 70 (47.3) | 78 (52.7) | ||
| Gender | 0.136 * | |||
| Male | 74 (52.5) | 67 (47.5) | ||
| Female | 67 (43.8) | 86 (56.2) | ||
| Ethnicity | 0.400 * | |||
| Malay | 104 (46.0) | 122 (54.0) | ||
| Chinese | 25 (52.1) | 23 (47.9) | ||
| Indian | 12 (60.0) | 8 (40.0) | ||
| Age (mean, SD) | <0.001 # | |||
| - | 58.68 ± 6.08 N = 141 | 61.63 ± 6.17 N = 153 | ||
| Duration of diabetes (years, SD) | 0.032 # | |||
| - | 9.62 ± 2.35 | 10.24 ± 3.23 | ||
| Disease outcomes | ||||
| HbA1c (%) | 11.15 ± 1.33 | 11.68 ± 1.50 | 0.061 | |
| FBS (mmol/L) | 14.63 ± 1.38 | 14.44 ± 1.53 | 0.265 | |
| Residence status | 0.438 * | |||
| Urban | 66 (46.2) | 77 (53.8) | ||
| Rural | 75 (49.7) | 76 (50.3) | ||
| Employment status | 0.587 * | |||
| Unemployed | 67 (46.2) | 78 (53.8) | ||
| Employed | 74 (49.0) | 77 (51.0) | ||
| Type of daily diet | 0.328 * | |||
| Vegetarian | 79 (50.6) | 77 (49.4) | ||
| Non-vegetarian | 62 (44.9) | 76 (55.1) | ||
| Smoking status | 0.635 * | |||
| Yes | 26 (51.0) | 25 (49.0) | ||
| No | 115 (47.3) | 128 (52.7) | ||
| Exercise status | 0.178 * | |||
| Yes | 41 (54.7) | 34 (45.3) | ||
| No | 100 (45.7) | 119 (54.3) | ||
| Type of antidiabetic therapy | 0.882 * | |||
| Oral only | 82 (48.8) | 86 (51.2) | ||
| Insulin | 44 (47.8) | 48 (52.2) | ||
| Oral + insulin | 15 (44.1) | 19 (55.9) | ||
| Outcome Measure | Baseline | Follow-Up 1 (After 6 Months of Baseline) | Follow-Up 2 (After 1 Year of Baseline) | ||||
|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean Difference | p-Value α | Mean ± SD | Mean Difference | p-Value β | ||
| FBS (mmol/L) | 14.63 ± 1.37 | 12.09 ± 1.34 | −2.54 | <0.001 | 11.79 ± 1.33 | −0.30 | 0.067 |
| RBS (mmol/L) | 17.65 ± 1.34 | 15.93 ± 1.35 | −1.72 | <0.001 | 16.81 ± 1.39 | +0.88 | 0.347 |
| HbA1c (%) | 11.15 ± 1.32 | 10.10 ± 1.04 | −1.05 | <0.001 | 9.72 ± 1.02 | −0.38 | 0.003 |
| BP Systolic (mmHg) | 132.71 ± 6.09 | 131.63 ± 5.98 | −0.08 | 0.365 | 135.13 ± 5.99 | +0.58 | 0.276 |
| BP Diastolic (mmHg) | 84.37 ± 5.63 | 85.17 ± 5.05 | +0.80 | 0.455 | 84.24 ± 5.49 | −0.93 | 0.064 |
| Total Cholesterol (mmol/L) | 5.67 ± 0.35 | 5.43 ± 0.29 | −0.24 | 0.004 | 5.41 ± 0.30 | −0.002 | 0.457 |
| Triglyceride (mmol/L) | 1.88 ± 0.18 | 1.70 ± 0.14 | −0.18 | 0.001 | 1.76 ± 0.12 | −0.06 | 0.345 |
| LDL-C (mmol/L) | 2.81 ± 0.17 | 2.73 ± 0.12 | −0.08 | 0.352 | 2.74 ± 0.12 | +0.01 | 0.542 |
| HDL-C (mmol/L) | 1.04 ± 0.02 | 1.17 ± 0.03 | +0.13 | 0.001 | 1.16 ± 0.03 | −0.01 | 0.067 |
| Outcome Measure | Baseline | Follow-Up 1 (After 6 Months of Baseline) | Follow-Up 2 (After 6 Months of 1st Follow-Up) | ||||
|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean Difference | p-Value α | Mean ± SD | Mean Difference | p-Value β | ||
| FBS (mmol/L) | 14.44 ± 1.53 | 10.01 ± 1.51 | −4.43 | <0.001 | 7.63 ± 1.45 | −2.38 | <0.001 |
| RBS (mmol/L) | 18.32 ± 1.48 | 13.87 ± 1.45 | −4.45 | <0.001 | 11.54 ± 1.39 | −2.33 | <0.001 |
| HbA1c (%) | 11.69 ± 1.50 | 9.94 ± 0.92 | −1.75 | <0.001 | 8.87 ± 0.79 | −1.07 | <0.001 |
| BP Systolic (mmHg) | 136.87 ± 5.60 | 131.27 ± 5.49 | −5.60 | <0.001 | 129.97 ± 5.31 | −1.30 | <0.001 |
| BP Diastolic (mmHg) | 85.49 ± 5.94 | 83.45 ± 5.87 | −2.04 | 0.001 | 81.31 ± 5.05 | −2.14 | 0.001 |
| Total Cholesterol (mmol/L) | 6.16 ± 0.35 | 5.41 ± 0.32 | −0.75 | <0.001 | 5.34 ± 0.0.29 | −0.07 | 0.067 |
| Triglyceride (mmol/L) | 1.97 ± 0.22 | 1.82 ± 0.22 | −0.15 | 0.001 | 1.71 ± 0.14 | −0.11 | 0.003 |
| LDL-C (mmol/L) | 3.45 ± 0.20 | 3.01 ± 0.35 | −0.44 | <0.001 | 2.72 ± 0.10 | −0.29 | <0.001 |
| HDL-C (mmol/L) | 0.91 ± 0.04 | 1.01 ± 0.10 | +0.1 | 0.001 | 1.02 ± 0.11 | +0.01 | 0.568 |
| Parameters | Cost in MYR for 3 Months Mean ± SD ** CG (N = 143) | Cost in MYR for 3 Months Mean ± SD ** IG (N = 156) | t-Statistic (df) | p-Value |
|---|---|---|---|---|
| Insulin | 763.90 ± 140.74 | 783.01 ± 149.67 | −1.13 (1, 297) | 0.258 |
| Oral antidiabetics | 48.71 ± 6.52 | 48.75 ± 6.94 | −0.04 (1, 297) | 0.963 |
| Diabetic comorbidities | 78.80 ± 7.55 | 78.88 ± 2.97 | 0.91 (1, 297) | 0.908 |
| Diabetic complications | 350.21 ± 21.57 | 347.49 ± 19.58 | 1.14 (1, 297) | 0.253 |
| Multivitamins and minerals | 15.85 ± 4.20 | 15.25 ± 3.22 | 1.38 (1, 297) | 0.167 |
| NSAIDs | 2.68 ± 0.73 | 2.59 ± 0.55 | 1.25 (1, 297) | 0.211 |
| Other medications | 22.86 ± 5.09 | 22.10 ± 3.96 | 1.44 (1, 297) | 0.150 |
| Parameters | Cost for 3 Months Mean ± SD CG (N = 143) | Difference from Baseline Price | Cost for 3 Months Mean ± SD IG (N = 156) | Difference from Baseline Price | t-Statistic (df) | p-Value |
|---|---|---|---|---|---|---|
| Insulin | RM 874.43 ± 218.33 | RM +110.53 | RM 816.40 ± 163.91 | RM +33.39 | 2.61 (1, 297) | 0.009 |
| Oral antidiabetics | RM 65.74 ± 35.50 | RM +17.03 | RM 51.53 ± 12.68 | RM +2.78 | 4.68 (1, 297) | <0.001 |
| Diabetic comorbidities | RM 81.79 ± 8.91 | RM +2.99 | RM 80.16 ± 5.73 | RM +1.28 | 1.88 (1, 297) | 0.060 |
| Diabetic complications | RM 361.32 ± 32.13 | RM +11.11 | RM 350.40 ± 23.59 | RM +2.91 | 3.36 (1, 297) | 0.001 |
| Multivitamins and minerals | RM 16.80 ± 4.60 | RM +0.95 | RM 15.38 ± 3.32 | RM +0.13 | 3.06 (1, 297) | 0.002 |
| NSAIDs | RM 2.85 ± 0.79 | RM +0.17 | RM 2.32 ± 0.75 | RM −0.27 | 5.91 (1, 297) | <0.001 |
| Other medications | RM 24.34 ± 6.11 | RM +1.48 | RM 21.15 ± 4.23 | RM −0.95 | 5.27 (1, 297) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iqbal, M.Z.; Alqahtani, S.S.; Shahid, S.; Orayj, K.M. Impact of Pharmacist Educational Intervention on Costs of Medication with Improved Clinical Outcomes for Diabetic Patients in Various Tertiary Care Hospitals in Malaysia: A Randomized Controlled Trial. Healthcare 2025, 13, 901. https://doi.org/10.3390/healthcare13080901
Iqbal MZ, Alqahtani SS, Shahid S, Orayj KM. Impact of Pharmacist Educational Intervention on Costs of Medication with Improved Clinical Outcomes for Diabetic Patients in Various Tertiary Care Hospitals in Malaysia: A Randomized Controlled Trial. Healthcare. 2025; 13(8):901. https://doi.org/10.3390/healthcare13080901
Chicago/Turabian StyleIqbal, Muhammad Zahid, Saad S. Alqahtani, Sara Shahid, and Khalid M. Orayj. 2025. "Impact of Pharmacist Educational Intervention on Costs of Medication with Improved Clinical Outcomes for Diabetic Patients in Various Tertiary Care Hospitals in Malaysia: A Randomized Controlled Trial" Healthcare 13, no. 8: 901. https://doi.org/10.3390/healthcare13080901
APA StyleIqbal, M. Z., Alqahtani, S. S., Shahid, S., & Orayj, K. M. (2025). Impact of Pharmacist Educational Intervention on Costs of Medication with Improved Clinical Outcomes for Diabetic Patients in Various Tertiary Care Hospitals in Malaysia: A Randomized Controlled Trial. Healthcare, 13(8), 901. https://doi.org/10.3390/healthcare13080901






