Occupational Diseases in Art Conservators and Restorers: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Information Sources
2.3. Search Strategy
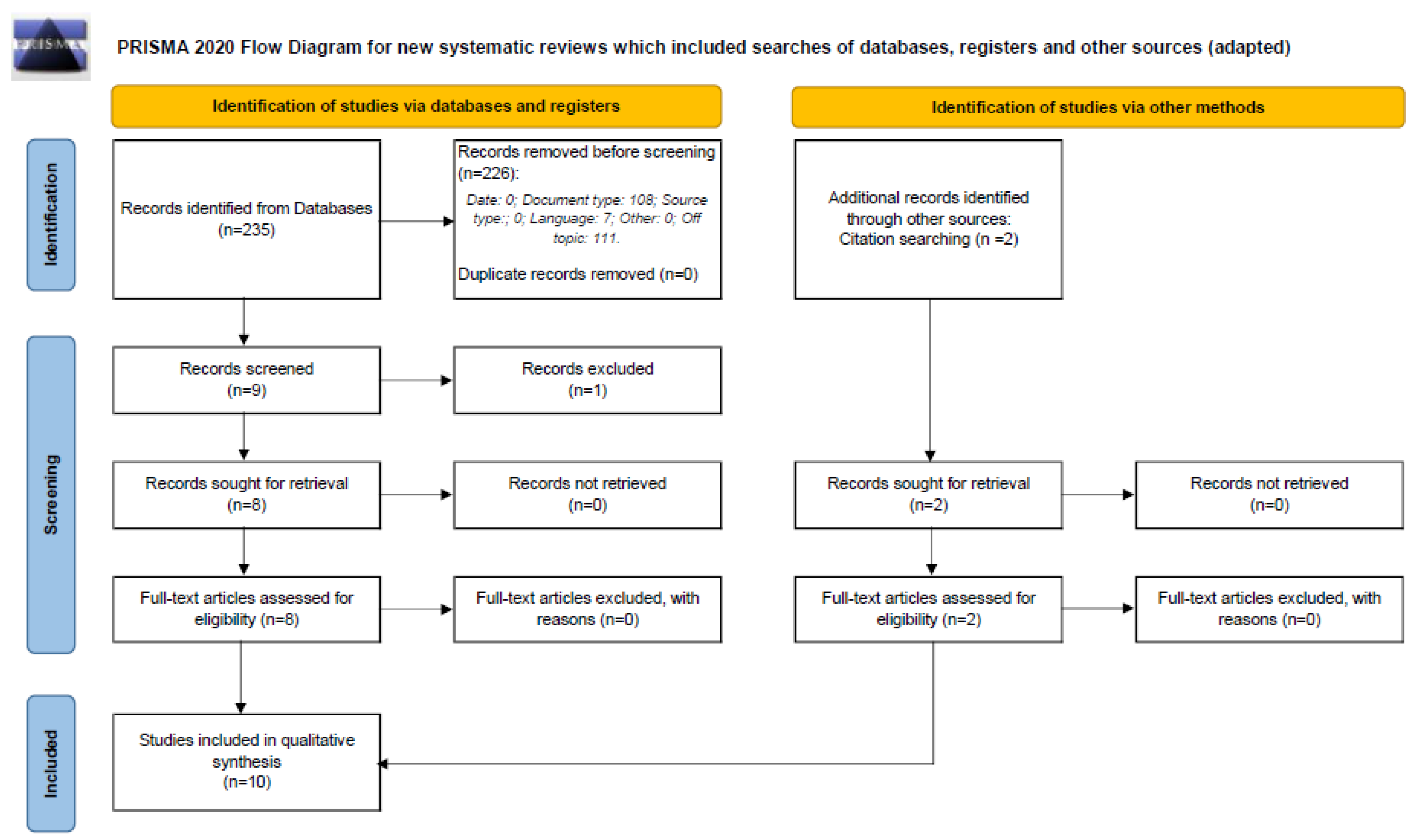
2.4. Selection Process
2.5. Data Collection Process and Data Items
2.6. Study of Risk of Bias
3. Results
3.1. Study Selection
3.2. Study Characteristics
3.2.1. Publication Year and Research Topics
3.2.2. Participants Characteristics
3.3. Environmental Conditions and Experimental Protocol
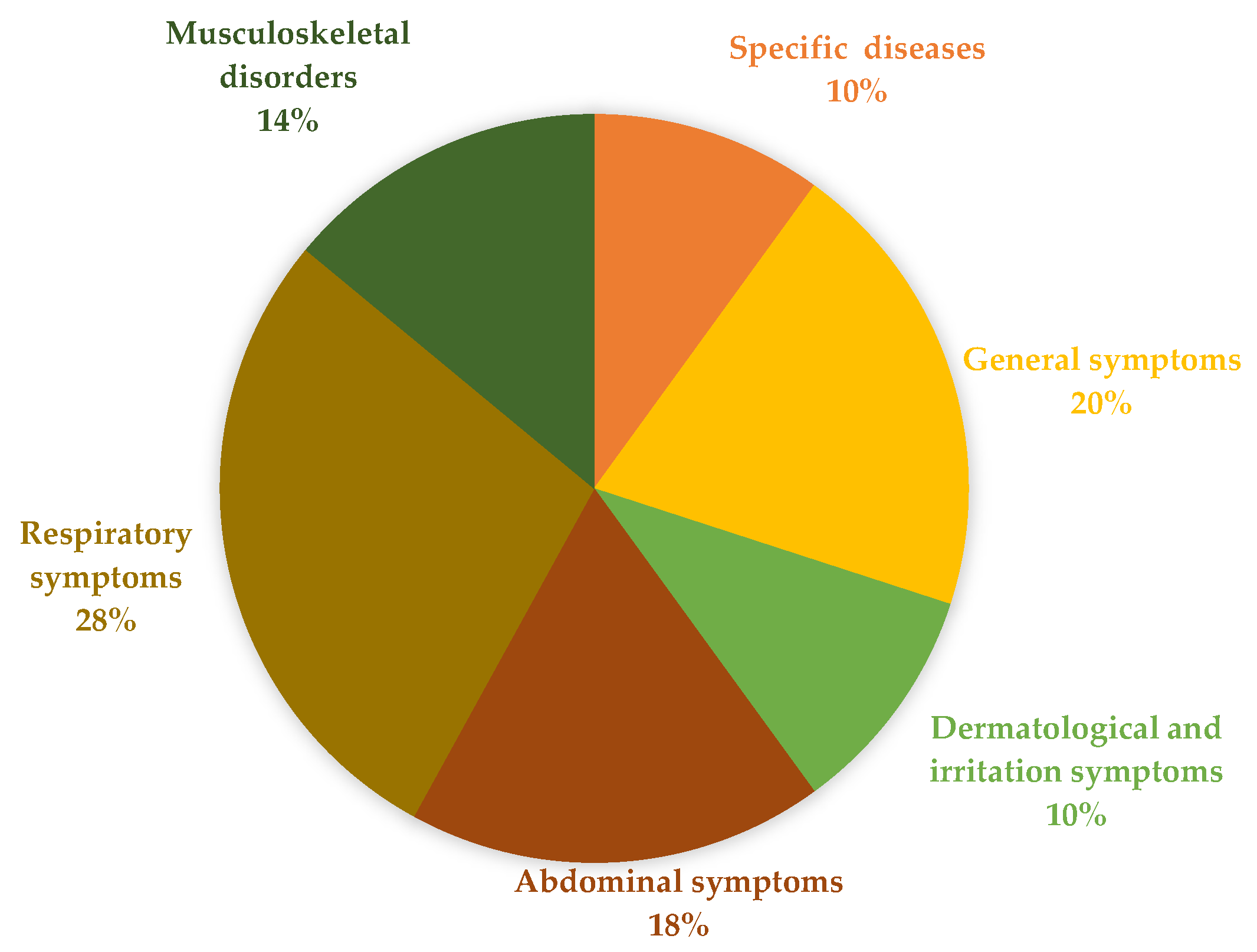
3.4. Outcomes
3.5. Risk-of-Bias Assessment
4. Discussion
4.1. Comparative Analysis with Similar Professions
4.2. Preventive Measures
4.3. Policy Interventions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Mekonnen, H.; Bires, Z.; Berhanu, K. Practices and challenges of cultural heritage conservation in historical and religious heritage sites: Evidence from North Shoa Zone, Amhara Region, Ethiopia. Herit. Sci. 2022, 10, 172. [Google Scholar] [CrossRef]
- Ballestrem, A.; von Imhoff, H.C.; McMillan, E.; Perrot, P.N. The conservator-restorer: A draft definition of the profession. Mus. Manag. Curatorship 1984, 3, 75–78. [Google Scholar] [CrossRef]
- Santos, A.; Dias, M.; Ribeirinho, A. ARP—Associação Profissional de Conservadores-Restauradores de Portugal. 2000. Available online: https://arp.org.pt/ (accessed on 12 March 2025).
- Pinheiro, A.C.; Ramos, A. Heritage keepers: The perils in textile conservation. Heritage 2021, 4, 4716–4726. [Google Scholar] [CrossRef]
- Saúde, I.-G. Manual de Segurança e Saúde no Trabalho DGR/2018; Despacho da Inspetora-Geral exarado na Informação nº 563/2018; Inspeção Geral das Atividades em Saúde (IGAS): Lisboa, Portugal, 2018. [Google Scholar]
- Carro, G.; Schalm, O.; Storme, P.; Blanckaert, G.; Demeyer, S. Indoor air quality for heritage objects and human health: Just a different interpretation of the same measurements? Air Qual. Atmos. Health 2024, 17, 19–34. [Google Scholar] [CrossRef]
- Varnai, V.M.; Macan, J.; Ćalušić, A.L.; Prester, L.; Macan, B.K. Upper respiratory impairment in restorers of cultural heritage. Occup. Med. 2011, 61, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Earn, J. Exploring the gap in the Occupational Safety and Health Administration (OSHA) laboratory standard: A literature review and recommendations to enhance histology laboratory safety practices. J. Histotechnol. 2022, 45, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Langford, M.; Beaumont, M.S.; Annett, D. Ergonomics, risk management and injury prevention in textiles conservation. J. Inst. Conserv. 2013, 36, 81–101. [Google Scholar] [CrossRef]
- Górny, R.L.; Harkawy, A.S.; Ławniczek-Wałczyk, A.; Karbowska-Berent, J.; Wlazło, A.; Niesler, A.; Gołofit-Szymczak, M.; Cyprowski, M. Exposure to culturable and total microbiota in cultural heritage conservation laboratories. Int. J. Occup. Med. Environ. Health 2016, 29, 255–275. [Google Scholar] [CrossRef] [PubMed]
- Ligor, T.; Gorczyca, P.; Buszewski, B. Using gas chromatography for indoor-air quality control in conservation and renovation studios. Int. J. Occup. Saf. Ergon. 2005, 11, 251–261. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, P.A.; Girão, F.; Henriques, P. A rich and blessed professional illness-organizing pneumonia due to gold dust. Rev. Port. Pneumol. 2011, 17, 182–185. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Medicine 2018, 169, 467–473. [Google Scholar]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions; Wiley: Hoboken, NJ, USA, 2019. [Google Scholar]
- Fischbein, A.; Wallace, J.; Anderson, K.E.; Sassa, S.; Kon, S.; Rohl, A.N.; Kappas, A. Lead Poisoning in an Art Conservator. JAMA 1982, 247, 2007–2009. [Google Scholar] [CrossRef] [PubMed]
- Kanceljak-Macan, B.; Trošíc, I.; Varnai, V.M.; Pavičíc, I.; Macan, J. Induced sputum evaluation in restorers and conservators of cultural heritage. Arch. Environ. Occup. Health 2012, 67, 229–238. [Google Scholar] [CrossRef] [PubMed]
- Costa-Moreira, P.; Coelho, R.; Pita, I.; Macedo, G. Acute Colonic Pseudo-Obstruction as a Manifestation of Lead Intoxication in a Conservator. ACG Case Rep. J. 2019, 6, 3. [Google Scholar] [CrossRef]
- Deering, K.; Spiegel, E.; Quaisser, C.; Nowak, D.; Rakete, S.; Garí, M.; Bose-O’Reilly, S. Exposure assessment of toxic metals and organochlorine pesticides among employees of a natural history museum. Environ. Res. 2020, 184, 11. [Google Scholar] [CrossRef]
- Ilies, D.C.; Herman, G.V.; Safarov, B.; Ilies, A.; Blaga, L.; Caciora, T.; Peres, A.C.; Grama, V.; Bambang, S.W.; Brou, T.; et al. Indoor Air Quality Perception in Built Cultural Heritage in Times of Climate Change. Sustainability 2023, 15, 8284. [Google Scholar] [CrossRef]
- Boniek, D.; de Abreu, C.S.; dos Santos, A.F.B.; de Resende Stoianoff, M.A. Filamentous fungi in Brazilian indoor cultural heritage as potential risk to human health and biodeterioration of artworks. Air Qual. Atmos. Health 2022, 1–8. [Google Scholar] [CrossRef]


| (Year) [Reference] | Conflict of Interest and Funding | Participants’ Characteristics (Age and Years of Exposure) | Environmental Conditions | Experimental Protocol | Risk Factors | Key Outcomes (Symptoms and Diseases) | Preventive Measures |
|---|---|---|---|---|---|---|---|
| Fischbein, A.; Wallace, J.; Anderson, K.E.; et al. (1982) [16] | Funded by National Institute of Environmental Health Sciences Center | 43 years old (female) Exposure—six weeks Art conservator | Studio Poorly ventilated room New York City | Routine gynecologic examination, physical examination, Hospitalized for chelation therapy with disodium calcium edetic acid | Exposure to lead | Fatigue, dizziness, diffuse muscle pain in upper and lower extremities, intermittent burning pain in the left upper quadrant of the abdomen, epigastric discomfort and crampy abdominal pain unrelated to eating Elevated blood lead levels (up to 130 mg/dL) |
|
| Varnai, V.M.; Macan, J.; Prester, L; et al. (2011) [7] | Funded by Ministry of Science and Technology of the Republic of Croatia | 147 recruited controls (29 men) Age in years, mean (38.6) Exposure—six, five years 56 recruited restorers (22 men) Age in years, mean (37.6) Exposure—6 years | Two Croatian institutions Control group: insurance company and librarians Restorers: in restoration and conservation laboratory | Medical interview, physical examination and medical examinations (venous blood sampling for total IgE measurement, skin prick testing to common inhalational allergens, non-specific bronchial challenge test) Simple questionnaire: medical history (smoking habit, years of working exposure, exposure to dust and chemicals at the workplace and data on ever experienced respiratory symptoms compatible with diagnoses of rhinitis and asthma | Exposure to volatile solvents hydrocarbons, ketones, esters and alcohols | More than two times higher prevalence of nasal hyperresponsiveness to histamine was found in restorers and conservators of cultural heritage compared to control subjects; no deterioration of lung function | Not mentioned |
| Ribeiro, Pa.A; Girão, F.; Henriques, P; et al. (2011) [12] | Not mentioned | 47 years old (man) Exposure—three weeks Restorer of religious art | Not mentioned During three weeks | Imaging studies, lung function tests, bronchoalveolar lavage, lung biopsy, treatment with Prednisolone 40 mg, follow-up computed tomography scan | Exposure to golden dust | Asthenia, myalgia, dry cough, fever, crackles in lung bases, hypoxemia and elevation of inflammatory markers, pneumonia |
|
| Kanceljak-Macan, B.; Trošíc, I.; Varnai, V. M.; et al. (2012) [17] | Funded by medical research and Occupational Health, Zagreb | 22 restorers (10 men) Exposure—five years 48 control workers (27 men) Exposure—six years | Two Croatian institutions Control group: without lower respiratory symptoms and with normal ventilatory parameters | Medical interview, physical examination, spirometry, skin prick testing to inhalator allergens | Chemical exposure varied according to restoration/conservation activity, but all the subjects reported being exposed to mixture of organic solvents, including 95% ethanol, acetone, benzine, white spirit, toluene and xylene, and the majority of them were also exposed to turpentine, ammonia, perchlorethylene, fungicides, vinyl polymers and epoxy resins | Restorers: Male: a higher percentage of neutrophils (34 vs. 15.5%), Female: lower proportion of neutrophils in sputum | Not mentioned |
| Langford, M., Beaumont, M. S., & Annett, D. (2013) [9] | Not mentioned | Textile conservators | Historic Royal Palaces (HRP) collections in the UK Average of 15 years of experience | Observation of work postures, analysis of accident and absenteeism records, ergonomic questionnaire and ergonomics workshop | 1. Manually handle loads (moving rolled tapestries to and from the store weighing around 100 kg); Chairs without footrests. | Musculoskeletal disorders (MSDs), lower back pain, neck pain, upper limb pain due to static postures and repetitive movements |
|
| Górny, R. L.; Harkawy, A. S.; Lawniczek-Walczyk, A.; et al. (2016) [10] | Not mentioned | Workers not defined | Nine naturally ventilated conservation laboratories with no history of water damage | Viable bioaerosol stationary samples were collected in both outdoor and indoor environments using 6-stage Andersen impactor Stationary and personal indoor bioaerosol measurements were carried out using both Gesamtstaubprobenahme an der Person and Button filter samplers, simple questionnaire | Exposure to microbiological agents | Headaches, fatigue, eye and throat irritation, as well as rhinorrhea and allergic inflammation |
|
| Costa-Moreira, P.; Coelho, R.; Pita, I.; et al. (2019) [18] | Not mentioned | 39 years old (male) Exposure—five months Art conservator | In an early 20th-century church | Physical examination, the blood tests, abdominal radiographs, tomography, a colonic pseudo-obstruction, an upper endoscopy, a colonoscopy and a liver biopsy, chelation with calcium disodium edetate was started at a dose of 20 mg/kg/d | Exposure to lead | Abdominal pain, constipation, irritability, concentration difficulties, decreased libido and sexual impotence, pseudo-obstruction, hemolytic anemia and abnormal liver chemistries | Not mentioned |
| Deering, K.; Spegel, E.; Quaisser, C.; et al. (2020) [19] | Funded by the Deutsche Bundesstiftung Umwelt DBU | 28 museum employees (20 men) between 27 and 65 years of age Exposure—six months, worked at least ten hours per week | In Museum für Naturkunde Berlin | Two blood samples and five urine samples were taken from each participant (during a working week), a questionnaire (work activity, exposure and information on fish and seafood intakes) | Exposure to arsenic, mercury and organochlorine pesticides | Cancer such as bladder, lung, liver, kidney, skin cancer, affect the development processes of infants during the prenatal and early postnatal period, the nervous, respiratory, immune, cardiovascular and endocrine system with various health issues |
|
| Pinheiro, A. C., & Ramos, A. (2021) [4] | Funded by the Foundation for Science and Technology | 6 textile conservators in Portugal, aged 39–62 years, experience ranging from 12 to 40 years | Textile conservation workshops; long hours in static postures; strenuous tasks such as textile consolidation | Nordic Musculoskeletal Questionnaire, Quick Exposure Check (QEC) to assess ergonomic risk | 1. Incorrect postures on the tapestry looms; Workers used wooden chair made specifically for the textile department in the 1980s–1990s. | Neck pain, back, shoulder and hand/wrist pain |
|
| Ilies, D.C.; Herman, G.V.; Safarov, B. et al. (2023) [20] | Funded by the Deanship of Scientific Research | Visitors and employees (250 respondents—108 men) | In Darvas-La Roche Museum House (Romania) Too low temperature, dry, unventilated air, as well as a large amount of dust in suspension | Questionnaire with 11 items (of the indoor environment and experienced symptoms of illness) September 2023–March 2023 | The air quality | Disease symptoms (nasal congestion, eye and skin irritations, coughs, migraines, frequent colds, etc.) and/or discomfort sensations (dry air, excess humidity, unpleasant smells, etc.) | Not mentioned |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferreira, M.R.; Brito, A.V.; Fernandes, R.J. Occupational Diseases in Art Conservators and Restorers: A Systematic Review. Healthcare 2025, 13, 819. https://doi.org/10.3390/healthcare13070819
Ferreira MR, Brito AV, Fernandes RJ. Occupational Diseases in Art Conservators and Restorers: A Systematic Review. Healthcare. 2025; 13(7):819. https://doi.org/10.3390/healthcare13070819
Chicago/Turabian StyleFerreira, Maria R., André V. Brito, and Ricardo J. Fernandes. 2025. "Occupational Diseases in Art Conservators and Restorers: A Systematic Review" Healthcare 13, no. 7: 819. https://doi.org/10.3390/healthcare13070819
APA StyleFerreira, M. R., Brito, A. V., & Fernandes, R. J. (2025). Occupational Diseases in Art Conservators and Restorers: A Systematic Review. Healthcare, 13(7), 819. https://doi.org/10.3390/healthcare13070819


_Rachiotis.png)





