Prevalence of Text Neck Between Different Female Students at Taibah University, Saudi Arabia; Cross Section Design
Abstract
1. Introduction
2. Methods
2.1. Sample and Subjects
2.2. Ethical Considerations
2.3. Eligibility Criteria
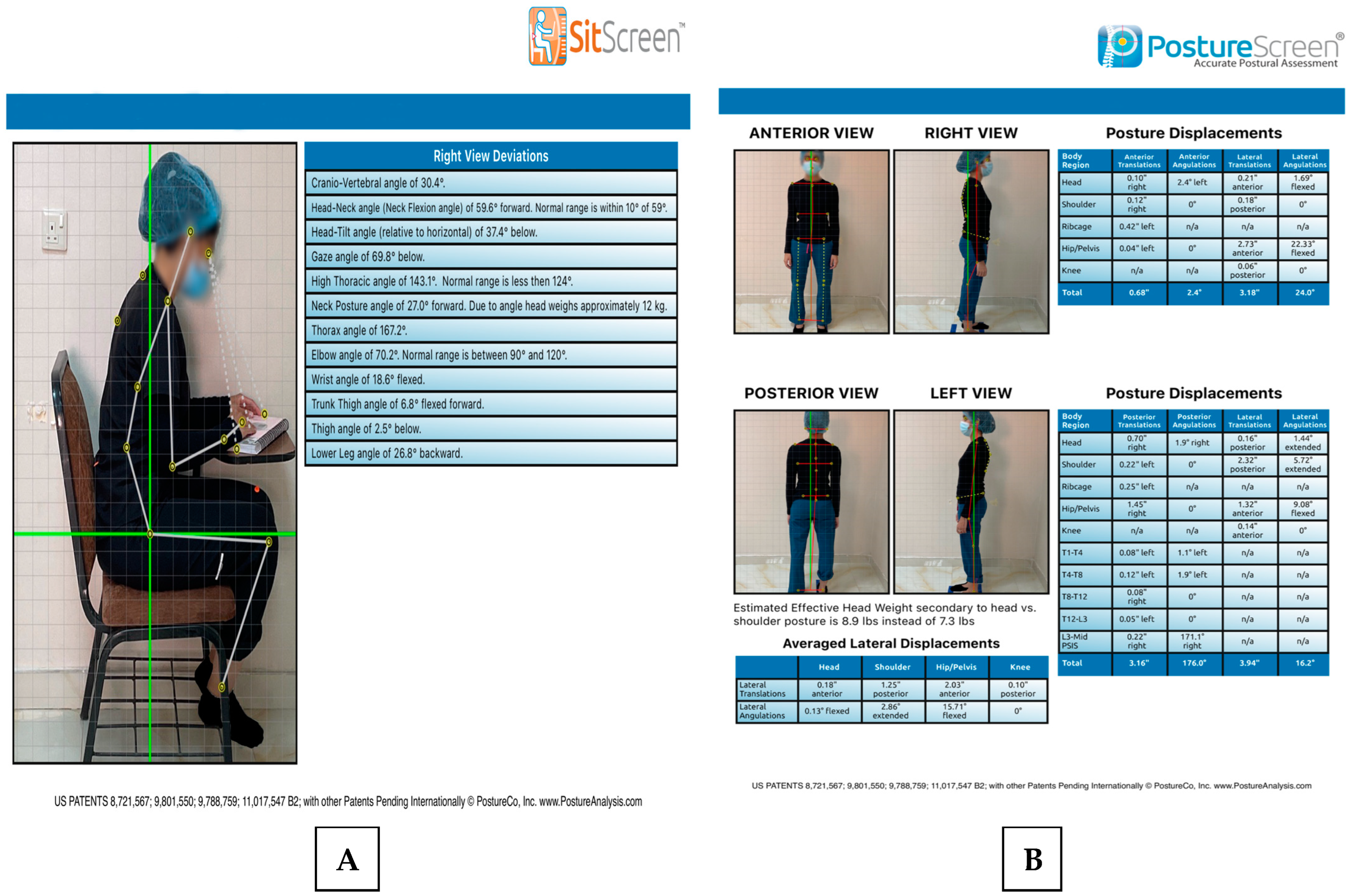
2.4. Assessment Tools
2.5. Procedure
2.6. Statistical Methods
Sample Size
3. Results
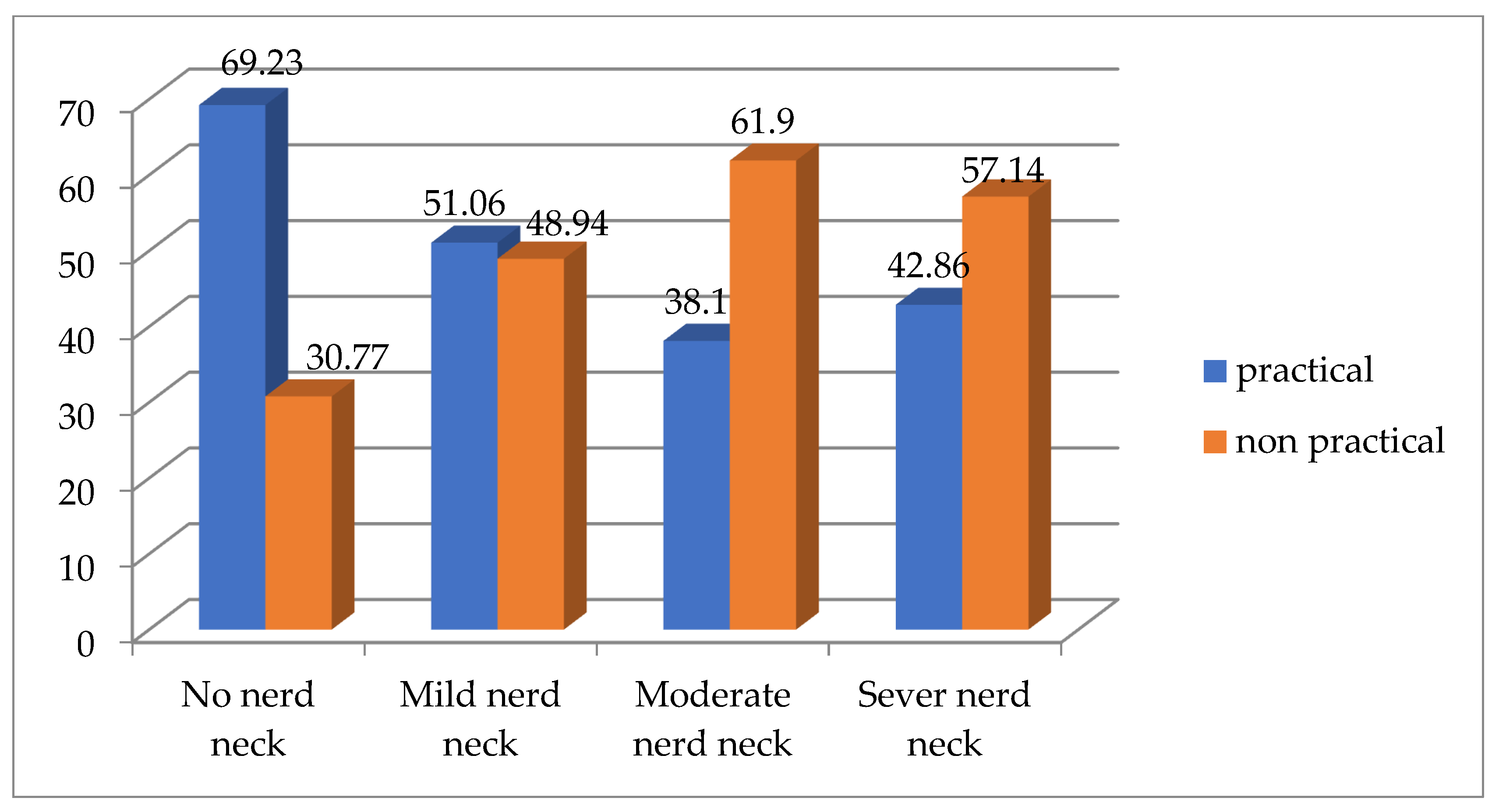
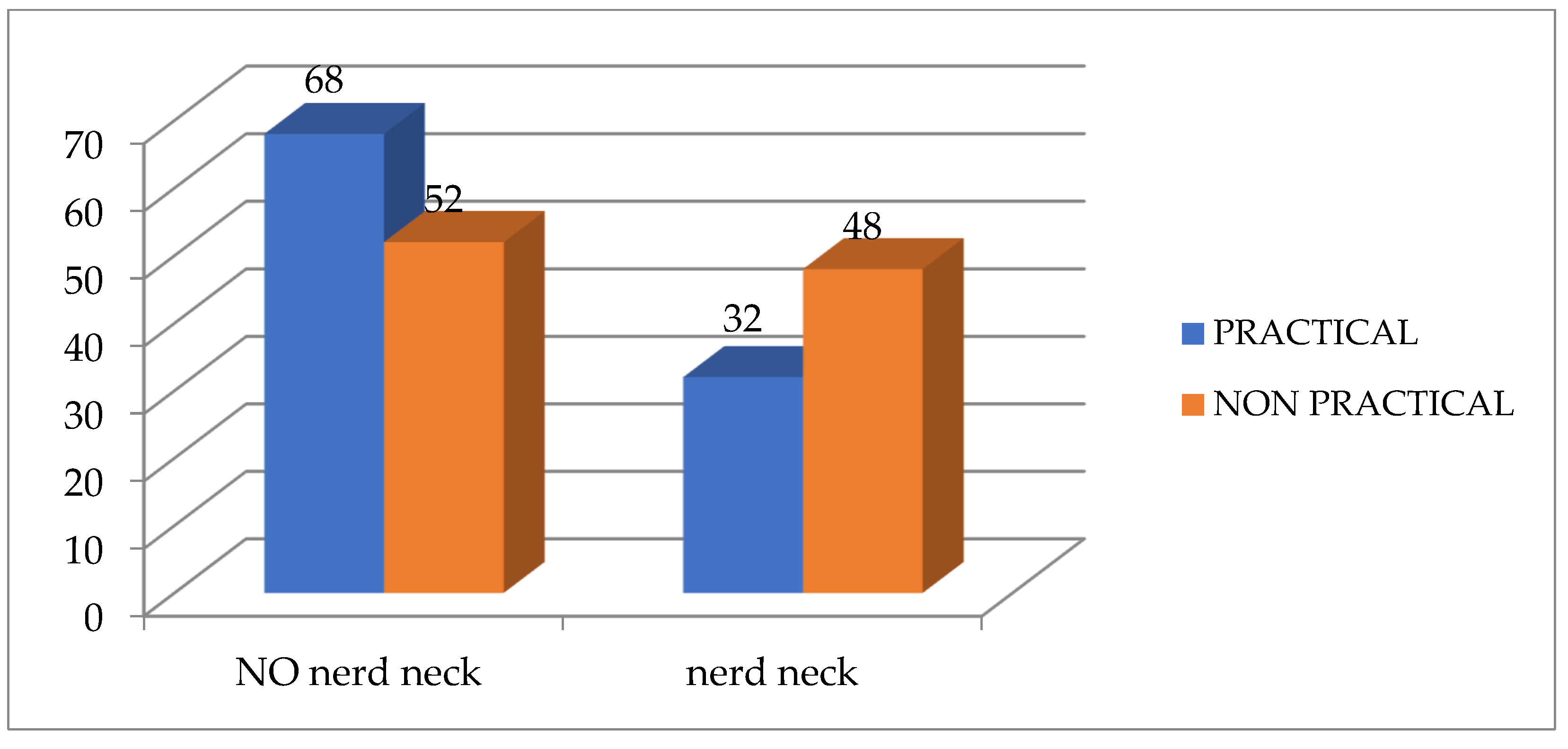
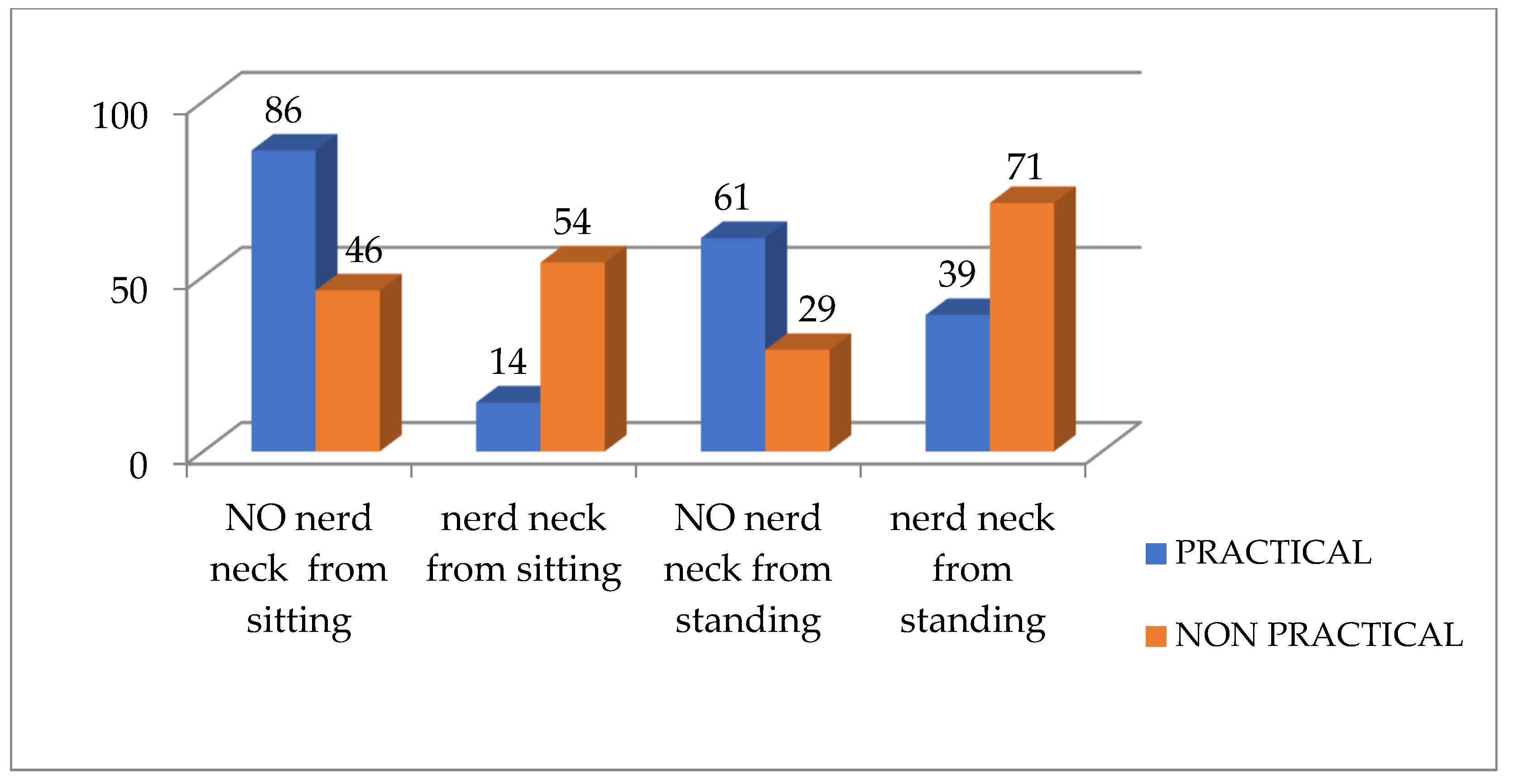
3.1. Prevalence of Text Neck by Observational Analysis
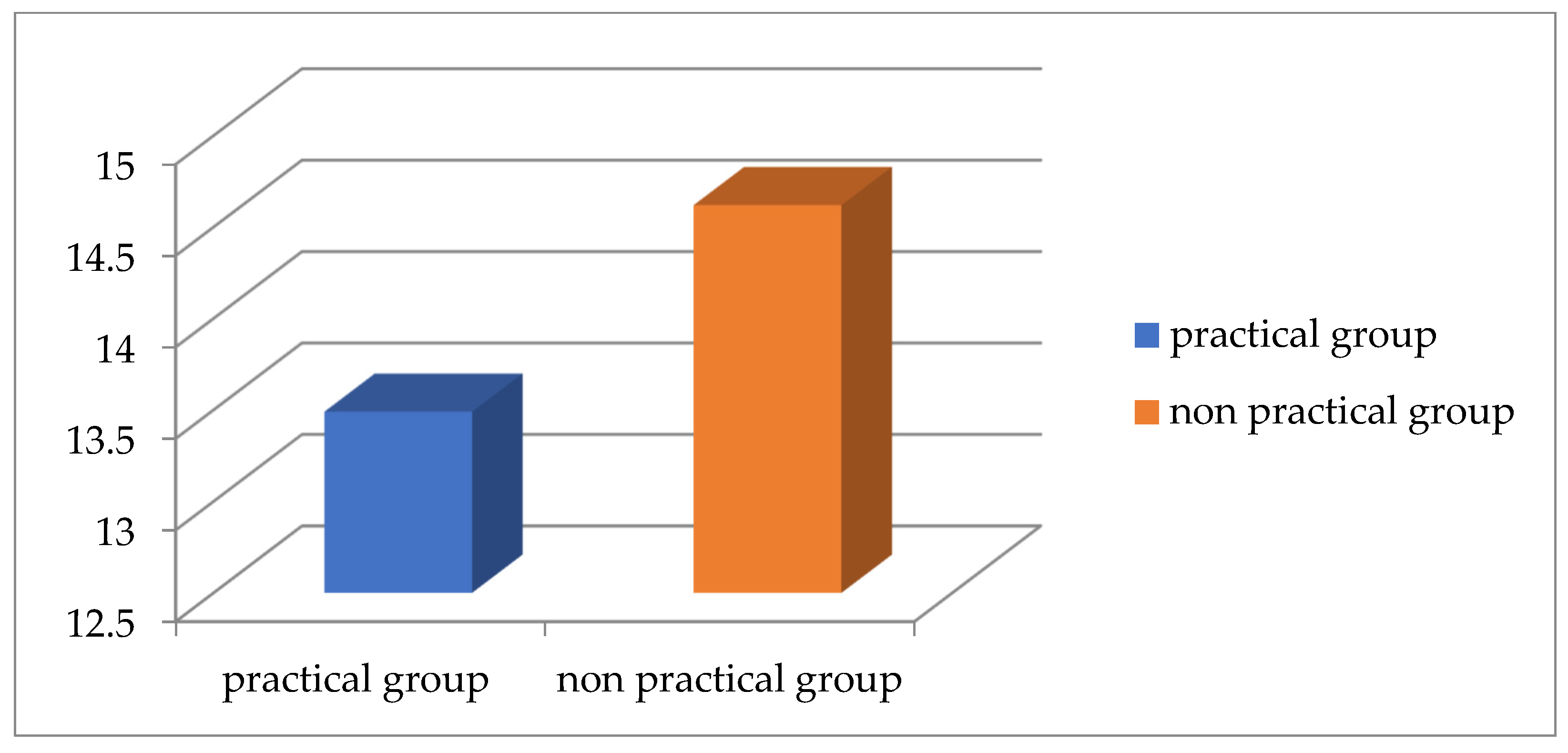
3.2. Statistical Analysis for Quantitative Measurements of Text Neck
4. Discussion
Limitations and Recommendations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mahmoud, N.F.; Hassan, K.A.; Abdelmajeed, S.F.; Moustafa, I.M.; Silva, A.G. The Relationship Between Forward Head Posture and Neck Pain: A Systematic Review and Meta-Analysis. Curr. Rev. Musculoskelet. Med. 2019, 12, 562–577. [Google Scholar] [CrossRef] [PubMed]
- Sheikhhoseini, R.; Shahrbanian, S.; Sayyadi, P.; O’Sullivan, K. Effectiveness of Therapeutic Exercise on Forward Head Posture: A Systematic Review and Meta-analysis. J. Manip. Physiol. Ther. 2018, 41, 530–539. [Google Scholar] [CrossRef] [PubMed]
- Kiruthika, S.; Rekha, K.; Preethy, G.; Abraham, M. Prevalence of Postural Dysfunction among Female College Students—A Qualitative Analysis. Biol. Med. 2018, 10, 1–3. [Google Scholar] [CrossRef]
- Naz, A.; Bashir, M.S.; Noor, R. Prevalence of forward head posture among university students. Rawal Med. J. 2018, 43, 260–262. Available online: https://www.rmj.org.pk/?mno=274422 (accessed on 5 April 2022).
- Ramalingam, V.; Subramaniam, A. Prevalence and Associated Risk Factors of Forward Head Posture among University Students. Indian J. Public Health Res. Dev. 2019, 10, 775–780. [Google Scholar] [CrossRef]
- Singh, S.; Kaushal, K.; Jasrotia, S. Prevalence of forward head posture and its impact on the activity of daily living among students of Adesh University–A cross-sectional study. J. Med. Sci. Res. 2020, 2, 99–102. [Google Scholar] [CrossRef]
- Verma, S.L.; Shaikh, J.; Mahato, R.K.; Sheth, M.S. Prevalence of forward head posture among 12–16-year-old school going students—A cross sectional study. Appl. Med. Res. 2018, 4, 18–21. [Google Scholar] [CrossRef]
- Alsiwed, K.T.; Alsarwani, R.M.; Alshaikh, S.A.; Howaidi, R.A.; Aljahdali, A.J.; Bassi, M.M. The prevalence of text neck syndrome and its association with smartphone use among medical students in Jeddah, Saudi Arabia. J. Musculoskelet. Surg. Res. 2021, 5, 266–272. [Google Scholar] [CrossRef]
- Mylonas, K.; Angelopoulos, P.; Billis, E.; Tsepis, E.; Fousekis, K. The effects of therapeutic exercise in improving forward head posture and functionality in patients with neck pain A literature update. Arch. Hell. Med. 2021, 38, 612–617. [Google Scholar] [CrossRef]
- Choi, W. Effect of 4 Weeks of Cervical Deep Muscle Flexion Exercise on Headache and Sleep Disorder in Patients with Tension Headache and Forward Head Posture. Int. J. Environ. Res. Public Health 2021, 18, 3410. [Google Scholar] [CrossRef]
- Szczygieł, E.; Fudacz, N.; Golec, J.; Golec, E. The impact of the position of the head on the functioning of the human body: A systematic review. Int. J. Occup. Med. Environ. Health 2020, 33, 559–568. [Google Scholar] [CrossRef] [PubMed]
- Boland, D.M.; Neufeld, E.V.; Ruddell, J.; Dolezal, B.A.; Cooper, C.B. Inter- and intra-rater agreement of static posture analysis using a mobile application. J. Phys. Ther. Sci. 2016, 28, 3398–3402. [Google Scholar] [CrossRef] [PubMed]
- Gray, K.; Dalal, R.; Weaver, J.D.; Randolph, S. Quantitative Measurements of Forward Head in College-Aged Students: A Conformation Study of Intra-Rater and Inter-Rater Reliability of a Novel Posture Measuring Device. J. Bodyw. Mov. Ther. 2020, 26, 233–237. [Google Scholar] [CrossRef] [PubMed]
- Gadotti, I.C.; Magee, D.J. Validity of surface measurements to assess craniocervical posture in the sagittal plane: A critical review. Phys. Ther. Rev. 2008, 13, 258–268. [Google Scholar] [CrossRef]
- Salahzadeh, Z.; Maroufi, N.; Ahmadi, A.; Behtash, H.; Razmjoo, A.; Gohari, M.; Parnianpour, M. Assessment of forward head posture in females: Observational and photogrammetry methods. J. Back Musculoskelet. Rehabil. 2014, 27, 131–139. [Google Scholar] [CrossRef]
- Oakley, P.A.; Moustafa, I.M.; Haas, J.W.; Betz, J.W.; Harrison, D.E. Two Methods of Forward Head Posture Assessment: Radiography vs. Posture and Their Clinical Comparison. J. Clin. Med. 2024, 13, 2149. [Google Scholar] [CrossRef]
- Szucs, K.A.; Brown, E.V.D. Rater reliability and construct validity of a mobile application for posture analysis. J. Phys. Ther. Sci. 2018, 30, 31–36. [Google Scholar] [CrossRef]
- Hakami, I.; Sherwani, A.; Hadadi, M.; Alzahrani, R.; Albukhari, A.; Omar, Y.; Alsaedi, K.; Aljadani, F.; Ali, N.; Khan, M.; et al. Assessing the Impact of Smartphone Use on Neck Pain and Related Symptoms Among Residents in Jeddah, Saudi Arabia: A Cross-Sectional Study. Cureus 2024, 16, e64299. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bustam, I.G.; Herdayanti, D. Forward Head Posture (FHP) Condition: Reliability of Cranio Vertebral Angle (CVA) Testing. J. Phys. Educ. Sport Health Recreat. 2024, 13, 519–524. [Google Scholar] [CrossRef]
- Macwan, N.S.; Radadiya, T.A. Methods to Analyse Forward Head Posture-A Narrative Review. Int. J. Biol. Pharm. Allied Sci. 2023, 12, 569–576. [Google Scholar] [CrossRef]
- Kumar, S.N.S.; Omar, B.; Htwe, O.; Joseph, L.H.; Krishnan, J.; Esfehani, A.J.; Min, L.L. Reliability, agreement, and validity of digital weighing scale with MatScan in limb load measurement. J. Rehabil. Res. Dev. 2014, 51, 591–598. [Google Scholar] [CrossRef] [PubMed]
- Shipe, N.K.; Billek-Sawhney, B.; Canter, T.A.; Meals, D.J.; Nestler, J.M.; Stumpff, J.L. The intra- and inter-rater reliability of the tragus wall distance (TWD) measurement in non-pathological participants ages 18–34. Physiother. Theory Pract. 2013, 29, 328–334. [Google Scholar] [CrossRef] [PubMed]
- Tudini, F.T.; Myers, B.J.; Bohannon, R.W. Forward flexed posture: Reliability and determinants of tragus-to-wall measurement. Physiother. Theory Pract. 2022, 38, 579–586. [Google Scholar] [CrossRef]
- Mylonas, K.; Tsekoura, M.; Billis, E.; Aggelopoulos, P.; Tsepis, E.; Fousekis, K. Reliability and Validity of Non-radiographic Methods of Forward Head Posture Measurement: A Systematic Review. Cureus 2022, 5, e27696. [Google Scholar] [CrossRef]
- Damasceno, G.M.; Ferreira, A.d.S.; Nogueira, L.A.C.; Reis, F.J.J.; Lara, R.W.; Meziat-Filho, N. Reliability of two pragmatic tools for assessing text neck. J. Bodyw. Mov. Ther. 2018, 22, 963–967. [Google Scholar] [CrossRef]
- Wadhwa, M.; Panchwan, M.; Arunmozhi, R.; Verma, V.; Singh, S. Reliability and Criterion Validity of Physio Master Application for the Measurement of Cervical Range of Motion in Healthy Individuals. Cureus 2024, 16, e73723. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gallego-Izquierdo, T.; Arroba-Díaz, E.; García-Ascoz, G.; Val-Cano, M.d.A.; Pecos-Martin, D.; Cano-De-La-Cuerda, R. Psychometric Proprieties of a Mobile Application to Measure the Craniovertebral Angle a Validation and Reliability Study. Int. J. Environ. Res. Public Health 2020, 17, 6521. [Google Scholar] [CrossRef]
- fitnesscaliper_w7t40b. Posture Screen Measurement Parameters. Available online: https://www.postureanalysis.com/knowledge-base/posturescreen-measurement-parameters/ (accessed on 5 April 2022).
- Nuttall, F.Q. Body Mass Index: Obesity, BMI, and Health A Critical Review. Nutr. Today 2015, 50, 117–128. [Google Scholar] [CrossRef]
- Lee, C.-H.; Lee, S.; Shin, G. Reliability of forward head posture evaluation while sitting, standing, walking and running. Hum. Mov. Sci. 2017, 55, 81–86. [Google Scholar] [CrossRef]
- Normand, M.C.; Descarreaux, M.; Harrison, D.D.; E Harrison, D.; Perron, D.L.; Ferrantelli, J.R.; Janik, T.J. Three- dimensional evaluation of posture in standing with the PosturePrint: An intra- and inter- examiner reliability study. Chiropr. Osteopat. 2007, 15, 15. [Google Scholar] [CrossRef]
- Shaghayeghfard, B.; Ahmadi, A.; Maroufi, N.; Sarrafzadeh, J. Evaluation of forward head posture in sitting and standing positions. Eur. Spine J. 2016, 25, 3577–3582. [Google Scholar] [CrossRef] [PubMed]
- Becker, L.A. Effect Size Calculators. Available online: https://lbecker.uccs.edu/ (accessed on 21 April 2022).
- Marusteri, M.; Bacarea, V. Comparing groups for statistical differences: How to choose the right statistical test? Biochem. Medica 2010, 20, 15–32. [Google Scholar] [CrossRef]
- Kim, H.S.; Shin, Y.J.; Kim, S.G. Analysis Of The Effect Of The Difference Between Standing And Sitting Postures On Neck Proprioception Using Joint Position Error Test. J. Mech. Med. Biol. 2021, 21, 2140048. [Google Scholar] [CrossRef]
- Wiguna, N.P.; Wahyuni, N.; Indrayani, A.W.; Wibawa, A.; Thanaya, S.A.P. The relationship between Smartphone Addiction and forward head posture in junior high school students in north Denpasar. J. Epidemiol. Kesehat. Komunitas 2019, 4, 84–89. [Google Scholar] [CrossRef]
- Kang, J.-H.; Park, R.-Y.; Lee, S.-J.; Kim, J.-Y.; Yoon, S.-R.; Jung, K.-I. The Effect of The Forward Head Posture on Postural Balance in Long Time Computer Based Worker. Ann. Rehabil. Med. 2012, 36, 98–104. [Google Scholar] [CrossRef] [PubMed]
- Vahedi, Z.; Mazloumi, A.; Sharifnezhad, A.; Kazemi, Z.; Garosi, E. Head forward flexion, lateral bending and viewing distance in smartphone users: A comparison between sitting and standing postures. Work 2020, 67, 837–846. [Google Scholar] [CrossRef]
- Amirdehi, M.A.; Hosseini, S.R.; Sam, S.H.; Irani, S.H.; Mirasi, S. Evaluation of Head Position Using Craniovertebral Angle in Two Sitting and Standing Positions in the Elderly. J. Babol Univ. Med. Sci. 2020, 22, 31–38. [Google Scholar] [CrossRef]
- Amirdehi, M.A.; Hosseini, S.R.; Irani, S.; Mirasi, S.; Sam, S. Influence of Body Positions on Craniovertebral Angle in the Elderly People With Forward Head Posture: A Pilot Study. J. Mod. Rehabil. 2019, 12, 85–88. Available online: https://jmr.tums.ac.ir/index.php/jmr/article/view/160 (accessed on 5 April 2022).
- Cho, C. Survey of Faulty Postures and Associated Factors Among Chinese Adolescents. J. Manip. Physiol. Ther. 2008, 31, 224–229. [Google Scholar] [CrossRef]
- Gh, M.E.; Alilou, A.; Ghafurinia, S.; Fereydounnia, S. Prevalence of faulty posture in children and youth from a rural region in Iran. Biomed. Hum. Kinet. 2012, 4, 121–126. [Google Scholar] [CrossRef]
- Sarraf, F.; Abbasi, S.; Varmazyar, S. Self-Management Exercises Intervention on Text Neck Syndrome Among University Students Using Smartphones. Pain Manag. Nurs. 2023, 24, 595–602. [Google Scholar] [CrossRef] [PubMed]
- Fathollahnejad, K.; Letafatkar, A.; Hadadnezhad, M. The effect of manual therapy and stabilizing exercises on forward head and rounded shoulder postures: A six-week intervention with a one-month follow-up study. BMC Musculoskelet Disord 2019, 20, 86. [Google Scholar] [CrossRef] [PubMed]
- Titcomb, D.A.; Melton, B.F.; Miyashita, T.; Bland, H.W. The Effects of Postural Education or Corrective Exercise on the Craniovertebral Angle in Young Adults with Forward Head Posture: A Randomized Controlled Trial. Int. J. Exerc. Sci. 2023, 16, 954–973. [Google Scholar] [CrossRef] [PubMed]





| Variables | Practical Group | Non-Practical Group | T Test | p-Value | ||
|---|---|---|---|---|---|---|
| Mean Values | SD | Mean Values | SD | |||
| Age (yo) | 21.1 | 1.1 | 20.9 | 1.4 | 1.99 | 0.49 |
| Weight (kg) | 53.88 | 11.9 | 49.66 | 8.9 | 1.99 | 0.07 |
| Height (cm) | 157.85 | 7.1 | 153.98 | 13.7 | 1.99 | 0.11 |
| BMI (kg/h2) | 21.61 | 4.7 | 22.77 | 16.7 | 1.99 | 0.67 |
| Text Neck Percentage | Normal Neck | Mild Text Neck | Moderate Text Neck | Severe Text Neck |
|---|---|---|---|---|
| Standing practical group | 20% | 55% | 18% | 7.00% |
| Standing non-practical group | 9% | 52.00% | 30.00% | 9% |
| Sitting practical group | 30% | 52% | 14% | 4.00% |
| Sitting non-practical group | 4.50% | 45.50% | 29.50% | 20.50% |
| Variables | Practical Group | Non-Practical Group | F Test | p Value | ||
|---|---|---|---|---|---|---|
| Mean Values | SD | Mean Values | SD | |||
| The tragus wall distance | 13.49 | 1.7 | 14.62 | 1.4 | 11.36 | 0.001 * |
| CVA Physiomaster from sitting position | 51.53 | 5.1 | 46.57 | 5.9 | 18.04 | 0.0001 * |
| CVA Physiomaster from standing position | 49.74 | 7.01 | 44.06 | 5.3 | 18.11 | 0.0001 * |
| CVA PostureCo from sitting position | 32.10 | 9.8 | 29.59 | 11.1 | 1.36 | 0.247 |
| CVA PostureCo from standing position | 57.08 | 4.6 | 56.03 | 4.6 | 1.31 | 0.255 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mashabi, A.; Ragab, W.; Alrayes, G.; Amoudi, J.; Tokhta, S.; Bashawri, G.; Alqaznili, R.; Ghaith, J.; Almadani, L.; Aljohani, M.M.A.; et al. Prevalence of Text Neck Between Different Female Students at Taibah University, Saudi Arabia; Cross Section Design. Healthcare 2025, 13, 651. https://doi.org/10.3390/healthcare13060651
Mashabi A, Ragab W, Alrayes G, Amoudi J, Tokhta S, Bashawri G, Alqaznili R, Ghaith J, Almadani L, Aljohani MMA, et al. Prevalence of Text Neck Between Different Female Students at Taibah University, Saudi Arabia; Cross Section Design. Healthcare. 2025; 13(6):651. https://doi.org/10.3390/healthcare13060651
Chicago/Turabian StyleMashabi, Abdulrhman, Walaa Ragab, Ghaida Alrayes, Joud Amoudi, Soundos Tokhta, Ghaida Bashawri, Ruqayyah Alqaznili, Jana Ghaith, Lama Almadani, Marwan M. A. Aljohani, and et al. 2025. "Prevalence of Text Neck Between Different Female Students at Taibah University, Saudi Arabia; Cross Section Design" Healthcare 13, no. 6: 651. https://doi.org/10.3390/healthcare13060651
APA StyleMashabi, A., Ragab, W., Alrayes, G., Amoudi, J., Tokhta, S., Bashawri, G., Alqaznili, R., Ghaith, J., Almadani, L., Aljohani, M. M. A., & Al-Shenqiti, A. (2025). Prevalence of Text Neck Between Different Female Students at Taibah University, Saudi Arabia; Cross Section Design. Healthcare, 13(6), 651. https://doi.org/10.3390/healthcare13060651






