1. Introduction
Disclosing errors in healthcare is vital for the safety of patients. When an error occurs, healthcare providers, including attending nurses, should be honest and offer patients and their families complete and detailed information about the incident. This honesty serves as a dual purpose of assisting in settling any further damage from occurring and contributing to trust building in the nursing profession [
1]. To establish a successful and thorough system for error disclosure in healthcare, it is crucial to systematically pinpoint and address the barriers that prevent healthcare providers (HCPs) from disclosing errors effectively [
2].
A number of barriers hinder this approach to transparent disclosure from being implemented, including ineffective training and a lack of communication skills. While other supporting reasons have been explored, miscommunication between HCPs and the patients they treat is still believed to be the primary cause prompting lawsuits against them [
3]. Furthermore, research-based evidence indicates that there are various barriers that significantly impede HCPs’ preparedness to disclose errors, including fear of legal consequences, professional reputation concerns, cultural and organizational factors, emotional and psychological barriers, fear of professional repercussions, lack of clear policies [
2], and the absence of training, guidance, or experience in communication related to disclosure [
4].
There are also institutional barriers that impede the disclosure of medical errors; these include unsupportive institutional cultures and a lack of clarity about policies concerning the disclosure of errors [
5]. In their study, Ragucci K et al. (2016) showed the importance of involving qualified and trained professionals in the error disclosure policy of a health organization [
6]. By providing guidance and assistance while error disclosures are performed, patient welfare and effective error handling can be ensured [
7].
Moreover, the decision to disclose certain information may be influenced by a number of psychological processes. These include fear of insult, feelings of guilt and embarrassment, and the belief that the negative perceptions of colleagues, in addition to patient perceptions, will compromise them in terms of respect and trust [
7]. Another fear-driven factor is the fear of being sued, concerns over losing their malpractice coverage, and considerations of having to pay increased premiums for malpractice insurance [
8]. Birks Y et al. (2015) concluded that these financial consequences can create barriers to the open disclosure of information amongst HCPs [
8].
In fact, a regular supply of education and training among health workers is one of the strategies that encourages the successful disclosure of medical errors. Improving medical error disclosure may include offering disclosure training to the healthcare team and creating a transparent environment. Studies indicate that specific training on the disclosure of medical errors enhances attitudes, skills, and knowledge concerning the same in medical professionals [
9].
For this, collaboration between HCPs will be the key to improving patient outcomes and experiences. However, team-based care can also become a source of encouraging the disclosure of medical errors among team members of healthcare workers (HCWs). Therefore, it is indeed a good approach for every HCP, even if they are working in a supportive role, to contribute toward enhancing medical error disclosure. According to a study by Yan S et al. (2017), actively engaging every level of healthcare in disclosure initiatives is critically important [
10]. Additionally, there are conflicting opinions regarding the timing of error disclosures: Some believe one should only disclose when there is severe patient harm, while others advocate disclosure for near-miss incidents [
7]. Nurses hold a certain anxiety that being transparent about errors may give the idea that they were unsafe during patient care and could potentially ruin patient trust in healthcare providers [
1].
The central aim of this research inquiry is to identify the barriers to error disclosure for the purpose of building safer healthcare environments by encouraging open and honest communication in error disclosure, thus creating the conditions for the ethical reporting of errors.
1.1. Research Problem
The Disclosure of Patient Safety Incidents (DPSIs) is a systematic and practical approach that addresses communication strategies following a patient safety incident. The DPSI outlines the following procedures: First, in the event of a patient safety incident, the attending medical professional will promptly inform the patient and caregiver about the situation, express sympathy and regret, and commit to investigating the cause of the incident. Second, a formal apology will be offered if a medical error is found to be the cause of the incident. Third, compensation will be provided in line with the extent of the damage caused by the incident. Final step, a pledge is made to prevent similar incidents from occurring in the future. As a result, in order to advance the DPSI, a number of nations and organizations have incorporated patient safety incident communication principles into their accreditation requirements [
1]. Moreover, there are policies that promote heightened transparency, and a more profound understanding of the factors that support successful open disclosure is essential for practical implementation [
11].
Many studies have observed that nurses are seldom involved in the DPSI. This might be attributed to the fact that nurses usually deal with problems autonomously, which could lead to further stress and burden on them [
1]. On the other hand, physicians emphasize the need for supportive networks, a mechanism to deal with errors after obtaining assistance, and how clear disclosure instructions should be laid down. In contrast, nurses have expressed concerns about ambiguity in organizational cultures, as well as potential liability issues that add to their fear of possible retribution [
11]. Undoubtedly, HCPs, including nurses, frequently face numerous challenges that prevent them from being open about their mistakes, as confirmed by research findings [
12].
1.2. Significance of the Research
There is evidence that if patient safety incidents are disclosed, they will avoid unnecessary legal costs, costs of litigation, and, in some cases, negligence findings against practitioners. However, there are no studies that have specifically focused on the DPSI for the nursing profession, despite the fact that nurses are in frequent contact with medical errors and issues related to patient safety. Barriers to the open and honest disclosure of incidents should be identified, such that honesty in the face of error can be encouraged. This research may inform training programs, policy changes, and support systems to create a culture of safety. Thus, the ongoing study takes on a problem of paramount consideration in the domain of patient safety, healthcare quality, and ethical considerations.
This study highlights the barriers that discourage nurses from divulging medical errors and supports the Vision 2030 strategy in the Kingdom of Saudi Arabia in developing public service sectors, including health, and enhancing life [
13]. It is concerned with patient safety, instilling confidence in providers and patients, and maintaining exemplary standards of care. The research also fosters a continuous improvement in culture and ethical practice in the health sector, which is critical for attaining the qualitative healthcare services envisioned in Vision 2030’s ambitious goals.
1.3. Research Questions
- i.
What are the barriers to error disclosure among nurses working at a tertiary hospital in the Kingdom of Saudi Arabia?
- ii.
How do these barriers relate to the sociodemographic characteristics of the nurses working at a tertiary hospital in the Kingdom of Saudi Arabia?
4. Discussion
Error disclosure in nursing is crucial for patient safety and quality of care; however, different barriers prevent nurses from truly communicating errors to patients and families. In their study to explore the factors that facilitate or hinder error disclosure in Saudi tertiary hospitals, Alyaemni (2023) argued that although ethical, professional, and legal standards in Saudi Arabia manage and direct the disclosure of medical errors, factors including lack of knowledge and training, as well as personal beliefs, affect disclosure [
15]. This study, with primary objectives, will analyze socio-demographic and clinical experience data with a basic focus on these barriers and their domains. This study found an association between barriers to error disclosure and socio-demographic factors among nurses, whereby male nurses scored higher on such barriers than female nurses. The under-representation of male nurses in the sample might also impact the study findings, as the trend of the nursing workforce continues to be female-dominated globally [
16].
Cultural ascription may contribute to the rising score of barriers among male nurses. In their study, Zaghloul et al. (2016) found that men were more inclined to disclose errors in general, regardless of their history of any past error experience. This disparity is attributed to cultural, social, or psychological factors wherein male nurses view error disclosure as a threat to their integrity, while female nurses might be more free to disclose such errors because of their caring and empathetic nature. This also proves the need to investigate how systemic and contextual factors contribute to these gender differences in error disclosure [
17].
Statistically, this study showed no significant difference in the barrier scores concerning age, nationality, education, or years of experience. This is contrary to the expectations that such relationships must exist across different healthcare contexts. Khachian et al. (2022) stated that contract nurses tend to feel less free than permanent nurses. There was no correlation found between the type of employment and perception of barriers in a recent study [
5]. While prior studies have found that job title, gender, and history of errors affect disclosure behaviors, physicians are less inclined than non-physicians to disclose errors [
18]. Furthermore, Zaghloul et al. (2016) stated that physicians are less likely to disclose errors compared to non-physicians, indicating that job title affects disclosure behaviors, as shown by the results. Such variations can be seen as grounded in underlying cultural influences on disclosure attitudes [
17]. These discrepancies can be explained by various cultural influences on attitudes toward disclosing.
Additionally, nurses in emergency and outpatient units reported experiencing more impediments to error disclosure than nurses in other units. In their study, Giraldo et al. (2017) showed that high-stress environments were correlated with major medical errors. These environments encourage rapid decision making and have large patient flows that induce more stress and feelings of fear that one will be judged or punished [
19].
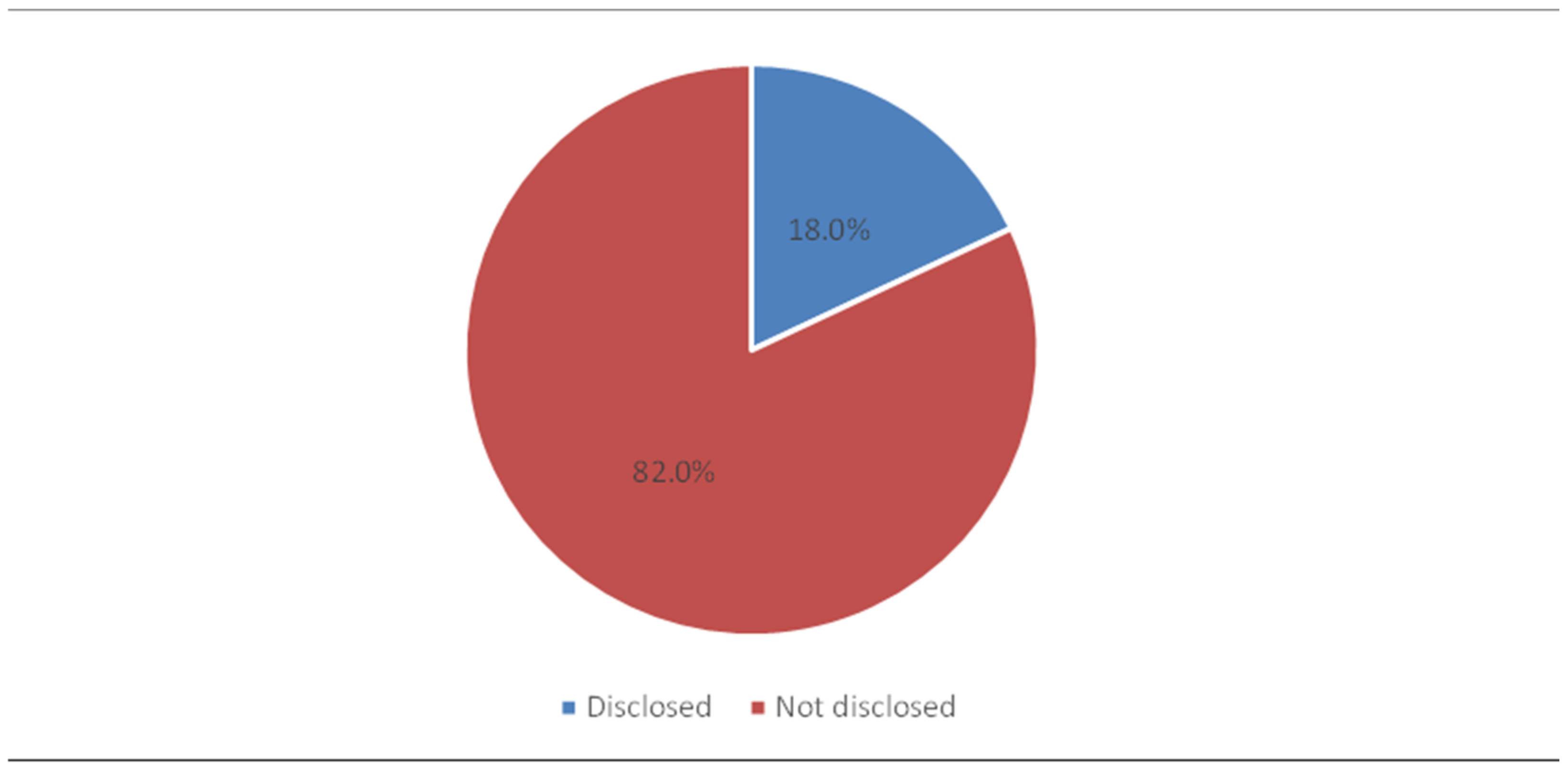
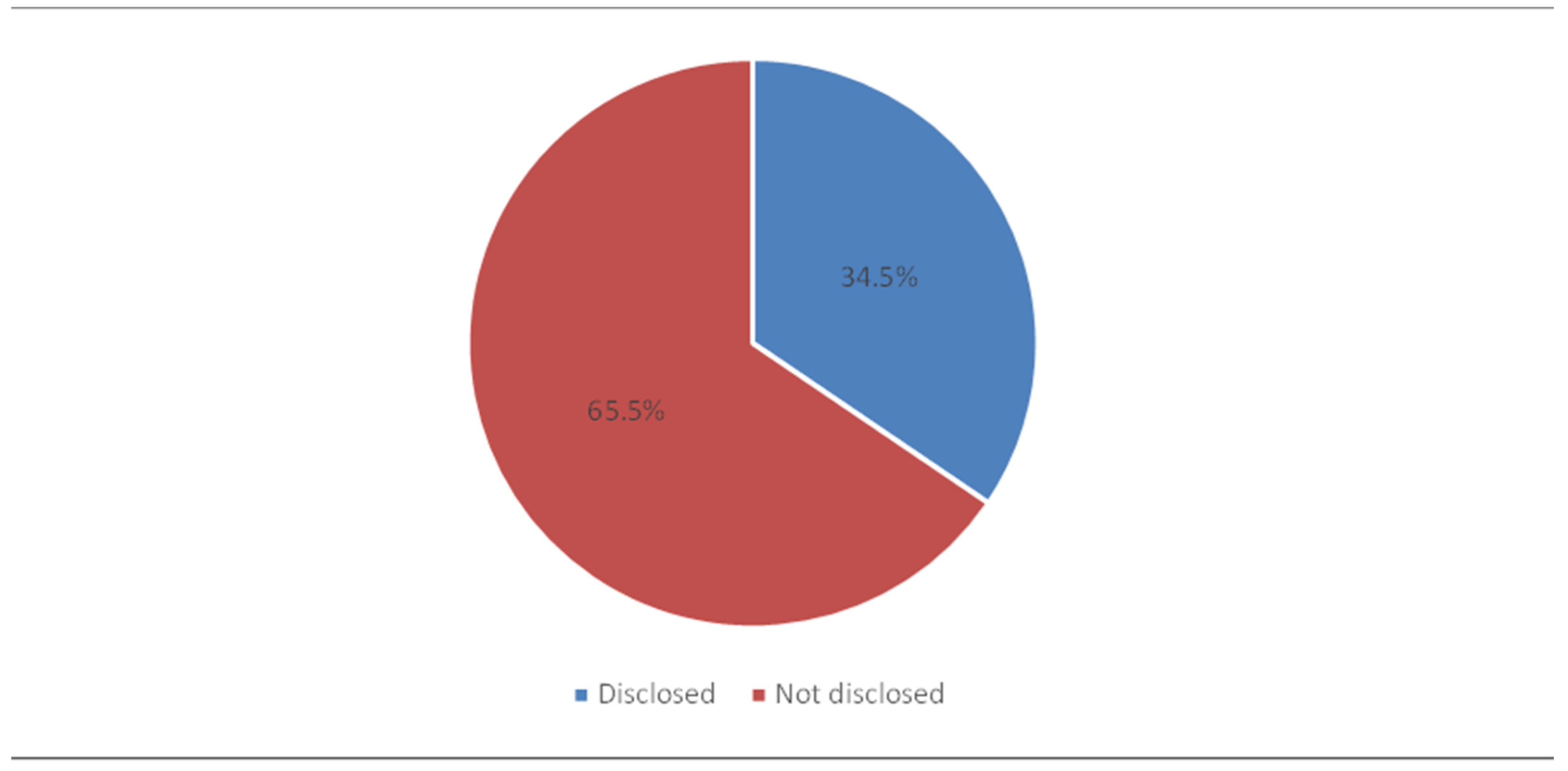
This study showed that nurses face moderately high barriers to disclosing medical errors, with 63% of the respondents reporting barriers to medical error disclosure. Specifically, just 12.2% indicated low barriers, 78% reported moderate barriers, and 9% reported high barriers. On the other hand, in their findings, Khachian et al. (2022) showed that nurses perceived more facilitators for the disclosure of medical errors and considered negative repercussions less significant, highlighting some other aspects [
5]. Those nurses might have viewed their work environment more positively compared to our participants, who indicated much greater challenges in this context.
This study analyzed barriers to error disclosure, concluding that psychological barriers rank highest, followed by institutional barriers and then financial concerns. Confidence and knowledge barriers scored the lowest. While most studies identified similar barriers, their rankings might vary based on the focus areas. These studies confirmed that the main barriers faced by healthcare providers (HCPs) include significant psychological barriers [
2,
19,
20,
21]. Other research suggested that different rankings for error disclosure are based on the occupational group, type of error, and health care setting [
22,
23].
As indicated by McLennan et al. (2016), hurdles to error disclosure arise from issues of intrapersonal and interpersonal communication. These authors point to problems associated with doctor–patient relationships, peer-to-peer interactions, and systemic factors, such as culture, policy, and legal pressures. Such barriers reduce openness and psychological safety, and they adversely impact the quality of error disclosure. A number of earlier studies pointed out similar barriers faced by individuals, confirming that consistent challenges across different contexts have been acknowledged in studies. Psychological, organizational, and financial reasons have all been implicated in non-disclosure of errors. The diversity across studies arises from differences in health systems, workplace cultures, and between populations. Nevertheless, this diversity points to specific solutions with respect to general and/or specific disclosure barriers [
23].
To clarify the different barriers faced by nurses, it is essential to pinpoint the concerns based on their own assessments. Among psychological barriers, the highest mean was obtained for “fear of losing patient trust”, meaning nurses often resisted disclosing information because of this fear. Studies have found that, for nurses, maintaining trust is a barrier to disclosure, while, for physicians, transparency enhances trust [
24]. In other words, nurses generally worry that openness places the patient–provider relationship, which is invaluable when it comes to the quality of care and patient satisfaction, at risk.
Nevertheless, the lowest mean score recorded in the present study within the psychological barrier dimension was “fear of shame”. However, despite this, it is still considered to be a significant barrier. This sentiment coincides with the study conducted by Iedema et al. (2011), where it was explained that HCPs most likely believe patients will blame them as individuals for mistakes instead of understanding the true complexity of medical errors [
25]. Again, emotional factors like shame and fear of negative reactions might discourage HCPs from being straightforward in sensitive situations. Thus, a culture of open dialogue and education on the importance of disclosure will enhance trust in the healthcare framework. Moreover, this notion parallels the findings of Carmichael T. (2017), which found that medical professionals hesitated to disclose errors due to fear of repercussions from colleagues. Such fears have built a culture in which the risks of disclosure outweigh the benefits [
26]. Similarly, some nurses do not report errors for fear of negative consequences on their reputation, credibility, and risk of isolation in the workplace, thus creating standing challenges for transparency in health care. Furthermore, these results correspond with the study by Albalawi et al. (2020), where it was highlighted that blame culture and ineffective communication in Arab nations, including Saudi Arabia, are prevalent issues contributing to a weak patient safety culture. These communication challenges were attributed to workforce diversity, language barriers, and cultural differences. Among nurses in Saudi Arabia, the fear of blame was identified as a significant obstacle to reporting incidents and medication errors [
27].
The second dimension preventing error disclosure among nurses, according to a recent study, is institutional barriers. The item that had the highest degree of agreement was “My institution does support healthcare providers in disclosing medical errors”. Thus, moderate support for error disclosure did exist for the study participants. There is an increased emphasis in the literature that a supportive institutional culture, strong leadership, and properly functioning organizational structures are required for effective error disclosure practices [
28].
Conversely, the statement, “My institution sends mixed messages about how to disclose an error”, received the lowest score, yet its mean still held relevance. This suggests some confusion in the institution’s communication regarding error disclosure policies. According to Choi J et al. (2019) and Pyo J et al. (2020), the failure to report errors was attributed to high workloads and a lack of adequate resources [
1,
29]. HCPs are under massive conflicting pressures imposed by leaders regarding disclosure and handling sensitive situations [
30]. Moreover, Walton M et al. (2019) noted that patients frequently revealed their experiences informally, thus making formal disclosure processes less viable in health institutions [
31]. Conversely, Waller R et al. (2020) argued that nurses are encumbered with disclosure barriers, such as a lack of institutional support and the burden of disclosure errors [
32].
After the above-mentioned two dimensions, an explicit barrier to error disclosure was found to be related to financial concerns. Another finding showed that “fear of litigation” obtained the highest rating and was deemed by the participants to be the most probable challenge to error disclosure among nurses; in contrast, the mean value for “fear of higher premiums” was the lowest, pointing to it as being somewhat less of an immediate concern.
Additional supporting evidence indicates that fear of lawsuits and the practices of insurers impede clinicians from disclosing errors [
25]. Other studies further showed that HCPs are expected to maintain transparency but generally avoid disclosing errors due to their fear of malpractice lawsuits [
3,
22,
33,
34]. Additionally, Aubin L et al. (2022) further mentioned that surgeons are not willing to report even minor adverse events due to such fears [
35]. Moreover, Alshaban, H et al. stressed that over half of nurses perceived error disclosure as a source from which lawsuits may derive [
36].
In addition, Albalawi A et al. (2020) reported that the issue of blame culture is further underscored by the increasing number of complaints and legal claims filed against healthcare providers, often stemming from adverse events linked to patient mortality or morbidity. In Saudi Arabia, the Ministry of Health revealed that, between 2012 and 2015, 91% of legal claim cases were deemed preventable. This highlights the critical need for fostering a non-punitive environment to promote error reporting and improve patient outcomes [
27].
In contrast, because of the possible worry of law that may complicate compromises, settlement agreements frequently encompass restrictive clauses of non-disclosure, with more than three-quarters of settlements prohibiting any acknowledgment of their existence. This trend, under the influence of tort reform, exemplifies a legal culture that is resistant to disclosure. In addition, Yan S et al. (2017) indicated that patients are concerned about complaint procedures and financial transparency in hospitals, which negatively affect physicians’ willingness to disclose errors due to fear of complaints [
10].
Although new initiatives have been implemented, economic and legal problems still remain relevant today. Based on a study of Pennsylvania’s 2002 Act 13, the institution of this law was meant to improve error disclosures within healthcare organizations. It reported that disclosed malpractice claims involve much higher settlements than undisclosed ones, with the maximum involving claims based on severe injuries. The number of claims per 1000 admissions has not changed, which indicates continuing economic problems [
37].
Thus, several programs have been implemented to target economic and legal problems in healthcare. Programs such as Communication, Apology, and Resolution (CARe) and the Collaborative Communication Resolution Program (CCRP) have demonstrated success in a marked reduction in malpractice claims and in cutting down resolution time. Painter R et al. (2018) estimated claims to have occurred in only 5% of incidents [
38], while Mello M et al. (2017) saw a decrease in the time resolution from 17 to 8 months [
39].
Thus, fear of lawsuits and financial repercussions discourage HCPs from communicating mistakes. While programs like CARe and CCRP promote open communication, the specter of legal consequences and financial loss persists. Reforms must go beyond the law to enhance protections for healthcare workers, improve insurance practices, and create a culture in which transparency is supported rather than punished.
Examining the barriers related to error disclosure, one major finding was that, according to slightly over half of the respondents, barriers relating to confidence and knowledge had the lowest score. The statement “I am not sure how much I should disclose to a patient/family member in the event I am involved in a medical error” showed a very high mean score. These findings are in agreement with a study by Iedema et al. (2011) wherein similar issues were raised, whereby providers frequently encountered uncertainty in making decisions regarding what details are to be shared after clinical errors have taken place [
25].
The interrelation with information sharing has been highlighted by various studies. In patient participation, according to LeCraw J et al. (2018), the balancing act of patient safety on the one side and the legal protections and liability in assessing informed confidentiality on the other side makes it difficult to implement policies [
40]. In addition, the disposition to withhold some information has been reported in other studies where there is an inclination for serious medical errors to be reported, while near misses are frequently not reported due to uncertainties as far as disclosure standards are concerned. It is commonly the severity of the error that usually determines whether it will be disclosed or not; with different cases, however, there is usually a broad variation among them [
19,
29,
33,
41].
On the other hand, there are some studies in support of disclosure. For instance, Mira J, et al. (2017) found that hospital pharmacists recommend full disclosure [
42], while Carmichael T. (2017) noted that many doctors seek to disclose harmful errors. Still, many nurses are not sure of what to disclose, although many believe that it is important to disclose any potentially harmful errors, regardless of whether harm has occurred or not [
26].
It has been noted that many studies have pointed out significant differences between how transparency is perceived in healthcare. Yan S et al. (2017) illustrated the gap between the expectations of healthcare providers and their consumers regarding transparency [
10]. Moreover, Jones T et al. (2019) observed a conflict between the desire for transparency and a need for protection during disclosure [
30]. In addition, Choi J et al. (2019) showed that Korean nurses recognize the importance of disclosure policies; however, they need enhanced training and clearer guidelines on disclosure [
1], while Kim S et al. (2017) added the role played by the media in publicizing medical errors, adding difficulty to the process of disclosure [
43].
Earlier studies have shown that, on the one hand, many acknowledge that error disclosure is an important art, while, on the other hand, the ways of performing it vary widely [
24,
30,
32]. Such variation is influenced by several factors, such as the nature of the legal environment, cultural attitudes, and organizational reporting policies [
3,
6]. General agreement about disclosure practices, training for those working in the health field, and policies that guarantee some level of transparency, while also protecting the parties involved with the errors, are needed. Enhanced policies can ensure that disclosures are ethical and meet patients’ expectations for open communication [
11].
Moreover, a lack of confidence is attributed to medical error disclosure in this study. Iedema R et al. (2011) revealed the challenge clinicians face in disclosing errors, particularly when confronted with an upset patient and their peers, as it requires high levels of poise to deal with this matter. In addition, Choi J et al. (2019) argued that there are no guidelines to govern the process of disclosing patient safety incidents. For many clinicians, the fear of disclosing errors often stems from emotional pressure from unhappy patients and worry about what might happen. Hence, a framework for improved communication among doctors regarding error disclosure needs to be developed [
1]. Nonetheless, unlike our study, Musharrafieh U et al. (2019) established that unawareness and lack of confidence cause significant barriers for nurses who reported making errors (even though they did not necessarily disclose information about their errors because of these barriers), and this is coupled with a lack of support [
44]. Different results were found in this study, perhaps due to variations in institutional support or training, and in the target groups recruited in previous studies compared to those in ours.
The last dimension that the study dealt with was termed “other barriers”. The top-ranked factor was fear of being blamed for making a medical error by not attending the meeting for disclosure of cases to patients or their families. In their findings, Aubin L et al. (2022) and Alshaban H et al. (2019) found that medical professionals often deflect disclosure of information because of the culture of defensive practice that fosters blame, shame, and fear of reprisal. In more explicitly drawn terms, nurses often find themselves under coercive, both emotional and institutional, pressures to refrain from disclosing errors, fearing that they may be blamed for the errors, especially when they are not in a privileged position in the decision-making process. To promote a less blameful culture and, therefore, better communication, institutional support needs to be strengthened or encouraged [
35,
36].
In addition, the lowest mean score related to “other barriers” was obtained for the belief that “the physician is ultimately responsible for disclosing the medical error, regardless of his or her involvement”. Thus, responsibilities for disclosing errors in healthcare settings require further exploration. Perez M et al. (2014) stated that it is the organization and not the individual nurse who is accountable for the error that has occurred [
24]. Furthermore, according to Mira J et al. (2017), some HCPs do not agree on who should take the lead in disclosing patient safety incidents [
42]. Additionally, Choi J et al. (2017) noted that certified nurses acknowledged the importance of disclosure, yet were not in consensus regarding the primary responsibility [
1]. In addition, Mohamed M et al. (2023) reported that nurses had higher awareness of what errors were and to whom they should report those errors than HCPs [
45]. Moreover, Walton M et al. (2019) reported that most informal disclosures were made by nurses and that medical practitioners were responsible for fewer than a quarter of informal disclosures [
31]. On the other hand, Gu Q. and Deng Y. (2021) argued that expectation regarding disclosure varies according to the level of harm: Moderate harm should be disclosed by HCPs, whereas, for serious harm, top management must be involved. This shows that the nurses have ambiguous definitions of their roles in the disclosure of medical errors, which, in turn, place conflicting practices on frontline healthcare providers [
46]. Organizations must, thus, support the roles of nurses and clarify responsibilities for error disclosure to avoid ambiguity.
Overall, this study extends current knowledge around barriers to medical error disclosure that are attributable to individual characteristics, such as the profession and nature of the working environment, as well as organizational factors, such as safety culture. This study shows that the practices of revealing errors vary significantly based on specific circumstances. Nurses in an emergency setting, as opposed to an outpatient setting, are less likely to disclose errors due to the immediacy of the consequences or due to the lack of support afforded in such dynamic environments. Job security can also be an influencing factor on individuals’ willingness to disclose errors, as those in more secure jobs often feel a greater commitment to their organization.