Epidemiology of Traumatic Injuries at a Single Regional Trauma Center in South Korea: Age-Specific and Temporal Trends (2014–2023)
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Source
2.3. Patient Stratification and Injury Classification
2.4. Statistical Analysis
3. Results
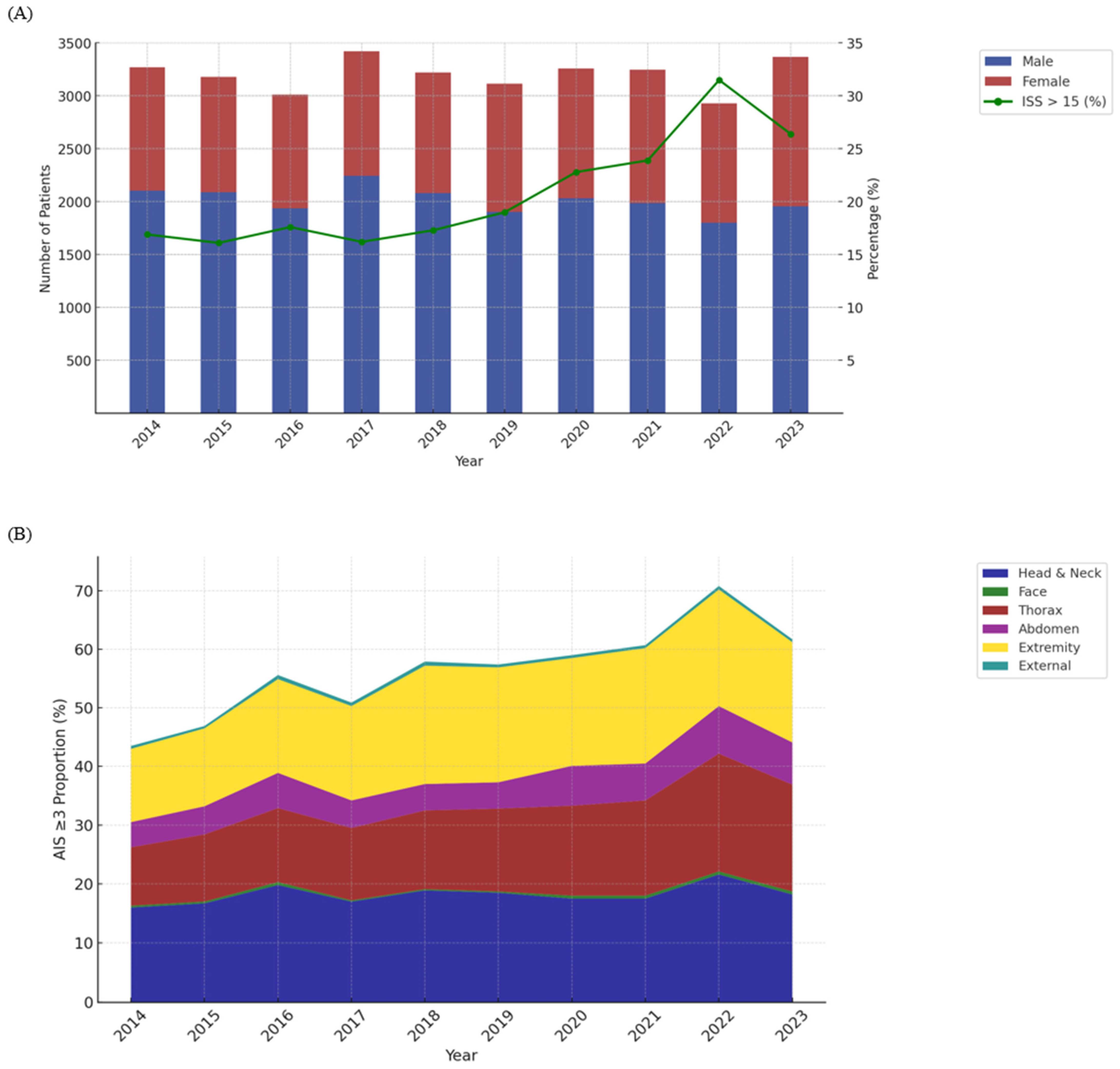
3.1. Patient Demographics
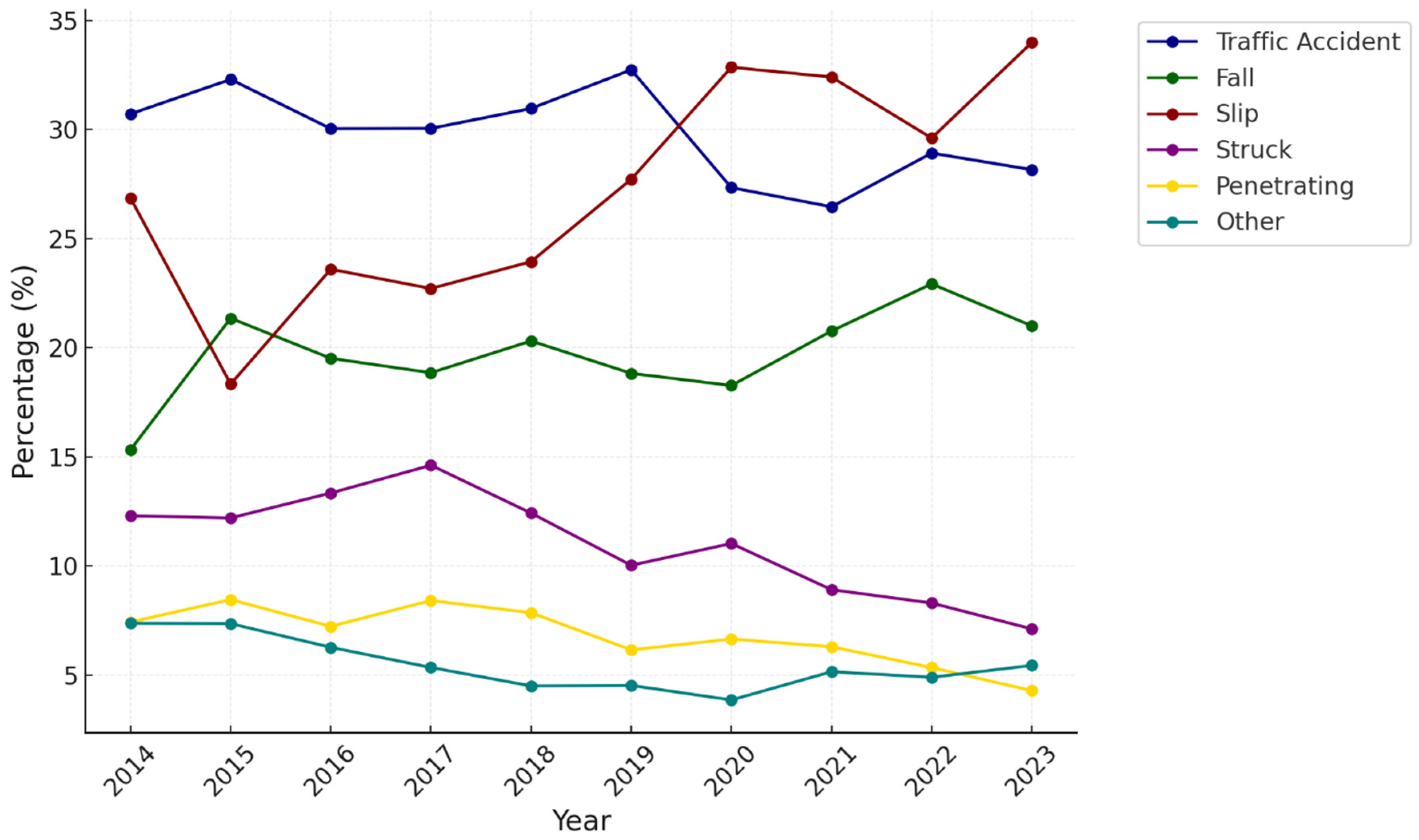
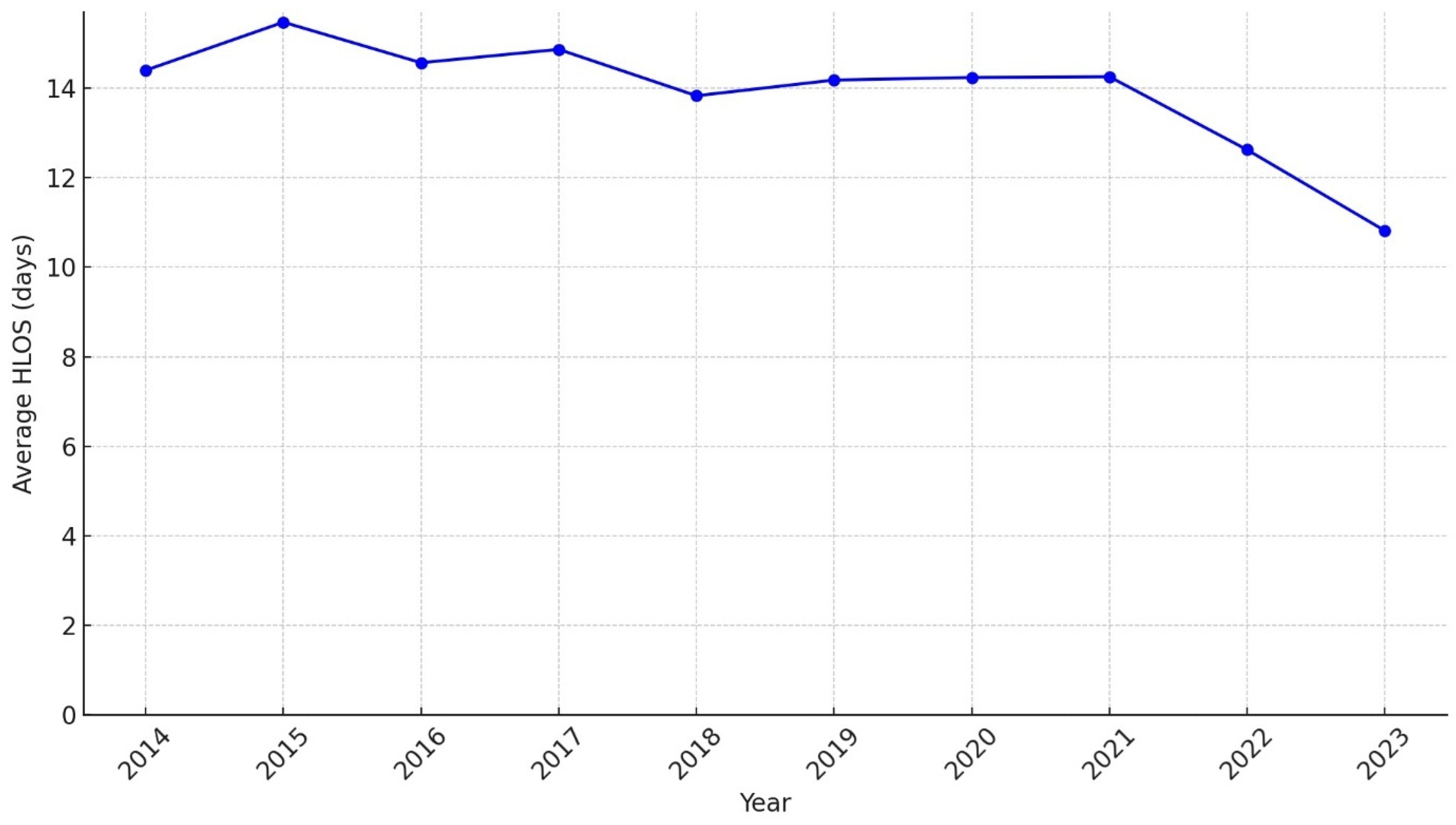
3.2. Yearly Trends
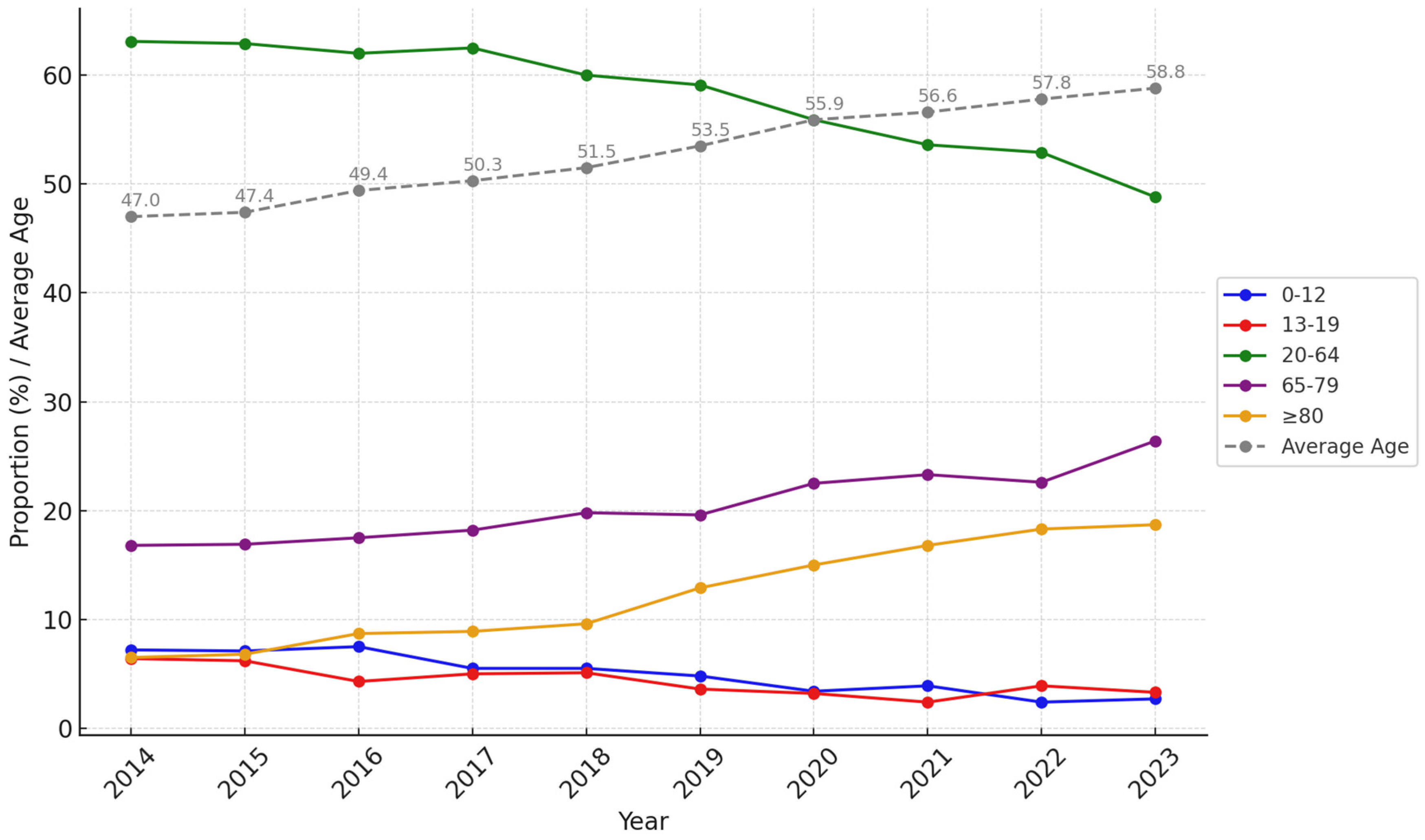
3.3. Age Group
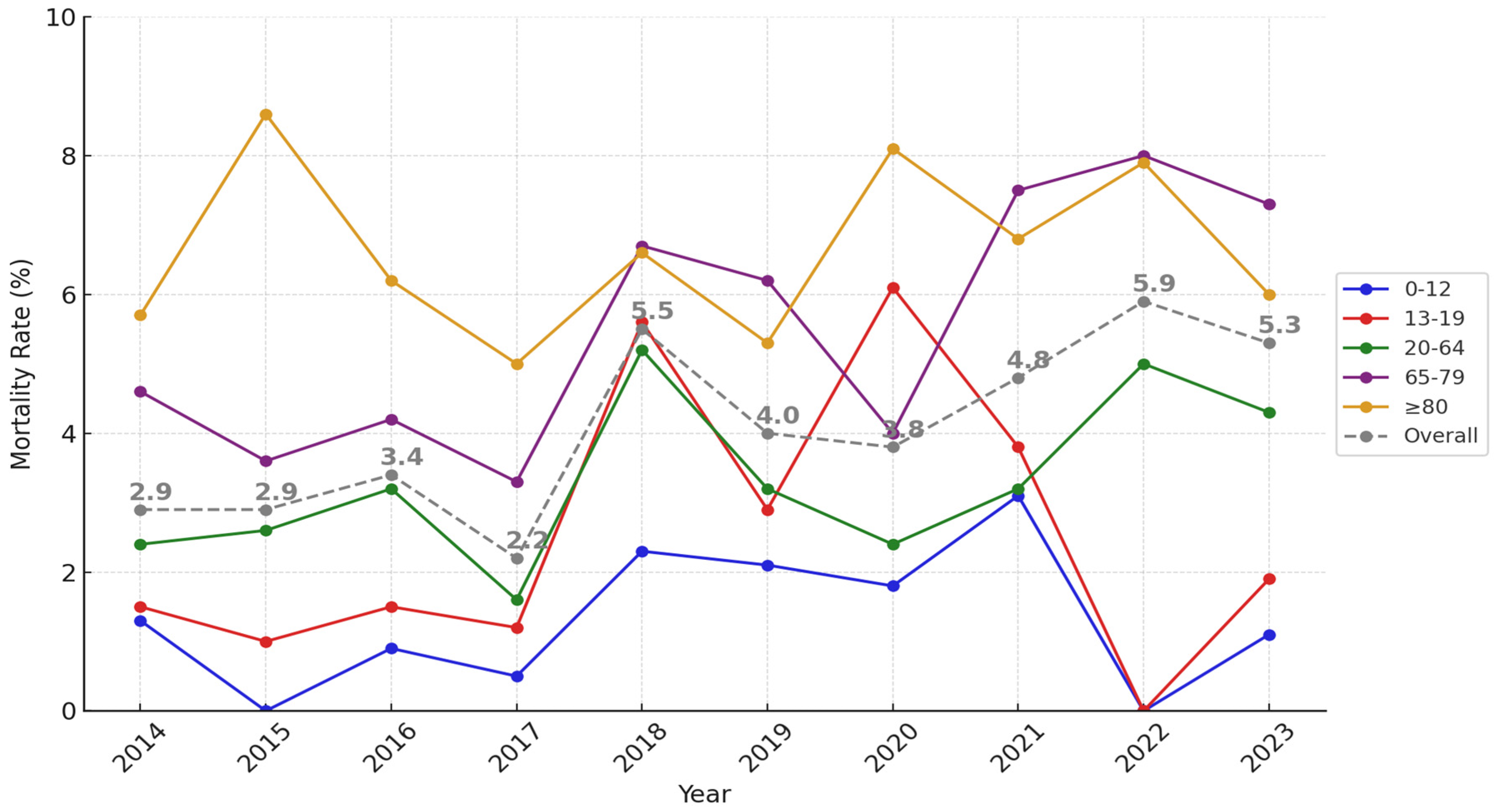
3.4. Mortality
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ANOVA | analysis of variance |
| CPR | Cardiopulmonary resuscitation |
| ED | Emergency department |
| HLOS | Hospital length of stay |
| IQR | Interquartile range |
| IRB | Institutional review board |
| ISS | Injury Severity Score |
| KTDB | Korean Trauma Database |
| OECD | Organization for Economic Cooperation and Development |
| SPSS | Statistical Package for the Social Sciences |
References
- Murphy, S.L.; Kochanek, K.D.; Xu, J.; Arias, E. Mortality in the United States, 2023. NCHS Data Brief 2024, 521, CS356116. [Google Scholar]
- Søreide, K.; Krüger, A.J.; Vårdal, T.; Lund, C.G.; Enger, M.; Søreide, E.; Lossius, H.M. Epidemiology and Contemporary Patterns of Trauma Deaths: Changing Place, Similar Pace, Older Face. World J. Surg. 2007, 31, 2092–2103. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Li, Z.; Li, X.; Zhang, J.; Zheng, L.; Jiang, C.; Li, J. Study on the Trend and Disease Burden of Injury Deaths in Chinese Population, 2004–2010. PLoS ONE 2014, 9, e85319. [Google Scholar] [CrossRef]
- World Health Organization. Global Status Report on Road Safety 2023; World Health Organization: Geneva, Switzerland, 2023. [Google Scholar]
- Alberdi, F.; García, I.; Atutxa, L.; Zabarte, M.; Trauma and Neurointensive Care Work Group of the SEMICYUC. Epidemiology of Severe Trauma. Med. Intensiva 2014, 38, 580–588. [Google Scholar] [CrossRef]
- Kwon, J.; Lee, M.; Moon, J.; Huh, Y.; Song, S.; Kim, S.; Lee, S.J.; Lim, B.; Kim, H.J.; Kim, Y.; et al. National Follow-Up Survey of Preventable Trauma Death Rate in Korea. J. Korean Med. Sci. 2022, 37, e349. [Google Scholar] [CrossRef]
- Jung, I.H.; Yun, J.H.; Lee, S.K. Preventable Trauma Death Rate in South Korea. Korean J. Neurotrauma 2023, 19, 4–5. [Google Scholar] [CrossRef]
- Im, J.; Seo, E.W.; Jung, K.; Kwon, K. Understanding Regional Trauma Centers and Managing a Trauma Care System in South Korea: A Systematic Review. Ann. Surg. Treat. Res. 2023, 104, 61–70. [Google Scholar] [CrossRef]
- Park, Y.; Chung, M.; Lee, G.J.; Lee, M.A.; Park, J.J.; Choi, K.K.; Hyun, S.Y.; Jeon, Y.B.; Ma, D.S.; Yoon, Y.C.; et al. Characteristics of Korean Trauma Patients: A Single-Center Analysis Using the Korea Trauma Database. J. Trauma Inj. 2016, 29, 155–160. [Google Scholar] [CrossRef][Green Version]
- Yu, B.; Lee, G.; Lee, M.A.; Choi, K.; Hyun, S.; Jeon, Y.; Yoon, Y.C.; Lee, J. Trauma Volume and Performance of a Regional Trauma Center in Korea: Initial 5-Year Analysis. J. Trauma Inj. 2020, 33, 31–37. [Google Scholar] [CrossRef]
- Bazzoli, G.J.; Meersman, P.J.; Chan, C. Factors That Enhance Continued Trauma Center Participation in Trauma Systems. J. Trauma 1996, 41, 876–885. [Google Scholar] [CrossRef]
- Ziran, B.H.; Barrette-Grischow, M.K.; Hileman, B. United States Level I Trauma Centers Are Not Created Equal—A Concern for Patient Safety? Patient Saf. Surg. 2008, 2, 18. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lundy, D.W.; Harvey, E.J.; Jahangir, A.A.; Leighton, R.K. Trauma Systems in North America. OTA Int. 2019, 2, e013. [Google Scholar] [CrossRef] [PubMed]
- Farmer, C.M. The Effects of Higher Speed Limits on Traffic Fatalities in the United States, 1993–2017. Insur. Inst. High. Saf. 2019. Available online: https://www.iihs.org/topics/bibliography/ref/2188 (accessed on 2 January 2025).
- Kokka, K.K.; Nightingale, G.; Williams, A.J.; Abbas, A.; Popov, V.; Sharp, S.; Hunter, R.F.; Jepson, R.; Woodcock, J. Effect of 20 mph Speed Limits on Traffic Injuries in Edinburgh, UK: A Natural Experiment and Modelling Study. J. Epidemiol. Community Health 2024, 78, 437–443. [Google Scholar] [CrossRef]
- Statistics Korea. Korean Social Trends 2023; Statistics Korea: Daejeon, Republic of Korea, 2023; pp. 69–70. [Google Scholar]
- Lee, M.S.; Jhone, J.H.; Kim, J.B.; Kweon, Y.S.; Hong, H.J. Characteristics of Korean Children and Adolescents Who Die by Suicide Based on Teachers’ Reports. Int. J. Environ. Res. Public Health 2022, 19, 6812. [Google Scholar] [CrossRef]
- Ajluni, V.; Amarasinghe, D. Youth Suicide Crisis: Identifying At-Risk Individuals and Prevention Strategies. Child Adolesc. Psychiatry Ment. Health 2024, 18, 58. [Google Scholar] [CrossRef]
- Wyman, P.A. Developmental Approach to Prevent Adolescent Suicides: Research Pathways to Effective Upstream Preventive Interventions. Am. J. Prev. Med. 2014, 47, S251–S256. [Google Scholar] [CrossRef]
- Robinson, J.; Bailey, E.; Witt, K.; Stefanac, N.; Milner, A.; Currier, D.; Pirkis, J.; Condron, P.; Hetrick, S. What Works in Youth Suicide Prevention? A Systematic Review and Meta-Analysis. EClinicalMedicine 2018, 4, 52–91. [Google Scholar] [CrossRef]
- Kim, S.Y.; Hong, K.J.; Shin, S.D.; Ro, Y.S.; Ahn, K.O.; Kim, Y.J.; Lee, E.J. Validation of the Shock Index, Modified Shock Index, and Age Shock Index for Predicting Mortality of Geriatric Trauma Patients in Emergency Departments. J. Korean Med. Sci. 2016, 31, 2026–2032. [Google Scholar] [CrossRef]
- Kim, J.G.; Choi, H.Y.; Kang, G.H.; Jang, Y.S.; Kim, W.; Lee, Y.; Ahn, C. Prognostic Association Between Injury Severity Score and the Outcomes of Elderly Patients with Trauma in South Korea. J. Pers. Med. 2024, 14, 674. [Google Scholar] [CrossRef]
- Bennett, K.M.; Scarborough, J.E.; Vaslef, S. Outcomes and Health Care Resource Utilization in Super-Elderly Trauma Patients. J. Surg. Res. 2010, 163, 127–131. [Google Scholar] [CrossRef] [PubMed]
- Ruff, S.; Royster, W.; Bholat, O.; Bank, M.; Kohn, N.; Georgiades, M. Pattern of Injury and Outcomes of Trauma in the Super-Elderly. Crit. Care Med. 2018, 46, 793. [Google Scholar] [CrossRef]
- Hashmi, A.; Ibrahim-Zada, I.; Rhee, P.; Aziz, H.; Fain, M.J.; Friese, R.S.; Joseph, B. Predictors of Mortality in Geriatric Trauma Patients: A Systematic Review and Meta-Analysis. J. Trauma Acute Care Surg. 2014, 76, 894–901. [Google Scholar] [CrossRef] [PubMed]
- Savioli, G.; Ceresa, I.F.; Macedonio, S.; Gerosa, S.; Belliato, M.; Luzzi, S.; Lucifero, A.G.; Manzoni, F.; Ricevuti, G.; Bressan, M.A. Major Trauma in Elderly Patients: Worse Mortality and Outcomes in an Italian Trauma Center. J. Emerg. Trauma Shock 2021, 14, 98–103. [Google Scholar] [CrossRef]
- Molendijk-van Nieuwenhuyzen, K.; Belt-van Opstal, R.; Hakvoort, L.; Dikken, J. Exploring Geriatric Trauma Unit Experiences Through Patients’ Eyes: A Qualitative Study. BMC Geriatr. 2024, 24, 476. [Google Scholar] [CrossRef]
- Bérubé, M.; Pasquotti, T.; Klassen, B.; Brisson, A.; Tze, N.; Moore, L. Implementation of the Best Practice Guidelines on Geriatric Trauma Care: A Canadian Perspective. Age Ageing 2020, 49, 227–232. [Google Scholar] [CrossRef]
- Neupane, I.; Mujahid, N.; Zhou, E.P.; Monteiro, J.F.G.; Lueckel, S.; Cizginer, S.; Yildiz, F.; Raza, S.; Singh, M.; Gravenstein, S.; et al. A Model of Care to Improve Survival of Older Trauma Patients: Geriatrics Comanagement. J. Gerontol. A Biol. Sci. Med. Sci. 2023, 78, 1212–1218. [Google Scholar] [CrossRef]
- Wintz, D.; Schaffer, K.B.; Hites, J.J.; Wybourn, C.; Bui, E.H.; Langness, S.; Hamel, M.; Wright, K.; Frey, J.R. GIFTS: Geriatric Intensive Functional Therapy Sessions for the Older Trauma Patient. J. Trauma Acute Care Surg. 2024, 97, 197–204. [Google Scholar] [CrossRef]
- Craig, H.A.; Lowe, D.J.; Khan, A.; Paton, M.; Gordon, M.W.G. Exploring the Impact of Traumatic Injury on Mortality: An Analysis of the Certified Cause of Death Within One Year of Serious Injury in the Scottish Population. Injury 2024, 55, 111470. [Google Scholar] [CrossRef]
- Carenzo, L.; Mercalli, C.; Reitano, E.; Tartaglione, M.; Ceolin, M.; Cimbanassi, S.; Del Fabbro, D.; Sammartano, F.; Cecconi, M.; Coniglio, C.; et al. State of the Art of Trauma Teams in Italy: A Nationwide Study. Injury 2024, 55, 111388. [Google Scholar] [CrossRef]
- Crandall, M.; Zarzaur, B.; Tinkoff, G. American Association for the Surgery of Trauma Prevention Committee Topical Overview: National Trauma Data Bank, Geographic Information Systems, and Teaching Injury Prevention. Am. J. Surg. 2013, 206, 709–713. [Google Scholar] [CrossRef] [PubMed]
- Acharya, P.; Amin, A.; Nallamotu, S.; Riaz, C.Z.; Kuruba, V.; Senthilkumar, V.; Kune, H.; Bhatti, S.S.; Moguel Sarlat, I.; Krishna, C.V.; et al. Prehospital Tranexamic Acid in Trauma Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Front. Med. 2023, 10, 1284016. [Google Scholar] [CrossRef]
- Mazzei, M.; Donohue, J.K.; Schreiber, M.; Rowell, S.; Guyette, F.X.; Cotton, B.; Eastridge, B.J.; Nirula, R.; Vercruysse, G.A.; O’Keeffe, T.; et al. Prehospital Tranexamic Acid Is Associated with a Survival Benefit Without an Increase in Complications: Results of Two Harmonized Randomized Clinical Trials. J. Trauma Acute Care Surg. 2024, 97, 697–702. [Google Scholar] [CrossRef] [PubMed]
- Pusateri, A.E.; Moore, E.E.; Moore, H.B.; Le, T.D.; Guyette, F.X.; Chapman, M.P.; Sauaia, A.; Ghasabyan, A.; Chandler, J.; McVaney, K.; et al. Association of Prehospital Plasma Transfusion with Survival in Trauma Patients with Hemorrhagic Shock When Transport Times Are Longer Than 20 Minutes: A Post Hoc Analysis of the PAMPer and COMBAT Clinical Trials. JAMA Surg. 2019, 155, e195085. [Google Scholar] [CrossRef]
- Deeb, A.P.; Guyette, F.X.; Daley, B.J.; Miller, R.S.; Harbrecht, B.G.; Claridge, J.A.; Phelan, H.A.; Eastridge, B.J.; Joseph, B.; Nirula, R.; et al. Time to Early Resuscitative Intervention Association with Mortality in Trauma Patients at Risk for Hemorrhage. J. Trauma Acute Care Surg. 2023, 94, 504–512. [Google Scholar] [CrossRef]
- Chio, J.C.T.; Piehl, M.; De Maio, V.J.; Simpson, J.T.; Matzko, C.; Belding, C.; Broome, J.M.; Duchesne, J. A Circulation-First Approach for Resuscitation of Trauma Patients with Hemorrhagic Shock. Shock 2023, 59, 1–4. [Google Scholar] [CrossRef]
| Characteristics | All Patients (n = 32,025) |
|---|---|
| Age, years, mean ± SD | 52.8 ± 22.2 |
| Male, n (%) | 20,138 (62.9) |
| Mechanism, n (%) | |
| Traffic accident | 9019 (29.9) |
| Fall | 5923 (19.6) |
| Slip | 8134 (26.9) |
| Struck by object | 3378 (11.2) |
| Penetrating | 2084 (6.9) |
| Others | 1664 (5.5) |
| Season, n (%) | |
| Spring | 7906 (24.7) |
| Summer | 8168 (25.5) |
| Autumn | 8590 (26.8) |
| Winter | 7361 (23.0) |
| Time of week, n (%) | |
| Weekdays | 22,523 (70.3) |
| Weekends | 9502 (29.7) |
| Times of the day, n (%) | |
| Morning | 12,078 (37.7) |
| Evening | 13,747 (42.9) |
| Night | 6200 (19.4) |
| Type of arrival to hospital, n (%) | |
| Direct | 22,358 (70.2) |
| Transfer | 9474 (29.8) |
| Initial triage, n (%) | |
| Trauma bay | 10,711 (33.4) |
| ER | 21,314 (66.6) |
| Initial Vital signs | |
| SBP, mmHg, mean ± SD | 138.4 ± 30.4 |
| HR, bpm, mean ± SD | 86.8 ± 18.5 |
| RR, breaths/min, mean ± SD | 20.2 ± 3.4 |
| GCS, median [IQR] | 15 [15–15] |
| AIS ≥ 3, n (%) | |
| Head and Neck ≥ 3 | 5800 (18.1) |
| Face ≥ 3 | 117 (0.4) |
| Thorax ≥ 3 | 4581 (14.3) |
| Abdomen ≥ 3 | 1829 (5.7) |
| Extremity ≥ 3 | 5478 (17.1) |
| External ≥ 3 | 171 (0.5) |
| Injury Severity Parameter | |
| ISS, median [IQR] | 9 [4–13] |
| 1–8, n (%) | 14,647 (48.5) |
| 9–15, n (%) | 9416 (31.1) |
| 16–24, n (%) | 3420 (11.3) |
| ≥25, n (%) | 2748 (9.1) |
| Hospital LOS, days mean ± SD | 13.9 ± 16.8 |
| Discharge disposition, n (%) | |
| Home | 17,099 (53.6) |
| Transfer to another hospital | 12,761 (40.0) |
| DOA (including death at ER) | 774 (2.4) |
| Expired (after admission) | 1256 (3.9) |
| Characteristics | Age Groups | p Value | ||||
|---|---|---|---|---|---|---|
| 0–12 | 13–19 | 20–64 | 65–79 | ≥80 | ||
| Male, n (%) | 1037 (64.7) | 1024 (73.7) | 13,369 (71.9) | 3417 (52.3) | 1291 (33.1) | <0.001 |
| Mechanism, n (%) | <0.001 | |||||
| Traffic accident | 378 (24.1) | 585 (43.0) | 5905 (33.1) | 1672 (27.9) | 479 (13.9) | |
| Fall | 483 (30.8) | 205 (15.1) | 3613 (20.2) | 1102 (18.4) | 520 (15.1) | |
| Slip | 300 (19.1) | 174 (12.8) | 3053 (17.1) | 2418 (40.4) | 2189 (63.6) | |
| Struck by object | 228 (14.5) | 173 (12.7) | 2566 (14.3) | 345 (5.8) | 79 (2.2) | |
| Penetrating | 78 (5.0) | 149 (10.9) | 1679 (9.4) | 153 (2.6) | 25 (0.7) | |
| Others | 101 (6.4) | 76 (5.6) | 1040 (5.8) | 297 (4.9) | 153 (4.4) | |
| Injury Severity Parameter | ||||||
| ISS, median [IQR] | 4 [2–5] | 4 [2–10] | 6 [4–14] | 9 [4–14] | 9 [5–10] | <0.001 |
| ISS > 15, n (%) | 125 (7.9) | 238 (17.5) | 3936 (22.0) | 1349 (22.6) | 520 (15.2) | <0.001 |
| Hospital LOS, days mean ± SD | 5.3 ± 8.9 | 11.2 ± 15.2 | 14.3 ± 18.0 | 15.2 ± 16.3 | 14.6 ± 13.9 | <0.001 |
| Discharge disposition, n (%) | ||||||
| Home | 1274 (79.6) | 946 (68.3) | 10,030 (54.2) | 3179 (48.9) | 1670 (42.9) | <0.001 |
| Characteristics | Total (n) | Death (n) | Mortality Rate (%) |
|---|---|---|---|
| Age group | |||
| 0–12 | 1588 | 20 | 1.3 |
| 13–19 | 1352 | 32 | 2.4 |
| 20–64 | 18,076 | 584 | 3.2 |
| 65–79 | 6390 | 364 | 5.7 |
| ≥80 | 3830 | 255 | 6.7 |
| Mechanism | |||
| Traffic accident | 8762 | 409 | 4.7 |
| Fall | 5522 | 304 | 5.5 |
| Slip | 8126 | 261 | 3.2 |
| Struck by object | 3345 | 35 | 1.0 |
| Penetrating | 2053 | 27 | 1.3 |
| Others | 1623 | 109 | 6.7 |
| ISS | |||
| 1–8 | 14,503 | 79 | 0.5 |
| 9–15 | 9202 | 165 | 1.8 |
| 16–24 | 3202 | 222 | 6.9 |
| ≥25 | 2565 | 677 | 26.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jeon, S.; Lee, G.-J.; Lee, M.; Choi, K.-K.; Lee, S.-H.; Hyun, S.-Y.; Jeon, Y.-B.; Yu, B. Epidemiology of Traumatic Injuries at a Single Regional Trauma Center in South Korea: Age-Specific and Temporal Trends (2014–2023). Healthcare 2025, 13, 773. https://doi.org/10.3390/healthcare13070773
Jeon S, Lee G-J, Lee M, Choi K-K, Lee S-H, Hyun S-Y, Jeon Y-B, Yu B. Epidemiology of Traumatic Injuries at a Single Regional Trauma Center in South Korea: Age-Specific and Temporal Trends (2014–2023). Healthcare. 2025; 13(7):773. https://doi.org/10.3390/healthcare13070773
Chicago/Turabian StyleJeon, Sebeom, Gil-Jae Lee, Mina Lee, Kang-Kook Choi, Seung-Hwan Lee, Sung-Youl Hyun, Yang-Bin Jeon, and Byungchul Yu. 2025. "Epidemiology of Traumatic Injuries at a Single Regional Trauma Center in South Korea: Age-Specific and Temporal Trends (2014–2023)" Healthcare 13, no. 7: 773. https://doi.org/10.3390/healthcare13070773
APA StyleJeon, S., Lee, G.-J., Lee, M., Choi, K.-K., Lee, S.-H., Hyun, S.-Y., Jeon, Y.-B., & Yu, B. (2025). Epidemiology of Traumatic Injuries at a Single Regional Trauma Center in South Korea: Age-Specific and Temporal Trends (2014–2023). Healthcare, 13(7), 773. https://doi.org/10.3390/healthcare13070773





