Disempowered Warriors: Insights on Psychological Responses of ICU Patients Through a Meta-Ethnography
Abstract
1. Introduction
Objective
2. Methods
2.1. Eligibility Criteria
2.2. Information Sources and Search Strategy
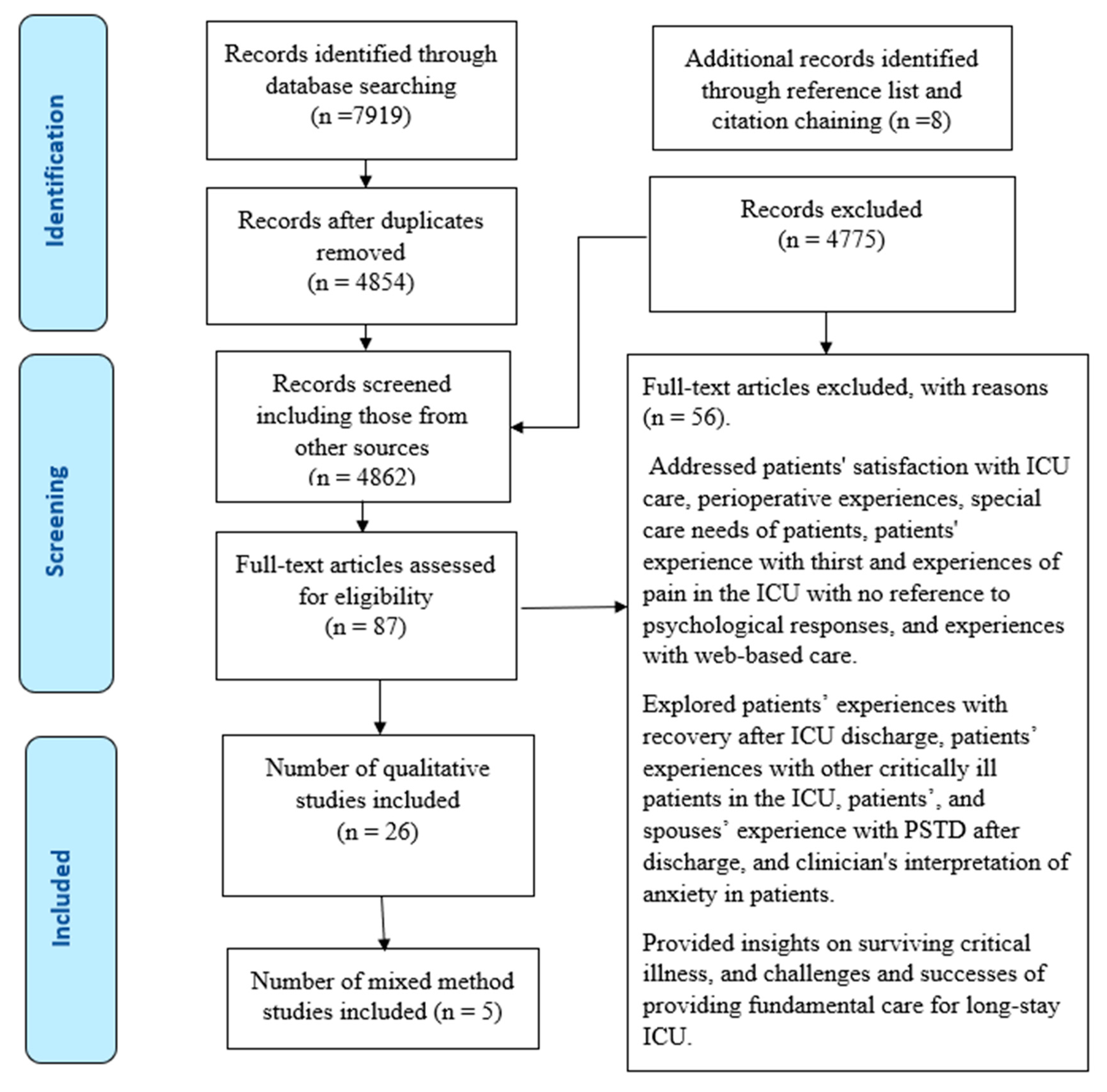
2.3. Selection of Sources of Evidence and Data Charting
2.4. Quality Assessment
2.5. Data Extraction and Analysis
3. Results
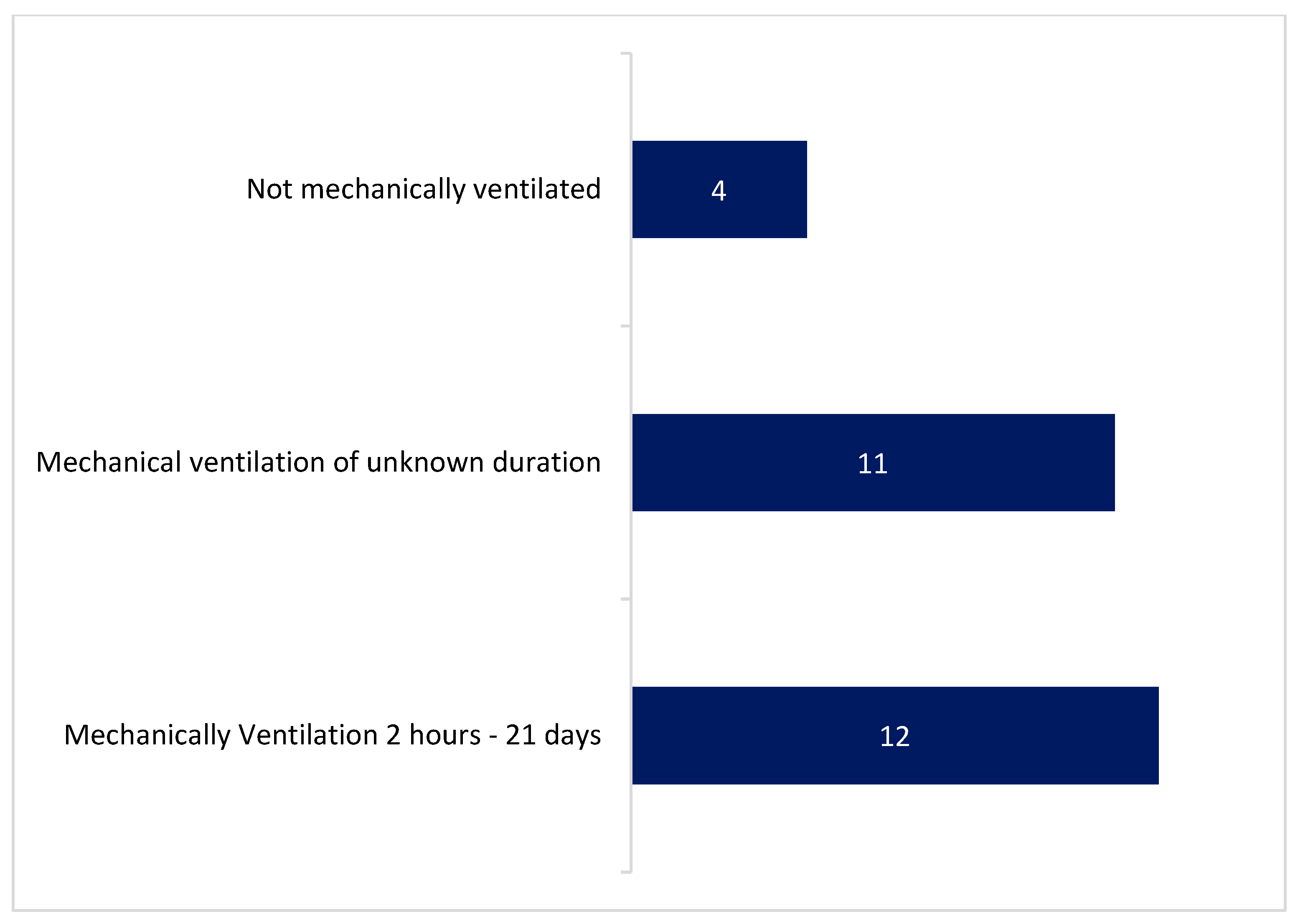
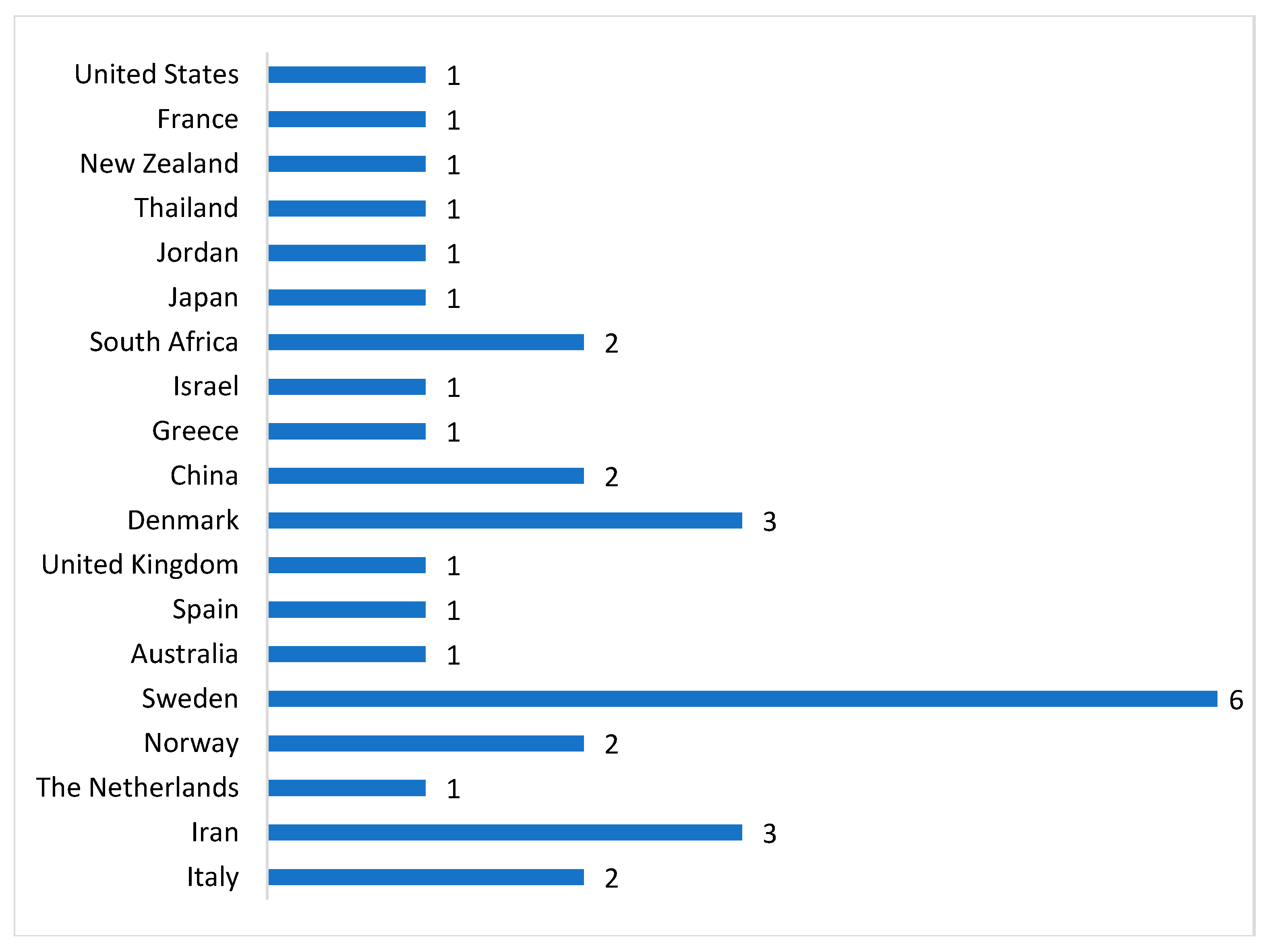
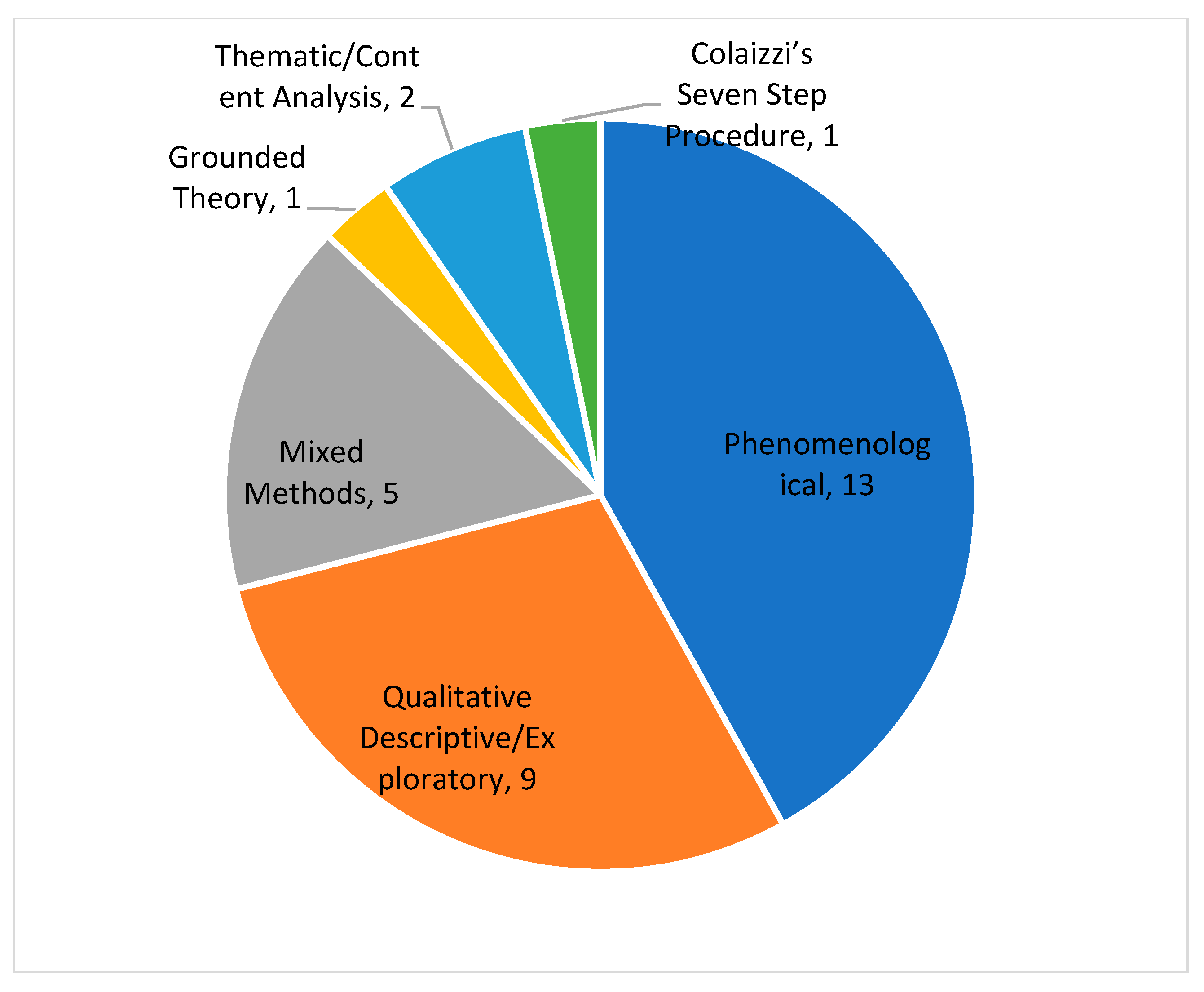
3.1. Study and Participants’ Characteristics
3.2. Quality Appraisal
3.3. Experiences of the Participants in the Reviewed Studies
The Disempowered Warrior
Disempowerment
Altered Self-Identity
Fighting
Torment
- Trauma
- Fear of Death
Hostile Environment
| Authors and Country | Aim | Sample Characteristics | Themes |
|---|---|---|---|
| Adeyemi (2016) [19] South Africa | To explore and describe the experiences of patients on mechanical ventilation in the intensive care unit of one public sector hospital in Johannesburg. | Female = 4, male = 6. Age = 39–48 years. Average length of stay in ICU (LOS): 4.9 days. Cognitive status: not reported. Mean duration on mechanical ventilation = 57.45 h. Sedation status: all patients were sedated. |
|
| Albanesi et al. (2020) [12] Italy | To describe the lived experiences of patients who underwent cardiac surgery. | Female = 9, male = 2. Age = 42–75 years. Cognitive status: consciousness. Ventilation status: not reported Sedation status: One patient described being on sedation. |
“not understanding time”
|
| Alpers et al., (2012) [43] Norway | To gain knowledge on what factors contribute to inner strength in critically ill patients cared for in an intensive care unit. | Female= 3, male =3. Age = 60–72. Ventilation and sedation status not reported. |
|
| Ashkenazy et al., (2021) [38] Israel | To describe mechanically ventilated ICU patients’ perception of discomfort and how they differentiate discomfort from pain. | 1 males, 3 females. Age 19–81 years. Ventilated for 2–8 days. LOS 3–20 days. Participants were fully conscious, oriented, and able to articulate their ICU experience. Most interviews were conducted 3–8 days post ICU discharge. |
|
| Aslani et al., (2017) [20] Iran | To explore the psychological experiences of patients under mechanical ventilation following an open-heart surgery in 2016. | Female = 8, male = 7. age range = 40–60. Cognitive status: not reported. All patients had received ventilation. Sedation status: all patients were sedated. |
|
| Engström et al. (2012) [21] Sweden | To describe the intensive care unit experiences of people undergoing mechanical ventilation. | Female = 4, male = 4. Age = 45 to 72 years. Ventilation status: 5–21 days. Sedation status: all patients were sedated. Duration on sedation not specified. |
|
| Eqylan et al., (2022) [39] Jordan | To explore critically ill Muslim patients’ experiences and perceptions related to confinement to isolation rooms in Jordan. | 5 male and 5 female. Mean age: 42.2 ± 17.3 years. Mean duration of isolation stay: 6.6 ± 2.2 days. Included only patients not ventilated or sedated. |
|
| Flahault et al., (2021) [30] France | To capture the intimate experience of ICU patients, to understand how they make sense of this experience, and to explore their experience and representations of an ICU diary. | 3 men and 2 women. Age: 24–72 years. LOS: 8–13 days. Duration of mechanical ventilation: 4–9 days. Patients experienced delirium and hallucinations during admission. |
|
| Foster et al., (2010) [22] United Kingdom | To describe the experience of having a tracheostomy tube as lived by a group of people who had this tube inserted as a part of their critical illness or as a procedure. | Female = 1, male = 2. LOS ≥ 14 days. Cognitive and mechanical ventilation status not reported. |
|
| Gilder et al., (2021) [23] New Zealand | To describe the patient experience of the endotracheal tube and suction, following mechanical ventilation in post-operative cardiac surgical patients. | Eight male, two female. Age: 26–84, mean= 64.1 years. LOS: mean = 24.5 h, range= 17–72 h. Duration of mechanical ventilation: mean = 6.3 h range = 4.1–17.4 h. |
|
| Herbst and Drenth, (2012) [32] South Africa | To increase insight into the thoughts, feelings, and bio-psychosocial needs of the patient receiving treatment in the ICU. | Single participant 27 years old female. Participant regained consciousness. after three weeks in the ICU. Ventilated and sedated but number of days involved not reported. LOS: not reported. |
|
| Hofhius et al., (2008) [36] The Netherlands. | To evaluate the perceptions of patients regarding nursing care in the ICU, and secondly, to explore patients’ perceptions and experiences of their ICU stay. | Female= 4, male =7. Age = 54–73 years. Ventilation status: 4–20 days. Sedation status: all patients were sedated. |
|
| Karlsson et al., (2011) [25] Sweden | To illuminate the lived experience of patients who were conscious during mechanical ventilation in an intensive care unit (ICU). | Female = 3, male = 9. Age = 23–88 years. LOS = 2–23 days. Ventilation status: All patients were ventilated. Number of days on ventilation not stated. Motor activity assessment scale = 3–4. Cognitive status: not reported. Sedation status: no patient was under sedation during interview. |
|
| Locsin and Kongsuwan, (2013) [24] Thailand | The purpose of this study was to describe the meaning of the experiences of patients who were dependent on technologies while being cared for in ICUs. | 7 male, 3 female. Age: mean = 43.9 years, range = 22–76 years. LOS: mean = 50.8, range = 2 days–3 months. Ventilation status: patients were ventilated but number of days on ventilation noted reported. |
|
| McKinley et al., (2002) [26] Australia | To gain an understanding of the experience of being a seriously ill patient in an (ICU). | 8 males, 6 females. Aged 17–71. LOS: 3–53 days. Ventilation status: not reported. |
|
| Mortensen et al., (2023) [31] Denmark | To explore everyday life experiences of critically ill patients with delirium during the ICU stay, from ICU discharge until 1-year follow-up, focusing on their health-related quality of life and cognitive function. | 9 women and 8 men. Age: median = 69 years, range = 57–73.5. LOS: median= 8, IQR = 5.5–26.5. Ventilation status: not reported. |
|
| Mylén et al., (2016) [41] Sweden | To explore the lived experiences of conscious patients in neurosurgical intensive care. | Female = 7, male = 4. Age range = 37–81. LOS = 5–15 days. Cognitive status: GSC 14—15. Ventilation status: no patients were ventilated. |
|
| Olausson et al., (2013) [37] Sweden | To reveal the meanings of the ICU settings as a place of care. | Female = 5, male = 4. Age range = 38–52. LOS = 5–90 days. Ventilation status: not reported. sedation status: not reported. |
|
| Olsen et al., (2017) [35] Norway | To investigate how adult ICU patients experienced the ICU stay, their recovery period, and the usefulness of the pamphlet. | Female = 10, male = 19. Age range = 20–80. Ventilation status: ventilated for ≥ 48. Sedation status: all patients were sedated. |
|
| Pakmehr et al., (2017) [42] Iran | To phenomenologically explore the intubated patients’ lived experiences of ICU care. | Female = 7, male = 5. Age = 19–48. Ventilation = 2–50 days. Sedation status: not reported. |
|
| Roberts et al., (2019) [34] United States | To determine the pervasive patient experience components and how the experience may have been influenced by targeted, light sedation practices. | Female = 5, male = 10. Average age = 61.8 Ventilation status: for less than 14 days. Average LOS = 3.5 days. Sedation status: Richmond agitation Sedation scale score = 1.7. |
|
| Rodriguez-Almagro et al., (2019) [27] Spain | To explore the perceptions about the experiences of patients in the ICU, their family members, and the nurses who attend them. | Female = 4, male = 5. Age = 22–67. Cognitive status: not reported. ventilation status: not reported. |
|
| Samuelson et al., (2011) [40] Sweden | To describe unpleasant and pleasant memories of the ICU stay in adult mechanically ventilated patients. | Female = 122, male = 128. Age = 63.4 ± 13.8. Cognitive status: no confusion, delirium. Median LOS = 3.4. Ventilation status: more than 24 h. Sedation status: not reported. |
|
| Sanson et al., (2021) [33] Italy | To explore the experiences of being cared for in an intensive care unit (ICU) through patients’ memories. | Female 42; male 58. Age: 66 (53–77) years. Glasgow Coma Scale: 13 (10–15). Duration of ventilation: 23.5 h (2–67). LOS: 69 h (40–141). |
|
| Schou and Egerod, (2009) [28] Denmark | To provide a contemporary description of the patient experience of weaning. | Female = 2, male = 8. Age range = 35–84. Cognitive status: not reported. Ventilation status: ≥24 h. |
|
| Takashima et al., (2018) [1] Japan | To clarify the stress experiences of patients mechanically ventilated in an intensive care unit (ICU) for more than 12 h. | 22 women and 74 men. Average age = 69.4± 11.5. Average duration of intubation: 54.7 ± 60.0 hr. Average LOS: 6.8 ± 5.9 days. |
|
| Tavakoli et al., (2022) [2] Iran | To study the experiences of discomfort and self-management strategies in patients admitted to the ICU. | 5 females and 8 males. Age range = 17–61 years. LOS: not reported. Ventilation status: not reported. Cognitive status: conscious for at least 72 h after admission to the ICU. |
|
| Vogel et al., (2021) [44] Sweden | To explore patients’ patterns of behaviour during the process from becoming critically ill to recovery at home. | 4 men and 9 women. Age = 22–82 years. LOS = 2–28 days. Ventilation status: not reported. |
|
| Wang et al., (2009) [29] China | To understand patients’ intensive care experience while receiving mechanical ventilation in intensive care units. | Female = 3, male = 8. Age = 33–78 years. Mean LOS= 174.6 h. Cognitive status: not reported. Mean length of mechanical ventilation = 107.3 h. Sedation status: all patients were sedated. |
|
| Yahui et al., (2022) [45] China | To explore the experience of ICU patients and their relatives and to investigate their daily needs within the closed management system in many Chinese ICUs. | 6 male and 9 female. Mean age: 59.60 ± 17.33, range = 28~88 years. Cognitive status: able to communicate verbally. LOS: at least 72 h. Ventilation status: not reported. |
|
| Zisopoulos et al., (2022) [3] Greece | To describe how participants describe their ICU experiences and make sense of their experience. | 17 males, 9 females. Age = 20–68 years. LOS = 2 weeks. Ventilation status: not recorded. Cognitive status: unclear. |
|
| Included Studies | Was There a Clear Statement of the Aims of the Research? | Is a Qualitative Methodology Appropriate? | Was the Research Design Appropriate to Address the Aims of the Research? | Was Recruitment Strategy Appropriate to the Aims | Were Data Collected in a Way that Addressed the Research Issue? | Has the Relationship Between Researcher and Participants Been Adequately Considered | Have Ethical Issues been Taken into Consideration? | Were the Data Analysis Sufficiently Rigorous? | Is There a Clear Statement of Findings? | How Valuable Is the Research? | Overall Risk of Bias Assessment |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Albanesi et al. 2020 [12] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Greatly | low |
| Ashkenazy et al. 2021 [38] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Greatly | low |
| Aslani et al., 2017 [20] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Moderately | moderate |
| Hofhuis et al., 2008 [36] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Moderately | moderate |
| Olsen et al., 2017 [35] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Moderately | moderate |
| Rodriguez-Almagro et al., 2019 [27] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Greatly | low |
| Alpers et al., 2012 [43] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Cannot tell | Yes | Moderately | moderate |
| Engström et al. 2012 [21] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Moderately | moderate |
| Samuelson et al. 2011 [40] | Yes | Cannot tell | Yes | No | No | No | Yes | Cannot tell | Yes | Moderately | moderate |
| Karlsson et al., 2011 [25] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Greatly | low |
| Wang et al., 2009 [29] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Moderately | low |
| Olausson et al., 2013 [37] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Moderately | moderate |
| McKinley et al., 2002 [26] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Greatly | low |
| Adeyemi, 2016 [19] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Greatly | low |
| Pakmehr et al., 2017 [42] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Moderately | moderate |
| Roberts et al., 2019 [34] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Greatly | low |
| Schou and Egerod, 2009 [28] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Moderately | low |
| Foster, 2009 [22] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Greatly | low |
| Mylen et al. 2015 [41] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Moderately | moderate |
| Vogel et al., 2021 [44] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Moderately | moderate |
| Tavakoli et al., 2022 [2] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Greatly | low |
| Zisopulos et al. 2022 [3] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Greatly | low |
| Locsin and Kongsuwan, 2013 [24] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Greatly | low |
| Herbst and Drenth, 2012 [32] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Moderately | moderate |
| Mortensen et al. 2023 [31] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Greatly | low |
| Flahault et al., 2021 [30] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Greatly | low |
| Gilder et al., 2022 [23] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Greatly | low |
| Sanson et al. 2021 [33] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Greatly | low |
| Eqylan et al., 2022 [39] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Greatly | low |
| Yahui et al., 2022 [45] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Greatly | low |
| Participant Quotes | Main Theme |
|---|---|
| “…I couldn’t get to sleep once, but that battle Axe [nurse] said I had” [25]. “You want to be treated as an adult instead of a child, right?” [36] “Yes, I mean I’m not an engine that needs to be fixed, I mean, I’m a human being” [36] “you know, not giving …updates … you just struggle. You feel so helpless, and you wonder if you are going to die” [34] “we were lying on bed like vegetables, it seemed that we did not exist to the nurses, they were chatting and laughing, too noisy” [29] “There were moments when [patients] almost cried in despair. [They were] suffering and [care practitioners] laugh[ed] at the top of their lungs a few meters away” [33] “You… [ring] the bell and no one shows up. […] It made me feel helpless, and powerless. … what can I say, you feel hurt and you could easily start to cry.” [36] “someone pressed my arms and legs forcefully, some others opened my mouth and put something into my throat, after that I knew that was the tracheal tube, why did nobody tell me about it before that?” [29] | Disempowerment |
| “Weak in [the] body……[some] felt like a child, … who doesn’t think too much, can’t do anything; can’t pee by…self, poo by …self, can’t do anything” [25] “like a vegetable… very defenseless and helpless” [40] “when I woke up from the coma the only thing that I confronted was fear, i.e., if I would be able to speak again because of the tracheotomy and if I would be able to walk again because I was confined in my bed…” [3] “felt strange… like there was a gap between [the] body and mind” [1] “It felt like my upper body was like an elephant, I didn’t expect my legs could carry me” [41] “I didn’t know what they were doing to me…I was a body, there, available” [33] | Altered self-identity: altered self perception, self-image and self competency |
| “Being in the ICU is just like a little child who could not swim [and] was thrown into a cold swimming pool [29] “You become very anxious, it is like you are fighting for your life, … you are just getting instructions push, breath or whatever…” [19] “I am sure that they want to hurt me and nobody explains to me what has happened. The only thing that they cared about is my coughing.” [3] “when a patient becomes ill, the ward falls apart, all the doctors and nurses are gone [leaving other patients] subconsciously restless and upset” [2] | Fighting |
| “Like a prisoner with tied hands and feet and closed mouth who is continually punctured with needles and cannot say anything” [42] “you do not see anyone, all in bed [with] a series of devices …connected to [them that] make noise” [2] “You [can] not move because of the tubes... you are attached to the bed” [38] “Since you are intubated, they passed it through the nose and the nose got sore. When the sore was recovering, they pulled it out and inserted [nasogastric tube] again into the nose. Doing this, they pressed the injured sore which made more pain” [42] “It was one of those things that you have to kind of grin and bear it” [34] | Torment |
| “to be honest, everyone who wakes up and does not know where he is and once sees all these devices hooked to him and cannot do anything, is definitely going to have another MI [myocardial infarction] from fear” [20] “Today, the doctor comes and says that the operation was very good, you will get up soon and you will not have any special complications. Tomorrow another doctor will come and say that it is too early for me to comment. Maybe you will have a series of complications after the operation!” [2] “There is a lot of can’t… you can’t do …so all of these accumulate to a bad experience” [19] “From the moment you woke up you wanted to get out, to flee, you don’t want to stay even a minute longer” [3] | Trauma |
| “I was very scared when I realized I was in the ICU. I told myself I was done!” [2] “when I woke up I found a tube in my throat, […] I could not stop thinking: Was I dying soon?” [29] “We were four and I was the only one left. Three died, and I saw them die… It was not easy holding on to the bed waiting for your moment to come” [20,33,37] “I have no fear of dying, but always of being in pain and suffering… the same pain, I would like to die instead. … I thought that if (I) didn’t die soon, it would be pitiful [24] I was in fear. I didn’t want to take my eyes off from the monitors…When the machine alarmed, I was frightened. Why did it alarm? What was happening with me?” [24] “I kept thinking of this: What should I do if there was anything wrong in the machine without someone knowing? Was that my last day of life?” [29] “I was scared because I thought the night nurse will kill me…so I yelled at her…” [31] | Fear of death |
| “for almost the entire [time], all the lights were on, there was no window, no clock, and [patients] didn’t have a sense of time” [3] “can hear all of it… it’s hard to explain but if you can’t sleep, can’t shut yourself down so to speak, and being afraid of all that may happen makes you scared. Yes all that makes you feel… I can’t hang on anymore” [36] “I did not know what is going on, I woke up, I felt a tube, I thought maybe I will pull a little bit, suddenly I saw the tube halfway out, so I took it out” [38] “when a patient becomes ill, the ward falls apart, all the doctors and nurses are gone [leaving other patients] subconsciously restless and upset” [2] “This thing that I put my wrist (referring to manometer connected to an arterial line) makes me both annoyed and afraid to make the slightest moan, because I think it will break and be dangerous for me!” [33] “an artificial environment, inappropriate to the human being, [and] not compatible with human expectations” [33] | Hostile environment |
4. Discussion
5. Practical Implications for Nursing and Healthcare Team
- Enhancing Patient-Centered CareNurses and healthcare professionals must prioritize patient autonomy and dignity, even in case of patients with impaired consciousness. This can be achieved through shared decision-making with patients and families, ensuring that care aligns with the patient’s values and preferences. Clear communications can help to mitigate feelings of powerlessness and perceived violations of autonomy. Moreover, empowering patients by involving them in their care/treatment pathways—whenever possible—can support their sense of control and mitigates feelings of helplessness.
- Integrating Psychological and Emotional Support into ICU CultureAddressing the psychological distress of ICU patients requires a fundamental shift in ICU culture, where emotional well-being is prioritized alongside implementing care routines for survival. Nurses should implement trauma-informed care strategies, therapeutic communication, and environmental modifications to foster a sense of safety and reduce perceptions of the ICU as a hostile or traumatic space. Routine psychological assessments should be incorporated into patient care, and healthcare teams should receive regular training in patient-centered communication and psychological resilience to ensure that ICU practices minimize distress and promote holistic well-being.
- Integrating Family for Emotional SupportEngaging family members as active participants in care can provide patients with a crucial sense of familiarity and reassurance, thereby alleviating psychological distress. For conscious patients, structured family interactions can help maintain emotional connections and enhance their sense of security. For unconscious patients, the presence of family members, along with verbal and non-verbal communication strategies, may contribute to emotional well-being and aid in recovery. Healthcare professionals should facilitate family engagement through flexible visitation policies and psychosocial support programs.
6. Limitations
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| SN | Search Strategy | Results |
|---|---|---|
| S1 | (MH “Intensive Care Units”) OR (MH “Coronary Care Units”) OR (MH “Post Anesthesia Care Units”) OR (MH “Respiratory Care Units”) OR (MH “Stroke Units”) | 44,040 |
| S2 | (MH “Critical Care”) | 23,517 |
| S3 | (MH “Critical Illness”) OR (MH “Critically Ill Patients”) | 25,309 |
| S4 | (“intensive care” or “critical care” or “critical* ill*” or “medical crisis” or ICU or ICUs or CCU or CCUs) | 155,015 |
| S5 | (MH “Respiration, Artificial + ”) | 34,536 |
| S6 | ((mechanic* or artificial* or assisted) N2 (ventilat* or respirat* or breath*)) | 42,132 |
| S7 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 | 191,298 |
| S8 | (MH “Stress, Psychological”) OR (MH “Reality Shock”) | 51,666 |
| S9 | (MH “Psychological Distress”) | 859 |
| S10 | (MH “Anxiety”) | 45,277 |
| S11 | (MH “Fear”) OR (MH “Suffering”) OR (MH “Worry”) OR (MH “Hopelessness”) | 17,461 |
| S12 | ((emotion* or psychologic* or mental*) N2 (stress* or pressure* or tension* or distress* or strain* or pain* or suffer* or trauma*)) | 163,910 |
| S13 | (anxiet* or anxious* or fear* or worry or worries or worrisome or panic*) | 145,937 |
| S14 | (MH “Stress Disorders, Post-Traumatic”) | 23,172 |
| S15 | (MH “Psychological Trauma”) | 1483 |
| S16 | (“stress disorder*” or PTSD) | 28,535 |
| S17 | S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 | 289,779 |
| S18 | qualitative OR ethnol* OR ethnog* OR ethnonurs* OR emic OR etic OR leininger OR noblit OR “field note*” OR “field record*” OR fieldnote* OR “field stud*” or “participant observ*” OR “participant observation*” OR hermaneutic* OR phenomenolog* OR “lived experience*” OR heidegger* OR husserl* OR “merleau-pont*” OR colaizzi OR giorgi OR ricoeur OR spiegelberg OR “van kaam” OR “van manen” OR “grounded theory” OR “constant compar*” OR “theoretical sampl*” OR glaser AND strauss OR “content analy*” OR “thematic analy*” OR narrative* OR “unstructured categor*” OR “structured categor*” OR “unstructured interview*” OR “semi-structured interview*” OR “maximum variation*” OR snowball OR audio* OR tape* OR video* OR metasynthes* OR “meta-synthes*” OR metasummar* OR “meta-summar*” OR metastud* OR “meta-stud*” OR “meta-ethnograph*” OR metaethnog* OR “meta-narrative*” OR metanarrat* OR “ meta-interpretation*” OR metainterpret* OR “qualitative meta-analy*” OR “qualitative metaanaly*” OR “qualitative metanaly*” OR “purposive sampl*” OR “action research” OR “focus group*” or photovoice or “photo voice” or “mixed method*” | 477,497 |
| S19 | S7 AND S17 AND S18 | 1839 |
| S20 | TI (PICU or NICU or “p?ediatric intensive care” or “neonatal intensive care”) | 7060 |
| S21 | S19 NOT S20 | 1666 |
| SN | Search Strategy | Results |
|---|---|---|
| 1. | exp intensive care units/ | 87,213 |
| 2. | Critical care/ | 53,383 |
| 3. | Critical illness/ | 264,863 |
| 4. | (“intensive care” or “critical care” or “critical* ill*” or “medical crisis” or ICU or ICUs or CCU or CCUs).mp. | 49,929 |
| 5. | Respiration, artificial/ | 49,929 |
| 6. | ((mechanic* or artificial* or assisted) adj2 (ventilat* or respirat* or breath*)).mp. | 110,073 |
| 7. | or/1–6 | 346,966 |
| 8. | Stress, psychological/ | 122,600 |
| 9. | Psychological Distress/ | 1126 |
| 10. | Anxiety/ | 83,550 |
| 11. | exp Fear/ | 33,719 |
| 12. | ((emotion* or psychologic* or mental*) adj2 (stress* or pressure* or tension* or distress* or strain* or pain* or suffer* or trauma*)).mp. | 165,424 |
| 13. | (anxiet* or anxious* or fear* or worry or worries or worrisome or panic*).mp. | 348,181 |
| 14. | stress disorders, traumatic/ or psychological trauma/ or stress disorders, post-traumatic/ or stress disorders, traumatic, acute/ | 35,336 |
| 15. | (“stress disorder*” or PTSD).mp. | 51,114 |
| 16. | or/8–15 | 511,111 |
| 17. | 7 and 16 | 7725 |
| 18. | exp qualitative research/ or grounded theory/ | 59,926 |
| 19. | exp Nursing Methodology Research/ | 16,381 |
| 20. | anthropology, cultural/ | 6566 |
| 21. | exp focus groups/ | 30,959 |
| 22. | qualitative.mp. | 259,782 |
| 23. | (ethnol$ or ethnog$ or ethnonurs$ or emic or etic).mp. | 177,175 |
| 24. | (leininger$ or noblit).mp. or hare.ti,ab. | 2632 |
| 25. | (field note$ or field record$ or fieldnote$ or field stud$).mp. | 18,878 |
| 26. | (participant$ adj3 observ$).mp. | 11,699 |
| 27. | (nonparticipant$ adj3 observ$).mp. | 161 |
| 28. | (non participant$ adj3 observ$).mp. | 676 |
| 29. | (hermeneutic$ or phenomenolog$ or lived experience$).mp. | 33,448 |
| 30. | (heidegger$ or husserl$ or merleau-pont$).mp. | 1112 |
| 31. | (colaizzi$ or giorgi$).mp. | 1495 |
| 32. | (ricoeur or spiegelberg$).mp. | 316 |
| 33. | (van kaam$ or van manen).mp. | 204 |
| 34. | (Grounded adj5 theor$).mp. | 13,927 |
| 35. | (constant compar$ or theoretical sampl$ or triangulat$).ti,ab. | 12,219 |
| 36. | (glaser and strauss).mp. | 110 |
| 37. | ((content or theme* or thematic or narrative or discourse) adj2 analys*).mp. [mp = title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, organism supplementary concept word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms] | 61,760 |
| 38. | (unstructured categor$ or structured categor$).mp.21 | |
| 39. | (unstructured interview$ or semi-structured interview$ or semistructured interview$).mp. | 45,122 |
| 40. | (maximum variation or snowball).mp. | 3845 |
| 41. | (audiorecord$ or taperecord$ or videorecord$ or videotap$).mp. | 21,203 |
| 42. | ((audio or tape or video$) adj5 record$).mp. | 62,580 |
| 43. | ((audio$ or video$ or tape$) adj5 interview$).mp. | 9764 |
| 44. | (metasynthes$ or meta-synthes$ or metasummar$ or meta-summar$ or metastud$ or meta-stud$).ti,ab. | 1548 |
| 45. | (meta-ethnog$ or metaethnog$ or meta-narrat$ or metanarrat$ or meta-interpret$ or metainterpret$).mp. | 837 |
| 46. | (qualitative adj5 meta-analy$).mp. | 640 |
| 47. | (qualitative adj5 metaanaly$).mp. | 3 |
| 48. | purposive sampl$.mp. | 8287 |
| 49. | action research.mp. | 4423 |
| 50. | focus group$.mp. | 54,612 |
| 51. | exp interview/ or exp interviews as topic/ or narration/ | 101,155 |
| 52. | ((audio* or video* or tape* or record*) and (interview* or transcri* or theme* or thematic)).mp. | 70,943 |
| 53. | experience*.ti. and (audio* or video* or tape* or record*).mp. and px.fs. | 3174 |
| 54. | ((interview* or audio* or video* or record*) and (views or perception* or belief* or attitude* or perspective*)).mp. | 206,632 |
| 55. | (photo voice or photovoice or mixed method*).mp. | 25,221 |
| 56. | or/18–55 | 827,158 |
| 57. | (mixed method* or multi-method* or multiple research method* or multiple method* or multimethod* or mixed model* or mixed research).tw. | 54,994 |
| 58. | ((qualitative or qual) and (quantitative or quan) and (nested or blend* or concurrent or complementary or expansion or initiation or holistic or transformative or embedded or iterative or triangulat*)).tw. | 5795 |
| 59. | ((quantitative or quan) and (phenomenolog* or ethno* or (grounded adj3 theor*) or hermeneutic* or lived experience* or content analys* or thematic or theme* or narrative* or interview* or focus group* or action research)).tw. | 23,943 |
| 60. | (triangulat* adj15 (method* or data or concurrent or sequential or simultaneous or design*)).tw. | 3586 |
| 61. | (qualitative adj5 quantitative adj5 (combin* or mixed or mix or integrat* or method* or analys*)).tw. | 19,248 |
| 62. | exp qualitative research/ and quantitative.tw. | 4485 |
| 63. | or/57–62 | 91,705 |
| 64. | (qualitative and quantitative).tw. | 80,055 |
| 65. | exp Nursing Research/ or exp Health Services Research/ or exp Rehabilitation/ | 517,202 |
| 66. | (px or nu or rh or ed or og or es or eh).fs. | 2,108,305 |
| 67. | (nurs* or educat* or rehabilitat* or psych* or social or socio* or service* or interview* or questionnaire* or survey*).af. | 6,681,233 |
| 68. | or/65–67 | 6,994,217 |
| 69. | 64 and 68 | 33,921 |
| 70. | 63 or 69 | 102,783 |
| 71. | (clinical trial* or evaluation studies or randomized controlled trial).pt. | 858,986 |
| 72. | (randomized or (clinical adj3 trial*) or (controlled adj3 trial*)).mp. | 1,570,183 |
| 73. | 71 or 72 | 1,570,208 |
| 74. | qualitative.mp. | 259,782 |
| 75. | 73 and 74 | 16,078 |
| 76. | ((qualitative or quantitative) adj5 nested).tw. | 750 |
| 77. | 70 or 75 or 76 | 114,804 |
| 78. | 56 or 77 | 858,542 |
| 79. | 17 and 78 | 1330 |
| 80. | (PICU or NICU or “p?ediatric intensive care” or “neonatal intensive care”).ti. | 10,908 |
| 81. | 79 not 80 | 1154 |
| SN | Search Strategy | Results |
|---|---|---|
| S1 | noft((“intensive care” or “critical care” or “critical* ill*” or “medical crisis” or ICU or ICUs or CCU or CCUs)) OR noft(((mechanic* or artificial* or assisted) NEAR/2 (ventilat* or respirat* or breath*))) | 7697 |
| S2 | noft(((emotion* OR psychologic* OR mental*) NEAR/2 (stress* OR pressure* OR tension* OR distress* OR strain* OR pain* OR suffer* OR trauma*))) OR noft((anxiet* OR anxious* OR fear* OR worry OR worries OR worrisome OR panic*)) OR noft((“stress disorder*” OR PTSD)) | 102,675 |
| S3 | noft(qualitative OR ethnol* OR ethnog* OR ethnonurs* OR emic OR etic OR leininger OR noblit OR “field note*” OR “field record*” OR fieldnote* OR “field stud*” or “participant observ*” OR “participant observation*” OR hermaneutic* OR phenomenolog* OR “lived experience*” OR heidegger* OR husserl* OR “merleau-pont*” OR colaizzi OR giorgi OR ricoeur OR spiegelberg OR “van kaam” OR “van manen” OR “grounded theory” OR “constant compar*” OR “theoretical sampl*” OR glaser AND strauss OR “content analy*” OR “thematic analy*” OR narrative* OR “unstructured categor*” OR “structured categor*” OR “unstructured interview*” OR “semi-structured interview*” OR “maximum variation*” OR snowball OR audio* OR tape* OR video* OR metasynthes* OR “meta-synthes*” OR metasummar* OR “meta-summar*” OR metastud* OR “meta-stud*” OR “meta-ethnograph*” OR metaethnog* OR “meta-narrative*” OR metanarrat* OR “ meta-interpretation*” OR metainterpret* OR “qualitative meta-analy*” OR “qualitative metaanaly*” OR “qualitative metanaly*” OR “purposive sampl*” OR “action research” OR “focus group*” or photovoice or “photo voice” or “mixed method*”) | 499,472 |
| S4 | S1 and S2 and S3 | 156 |
| S5 | ti((PICU OR NICU OR “p?ediatric intensive care” OR “neonatal intensive care”)) OR ti(child* or infant* or neonate* or adolescen*) | 143,497 |
| S6 | S4 and S5 | 102 |
| SN | Search Strategy | Results |
|---|---|---|
| (((TITLE-ABS-KEY (“intensive care” OR “critical care” OR “critical* ill*” OR “medical crisis” OR icu OR icus OR ccu OR ccus)) OR (TITLE-ABS-KEY ((mechanic* OR artificial* OR assisted) W/2 (ventilat* OR respirat* OR breath*)))) AND ((TITLE-ABS-KEY ((emotion* OR psychologic* OR mental*) W/2 (stress* OR pressure* OR tension* OR distress* OR strain* OR pain* OR suffer* OR trauma*))) OR (TITLE-ABS-KEY (anxiet* OR anxious* OR fear* OR worry OR worries OR worrisome OR panic*)) OR (TITLE-ABS-KEY (“stress disorder*” OR ptsd))) AND (TITLE-ABS-KEY (qualitative OR ethnol* OR ethnog* OR ethnonurs* OR emic OR etic OR leininger OR noblit OR “field note*” OR “field record*” OR fieldnote* OR “field stud*” OR “participant observ*” OR “participant observation*” OR hermaneutic* OR phenomenolog* OR “lived experience*” OR heidegger* OR husserl* OR “merleau-pont*” OR colaizzi OR giorgi OR ricoeur OR spiegelberg OR “van kaam” OR “van manen” OR “grounded theory” OR “constant compar*” OR “theoretical sampl*” OR glaser AND strauss OR “content analy*” OR “thematic analy*” OR narrative* OR “unstructured categor*” OR “structured categor*” OR “unstructured interview*” OR “semi-structured interview*” OR “maximum variation*” OR snowball OR audio* OR tape* OR video* OR metasynthes* OR “meta-synthes*” OR metasummar* OR “meta-summar*” OR metastud* OR “meta-stud*” OR “meta-ethnograph*” OR metaethnog* OR “meta-narrative*” OR metanarrat* OR “ meta-interpretation*” OR metainterpret* OR “qualitative meta-analy*” OR “qualitative metaanaly*” OR “qualitative metanaly*” OR “purposive sampl*” OR “action research” OR “focus group*” OR photovoice OR “photo voice” OR “mixed method*”))) AND NOT (TITLE (picu OR nicu OR “p?ediatric intensive care” OR “neonatal intensive care”)) AND (LIMIT-TO (DOCTYPE, “ar”) OR LIMIT-TO (DOCTYPE, “re”)) | 461 |
| SN | Search Strategy | Results |
|---|---|---|
| 1. | intensive care unit/ or burn unit/ or coronary care unit/ or medical intensive care unit/ or neurological intensive care unit/ or psychiatric intensive care unit/ or stroke unit/ or surgical intensive care unit/ | 185,005 |
| 2. | intensive care/ or exp artificial feeding/ or exp artificial ventilation/ or exp intensive care nursing/ or exp patient monitoring/ or exp resuscitation/ | 700,851 |
| 3. | critical illness/ | 30,491 |
| 4. | (“intensive care” or “critical care” or “critical* ill*” or “medical crisis” or ICU or ICUs or CCU or CCUs).mp. | 461,516 |
| 5. | ((mechanic* or artificial* or assisted) adj2 (ventilat* or respirat* or breath*)).mp. | 194,598 |
| 6. | or/1–5 | 993,957 |
| 7. | mental stress/ | 84,638 |
| 8. | distress syndrome/ | 46,611 |
| 9. | fear/ or anxiety/ | 266,725 |
| 10. | ((emotion* or psychologic* or mental*) adj2 (stress* or pressure* or tension* or distress* or strain* or pain* or suffer* or trauma*)).mp. | 157,928 |
| 11. | (anxiet* or anxious* or fear* or worry or worries or worrisome or panic*).mp. | 519,120 |
| 12. | exp anxiety disorder/ | 251,161 |
| 13. | psychotrauma/ | 9117 |
| 14. | (“stress disorder*” or PTSD).mp. | 70,861 |
| 15. | or/7–14 | 733,756 |
| 16. | 6 and 15 | 23,866 |
| 17. | (mixed method* or multi-method* or multiple method* or multiple research method* or multimethod* or mixed model* or mixed research).tw. | 72,100 |
| 18. | ((qualitative or qual) and (quantitative or quan) and (nested or concurrent or complementary or expansion or initiation or holistic or transformative or embedded or iterative or triangulat*)).tw. | 7464 |
| 19. | ((quantitative or quan) and (phenomenolog* or ethno* or (grounded adj3 theor*) or hermeneutic* or lived experience* or content analys* or thematic or theme* or narrative* or interview* or focus group* or action research)).tw. | 30,882 |
| 20. | (triangulat* adj15 (method* or data or concurrent or sequential or simultaneous or design*)).tw. | 4433 |
| 21. | (qualitative adj5 quantitative adj5 (combin* or blend* or mixed or mix or integrat* or method* or analys*)).tw. | 24,598 |
| 22. | exp qualitative research/ and quantitative.tw. | 7318 |
| 23. | or/17–22 | 120,842 |
| 24. | (qualitative and quantitative).tw. | 103,492 |
| 25. | (nurs* or educat* or rehabilitat* or psych* or social or socio* or service* or interview* or questionaire* or survey*).af. | 8,661,137 |
| 26. | 24 and 25 | 449,94 |
| 27. | 23 or 26 | 136,347 |
| 28. | (qualitative and (randomized or (clinical adj3 trial*) or (controlled adj3 trial*))).mp. [mp = title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word] | 25,586 |
| 29. | ((qualitative or quantitative) adj5 nested).tw. | 969 |
| 30. | 27 or 28 or 29 | 156,067 |
| 31. | qualitative.mp. | 341,811 |
| 32. | (ethnol$ or ethnog$ or ethnonurs$ or emic or etic).mp. | 87,812 |
| 33. | (leininger$ or noblit or hare).ti,ab. | 2805 |
| 34. | (field note$ or field record$ or fieldnote$ or field stud$).mp. | 25,400 |
| 35. | (participant$ adj3 observ$).mp. | 20,105 |
| 36. | (nonparticipant$ adj3 observ$).mp. | 172 |
| 37. | (non participant$ adj3 observ$).mp. | 870 |
| 38. | (hermeneutic$ or phenomenolog$ or lived experience$).mp. | 41,604 |
| 39. | (heidegger$ or husserl$ or merleau-pont$).mp. | 1301 |
| 40. | (colaizzi$ or giorgi$).mp. | 1833 |
| 41. | (ricoeur or spiegelberg$).mp. | 437 |
| 42. | (van kaam$ or van manen).mp. | 260 |
| 43. | (Grounded adj5 theor$).mp. | 17,396 |
| 44. | (constant compar$ or theoretical sampl$ or triangulat$).ti,ab. | 15,320 |
| 45. | (glaser and strauss).mp. | 143 |
| 46. | (content analys$ or thematic analys$ or narrative analys$).mp. | 69,915 |
| 47. | (unstructured categor$ or structured categor$).mp. | 28 |
| 48. | (unstructured interview$ or semi-structured interview$ or semistructured interview$).mp. | 67,154 |
| 49. | (maximum variation or snowball).mp. | 4952 |
| 50. | (audiorecord$ or taperecord$ or videorecord$ or videotap$).mp. | 104,605 |
| 51. | ((audio or tape or video$) adj5 record$).mp. | 39,686 |
| 52. | ((audio$ or video$ or tape$) adj5 interview$).mp. | 13,842 |
| 53. | (metasynthes$ or meta-synthes$ or metasummar$ or meta-summar$ or metastud$ or meta-stud$).ti,ab. | 1726 |
| 54. | (meta-ethnog$ or metaethnog$ or meta-narrat$ or metanarrat$ or meta-interpret$ or metainterpret$).mp. | 948 |
| 55. | (qualitative adj5 meta-analy$).mp. | 911 |
| 56. | (qualitative adj5 metaanaly$).mp. | 18 |
| 57. | purposive sampl$.mp. | 11,861 |
| 58. | action research.mp. | 5655 |
| 59. | focus group$.mp. | 62,086 |
| 60. | (photo voice or photovoice).mp. | 925 |
| 61. | 61 or/31–60 | 701,223 |
| 62. | 30 or 61 | 754,998 |
| 63. | 16 and 62 | 2261 |
| 64. | (PICU or NICU or “p?ediatric intensive care” or “neonatal intensive care”).ti. | 15,669 |
| 65. | 63 not 64 | 2086 |
| SN | Search Strategy | Results |
|---|---|---|
| 1. | intensive care/ | 4386 |
| 2. | artificial respiration/ | 245 |
| 3. | (“intensive care” or “critical care” or “critical* ill*” or “medical crisis” or ICU or ICUs or CCU or CCUs).mp. | 12,604 |
| 4. | ((mechanic* or artificial* or assisted) adj2 (ventilat* or respirat* or breath*)).mp. | 1656 |
| 5. | or/1–4 | 13,580 |
| 6. | psychological stress/ | 8990 |
| 7. | distress/ | 23,101 |
| 8. | anxiety/ | 63,637 |
| 9. | fear/ or panic/ | 20,310 |
| 10. | ((emotion* or psychologic* or mental*) adj2 (stress* or pressure* or tension* or distress* or strain* or pain* or suffer* or trauma*)).mp. | 85,994 |
| 11. | (anxiet* or anxious* or fear* or worry or worries or worrisome or panic*).mp. | 330,909 |
| 12. | exp posttraumatic stress disorder/ or acute stress disorder/ or emotional trauma/ or posttraumatic stress/ | 45,871 |
| 13. | (“stress disorder*” or PTSD).mp. | 53,876 |
| 14. | or/6–13 | 430,776 |
| 15. | 5 and 14 | 1715 |
| 16. | qualitative study.md. | 241,389 |
| 17. | exp qualitative research/ or grounded theory/ | 16,173 |
| 18. | phenomenology/ or constructivism/ or hermeneutics/ | 21,484 |
| 19. | ETHNOGRAPHY/ | 9050 |
| 20. | exp Content Analysis/ | 17,649 |
| 21. | qualitative.mp. | 175,473 |
| 22. | (ethno$ or emic or etic).mp. | 41,675 |
| 23. | (leininger$ or noblit or hare).ti,ab. | 1348 |
| 24. | leininger m$.cu. | 8 |
| 25. | noblit g$.cu. | 0 |
| 26. | hare r$.cu. | 3 |
| 27. | (field note$ or field record$ or fieldnote$ or field stud$).mp. | 13,210 |
| 28. | (participant$ adj3 observ$).mp. | 14,119 |
| 29. | (nonparticipant$ adj3 observ$).mp. | 205 |
| 30. | (non participant$ adj3 observ$).mp. | 413 |
| 31. | (hermeneutic$ or phenomenolog$ or lived experience$).mp. | 59,318 |
| 32. | (heidegger$ or husserl$ or merleau-pont$).mp,cu. | 15,996 |
| 33. | (colaizzi$ or giorgi$).mp,cu. | 7205 |
| 34. | (ricoeur or spiegelberg$).mp,cu. | 6216 |
| 35. | (van kaam$ or van manen).mp,cu. | 4451 |
| 36. | (Grounded adj5 theor$).mp. | 21,263 |
| 37. | (constant compar$ or theoretical sampl$ or triangulat$).ti,ab. | 12,128 |
| 38. | (glaser or strauss).mp. | 3194 |
| 39. | glaser b$.cu. | 5 |
| 40. | strauss a$.cu. | 9 |
| 41. | ((content or theme* or thematic or narrative or discourse) adj2 analys*).mp. [mp = title, abstract, heading word, table of contents, key concepts, original title, tests & measures, mesh] | 63,902 |
| 42. | (unstructured categor$ or structured categor$).mp. | 29 |
| 43. | (unstructured interview$ or semi-structured interview$ or semistructured interview$).mp. | 46,410 |
| 44. | (maximum variation or snowball).mp. | 2703 |
| 45. | (audiorecord$ or taperecord$ or videorecord$ or videotap$).mp. | 23,803 |
| 46. | (((audio or video*) adj5 (recorded or recording or tape* or taping)) or (tape adj3 record*)).mp. | 15,183 |
| 47. | ((audio* or video* or tape* or taping or recording) and (interview* or transcri* or theme* or thematic)).mp. [mp = title, abstract, heading word, table of contents, key concepts, original title, tests & measures, mesh] | 26,649 |
| 48. | (metasynthes$ or meta-synthes$ or metasummar$ or meta-summar$ or metastud$ or meta-stud$).ti,ab. | 971 |
| 49. | (meta-ethnog$ or metaethnog$ or meta-narrat$ or metanarrat$ or meta-interpret$ or metainterpret$).mp. | 757 |
| 50. | (qualitative adj5 meta-analy$).mp. | 285 |
| 51. | (qualitative adj5 metaanaly$).mp. | 3 |
| 52. | purposive sampl$.mp.5304 | |
| 53. | action research.mp.9589 | |
| 54. | focus group$.mp. | 39,087 |
| 55. | (photo voice or photovoice or mixed method*).mp. | 26,884 |
| 56. | or/16–55 | 513,897 |
| 57. | (mixed method* or multi-method* or multiple method* or multimethod* or mixed model* or mixed research).tw. | 40,823 |
| 58. | (triangulat* adj15 (method* or data or concurrent or sequential or simultaneous or design*)).tw. | 4688 |
| 59. | (quantitative or quan).tw,md. | 103,896 |
| 60. | (phenomenolog* or ethno* or (grounded adj3 theor*) or hermeneutic* or lived experience* or content analys* or thematic or theme* or narrative* or interview* or focus group* or action research).mp. | 644,155 |
| 61. | 60 and 59 | 27,527 |
| 62. | (qualitative.mp. or qualitative study.md.) and (quantitative.mp. or quantitative study.md.) | 101,561 |
| 63. | ((qualitative or quantitative) adj5 nested).tw. | 132 |
| 64. | (qualitative and (randomized or (clinical adj5 trial*) or (controlled adj5 trial*))).tw. | 3139 |
| 65. | or/57–58,61–64 | 131,796 |
| 66. | 56 or 65 | 528,987 |
| 67. | 15 and 66 | 348 |
| 68. | (PICU or NICU or “p?ediatric intensive care” or “neonatal intensive care”).ti. | 1159 |
| 69. | 67 not 68 | 301 |
| Patient Quotes | First-Order Interpretation | Second-Order Interpretation | Third-Order Interpretation |
|---|---|---|---|
| “Like a prisoner with tied hands and feet and closed mouth who is continually punctured with needles and cannot say anything” [42] “you do not see anyone, all in bed [with] a series of devices …connected to [them that] make noise” [2] “You [can] not move because of the tubes... you are attached to the bed” [38] “Since you are intubated, they passed it through the nose and the nose got sore. When the sore was recovering, they pulled it out and inserted [nasogastric tube] again into the nose. Doing this, they pressed the injured sore which made more pain” [42] “It was one of those things that you have to kind of grin and bear it” [34] “an infinite sense of loneliness as the most negative feeling” [3] | Feeling oppressed with endotracheal tube [12,21] Experiencing horror from being on a ventilator [29,35] Experiencing intubation and extubation as a source of trauma and torture [19] Agitated about frequent interruption of sleep [40] Frustrations and terror related to intubation [19,42] A permanent sense of torture from intubation and NG replacement [42] Pain of being unable to control one’s self [1] Feeling sad and isolated [40] Feeling distressed and lonely [27] Anxiety related to daily routine [1] Anxiety about excretion in bed [1] | Psychological suffering and feelings of imprisonment | Torment |
| “to be honest, everyone who wakes up and does not know where he is and once sees all these devices hooked to him and cannot do anything, is definitely going to have another MI [myocardial infarction] from fear” [20] “Today, the doctor comes and says that the operation was very good, you will get up soon and you will not have any special complications. Tomorrow another doctor will come and say that it is too early for me to comment. Maybe you will have a series of complications after the operation!” [2] “There is a lot of can’t… you can’t do …so all of these accumulate to a bad experience” [19] “From the moment you woke up you wanted to get out, to flee, you don’t want to stay even a minute longer” [3] “You want to calm down and you can’t…Doctors are constantly passing by to see how you are, but also to quarrel with you or your neighbor, because you are shaking and breaking the contacts from the cables” [3] | Feeling of shock [29,40] Feeling terrified by the ICU room [37] Fear of disability [12,22,27,34,39,41,43] Fear of experiencing mouth ulcers again [22] Hallucinations [3] Delusion about the hostility of ICU care team [3] Confused and vulnerable [2,3,19] The feeling of being in hell [1] Worrying about the emotional toll of ICU experience [2,22] | Depressive feelings and anxiety | Trauma |
| “when a patient becomes ill, the ward falls apart, all the doctors and nurses are gone [leaving other patients] subconsciously restless and upset” [2] “You become very anxious, it is like you are fighting for your life, … you are just getting instructions push, breath or whatever…” [19] “I am sure that they want to hurt me and nobody explains to me what has happened. The only thing that they cared about is my coughing.” [3] “Being in the ICU is “just like a little child who could not swim [and] was thrown into a cold swimming pool” [29] | Feelings of intentional neglect from ICU staff [3] Anger, fear and frustration from not being able to talk or not being understood [3,29,36] The wish to go on living [43] To be seen [43] | Fighting for survival and to be heard by the ICU staff | Fighting |
| “Weak in [the] body……[some] felt like a child, … who doesn’t think too much, can’t do anything; can’t pee by…self, poo by …self, can’t do anything” [25] “when I woke up from the coma the only thing that I confronted was fear, i.e., if I would be able to speak again because of the tracheotomy and if I would be able to walk again because I was confined in my bed…” [3] “felt strange… like there was a gap between [the] body and mind” [1] “It felt like my upper body was like an elephant, I didn’t expect my legs could carry me” [41] “I didn’t know what they were doing to me … I was a body, there, available” [33] “like a vegetable…. very defenseless and helpless” [40] | Feeling uncomfortable over loss of body control [12] Experiencing loss of functional ability [19] A sense of losing control over self and environment [38,44] Experiencing a disconnect between the heart and brain [1] Feeling a gab between the body and the mind [1] Pain accompanied with gap in perception, feeling and memory [1] Feeling of embarrassment and loss of personal dignity [19] Becoming paranoid [3] Uncertainties about the return of bodily functions [19,38] Feelings of not being able to talk again when weaned off breathing supports [3] Being dependent on breathing devices and fear of obstructed breathing from endotracheal tube dislodgment [20,29] Fear that the ventilator will stop working without the nurses’ notice [25,29] Depending on others [21] Fear of not being able to breath after weaning [28] Sense of loneliness [2,3,19,20,28,37,38] | Vulnerability and dependence | Altered identities |
| “…I couldn’t get to sleep once, but that battle axe [nurse] said I had” [25] “You want to be treated as an adult instead of a child, right? Yes, I mean I’m not an engine that needs to be fixed, I mean, I’m a human being” [36] “you know, not giving …updates … you just struggle. You feel so helpless, and you wonder if you are going to die” [34] “we were lying on bed like vegetables, it seemed that we did not exist to the nurses, they were chatting and laughing, too noisy” [29] “There were moments when [patients] almost cried in despair. [They were] suffering and [care practitioners] laugh[ed] at the top of their lungs a few meters away” [33] “You… [ring] the bell and no one shows up. […] It made me feel helpless, and powerless. … what can I say, you feel hurt and you could easily start to cry.” [36] “someone pressed my arms and legs forcefully, some others opened my mouth and put something into my throat, after that I knew that was the tracheal tube, why did nobody tell me about it before that?” [29] | Horrible experience of despair and disappointments [20] Feeling one’s freedom has been restricted [1] Feeling unsafe [20,35] Lack of information about care process [3] Feeling care practitioners were disinterested in providing essential practical care for pain [3] Hurtful feelings of powerlessness and helplessness due to delayed care [19,25,28,36] Feeling defenseless and helpless [21,40] Feeling degraded from depending on others [21,27,28,29,37] Feeling the coldness of nurses giving care [36] Irritation from nurses not extubating patients on time [28] Sadness from feeling ignored or not being taken seriously [36] Frustrations from inadequate information about patients’ illness and care procedures [38] Frustrations from communication problems [1,19,21,22,25,28,35,40,42] | Experiencing the loss of emotional safety in the ICU | Disempowerment |
| “I was very scared when I realized I was in the ICU. I told myself I was done!” [2] “You feel so helpless, and you wonder if you are going to die” [34] “when I woke up I found a tube in my throat, […] I could not stop thinking: Was I dying soon?” [29] “We were four and I was the only one left. Three died, and I saw them die…It was not easy holding on to the bed waiting for your moment to come” [20,33,37] “I have no fear of dying, but always of being in pain and suffering …. the same pain, I would like to die instead. … I thought that if (I) didn’t die soon, it would be pitiful” [24] I was in fear. I didn’t want to take my eyes off from the monitors…When the machine alarmed, I was frightened. Why did it alarm? What was happening with me?” [24] “I kept thinking of this: What should I do if there was anything wrong in the machine without someone knowing? Was that my last day of life?” [29] “I was scared because I thought the night nurse will kill me…so I yelled at her…” [31] | Fear of death [2,20,21,27,29,37,40,42] Perceiving the proximity of death through spoken words, condition of others and the death of others [3] | Perceiving the nearness of death | Fear of death |
| “for almost the entire [time], all the lights were on, there was no window, no clock, and [patients] didn’t have a sense of time” [3] “can hear all of it… it’s hard to explain but if you can’t sleep, can’t shut yourself down so to speak, and being afraid of all that may happen makes you scared. Yes all that makes you feel … I can’t hang on anymore” [36] “I did not know what is going on, I woke up, I felt a tube, I thought maybe I will pull a little bit, suddenly I saw the tube halfway out, so I took it out” [38] “when a patient becomes ill, the ward falls apart, all the doctors and nurses are gone [leaving other patients] subconsciously restless and upset” [2] “This thing that I put my wrist (referring to manometer connected to an arterial line) makes me both annoyed and afraid to make the slightest mone, because I think it will break and be dangerous for me!” [33] “an artificial environment, inappropriate to the human being, [and] not compatible with human expectations” [33] | Losing the sense of time [3] A permanent sense of torture from intubation and NG replacement [42] Discomfort and suffering from equipment and technologies used for treatment [29] | ICU environment as a source of anxiety and fear | Hostile environment |


References
- Takashima, N.; Yosihno, Y.; Sakaki, K. Quantitative and qualitative investigation of the stress experiences of intensive care unit patients mechanically ventilated for more than 12 hr. Jpn. J. Nurs. Sci. 2019, 16, 468–480. [Google Scholar] [CrossRef] [PubMed]
- Tavakoli, P.; Cheraghi, M.A.; Jahani, S.; Asadizaker, M. Experience of discomfort and its self-management strategies in ICU patients. J. Fam. Med. Prim. Care 2022, 11, 269–276. [Google Scholar] [CrossRef] [PubMed]
- Zisopoulos, G.; Triliva, S.; Roussi, P. Processing Intensive Care Unit Treatment Experiences: A Thematic Analysis of a Diary Intervention. Qual. Health Res. 2022, 32, 371–384. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, C.; Rosa, R.G.; Sganzerla, D.; Sanchez, E.C.; Robinson, C.C.; Dietrich, C.; Kochhann, R.; de Souza, D.; Rech, G.S.; da Rosa, R.; et al. The burden of mental illness among survivors of critical care—Risk factors and impact on quality of life: A multicenter prospective cohort study. Chest 2021, 160, 157–164. [Google Scholar] [CrossRef]
- Da Costa, J.B.; Taba, S.; Scherer, J.R.; Oliveira, L.L.F.; Luzzi, K.C.B.; Gund, D.P.; Sartori, G.; Porto, I.R.P.; Jorge, A.C.; Duarte, P.A.D. Psychological disorders in post-ICU survivors and impairment in quality of life. Psychol. Neurosci. 2019, 12, 391–406. [Google Scholar] [CrossRef]
- Yuan, C.; Timmins, F.; Thompson, D.R. Post-intensive care syndrome: A concept analysis. Int. J. Nurs. Stud. 2021, 114, 103814. [Google Scholar] [CrossRef]
- Hatch, R.; Young, D.; Barber, V.; Griffiths, J.; Harrison, D.A.; Watkinson, P. Anxiety, Depression and Post traumatic stress disorder after critical illness: A UK-wide prospective cohort study. Crit. Care 2018, 22, 10. [Google Scholar] [CrossRef]
- McGiffin, J.N.; Galatzer-Levy, I.R.; Bonanno, G.A. Is the intensive care unit traumatic? What we know and don’t know about the intensive care unit and posttraumatic stress responses. Rehabil. Psychol. 2016, 61, 120–131. [Google Scholar] [CrossRef]
- Wade, D.M.; Brewin, C.R.; Howell, D.C.; White, E.; Mythen, M.G.; Weinman, J.A. Intrusive memories of hallucinations and delusions in traumatized intensive care patients: An interview study. Br. J. Health Psychol. 2015, 20, 613–631. [Google Scholar] [CrossRef]
- Hosey, M.; Ali, M.; Mantheiy, E.; Albert, K.; Wegener, S.; Needham, D. Psychology consultation patterns in a medical intensive care unit: A brief report. Rehabil. Psychol. 2019, 64, 360–365. [Google Scholar] [CrossRef]
- Karnatovskaia, L.; Johnson, M.; Benzo, R.; Gajic, O. The spectrum of psychocognitive morbidity in the critically ill: A review of the literature and call for improvement. J. Crit. Care 2015, 30, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Albanesi, B.; Nania, T.; Barello, S.; Villa, G.; Rosa, D.; Caruso, R.; Udugampolage, N.S.; Casole, L.; Dellafiore, F. Lived experience of patients in ICU after cardiac surgery: A phenomenological study. Nurs. Crit. Care 2022, 27, 204–213. [Google Scholar] [CrossRef] [PubMed]
- Noblit, G.W.; Hare, R.D.; Hare, R.D. Meta-Ethnography: Synthesizing Qualitative Studies; Sage: Thousand Oaks, CA, USA, 1988; Volume 11. [Google Scholar]
- Sattar, R.; Lawton, R.; Panagioti, M.; Johnson, J. Meta-ethnography in healthcare research: A guide to using a meta-ethnographic approach for literature synthesis. BMC Health Serv. Res. 2021, 21, 50. [Google Scholar] [CrossRef]
- Cooke, A.; Smith, D.; Booth, A. Beyond PICO: The SPIDER tool for qualitative evidence synthesis. Qual. Health Res. 2012, 22, 1435–1443. [Google Scholar] [CrossRef] [PubMed]
- Carrozzino, D.; Patierno, C.; Pignolo, C.; Christensen, K.S. The concept of psychological distress and its assessment: A clinimetric analysis of the SCL-90-R. Int. J. Stress Manag. 2023, 30, 235–248. [Google Scholar] [CrossRef]
- Barr, J.; Fraser, G.; Puntillo, K.; Ely, E.; Gélinas, C.; Dasta, J.; Davidson, J.; Devlin, J.; Kress, J.; Joffe, A.; et al. Clinical Practice Guidelines for the Management of Pain, Agitation, and Delirium in Adult Patients in the Intensive Care Unit. Crit. Care Med. 2013, 41, 263–306. [Google Scholar] [CrossRef]
- Critical Appraisal Skills Programme. CASP Qualitative Checklist. Available online: https://casp-uk.net/casp-tools-checklists/ (accessed on 20 February 2025).
- Adeyemi, O. Patients Experiences of Mechanical Ventilation in the Intensive Care Unit of a Public Sector Tertiary Hospital University of the Witwatersrand. Master’s Thesis, University of the Witwatersrand, Johannesburg, South Africa, 2016. [Google Scholar]
- Aslani, Y.; Niknejad, R.; Moghimian, M.; Maghaddasi, J.; Akbari, M. An investigation of the psychological experiences of patients under mechanical ventilation following open heart surgery. ARYA Atheroscler. 2017, 13, 274–281. [Google Scholar]
- Engström, Å.; Nyström, N.; Sundelin, G.; Rattray, J. People’s experiences of being mechanically ventilated in an ICU: A qualitative study. Intensive Crit. Care Nurs. 2013, 29, 88–95. [Google Scholar] [CrossRef]
- Foster, A. More than nothing: The lived experience of tracheostomy while acutely ill. Intensive Crit. Care Nurs. 2010, 26, 33–43. [Google Scholar] [CrossRef]
- Gilder, E.; Jull, A.; Slark, J.; Parke, R.L. Patient’s experiences of endotracheal tubes and suction following cardiac surgery. Nurs. Crit. Care 2022, 27, 187–194. [Google Scholar] [CrossRef]
- Locsin, R.C.; Kongsuwan, W. Lived experience of patients being cared for in ICUs in Southern Thailand. Nurs. Crit. Care. 2013, 18, 200–211. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, V.; Bergbom, I.; Forsberg, A. The lived experiences of adult intensive care patients who were conscious during mechanical ventilation: A phenomenological-hermeneutic study. Intensive Crit. Care Nurs. 2012, 28, 6–15. [Google Scholar] [CrossRef]
- McKinley, S.; Nagy, S.; Stein-Parbury, J.; Bramwell, M.; Hudson, J. Vulnerability and security in seriously ill patients in intensive care. Intensive Crit. Care Nurs. 2002, 18, 27–36. [Google Scholar] [CrossRef]
- Rodriguez-Almagro, J.; Quero Palomino, M.A.; Aznar Sepulveda, E.; Fernandez-Espartero Rodriguez-Barbero, M.D.M.; Ortiz Fernandez, F.; Soto Barrera, V.; Hernandez-Martinez, A. Experience of care through patients, family members and health professionals in an intensive care unit: A qualitative descriptive study. Scand. J. Caring Sci. 2019, 33, 912–920. [Google Scholar] [CrossRef] [PubMed]
- Schou, L.; Egerod, I. A qualitative study into the lived experience of post-CABG patients during mechanical ventilator weaning. Intensive Crit. Care Nurs. 2008, 24, 171–179. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Zhang, B.; Li, C.; Wang, C. Qualitative analysis of patients’ intensive care experience during mechanical ventilation. J. Clin. Nurs. 2009, 18, 183–190. [Google Scholar] [CrossRef]
- Flahault, C.; Trosdorf, M.; Sonrier, M.; Vioulac, C.; Fasse, L.; Timsit, J.F.; Bailly, S.; Garrouste-Orgeas, M. ICU Survivors Experience of ICU Diaries: An Ancillary Qualitative Analysis of the ICU Diary Study. Crit. Care Explor. 2021, 3, e0384. [Google Scholar] [CrossRef]
- Mortensen, C.B.; Collet, M.O.; Samuelson, K. Struggling to return to everyday life-The experiences of quality of life 1 year after delirium in the intensive care unit. Nurs. Crit. Care 2023, 28, 670–678. [Google Scholar] [CrossRef]
- Herbst, A.; Drenth, C. The intensity of intensive care: A patient’s narrative. Glob. J. Health Sci. 2012, 4, 20–29. [Google Scholar] [CrossRef]
- Sanson, G.; Lobefalo, A.; Fascì, A. Love can’t be taken to the hospital. If it were possible, it would be better: Patients’ experiences of being cared for in an intensive care unit. Qual. Health Res. 2021, 31, 736–753. [Google Scholar] [CrossRef]
- Roberts, M.; Bortolotto, S.J.; Weyant, R.A.; Jock, L.; LaLonde, T.; Henderson, A. The experience of acute mechanical ventilation from the patient’s perspective. Dimens. Crit. Care Nurs. 2019, 38, 201–212. [Google Scholar] [CrossRef]
- Olsen, K.D.; Nester, M.; Hansen, B.S. Evaluating the past to improve the future–a qualitative study of ICU patients’ experiences. Intensive Crit. Care Nurs. 2017, 43, 61–67. [Google Scholar] [CrossRef]
- Hofhuis, J.G.; Spronk, P.E.; Van Stel, H.F.; Schrijvers, A.J.; Rommes, J.H.; Bakker, J. Experiences of critically ill patients in the ICU. Intensive Crit. Care Nurs. 2008, 24, 300–313. [Google Scholar] [CrossRef] [PubMed]
- Olausson, S.; Lindahl, B.; Ekebergh, M. A phenomenological study of experiences of being cared for in a critical care setting: The meanings of the patient room as a place of care. Intensive Crit. Care Nurs. 2013, 29, 234–243. [Google Scholar] [CrossRef] [PubMed]
- Ashkenazy, S.; Weissman, C.; Ganz, F.D. Perception of discomfort by mechanical ventilation patients in the Intensive Care Unit: A qualitative study. Intensive Crit. Care Nurs. 2021, 64, 103016. [Google Scholar] [CrossRef] [PubMed]
- Eqylan, S.B.; Safadi, R.R.; Swigart, V. The Lived Experience of Critically-III Muslim Patients in Isolation. Int. J. Qual. Stud. Health Well-Being 2022, 17, 2032548. [Google Scholar] [CrossRef]
- Samuelson, K.A. Unpleasant and pleasant memories of intensive care in adult mechanically ventilated patients—Findings from 250 interviews. Intensive Crit. Care Nurs. 2011, 27, 76–84. [Google Scholar] [CrossRef]
- Mylén, J.; Nilsson, M.; Berterö, C. To feel strong in an unfamiliar situation; Patients’ lived experiences of neurosurgical intensive care. A Qual. Study. Intensive Crit. Care Nurs. 2016, 32, 42–48. [Google Scholar] [CrossRef]
- Pakmehr, M.; Rahnama, M.; Firouzkouhi, M.; Abdollahimohammad, A. Lived experience of intubated patients: A phenomenological study. Indian J. Public Health Res. Dev. 2017, 8, 296–301. [Google Scholar] [CrossRef]
- Alpers, L.-M.; Helseth, S.; Bergbom, I. Experiences of inner strength in critically ill patients—A hermeneutical approach. Intensive Crit. Care Nurs. 2012, 28, 150–158. [Google Scholar] [CrossRef]
- Vogel, G.; Joelsson-Alm, E.; Forinder, U.; Svensen, C.; Sandgren, A. Stabilizing life: A grounded theory of surviving critical illness. Intensive Crit. Care Nurs. 2021, 67, 103096. [Google Scholar] [CrossRef] [PubMed]
- Yahui, Y.; Juan, W.; Huifen, X.; Xiaoqin, L.; Yinan, W.; Yang, G.; Chunmei, S. Experiences and needs of patients and relatives during hospitalization in an intensive care unit in China: A qualitative study. J. Transcult. Nurs. 2022, 33, 141–149. [Google Scholar] [CrossRef]
- Schandl, A.; Bottai, M.; Hellgren, E.; Sundin, Ö.; Sackey, P. Gender differences in psychological morbidity and treatment in intensive care survivors—A cohort study. Crit. Care 2012, 16, R80. [Google Scholar] [CrossRef]
- Tan, R.; Yu, T.; Luo, K.; Teng, F.; Liu, Y.; Luo, J.; Hu, D. Experiences of clinical first-line nurses treating patients with COVID-19: A qualitative study. J. Nurs. Manag. 2020, 28, 1381–1390. [Google Scholar] [CrossRef]
- Sheridan, N.F.; Kenealy, T.W.; Kidd, J.D.; Schmidt-Busby, J.I.; Hand, J.E.; Raphael, D.L.; McKillop, A.M.; Rea, H.H. Patients’ engagement in primary care: Powerlessness and compounding jeopardy. A qualitative study. Health Expect. 2015, 18, 32–43. [Google Scholar] [CrossRef] [PubMed]
- Zengin, N.; Ören, B.; Üstündag, H. The relationship between stressors and intensive care unit experiences. Nurs. Crit. Care 2020, 25, 109–116. [Google Scholar] [CrossRef]
- Christensen, M.; Hewitt-Taylor, J. Patient empowerment: Does it still occur in the ICU? Intensive Crit. Care Nurs. 2007, 23, 156–161. [Google Scholar] [CrossRef] [PubMed]
- Lykkegaard, K.; Delmar, C. A threat to the understanding of oneself: Intensive care patients’ experiences of dependency. Int. J. Qual. Stud. Health Well-Being 2013, 8, 20934. [Google Scholar] [CrossRef][Green Version]
- Yang, R. Dependency in Critically III Patients: A Meta-Synthesis. Glob. Qual. Nurs. Res. 2016, 3. [Google Scholar] [CrossRef]
- Halvorsen, K.; Jensen, J.F.; Collet, M.O.; Olausson, S.; Lindahl, B.; Hansen, B.S.; Lind, R.; Eriksson, T. Patients’ experiences of well-being when being cared for in the intensive care unit—An integrative review. J. Clin. Nurs. 2022, 31, 3–19. [Google Scholar] [CrossRef]
- Foucault, M. The Birth of the Clinic: An Archaeology of Medical Perception; Routledge: London, UK, 2003. [Google Scholar]
- Krampe, H.; Denke, C.; Gülden, J.; Mauersberger, V.M.; Ehlen, L.; Schönthaler, E.; Wunderlich, M.M.; Lütz, A.; Balzer, F.; Weiss, B.; et al. Perceived Severity of Stressors in the Intensive Care Unit: A Systematic Review and Semi-Quantitative Analysis of the Literature on the Perspectives of Patients, Health Care Providers and Relatives. J. Clin. Med. 2021, 10, 3928. [Google Scholar] [CrossRef] [PubMed]
- Darbyshire, J.L.; Müller-Trapet, M.; Cheer, J.; Fazi, F.M.; Young, J.D. Mapping sources of noise in an intensive care unit. Anaesthesia 2019, 74, 1018–1025. [Google Scholar] [CrossRef] [PubMed]
- Latour, J.M.; Kentish-Barnes, N.; Jacques, T.; Wysocki, M.; Azoulay, E.; Metaxa, V. Improving the intensive care experience from the perspectives of different stakeholders. Crit. Care 2022, 26, 218. [Google Scholar] [CrossRef]
- Tronstad, O.; Patterson, S.; Zangerl, B.; Flaws, D.; Holdsworth, R.; Irvine, L.; Yerkovich, S.; Pearse, I.; Fraser, J.F. The introduction of a sound reduction bundle in the intensive care unit and its impact on sound levels and patients. Aust. Crit. Care 2024, 37, 716–726. [Google Scholar] [CrossRef] [PubMed]
- Ruppel, H.; Funk, M.; Whittemore, R. Measurement of physiological monitor alarm accuracy and clinical relevance in intensive care units. Am. J. Crit. Care 2018, 27, 11–21. [Google Scholar] [CrossRef]
- Dziadzko, V.; Dziadzko, M.; Johnson, M.; Gajic, O.; Karnatovskaia, L. Acute psychological trauma in the critically ill: Patient and family perspectives. Gen. Hosp. Psychiatry 2017, 47, 68–74. [Google Scholar] [CrossRef]
- TenHouten, W.D. The emotions of powerlessness. J. Political Power 2016, 9, 83–121. [Google Scholar] [CrossRef]

| Sample | Adult patients hospitalized or discharged from the ICU, who experienced psychological distress during ICU hospitalization. |
| Phenomenon of Interest | Psychological distress during ICU hospitalization. Psychological distress is defined as a subjective experience of discomfort and stress, which may also include a sense of demoralization, the experience of feeling broken or mental pain, a sense of anguish, symptoms of somatization and cognitive alterations, feelings of anger, self-perceived lack of control, and self-criticism [16]. |
| Study Design | Any type of qualitative research design (i.e., phenomenology, grounded theory, and ethnography) utilizing any type of qualitative data collection (i.e., interviews, focus groups, journals, and field notes). |
| Evaluation | Experiences and/or perspectives and/or interpretations of psychological distress in the ICU and its impact on individuals’ perceptions and meanings of self and of their disease. |
| Research type | All types of published qualitative research papers and accessible grey literature. Mixed method studies with rich qualitative data were also included. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kusi-Appiah, E.; Karanikola, M.; Pant, U.; Meghani, S.; Kennedy, M.; Papathanassoglou, E. Disempowered Warriors: Insights on Psychological Responses of ICU Patients Through a Meta-Ethnography. Healthcare 2025, 13, 894. https://doi.org/10.3390/healthcare13080894
Kusi-Appiah E, Karanikola M, Pant U, Meghani S, Kennedy M, Papathanassoglou E. Disempowered Warriors: Insights on Psychological Responses of ICU Patients Through a Meta-Ethnography. Healthcare. 2025; 13(8):894. https://doi.org/10.3390/healthcare13080894
Chicago/Turabian StyleKusi-Appiah, Elizabeth, Maria Karanikola, Usha Pant, Shaista Meghani, Megan Kennedy, and Elizabeth Papathanassoglou. 2025. "Disempowered Warriors: Insights on Psychological Responses of ICU Patients Through a Meta-Ethnography" Healthcare 13, no. 8: 894. https://doi.org/10.3390/healthcare13080894
APA StyleKusi-Appiah, E., Karanikola, M., Pant, U., Meghani, S., Kennedy, M., & Papathanassoglou, E. (2025). Disempowered Warriors: Insights on Psychological Responses of ICU Patients Through a Meta-Ethnography. Healthcare, 13(8), 894. https://doi.org/10.3390/healthcare13080894