Risk Factors for Poor Sleep Quality and Subjective Cognitive Decline in Older Adults Living in the United States During the COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
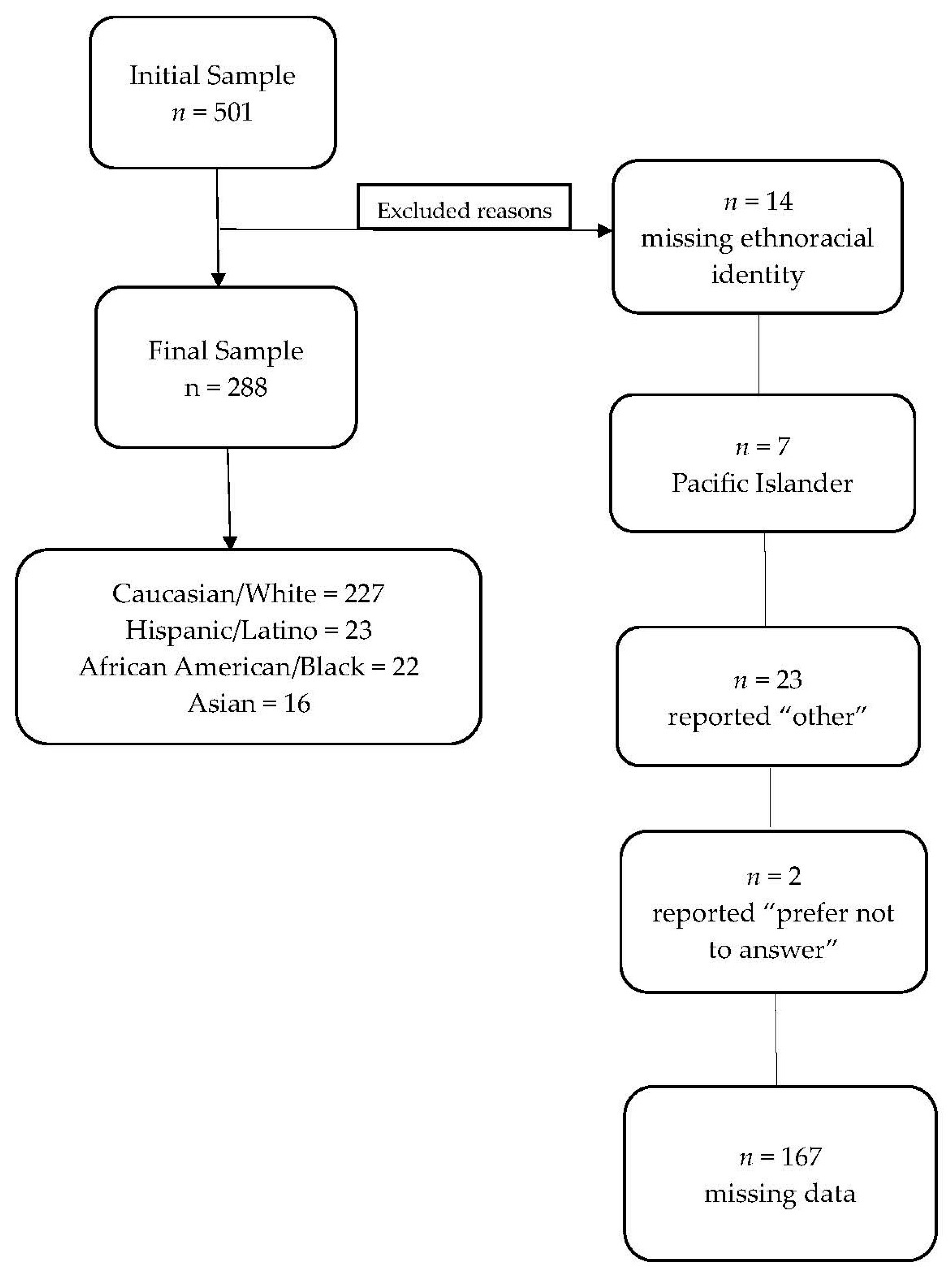
2.1. Participants
2.2. Measures
2.3. Analyses
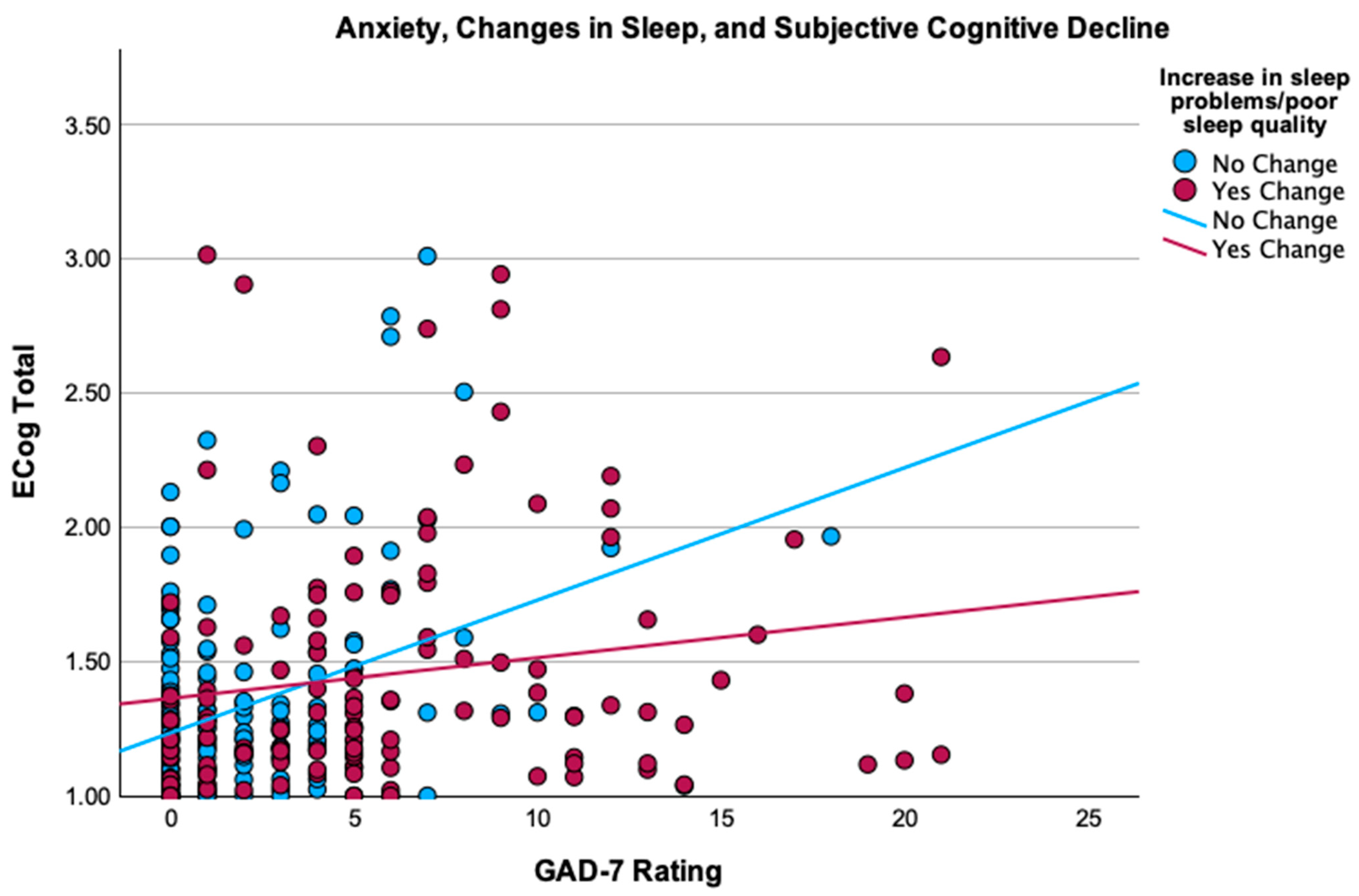
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gupta, R.; Grover, S.; Basu, A.; Krishnan, V.; Tripathi, A.; Subramanyam, A.; Nischal, A.; Hussain, A.; Mehra, A.; Ambekar, A.; et al. Changes in Sleep Pattern and Sleep Quality during COVID-19 Lockdown. Indian J. Psychiatry 2020, 62, 370–378. [Google Scholar] [CrossRef] [PubMed]
- Kocevska, D.; Blanken, T.F.; Van Someren, E.J.W.; Rösler, L. Sleep Quality during the COVID-19 Pandemic: Not One Size Fits All. Sleep Med. 2020, 76, 86–88. [Google Scholar] [CrossRef] [PubMed]
- Tull, M.T.; Edmonds, K.A.; Scamaldo, K.M.; Richmond, J.R.; Rose, J.P.; Gratz, K.L. Psychological Outcomes Associated with Stay-at-Home Orders and the Perceived Impact of COVID-19 on Daily Life. Psychiatry Res. 2020, 289, 113098. [Google Scholar] [CrossRef]
- Pace-Schott, E.F.; Spencer, R.M.C. Age-Related Changes in the Cognitive Function of Sleep. Prog. Brain Res. 2011, 191, 75–89. [Google Scholar] [CrossRef] [PubMed]
- Cipriani, G.E.; Bartoli, M.; Amanzio, M. Are Sleep Problems Related to Psychological Distress in Healthy Aging during the COVID-19 Pandemic? A Review. Int. J. Environ. Res. Public Health 2021, 18, 10676. [Google Scholar] [CrossRef]
- Bubu, O.M.; Brannick, M.; Mortimer, J.; Umasabor-Bubu, O.; Sebastião, Y.V.; Wen, Y.; Schwartz, S.; Borenstein, A.R.; Wu, Y.; Morgan, D.; et al. Sleep, Cognitive Impairment, and Alzheimer’s Disease: A Systematic Review and Meta-Analysis. Sleep 2017, 40, zsw032. [Google Scholar] [CrossRef]
- Kim, J.H.; Ahn, J.H.; Min, C.Y.; Yoo, D.M.; Choi, H.G. Association between Sleep Quality and Subjective Cognitive Decline: Evidence from a Community Health Survey. Sleep Med. 2021, 83, 123–131. [Google Scholar] [CrossRef]
- Tsapanou, A.; Vlachos, G.S.; Cosentino, S.; Gu, Y.; Manly, J.J.; Brickman, A.M.; Schupf, N.; Zimmerman, M.E.; Yannakoulia, M.; Kosmidis, M.H.; et al. Sleep and Subjective Cognitive Decline in Cognitively Healthy Elderly: Results from Two Cohorts. J. Sleep Res. 2019, 28, e12759. [Google Scholar] [CrossRef]
- Jessen, F.; Amariglio, R.E.; Buckley, R.F.; van der Flier, W.M.; Han, Y.; Molinuevo, J.L.; Rabin, L.; Rentz, D.M.; Rodriguez-Gomez, O.; Saykin, A.J.; et al. The Characterisation of Subjective Cognitive Decline. Lancet Neurol. 2020, 19, 271–278. [Google Scholar] [CrossRef]
- Sutton, E.; Catling, J.; Segaert, K.; Veldhuijzen Van Zanten, J. Cognitive Health Worries, Reduced Physical Activity and Fewer Social Interactions Negatively Impact Psychological Wellbeing in Older Adults during the COVID-19 Pandemic. Front. Psychol. 2022, 13, 823089. [Google Scholar] [CrossRef]
- De Pue, S.; Gillebert, C.; Dierckx, E.; Vanderhasselt, M.-A.; De Raedt, R.; Van Den Bussche, E. The Impact of the COVID-19 Pandemic on Wellbeing and Cognitive Functioning of Older Adults. Sci. Rep. 2021, 11, 4636. [Google Scholar] [CrossRef]
- Liew, T.M. Depression, Subjective Cognitive Decline, and the Risk of Neurocognitive Disorders. Alzheimer’s Res. Ther. 2019, 11, 70. [Google Scholar] [CrossRef] [PubMed]
- Liew, T.M. Subjective Cognitive Decline, Anxiety Symptoms, and the Risk of Mild Cognitive Impairment and Dementia. Alzheimer’s Res. Ther. 2020, 12, 107. [Google Scholar] [CrossRef]
- Fiorenzato, E.; Zabberoni, S.; Costa, A.; Cona, G. Cognitive and Mental Health Changes and Their Vulnerability Factors Related to COVID-19 Lockdown in Italy. PLoS ONE 2021, 16, e0246204. [Google Scholar] [CrossRef]
- Robbins, R.; Weaver, M.D.; Czeisler, M.É.; Barger, L.K.; Quan, S.F.; Czeisler, C.A. Associations between Changes in Daily Behaviors and Self-Reported Feelings of Depression and Anxiety about the COVID-19 Pandemic among Older Adults. J. Gerontol. Ser. B 2022, 77, e150–e159. [Google Scholar] [CrossRef]
- Friedman, E.M.; Love, G.D.; Rosenkranz, M.A.; Urry, H.L.; Davidson, R.J.; Singer, B.H.; Ryff, C.D. Socioeconomic Status Predicts Objective and Subjective Sleep Quality in Aging Women. Psychosom. Med. 2007, 69, 682–691. [Google Scholar] [CrossRef]
- Grandner, M.A.; Patel, N.P.; Gehrman, P.R.; Xie, D.; Sha, D.; Weaver, T.; Gooneratne, N. Who Gets the Best Sleep? Ethnic and Socioeconomic Factors Related to Sleep Complaints. Sleep Med. 2010, 11, 470–478. [Google Scholar] [CrossRef]
- Collinge, A.N.; Bath, P.A. Socioeconomic Background and Self-Reported Sleep Quality in Older Adults during the COVID-19 Pandemic: An Analysis of the English Longitudinal Study of Ageing (ELSA). Int. J. Environ. Res. Public Health 2023, 20, 4534. [Google Scholar] [CrossRef]
- Li, Y.; Mutchler, J.E. Older Adults and the Economic Impact of the COVID-19 Pandemic. J. Aging Soc. Policy 2020, 32, 477–487. [Google Scholar] [CrossRef] [PubMed]
- Babulal, G.M.; Torres, V.L.; Acosta, D.; Agüero, C.; Aguilar-Navarro, S.; Amariglio, R.; Ussui, J.A.; Baena, A.; Bocanegra, Y.; Brucki, S.M.D.; et al. The Impact of COVID-19 on the Well-Being and Cognition of Older Adults Living in the United States and Latin America. eClinicalMedicine 2021, 35, 100848. [Google Scholar] [CrossRef] [PubMed]
- Grasso, D.J.; Briggs-Gowan, M.J.; Ford, J.D.; Carter, A.S. The Epidemic—Pandemic Impacts Inventory (EPII); University of Connecticut School of Medicine: Farmington, CT, USA, 2020. [Google Scholar]
- Andresen, E.M.; Malmgren, J.A.; Carter, W.B.; Patrick, D.L. Screening for Depression in Well Older Adults: Evaluation of a Short Form of the CES-D. Am. J. Prev. Med. 1994, 10, 77–84. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092. [Google Scholar] [CrossRef] [PubMed]
- Wild, B.; Eckl, A.; Herzog, W.; Niehoff, D.; Lechner, S.; Maatouk, I.; Schellberg, D.; Brenner, H.; Müller, H.; Löwe, B. Assessing Generalized Anxiety Disorder in Elderly People Using the GAD-7 and GAD-2 Scales: Results of a Validation Study. Am. J. Geriatr. Psychiatry 2014, 22, 1029–1038. [Google Scholar] [CrossRef]
- Farias, S.T.; Mungas, D.; Reed, B.R.; Cahn-Weiner, D.; Jagust, W.; Baynes, K.; DeCarli, C. The Measurement of Everyday Cognition (ECog): Scale Development and Psychometric Properties. Neuropsychology 2008, 22, 531–544. [Google Scholar] [CrossRef]
- Kline, R.B. Principles and Practice of Structural Equation Modeling, 4th ed.; Guilford Publications: New York, NY, USA, 2016. [Google Scholar]
- Farias, S.T.; Lau, K.; Harvey, D.; Denny, K.G.; Barba, C.; Mefford, A.N. Early Functional Limitations in Cognitively Normal Older Adults Predict Diagnostic Conversion to Mild Cognitive Impairment. J. Am. Geriatr. Soc. 2017, 65, 1152–1158. [Google Scholar] [CrossRef]
- Van Patten, R.; Nguyen, T.T.; Mahmood, Z.; Lee, E.E.; Daly, R.E.; Palmer, B.W.; Wu, T.-C.; Tu, X.; Jeste, D.V.; Twamley, E.W. Physical and Mental Health Characteristics of Adults with Subjective Cognitive Decline: A Study of 3,407 People Aged 18–81 Years from an MTurk-Based U.S. National Sample. bioRxviv 2020. [Google Scholar] [CrossRef]
- Wu, Y.; Mao, Z.; Cui, F.; Fan, J.; Yuan, Z.; Tang, L. Neurocognitive Characteristics of Subjective Cognitive Decline and its Association with Objective Cognition, Negative Emotion, and Sleep Quality in Chinese Elderly. Neuropsychiatr. Dis. Treat. 2023, 19, 2261–2270. [Google Scholar] [CrossRef]
- De Pue, S.; Gillebert, C.; Dierckx, E.; Van den Bussche, E. The Longer-Term Impact of the COVID-19 Pandemic on Wellbeing and Subjective Cognitive Functioning of Older Adults in Belgium. Sci. Rep. 2023, 13, 9708. [Google Scholar] [CrossRef]
- Bentham, C.; Eaves, L. The Impact of Cognitive-Behavioral Interventions on Sleep Disturbance in Depressed and Anxious Community-Dwelling Older Adults: A Systematic Review. Behav. Sleep Med. 2022, 20, 477–499. [Google Scholar] [CrossRef]
| Total Sample (n = 288) Mean (SD) | White (n = 227) Mean (SD) | Latino (n = 23) Mean (SD) | Black (n = 22) Mean (SD) | Asian (n = 16) Mean (SD) | p | |
|---|---|---|---|---|---|---|
| Age (years) | 67.41 (7.43) | 67.97 (7.19) | 63.00 (6.38) | 66.23 (7.93) | 65.76 (7.67) | 0.02 |
| Education (years) | 17.68 (2.31) | 17.63 (2.36) | 17.91 (1.95) | 17.14 (2.34) | 18.75 (1.77) | 0.17 |
| Sex (male:female) | 73:215 | 62:165 | 3:20 | 3:19 | 5:11 | 0.24 |
| Marital status (married:unmarried) | 95:193 | 79:148 | 6:17 | 8:14 | 2:14 | 0.26 |
| Income (low/middle/high) | 32/200/56 | 23/157/47 | 3/16/4 | 5/15/2 | 1/12/3 | 0.57 |
| Occupational status (employed:not employed) | 87:201 | 66:161 | 14:9 | 4:18 | 3:13 | 0.005 |
| Sleep changes (yes:no) | 120:168 | 86:138 | 15:8 | 10:12 | 6:10 | 0.11 |
| CES-D-10 | 7.94 (6.09) | 8.12 (6.13) | 7.39 (5.19) | 7.45 (5.83) | 6.88 (7.23) | 0.80 |
| GAD-7 | 3.61 (4.42) | 3.74 (4.50) | 3.57 (3.59) | 2.77 (3.99) | 3.00 (5.13) | 0.73 |
| ECog | 1.38 (0.42) | 1.39 (0.44) | 1.35 (0.33) | 1.34 (0.28) | 1.29 (0.29) | 0.87 |
| B | SEB | Wald | p-Value | OR | 95% CI | |
|---|---|---|---|---|---|---|
| Age (years) | −0.001 | 0.02 | 0.004 | 0.95 | 1.00 | 0.96–1.04 |
| Sex | 0.39 | 0.35 | 1.23 | 0.27 | 1.47 | 0.74–2.91 |
| Education (years) | 0.08 | 0.06 | 1.5 | 0.22 | 1.08 | 0.936–1.22 |
| CES-D-10 | 0.14 | 0.04 | 14.09 | <0.001 | 1.15 | 1.07–1.24 |
| GAD-7 | 0.14 | 0.06 | 6.74 | 0.009 | 1.15 | 1.04–1.29 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pluim McDowell, C.; Martinez, J.E.; Giudicessi, A.; Munera, D.; Vila-Castelar, C.; Guzmán-Vélez, E.; Ramirez-Gomez, L.; Duffy, J.F.; Cronin-Golomb, A.; Quiroz, Y.T. Risk Factors for Poor Sleep Quality and Subjective Cognitive Decline in Older Adults Living in the United States During the COVID-19 Pandemic. Healthcare 2025, 13, 675. https://doi.org/10.3390/healthcare13060675
Pluim McDowell C, Martinez JE, Giudicessi A, Munera D, Vila-Castelar C, Guzmán-Vélez E, Ramirez-Gomez L, Duffy JF, Cronin-Golomb A, Quiroz YT. Risk Factors for Poor Sleep Quality and Subjective Cognitive Decline in Older Adults Living in the United States During the COVID-19 Pandemic. Healthcare. 2025; 13(6):675. https://doi.org/10.3390/healthcare13060675
Chicago/Turabian StylePluim McDowell, Celina, Jairo E. Martinez, Averi Giudicessi, Diana Munera, Clara Vila-Castelar, Edmarie Guzmán-Vélez, Liliana Ramirez-Gomez, Jeanne F. Duffy, Alice Cronin-Golomb, and Yakeel T. Quiroz. 2025. "Risk Factors for Poor Sleep Quality and Subjective Cognitive Decline in Older Adults Living in the United States During the COVID-19 Pandemic" Healthcare 13, no. 6: 675. https://doi.org/10.3390/healthcare13060675
APA StylePluim McDowell, C., Martinez, J. E., Giudicessi, A., Munera, D., Vila-Castelar, C., Guzmán-Vélez, E., Ramirez-Gomez, L., Duffy, J. F., Cronin-Golomb, A., & Quiroz, Y. T. (2025). Risk Factors for Poor Sleep Quality and Subjective Cognitive Decline in Older Adults Living in the United States During the COVID-19 Pandemic. Healthcare, 13(6), 675. https://doi.org/10.3390/healthcare13060675







