Development, Implementation, and Evaluation of a ‘Virtual Patient’ with Chronic Low Back Pain: An Education Resource for Physiotherapy Students †
Abstract
1. Introduction
1.1. Aim
1.2. Objectives
- (a)
- Develop a virtual patient to simulate a clinical scenario that fosters a person-centred (biopsychosocial) line of enquiry during a consultation focusing on assessment, diagnosis and management of non-specific chronic low back pain.
- (b)
- Pilot the tool with pre-registration physiotherapy students to evaluate their ability and confidence to follow a person-centred (biopsychosocial) line of inquiry
- (c)
- Capture the attitudes and beliefs of the students on the value of the simulation as a learning tool, including (i) virtual learning environment, (ii) authenticity of the simulation, (iii) person-centred line of inquiry
2. Materials and Methods
2.1. Phase I: Development of the Virtual Clinical Simulation
- Designing and educational framework—the authorship team drew on their experience in higher education to agree on clear learning objectives that aligned the virtual tool with curriculum standards and effectively supported student learning outcomes.
- Character design—a realistic virtual patient with lifelike characteristics, behaviors, and medical history to enhance authenticity and engagement in the learning experience.
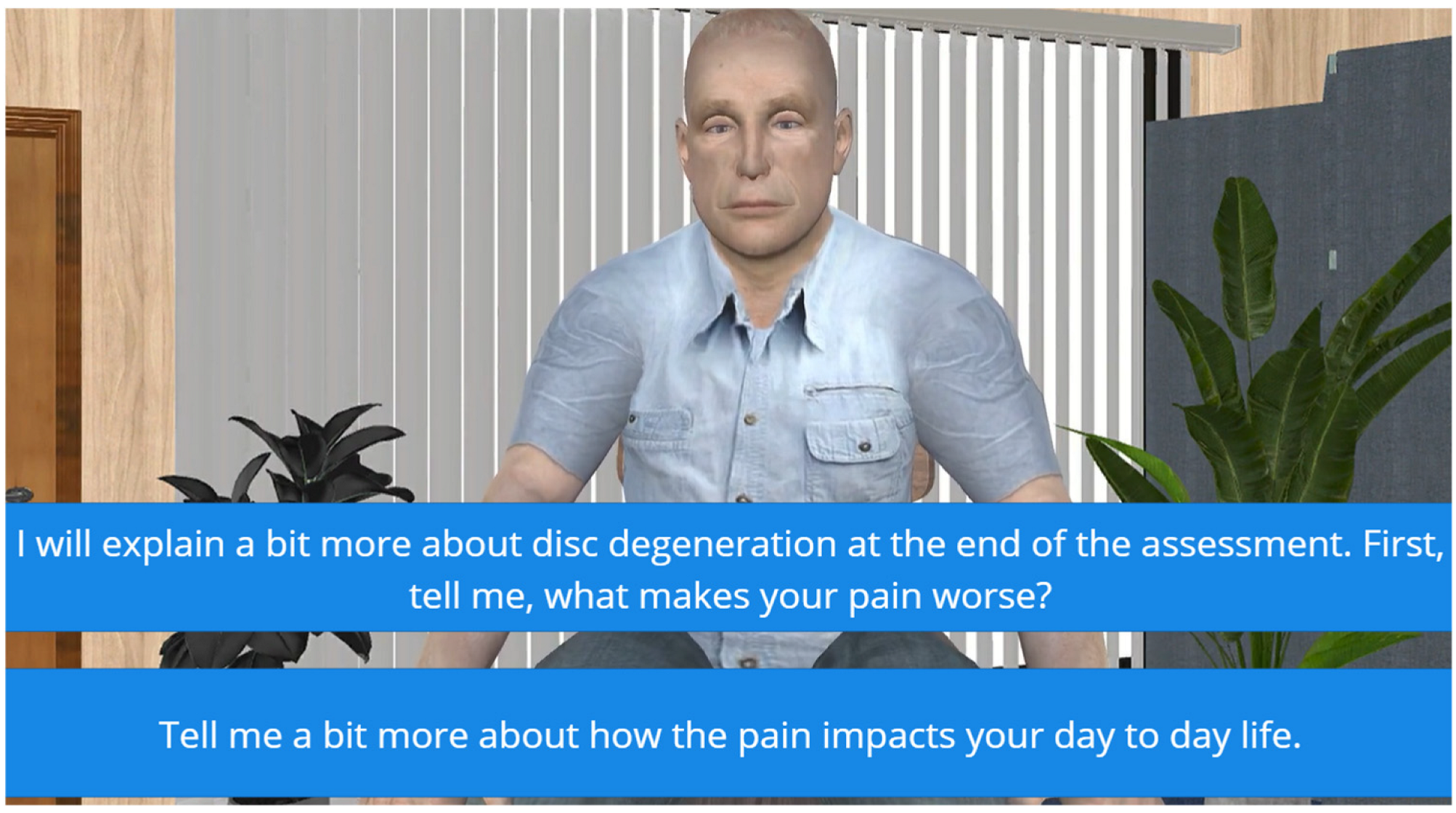
- Dialogue and question design—interactive dialogue, structured question flow, and adaptive responses were created to simulate a conversation between students and the virtual patient.
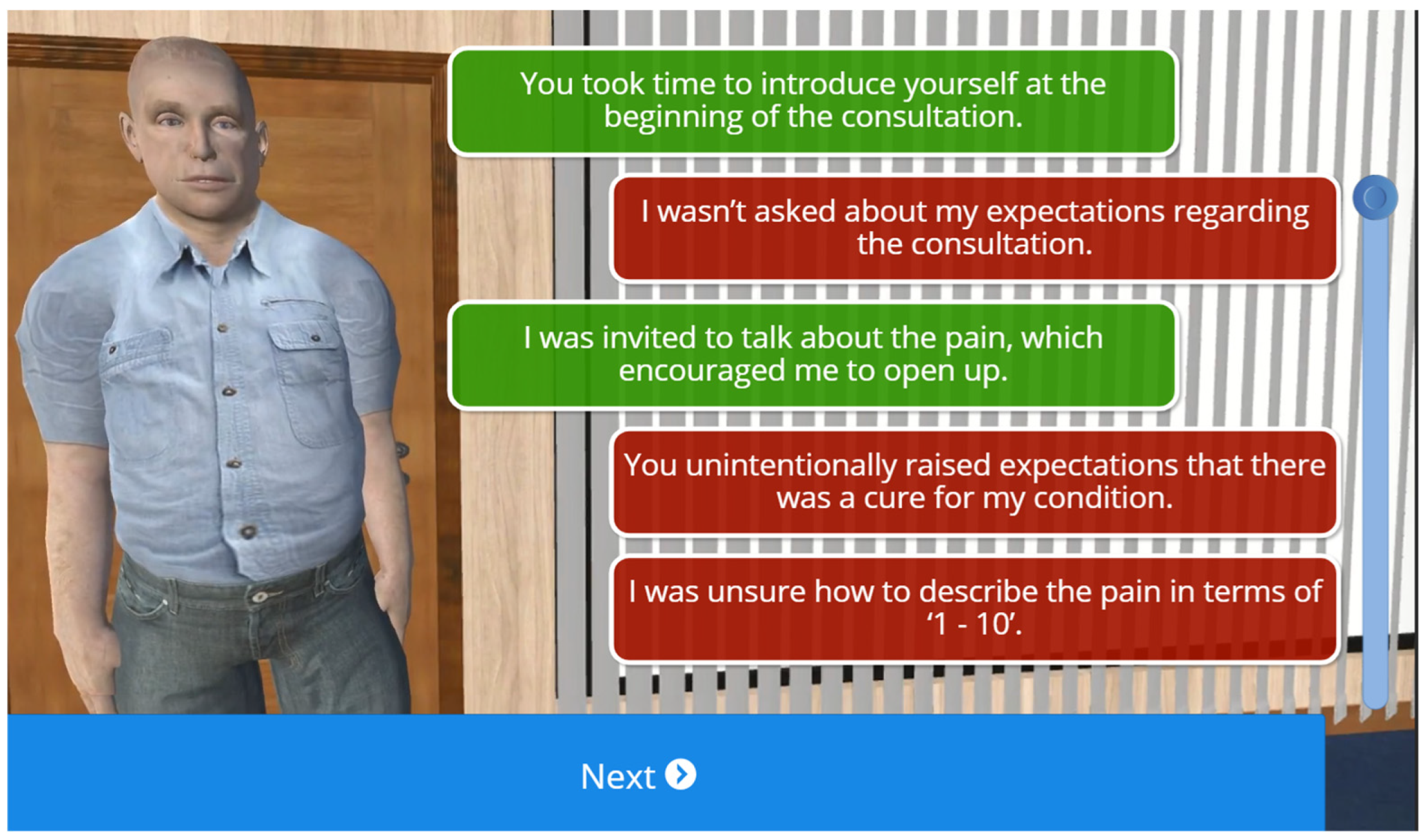
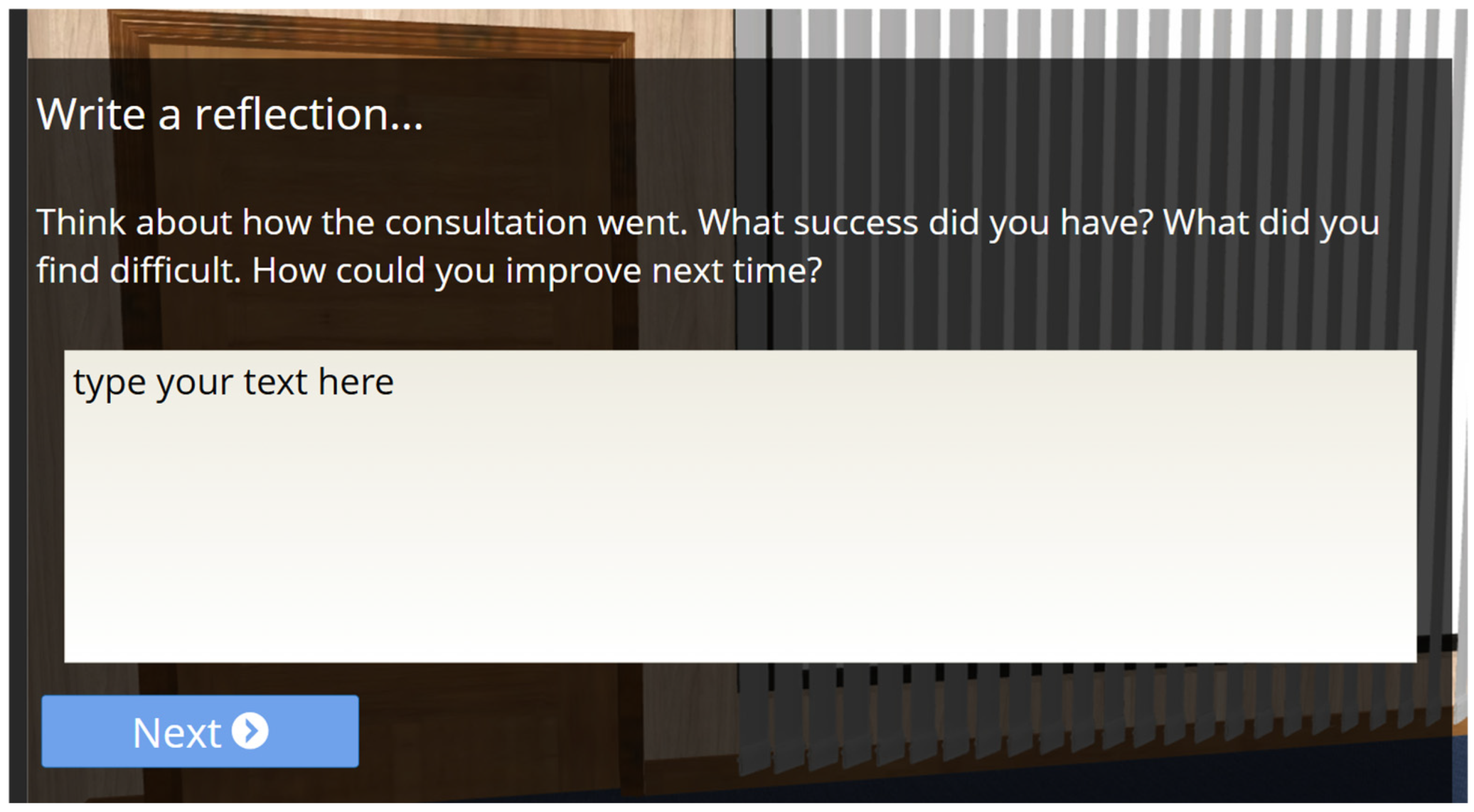
- Feedback and scoring system development—a structured feedback mechanism was designed that provided students with constructive insights based on their interactions, helping them refine their clinical reasoning and decision-making skills.
- Building the virtual tool—the e-platform was developed by integrating animation, sound, and an intuitive interface to create a user-friendly learning experience that enhances engagement and knowledge retention.
2.2. Phase II: Implementation and Evaluation
2.2.1. Implementation
- ▪ Step 1: Introduction to the session (10 min)
- ▪ Step 2: Working ‘alone’ with the virtual patient (30 min)
- ▪ Step 3: Working in small groups (30 min)
- ▪ Step 4: Educator-led full class debrief (45 min)
2.2.2. Evaluation
3. Results
3.1. Phase I: The Virtual Clinical Simulation
3.1.1. Educational Framework Design
- Students will conduct an interactive holistic clinical consultation with a virtual person experiencing chronic pain.
- Students will engage in a clinical consultation that explores biopsychosocial factors contributing to their pain experience.
- Students will practice in a safe, controlled, and supportive environment.
3.1.2. Character Design
3.1.3. Dialogue and Question Design
3.1.4. Technical Considerations
3.1.5. Feedback and Scoring System Design
3.2. Phase II: Implementation and Evaluation
3.2.1. Demographics
3.2.2. Frequency & Confidence in Selecting Person-Centred Questions
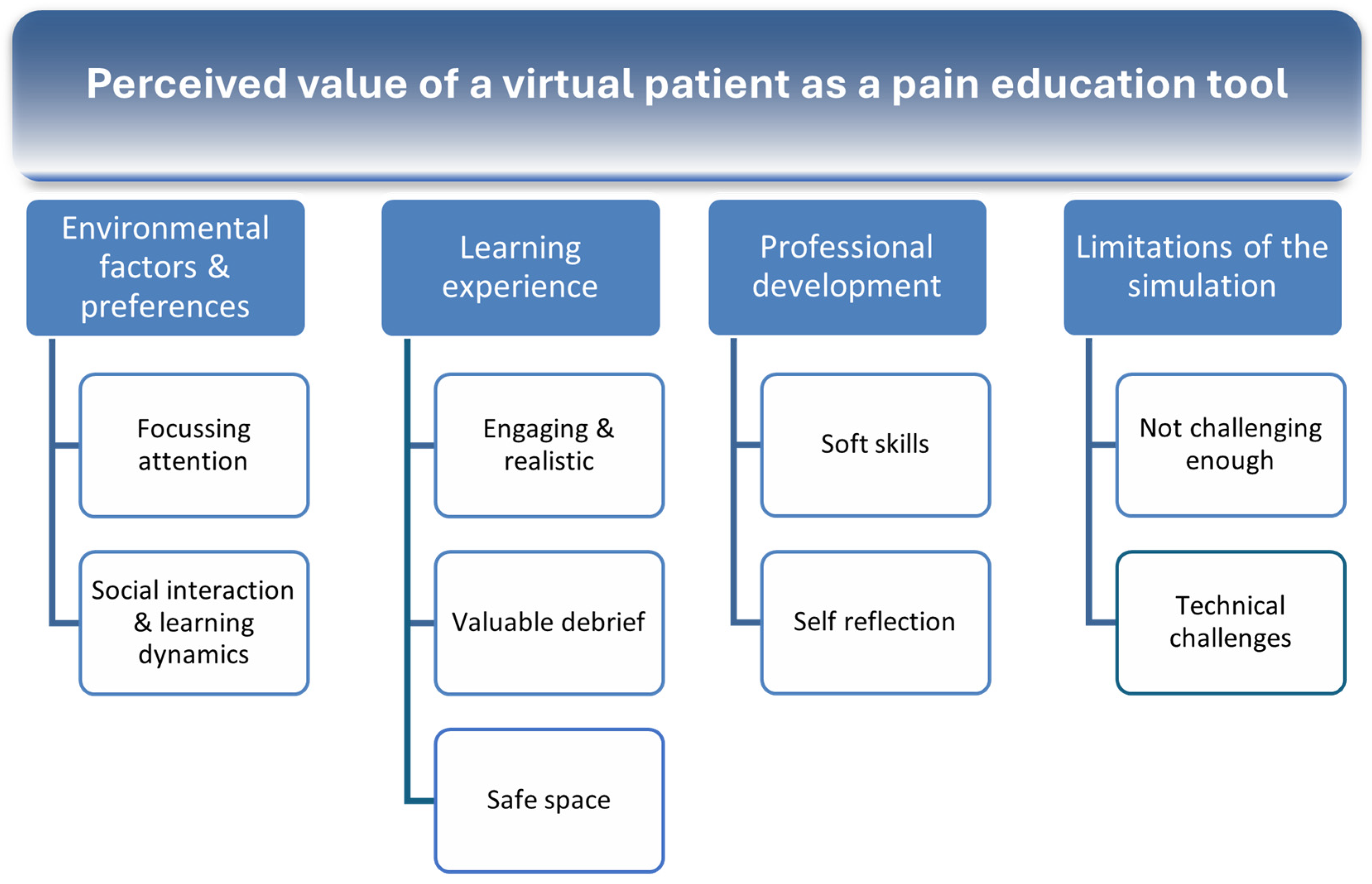
3.2.3. Analysis of Attitudes Towards the Value and Impact of Simulation
- (1)
- I enjoyed interacting with Paul [the virtual pain patient]—89.8% ‘strongly’ or ‘somewhat’ agreed
- (2)
- Interacting with Paul improved my understanding of complex subjective pain assessment—81.7% ‘strongly’ or ‘somewhat’ agreed
- (3)
- Interacting with Paul increased my confidence in dealing with complex subjective pain assessment—85.7% ‘strongly’ or ‘somewhat’ agreed
- (4)
- Interacting with Paul helped my understanding of the impact of biopsychosocial versus biomedical pain assessment—79.6% ‘strongly’ or ‘somewhat’ agreed
- (5)
- The on-screen instructions were clear—96% ‘strongly’ or ‘somewhat’ agreed
- (6)
- I could see how the activity would be relevant to my learning about pain—93.8% ‘strongly’ or ‘somewhat’ agreed
- (7)
- Paul was a believable character—93.9% ‘strongly’ or ‘somewhat’ agreed
- (8)
- The scenario seemed authentic—93.9% ‘strongly’ or ‘somewhat’ agreed
- (9)
- Practicing online with Paul gave me a safe space to practice my skills—93.9% ‘strongly’ or ‘somewhat’ agreed
- (10)
- Practicing online with Paul will help me prepare for clinical placement—87.8% ‘strongly’ or ‘somewhat’ agreed
- (1)
- I would like to repeat the activity with Paul several times—53% ‘strongly’ or ‘somewhat’ agreed
- (2)
- I found selecting person-centred questions challenging—42.8% ‘strongly’ or ‘somewhat’ agreed
3.2.4. Qualitative Analysis of Student Responses to Open Text Questions
3.3. Environmental Factors & Preferences
3.3.1. Focusing Attention
“Somewhere in a quiet environment, where you can focus on the questions with no distractions.” (BSc Physiotherapy student, Male, 22–34 years)
“Somewhere quiet, at home, may allow people to answer more honestly. But the classroom can also be quiet too. Some people may not want others to watch what they’re doing.” (MSc Physiotherapy student, Female, 22–34 years)
3.3.2. Social Interaction & Learning Dynamics
“In the classroom, it is really good to get feedback from other people and to change/rethink options.” (MSc Physiotherapy student, Male, 22–34 years)
“I liked coming in and completing [it] in the classroom with headphones as I find it easier to focus in person. However, it’s possible to complete it at home. It’s also good to have someone explain the simulation and have the opportunity to ask questions after.” (BSc Physiotherapy student, Male, 18–21 years)
“It was useful to have the class discussion afterwards.” (BSc Physiotherapy student, Female, 18–21 years)
3.4. Learning Experience
3.4.1. Engaging & Realistic
“It gave me ideas of questions to ask a complex pain patient as I feel it is hard to know what to say sometimes or how to word questions.” (BSc Physiotherapy student, Female, 18–21 years)
“Interacting with a real patient was more beneficial than just talking about it.” (MSc Physiotherapy student, Male, 22–34 years)
“It made it more relatable than a written case study. Seemed more like a real patient.” (BSc Physiotherapy student, Female, 18–21 years)
“It helped me understand a subject assessment of complex pain. Also helped me understand different ways of questioning to build trust.” (BSc Physiotherapy student, Male, 18–21 years)
3.4.2. Valuable Feedback and Debrief
“The discussion with others in big groups, is very valuable, especially then getting clinical feedback from the teacher.” (BSc Physiotherapy student, Female, 18–21 years)
“The feedback at the end from Paul, as it points out how specific lines of enquiry may have made him feel.” (BSc Physiotherapy student, Female, 18–21 years)
“The feedback at the end was very good and can help me on placement.” (MSc Physiotherapy student, Male, 22–34 years)
3.4.3. Safe Space to Build Confidence
“Experience without a real person avoids real-life initial interaction being ‘messy’—gives us experience that allows us to have ideas of what to ask in our head before real-life interactions.” (MSc Physiotherapy student, Male, 22–34 years)
“Paul is interactive with my answers and his story seems authentic with the details.” (BSc Physiotherapy student, Female, 18–21 years)
“That ‘Paul’ had more realistic emotional responses to questions. This helped to see and understand how the way questions are asked could impact the assessment rapport with the patient.” (MSc Physiotherapy student, Female, 22–34 years)
3.5. Professional Development
3.5.1. Development of Soft Skills
“Listening to his concerns is the most important thing as [it] allows for a better rapport to be built up.” (BSc Physiotherapy student, Male, 18–21 years)
“It is important to ask about the patient, their understanding, lifestyle, how they cope, and what they want from the assessment rather than jumping straight to a diagnosis.” (BSc Physiotherapy student, Female, 18–21 years)
3.5.2. Self-Reflection & Recognition of Own Biases
“‘Paul’ had realistic emotional responses to questions. This helped to see and understand how the way questions are asked could impact the assessment rapport with the patient.” (MSc Physiotherapy student, Male, 22–34 years)
“The importance of letting patients have time to speak about their experience.” (MSc Physiotherapy student, Female, 22–34 years)
“How much of a tendency I have towards a biological model of pain/treatment/assessment.” (BSc Physiotherapy student, Male, 22–34 years)
3.6. Limitations of the Simulation
3.6.1. Not Challenging Enough
“Sometimes it was too obvious which was the ‘correct’ question.” (BSc Physiotherapy student, Female, 22–34 years)
“Some of the questions felt very similar, like both could have been correct, (e.g., we have talked about rating pain 1–10), but the other answer also seemed more acceptable.” (BSc Physiotherapy student, Female, 18–21 years)
“Some pairs of questions seemed to not link well, therefore difficult to choose which route to go down.” (MSc Physiotherapy student, Male, 22–34 years)
“There is only 2 questions to pick from, maybe more variety would give you more examples of how to understand what a psychosocial question is.” (MSc Physiotherapy student, Female, 22–34 years)
“The questions could have led down different ‘paths’ instead of following questions not changing depending on the last question/answer.” (BSc Physiotherapy student, Male, 22–34 years)
3.6.2. Technical Challenges
“The webpage kept freezing so I had to refresh it and start again, but not sure if this was due to my laptop or the way the activity was set up.” (BSc Physiotherapy student, Female, 18–21 years)
“Maybe try to fix technical issues with the glitching.” (BSc Physiotherapy student, Male, 18–21 years)
“Opportunity to go back if accidentally clicked answer you deem incorrect.” (BSc Physiotherapy student, Female, 18–21 years)
4. Discussion
4.1. Future Scope
4.2. Strengths and Limitations of the Project
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fayaz, A.; Croft, P.; Langford, R.M.; Donaldson, L.J.; Jones, G.T. Prevalence of chronic pain in the UK: A systematic review and meta-analysis of population studies. BMJ Open 2016, 6, e010364. [Google Scholar] [CrossRef] [PubMed]
- Dahlhamer, J.; Lucas, J.; Zelaya, C.; Nahin, R.; Mackey, S.; DeBar, L.; Kerns, R.; Von Korff, M.; Porter, L.; Helmick, C. Prevalence of chronic pain and high-impact chronic pain among adults—United States, 2016. Morb. Mortal. Wkly. Rep. 2018, 67, 1001. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.P.; Vase, L.; Hooten, W.M. Chronic pain: An update on burden, best practices, and new advances. Lancet 2021, 397, 2082–2097. [Google Scholar] [CrossRef] [PubMed]
- Thompson, K.; Johnson, M.I.; Milligan, J.; Briggs, M. Twenty-five years of pain education research-what have we learned? Findings from a comprehensive scoping review of research into pre-registration pain education for health professionals. PAIN 2018, 159, 2146–2158. [Google Scholar] [CrossRef]
- Mankelow, J.; Ryan, C.G.; Taylor, P.C.; Casey, M.-B.; Naisby, J.; Thompson, K.; McVeigh, J.G.; Seenan, C.; Cooper, K.; Hendrick, P.; et al. International, multi-disciplinary, cross-section study of pain knowledge and attitudes in nursing, midwifery and allied health professions students. BMC Med. Educ. 2022, 22, 547. [Google Scholar] [CrossRef]
- Nicholas, M.; Vlaeyen, J.W.S.; Rief, W.; Barke, A.; Aziz, Q.; Benoliel, R.; Cohen, M.; Evers, S.; Giamberardino, M.A.; Goebel, A.; et al. The IASP classification of chronic pain for ICD-11: Chronic primary pain. PAIN 2019, 160, 28–37. [Google Scholar] [CrossRef]
- Raja, S.N.; Carr, D.B.; Cohen, M.; Finnerup, N.B.; Flor, H.; Gibson, S.; Keefe, F.J.; Mogil, J.S.; Ringkamp, M.; Sluka, K.A.; et al. The revised International Association for the Study of Pain definition of pain: Concepts, challenges, and compromises. PAIN 2020, 161, 1976–1982. [Google Scholar] [CrossRef]
- Fishman, S.M.; Young, H.M.; Lucas Arwood, E.; Chou, R.; Herr, K.; Murinson, B.B.; Watt-Watson, J.; Carr, D.B.; Gordon, D.B.; Stevens, B.J.; et al. Core Competencies for Pain Management: Results of an Interprofessional Consensus Summit. Pain Med. 2013, 14, 971–981. [Google Scholar] [CrossRef]
- IASP. IASP Curricula List. Available online: https://www.iasp-pain.org/Education/CurriculaList.aspx?navItemNumber=647 (accessed on 17 March 2025).
- BPS. Pre-registration Pain Education: A Practical Guide to Incorporating Pain Education into Pre-Registration Curricula for Healthcare Professionals in the UK. British Pain Society. 2018. Available online: https://www.britishpainsociety.org/for-members/professional-publications/ (accessed on 17 March 2025).
- Wilkinson, P. The Gap Between Knowledge and Practice. Available online: https://www.iasp-pain.org/resources/fact-sheets/the-gap-between-knowledge-and-practice/ (accessed on 17 March 2025).
- Carr, E.C.; Briggs, E.V.; Briggs, M.; Allcock, N.; Black, P.; Jones, D. Understanding factors that facilitate the inclusion of pain education in undergraduate curricula: Perspectives from a UK survey. Br. J. Pain 2016, 10, 100–107. [Google Scholar] [CrossRef]
- Briggs, E.V.; Battelli, D.; Gordon, D.; Kopf, A.; Ribeiro, S.; Puig, M.M.; Kress, H.G. Current pain education within undergraduate medical studies across Europe: Advancing the Provision of Pain Education and Learning (APPEAL) study. BMJ Open 2015, 5, e006984. [Google Scholar] [CrossRef]
- Kolb, D.A. Experiential Learning: Experience as the Source of Learning and Development; FT Press: Upper Saddle River, NJ, USA, 2014. [Google Scholar]
- Lowe, C.M.; Heneghan, N.; Herbland, A.; Atkinson, K.; Beeton, K. Project Report for the Chartered Society of Physiotherapy; University of Hertfordshire: Hatfield, UK, 2022. [Google Scholar]
- HEE. Health Education England: About. 2023. Available online: https://www.hee.nhs.uk/about-2 (accessed on 1 March 2022).
- CSP. KNOWBEST: The KNOWledge, Behaviours and Skills Required of the Modern PhysioTherapy Graduate Including the Future Role of Practice Based Learning; Chartered Society of Physiotherapy: London, UK, 2022. [Google Scholar]
- Sandoval-Cuellar, C.; Alfonso-Mora, M.L.; Castellanos-Garrido, A.L.; Del Pilar Villarraga-Nieto, A.; Goyeneche-Ortegón, R.L.; Acosta-Otalora, M.L.; Del Pilar Castellanos-Vega, R.; Cobo-Mejía, E.A. Simulation in physiotherapy students for clinical decisions during interaction with people with low back pain: Randomised controlled trial. BMC Med. Educ. 2021, 21, 375. [Google Scholar] [CrossRef]
- Barranco-i-Reixachs, D.; Bravo, C.; Orio, A.; Rubí-Carnacea, F. Physiotherapy education: Simulation-based learning on biopsychosocial training in chronic pain—A mixed-methods study. Fisioterapia 2024, 46, 325–333. [Google Scholar] [CrossRef]
- Forbes, R.; Irving, P.; Copley, J. Development and evaluation of interprofessional patient simulation activity for physiotherapy and occupational therapy students to assess and manage patients with chronic pain. Int. J. Ther. Rehabil. 2020, 27, 1–12. [Google Scholar] [CrossRef]
- Kononowicz, A.A.; Woodham, L.A.; Edelbring, S.; Stathakarou, N.; Davies, D.; Saxena, N.; Tudor Car, L.; Carlstedt-Duke, J.; Car, J.; Zary, N. Virtual Patient Simulations in Health Professions Education: Systematic Review and Meta-Analysis by the Digital Health Education Collaboration. J. Med. Internet Res. 2019, 21, e14676. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Conceptual and design thinking for thematic analysis. Qualitative Psychology 2022, 9, 3–26. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Toward good practice in thematic analysis: Avoiding common problems and be(com)ing a knowing researcher. Int. J. Transgender Health 2023, 24, 1–6. [Google Scholar] [CrossRef]
- Articulate Global, LLC. Articulate Storyline (Version 3.61.27106.0) [Software]. 2022. Articulate. Available online: https://www.articulate.com (accessed on 1 March 2022).
- Unity Technologies. Unity (Version 2020.3.30f1) [Software]. Unity Technologies. 2022. Available online: https://unity.com (accessed on 1 March 2022).
- Autodesk, Inc. AutoDesk Character Generator (Version 2022) [Software]. Autodesk. 2022. Available online: https://charactergenerator.autodesk.com (accessed on 1 March 2022).
- Crazy Minnow Studio. Salsa Lipsync (Version 2.5.4.125) [Software]. Crazy Minnow Studio. 2022. Available online: https://crazyminnowstudio.com/unity-3d/lip-sync-salsa (accessed on 1 March 2022).
- Thomas, D.R. A General Inductive Approach for Analyzing Qualitative Evaluation Data. Am. J. Eval. 2006, 27, 237–246. [Google Scholar]
- Pritchard, S.A.; Blackstock, F.C.; Nestel, D.; Keating, J.L. Simulated patients in physical therapy education: Systematic review and meta-analysis. Phys. Ther. 2016, 96, 1342–1353. [Google Scholar]
- Roberts, F.; Cooper, K. Effectiveness of high fidelity simulation versus low fidelity simulation on practical/clinical skill development in pre-registration physiotherapy students: A systematic review. JBI Evid. Synth. 2019, 17, 1229–1255. [Google Scholar]
- Sawyer, T.; Eppich, W.; Brett-Fleegler, M.; Grant, V.; Cheng, A. More Than One Way to Debrief: A Critical Review of Healthcare Simulation Debriefing Methods. Simul. Healthc. 2016, 11, 209–217. [Google Scholar]
- Favolise, M. Post-Simulation Debriefing Methods: A Systematic Review. Arch. Phys. Med. Rehabil. 2024, 105, e146. [Google Scholar] [CrossRef]
- Johnson, M.I.; Woodall, J. A healthy settings approach to addressing painogenic environments: New perspectives from health promotion. Front. Pain Res. 2022, 3, 1000170. [Google Scholar] [CrossRef]
- Johnson, M.I.; Bonacaro, A.; Georgiadis, E.; Woodall, J. Reconfiguring the biomedical dominance of pain: Time for alternative perspectives from health promotion? Health Promot. Int. 2022, 37, daac128. [Google Scholar] [CrossRef] [PubMed]
- Johnson, M.I.; Page, K.; Woodall, J.; Thompson, K. Perspectives on Community-Based System Change for People Living with Persistent Pain: Insights from Developing the “Rethinking Pain Service”. Front. Pain Res. 2024, 5, 1299027. [Google Scholar] [CrossRef]
- Thompson, K.; Milligan, J.; Briggs, M.; Deane, J.A.; Johnson, M.I. A qualitative study to explore the acceptability and feasibility of implementing person-focused evidence-based pain education concepts in pre-registration physiotherapy training. Front. Pain Res. 2023, 4, 1162387. [Google Scholar] [CrossRef]
- Thompson, K.; Johnson, M.I.; Milligan, J.; Briggs, M. Rethinking pain education from the perspectives of people experiencing pain: A meta-ethnography to inform physiotherapy training. BMJ Open 2022, 12, e046363. [Google Scholar] [CrossRef]
- Crawford, S.B. ASPiH standards for simulation-based education: Process of consultation, design and implementation. BMJ Simul. Technol. Enhanc. Learn. 2018, 4, 103–104. [Google Scholar] [CrossRef]
- INACSL Standards of Best Practice: SimulationSM Simulation Design. Clin. Simul. Nurs. 2016, 12, S5–S12. [CrossRef]
- Thompson, K.G.; Kate, S.; David, J.; Mark, I. Development and Evaluation of an innovative and practical simulation tool to develop person-centred pain assessment skills in physiotherapy students. In Proceedings of the Second Durham Conference on Using VR and AR in Education Durham, Virtual Meeting, 17 July 2024. [Google Scholar]
| Demographic Category | Subcategory | Number of Respondents (n = 46) | Percentage (%) |
|---|---|---|---|
| Degree Program | BSc | 29 | 59.2% |
| MSc | 17 | 34.7% | |
| Missing Data | 0 | 0.0% | |
| Age Bracket | 18–21 years | 23 | 50.0% |
| 22–34 years | 21 | 45.7% | |
| 35–44 years | 2 | 4.3% | |
| Missing Data | 3 | 6.1% | |
| Ethnicity | Asian | 1 | 2.0% |
| Black or African American | 2 | 4.1% | |
| White British | 38 | 77.6% | |
| White Other | 2 | 4.1% | |
| Other | 1 | 2.0% | |
| Prefer not to say | 2 | 4.1% | |
| Missing Data | 3 | 6.1% | |
| Gender | Female | 32 | 65.3% |
| Male | 14 | 28.6% | |
| Missing Data | 3 | 6.1% |
| Question | Response (n = 49) | Frequency | Percentage |
|---|---|---|---|
| I enjoyed interacting with Paul | Strongly agree | 22 | 44.9 |
| Somewhat agree | 22 | 44.9 | |
| Neither agree nor disagree | 3 | 6.1 | |
| Somewhat disagree | 0 | 0 | |
| Strongly disagree | 1 | 2 | |
| Missing data | 1 | 2 | |
| I found selecting person-centred questions challenging | Strongly agree | 3 | 6.1 |
| Somewhat agree | 18 | 36.7 | |
| Neither agree nor disagree | 7 | 14.3 | |
| Somewhat disagree | 17 | 34.7 | |
| Strongly disagree | 2 | 4.1 | |
| Missing data | 2 | 4.1 | |
| Interacting with ‘Paul’ improved my understanding of complex subjective pain assessment | Strongly agree | 16 | 32.7 |
| Somewhat agree | 24 | 49 | |
| Neither agree nor disagree | 6 | 12.2 | |
| Somewhat disagree | 1 | 2 | |
| Strongly disagree | 0 | 0 | |
| Missing data | 2 | 4.1 | |
| Interacting with ‘Paul’ increased my confidence in dealing with complex subjective pain assessment | Strongly agree | 5 | 10.2 |
| Somewhat agree | 37 | 75.5 | |
| Neither agree nor disagree | 3 | 6.1 | |
| Somewhat disagree | 2 | 4.1 | |
| Strongly disagree | 1 | 2 | |
| Missing data | 1 | 2 | |
| Interacting with ‘Paul’ helped my understanding of the impact of biopsychosocial v biomedical pain assessment | Strongly agree | 18 | 36.7 |
| Somewhat agree | 21 | 42.9 | |
| Neither agree nor disagree | 7 | 14.3 | |
| Somewhat disagree | 1 | 2 | |
| Strongly disagree | 1 | 2 | |
| Missing data | 1 | 2 | |
| The on-screen instructions were clear | Strongly agree | 38 | 77.6 |
| Somewhat agree | 9 | 18.4 | |
| Neither agree nor disagree | 0 | 0 | |
| Somewhat disagree | 0 | 0 | |
| Strongly disagree | 1 | 2 | |
| Missing data | 1 | 2 | |
| I could see how the activity would be relevant to my learning about pain | Strongly agree | 28 | 57.1 |
| Somewhat agree | 18 | 36.7 | |
| Neither agree nor disagree | 2 | 4.1 | |
| Somewhat disagree | 0 | 0 | |
| Strongly disagree | 0 | 0 | |
| Missing data | 1 | 2 | |
| Paul was a believable character | Strongly agree | 29 | 59.2 |
| Somewhat agree | 17 | 34.7 | |
| Neither agree nor disagree | 1 | 2 | |
| Somewhat disagree | 1 | 2 | |
| Strongly disagree | 0 | 0 | |
| Missing data | 1 | 2 | |
| The scenario seemed authentic | Strongly agree | 29 | 59.2 |
| Somewhat agree | 17 | 34.7 | |
| Neither agree nor disagree | 1 | 2 | |
| Somewhat disagree | 1 | 2 | |
| Strongly disagree | 0 | 0 | |
| Missing data | 1 | 2 | |
| Practicing online with Paul gave me a safe space to test my skills | Strongly agree | 37 | 75.5 |
| Somewhat agree | 9 | 18.4 | |
| Neither agree nor disagree | 1 | 2 | |
| Somewhat disagree | 0 | 0 | |
| Strongly disagree | 0 | 0 | |
| Missing data | 2 | 4.1 | |
| Practicing online with Paul will help me prepare for clinical placement | Strongly agree | 16 | 32.7 |
| Somewhat agree | 27 | 55.1 | |
| Neither agree nor disagree | 3 | 6.1 | |
| Somewhat disagree | 2 | 4.1 | |
| Strongly disagree | 0 | 0 | |
| Missing data | 1 | 2 | |
| I would like to repeat the activity with Paul several times | Strongly agree | 11 | 22.4 |
| Somewhat agree | 15 | 30.6 | |
| Neither agree nor disagree | 11 | 22.4 | |
| Somewhat disagree | 6 | 12.2 | |
| Strongly disagree | 3 | 6.1 | |
| Missing data | 3 | 6.1 | |
| The online feedback helped me understand what areas I needed to improve on | Strongly agree | 17 | 34.7 |
| Somewhat agree | 12 | 24.5 | |
| Neither agree nor disagree | 3 | 6.1 | |
| Somewhat disagree | 2 | 4.1 | |
| Strongly disagree | 1 | 2 | |
| Missing data | 14 | 28.6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thompson, K.; Bathe, S.; Grafton, K.; Jones, N.; Spark, D.; Trewern, L.; van Hille, T.; Johnson, M.I. Development, Implementation, and Evaluation of a ‘Virtual Patient’ with Chronic Low Back Pain: An Education Resource for Physiotherapy Students. Healthcare 2025, 13, 750. https://doi.org/10.3390/healthcare13070750
Thompson K, Bathe S, Grafton K, Jones N, Spark D, Trewern L, van Hille T, Johnson MI. Development, Implementation, and Evaluation of a ‘Virtual Patient’ with Chronic Low Back Pain: An Education Resource for Physiotherapy Students. Healthcare. 2025; 13(7):750. https://doi.org/10.3390/healthcare13070750
Chicago/Turabian StyleThompson, Kate, Steven Bathe, Kate Grafton, Niki Jones, David Spark, Louise Trewern, Thomas van Hille, and Mark I. Johnson. 2025. "Development, Implementation, and Evaluation of a ‘Virtual Patient’ with Chronic Low Back Pain: An Education Resource for Physiotherapy Students" Healthcare 13, no. 7: 750. https://doi.org/10.3390/healthcare13070750
APA StyleThompson, K., Bathe, S., Grafton, K., Jones, N., Spark, D., Trewern, L., van Hille, T., & Johnson, M. I. (2025). Development, Implementation, and Evaluation of a ‘Virtual Patient’ with Chronic Low Back Pain: An Education Resource for Physiotherapy Students. Healthcare, 13(7), 750. https://doi.org/10.3390/healthcare13070750







