Exploring the Role of Artificial Intelligence (AI)-Driven Training in Laparoscopic Suturing: A Systematic Review of Skills Mastery, Retention, and Clinical Performance in Surgical Education
Abstract
1. Introduction
2. Methodology
2.1. Search Strategy and Databases
2.2. Inclusion and Exclusion Criteria
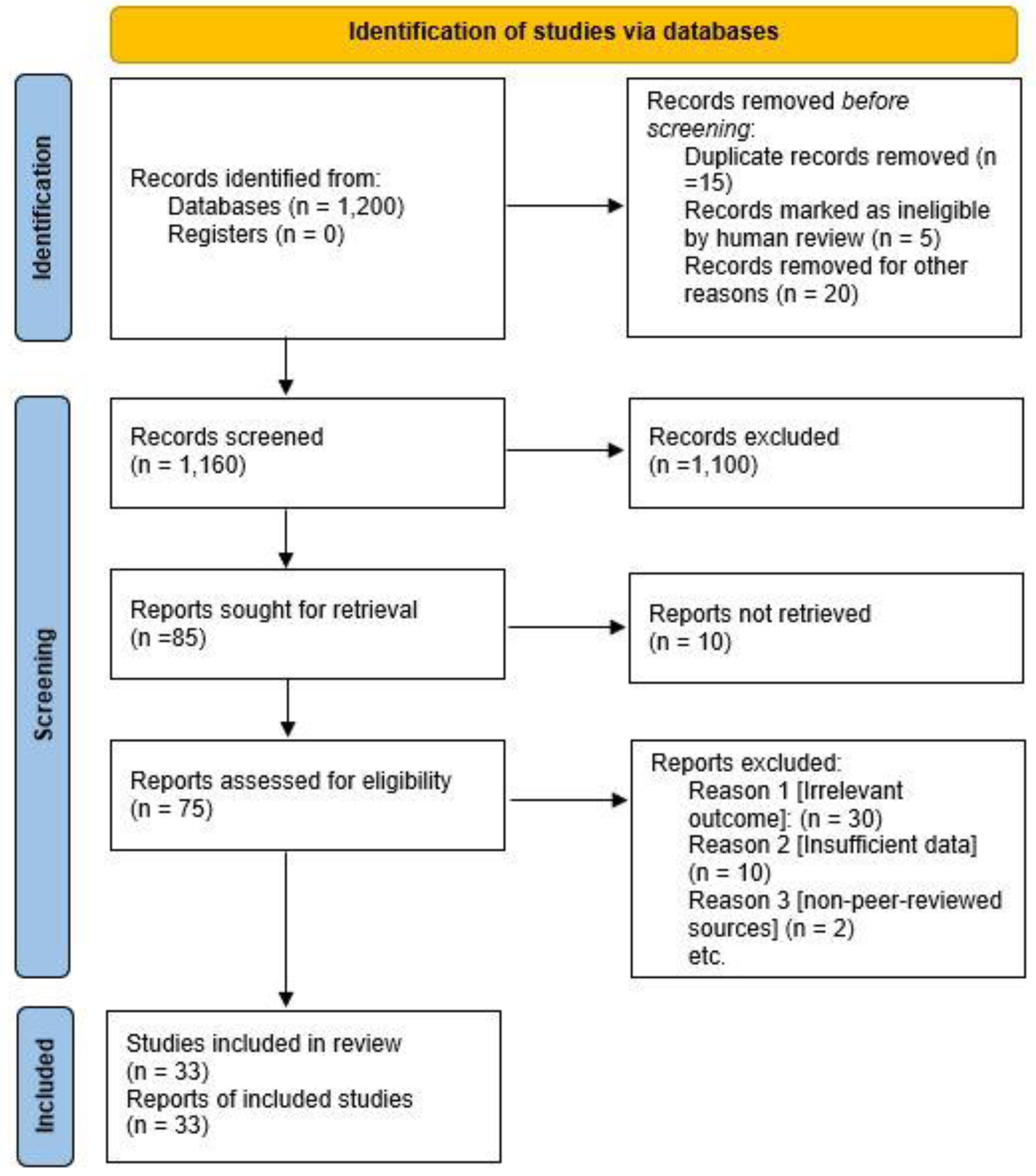
2.3. Study Selection and Screening Process
2.4. Data Extraction
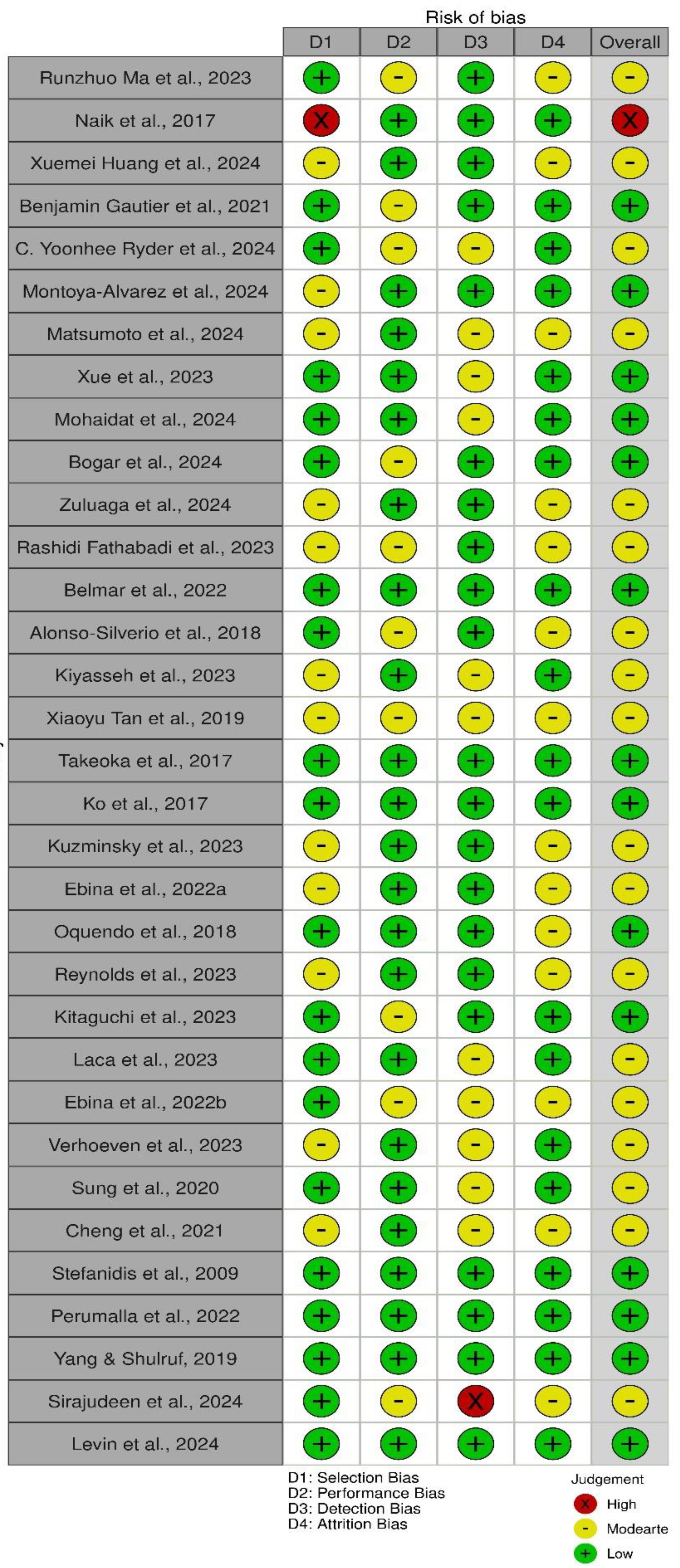
2.5. Risk of Bias Assessment
3. Results and Findings
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AI | Artificial Intelligence |
| DTW | Dynamic Time Warping |
| FP | Future Potential |
| FST | Future Surgeons Training |
| LST | Laparoscopic Suturing Training |
| LR | Large-Scale Research |
| LE | Lasting Retention of Essential Techniques |
| ML | Machine Learning |
| MU | Multi-Center Studies |
| OSATS | Objective Structured Assessment of Technical Skills |
| PA | Procedural Accuracy |
| RC | Resource-Constrained |
| RCT | Randomized Controlled Trial |
| RTC | Real-Time Feedback and Correction |
| SR | Skill Retention |
| STP | Short-Term Performance |
| SSE | Sustainable Surgical Education |
| SS | Surgical Skills |
| LTP | Long-Term Performance |
| VR | Virtual Reality |
References
- Monnet, E.; Twedt, D.C. Laparoscopy. Vet. Clin. Small Anim. Pract. 2003, 33, 1147–1163. [Google Scholar] [CrossRef]
- Chamberlain, G. Gynaecological laparoscopy. Ann. R. Coll. Surg. Engl. 1980, 62, 113. [Google Scholar] [PubMed]
- Soper, N.J.; Brunt, L.M.; Kerbl, K. Laparoscopic general surgery. N. Engl. J. Med. 1994, 330, 409–419. [Google Scholar] [CrossRef] [PubMed]
- Himal, H.S. Minimally invasive (laparoscopic) surgery. Surg. Endosc. Other Interv. Tech. 2002, 16, 1647–1652. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.; Ghosh, S.; Niklewski, P.; Roy, S. Laparoscopic suturing as a barrier to broader adoption of laparoscopic surgery. JSLS 2017, 21, e2017. [Google Scholar] [CrossRef] [PubMed]
- Baron, T.H.; DiMaio, C.J.; Wang, A.Y.; Morgan, K.A. American Gastroenterological Association clinical practice update: Management of pancreatic necrosis. Gastroenterology 2020, 158, 67–75. [Google Scholar] [CrossRef]
- de’Angelis, N.; Catena, F.; Memeo, R.; Coccolini, F.; Martínez-Pérez, A.; Romeo, O.M.; De Simone, B.; Di Saverio, S.; Brustia, R.; Rhaiem, R.; et al. 2020 WSES guidelines for the detection and management of bile duct injury during cholecystectomy. World J. Emerg. Surg. 2021, 16, 30. [Google Scholar] [CrossRef]
- Vilos, G.A.; Ternamian, A.; Laberge, P.Y.; Vilos, A.G.; Abu-Rafea, B.; Scattolon, S.; Leyland, N. Guideline No. 412: Laparoscopic entry for gynaecological surgery. J. Obstet. Gynaecol. Can. 2021, 43, 376–389. [Google Scholar] [CrossRef]
- Berguer, R.; Forkey, D.L.; Smith, W.D. Ergonomic problems associated with laparoscopic surgery. Surg. Endosc. 1999, 13, 466–468. [Google Scholar] [CrossRef]
- Bansal, V.K.; Tamang, T.; Misra, M.C.; Prakash, P.; Rajan, K.; Bhattacharjee, H.K.; Kumar, S.; Goswami, A. Laparoscopic suturing skills acquisition: A comparison between laparoscopy-exposed and laparoscopy-naive surgeons. JSLS 2012, 16, 623. [Google Scholar] [CrossRef]
- Elbiss, H.M.; Abu-Zidan, F.M. Establishment of a urogynecology cadaver-based hands-on workshop. Afr. Health Sci. 2023, 23, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Yiasemidou, M.; Gkaragkani, E.; Glassman, D.; Biyani, C.S. Cadaveric simulation: A review of reviews. Ir. J. Med. Sci. 2018, 187, 827–833. [Google Scholar] [CrossRef] [PubMed]
- Tamate, M.; Matsuura, M.; Kanao, H.; Saito, T. A mixed-method evaluation of cadaver surgery training for gynecologic oncology. J. Obstet. Gynaecol. Res. 2022, 48, 3252–3261. [Google Scholar] [CrossRef] [PubMed]
- Tang, B.; Zhang, L.; Alijani, A. Evidence to support the early introduction of laparoscopic suturing skills into the surgical training curriculum. BMC Med. Educ. 2020, 20, 70. [Google Scholar] [CrossRef]
- Westwood, E.; Malla, B.; Ward, J.; Lal, R.; Aryal, K. The impact of a laparoscopic surgery training course in a developing country. World J. Surg. 2020, 44, 3284–3289. [Google Scholar] [CrossRef]
- Ohtake, S.; Makiyama, K.; Yamashita, D.; Tatenuma, T.; Yao, M. Training on a virtual reality laparoscopic simulator improves performance of live laparoscopic surgery. Asian J. Endosc. Surg. 2022, 15, 313–319. [Google Scholar] [CrossRef]
- Ackermann, J.; Pahls, J.; Baumann, J.; Spüntrup, C.; Holthaus, B.; Noé, G.; Anapolski, M.; Meinhold-Heerlein, I.; Laganà, A.S.; Peters, G.; et al. The pelvitrainer for training in laparoscopic surgery–a prospective, multicenter, interdisciplinary study: Experimental research. Int. J. Surg. 2022, 101, 106604. [Google Scholar] [CrossRef]
- Bogar, P.Z.; Virag, M.; Bene, M.; Hardi, P.; Matuz, A.; Schlegl, A.T.; Toth, L.; Molnar, F.; Nagy, B.; Rendeki, S.; et al. Validation of a novel, low-fidelity virtual reality simulator and an artificial intelligence assessment approach for peg transfer laparoscopic training. Sci. Rep. 2024, 14, 16702. [Google Scholar] [CrossRef]
- Chuang, S.-H.; Chuang, S.-C. Single-incision laparoscopic surgery to treat hepatopancreatobiliary cancer: A technical review. World J. Gastroenterol. 2022, 28, 3359. [Google Scholar] [CrossRef]
- Hamilton, A. The Future of Artificial Intelligence in Surgery. Cureus 2024, 16, e63699. [Google Scholar] [CrossRef]
- Varas, J.; Coronel, B.V.; Villagrán, I.; Escalona, G.; Hernandez, R.; Schuit, G.; Durán, V.; Lagos-Villaseca, A.; Jarry, C.; Neyem, A.; et al. Innovations in surgical training: Exploring the role of artificial intelligence and large language models (LLM). Rev. Col. Bras. Cir. 2023, 50, e20233605. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Ma, R.; Kiyasseh, D.; Laca, J.A.; Kocielnik, R.; Wong, E.Y.; Chu, T.N.; Cen, S.Y.; Yang, C.H.; Dalieh, I.S.; Haque, T.F.; et al. Artificial intelligence-based video feedback to improve novice performance on robotic suturing skills: A pilot study. J. Endourol. 2024, 38, 884–891. [Google Scholar] [CrossRef]
- Naik, N.D.; Abbott, E.F.; Gas, B.L.; Murphy, B.L.; Farley, D.R.; Cook, D.A. Personalized video feedback improves suturing skills of incoming general surgery trainees. Surgery 2018, 163, 921–926. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Wang, P.; Chen, J.; Huang, Y.; Liao, Q.; Huang, Y.; Liu, Z.; Peng, D. An intelligent grasper to provide real-time force feedback to shorten the learning curve in laparoscopic training. BMC Med. Educ. 2024, 24, 161. [Google Scholar] [CrossRef]
- Gautier, B.; Tugal, H.; Tang, B.; Nabi, G.; Erden, M.S. Real-time 3D tracking of laparoscopy training instruments for assessment and feedback. Front. Robot. AI 2021, 8, 751741. [Google Scholar] [CrossRef]
- Ryder, C.Y.; Mott, N.M.; Gross, C.L.; Anidi, C.; Shigut, L.; Bidwell, S.S.; Kim, E.; Zhao, Y.; Ngam, B.N.; Snell, M.J.; et al. Using artificial intelligence to gauge competency on a novel laparoscopic training system. J. Surg. Educ. 2024, 81, 267–274. [Google Scholar] [CrossRef]
- Salvador, M.-A.; Arturo, M.-M.; Fernando, P.-E.; Danely, M.-G.D.; Jorge, R.-L.; Roberto, S.-M.; Rafael, R.-B.J.; Jesús, T.-J. Effects of Real Time Feedback on Novice’s Laparoscopic Learning Curve. J. Surg. Educ. 2024, 81, 1133–1153. [Google Scholar] [CrossRef]
- Matsumoto, S.; Kawahira, H.; Fukata, K.; Doi, Y.; Kobayashi, N.; Hosoya, Y.; Sata, N. Laparoscopic distal gastrectomy skill evaluation from video: A new artificial intelligence-based instrument identification system. Sci. Rep. 2024, 14, 12432. [Google Scholar] [CrossRef]
- Xue, Y.; Hu, A.; Muralidhar, R.; Ady, J.W.; Bongu, A.; Roshan, U. An AI system for evaluating pass fail in fundamentals of laparoscopic surgery from live video in realtime with performative feedback. In Proceedings of the 2023 IEEE International Conference on Bioinformatics and Biomedicine (BIBM), Istanbul, Turkiye, 5–8 December 2023; IEEE: Piscataway, NJ, USA, 2023; pp. 4167–4171. [Google Scholar]
- Mohaidat, M.; Fathabadi, F.R.; Alkhamaiseh, K.N.; Grantner, J.; Shebrain, S.A.; Abdel-Qader, I. A Systematic Approach to the Development of an Automated Assessment System for Laparoscopic Surgery Fundamentals. In Proceedings of the 2024 IEEE 18th International Symposium on Applied Computational Intelligence and Informatics (SACI), Timisoara, Romania, 23–25 May 2024; IEEE: Piscataway, NJ, USA, 2024; pp. 133–138. [Google Scholar]
- Zuluaga, L.; Rich, J.M.; Gupta, R.; Pedraza, A.; Ucpinar, B.; Okhawere, K.E.; Saini, I.; Dwivedi, P.; Patel, D.; Zaytoun, O.; et al. AI-powered real-time annotations during urologic surgery: The future of training and quality metrics. In Urologic Oncology: Seminars and Original Investigations; Elsevier: Amsterdam, The Netherlands, 2024; pp. 57–66. [Google Scholar]
- Fathabadi, F.R.; Grantner, J.L.; Shebrain, S.A.; Abdel-Qader, I. Autonomous sequential surgical skills assessment for the peg transfer task in a laparoscopic box-trainer system with three cameras. Robotica 2023, 41, 1837–1855. [Google Scholar] [CrossRef]
- Belmar, F.; Gaete, M.I.; Escalona, G.; Carnier, M.; Durán, V.; Villagrán, I.; Asbun, D.; Cortés, M.; Neyem, A.; Crovari, F.; et al. Artificial intelligence in laparoscopic simulation: A promising future for large-scale automated evaluations. Surg. Endosc. 2023, 37, 4942–4946. [Google Scholar] [CrossRef]
- Alonso-Silverio, G.A.; Pérez-Escamirosa, F.; Bruno-Sanchez, R.; Ortiz-Simon, J.L.; Muñoz-Guerrero, R.; Minor-Martinez, A.; Alarcón-Paredes, A. Development of a laparoscopic box trainer based on open source hardware and artificial intelligence for objective assessment of surgical psychomotor skills. Surg. Innov. 2018, 25, 380–388. [Google Scholar] [CrossRef] [PubMed]
- Kiyasseh, D.; Laca, J.; Haque, T.F.; Miles, B.J.; Wagner, C.; Donoho, D.A.; Anandkumar, A.; Hung, A.J. A multi-institutional study using artificial intelligence to provide reliable and fair feedback to surgeons. Commun. Med. 2023, 3, 42. [Google Scholar] [CrossRef] [PubMed]
- Tan, X.; Chng, C.-B.; Su, Y.; Lim, K.-B.; Chui, C.-K. Robot-assisted training in laparoscopy using deep reinforcement learning. IEEE Robot. Autom. Lett. 2019, 4, 485–492. [Google Scholar] [CrossRef]
- Takeoka, T.; Takiguchi, S.; Uemura, M.; Miyazaki, Y.; Takahashi, T.; Kurokawa, Y.; Makino, T.; Yamasaki, M.; Mori, M.; Doki, Y. Assessment potential of a new suture simulator in laparoscopic surgical skills training. Minim. Invasive Ther. Allied Technol. 2017, 26, 338–345. [Google Scholar] [CrossRef]
- Ko, J.K.Y.; Cheung, V.Y.T.; Pun, T.C.; Tung, W.K. A randomized controlled trial comparing trainee-directed virtual reality simulation training and box trainer on the acquisition of laparoscopic suturing skills. J. Obstet. Gynaecol. Can. 2018, 40, 310–316. [Google Scholar] [CrossRef]
- Kuzminsky, J.; Phillips, H.; Sharif, H.; Moran, C.; Gleason, H.E.; Topulos, S.P.; Pitt, K.; McNeil, L.K.; McCoy, A.M.; Kesavadas, T. Reliability in performance assessment creates a potential application of artificial intelligence in veterinary education: Evaluation of suturing skills at a single institution. Am. J. Vet. Res. 2023, 84. [Google Scholar] [CrossRef]
- Ebina, K.; Abe, T.; Hotta, K.; Higuchi, M.; Furumido, J.; Iwahara, N.; Kon, M.; Miyaji, K.; Shibuya, S.; Lingbo, Y.; et al. Objective evaluation of laparoscopic surgical skills in wet lab training based on motion analysis and machine learning. Langenbeck’s Arch. Surg. 2022, 407, 2123–2132. [Google Scholar] [CrossRef] [PubMed]
- Oquendo, Y.A.; Riddle, E.W.; Hiller, D.; Blinman, T.A.; Kuchenbecker, K.J. Automatically rating trainee skill at a pediatric laparoscopic suturing task. Surg. Endosc. 2018, 32, 1840–1857. [Google Scholar] [CrossRef]
- Reynolds, C.W.; Rooney, D.M.; Jeffcoach, D.R.; Barnard, M.; Snell, M.J.; El-Hayek, K.; Ngam, B.N.; Bidwell, S.S.; Anidi, C.; Tanyi, J.; et al. Evidence supporting performance measures of laparoscopic appendectomy through a novel surgical proficiency assessment tool and low-cost laparoscopic training system. Surg. Endosc. 2023, 37, 7170–7177. [Google Scholar] [CrossRef]
- Kitaguchi, D.; Teramura, K.; Matsuzaki, H.; Hasegawa, H.; Takeshita, N.; Ito, M. Automatic purse-string suture skill assessment in transanal total mesorectal excision using deep learning-based video analysis. BJS Open 2023, 7, zrac176. [Google Scholar] [CrossRef]
- Laca, J.A.; Kiyasseh, D.; Kocielnik, R.; Haque, T.F.; Ma, R.; Anandkumar, A.; Hung, A.J. PD30-05 AI-based video feedback to improve novice performance on a robotic suturing task. J. Urol. 2023, 209 (Suppl. 4), e832. [Google Scholar] [CrossRef]
- Ebina, K.; Abe, T.; Hotta, K.; Higuchi, M.; Furumido, J.; Iwahara, N.; Kon, M.; Miyaji, K.; Shibuya, S.; Lingbo, Y.; et al. Automatic assessment of laparoscopic surgical skill competence based on motion metrics. PLoS ONE 2022, 17, e0277105. [Google Scholar] [CrossRef] [PubMed]
- Verhoeven, D.J.; Hillemans, V.; Leijte, E.; Verhoeven, B.H.; Botden, S.M.B.I. Assessment of minimally invasive suturing skills: Is instrument tracking an accurate prediction? J. Laparoendosc. Adv. Surg. Tech. 2023, 33, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Sung, M.Y.; Kang, B.; Kim, J.; Kim, T.; Song, H. Intelligent haptic virtual simulation for suture surgery. Int. J. Adv. Comput. Sci. Appl. 2020, 11, 54–59. [Google Scholar] [CrossRef]
- Cheng, K.; You, J.; Wu, S.; Chen, Z.; Zhou, Z.; Guan, J.; Peng, B.; Wang, X. Artificial intelligence-based automated laparoscopic cholecystectomy surgical phase recognition and analysis. Surg. Endosc. 2022, 36, 3160–3168. [Google Scholar] [CrossRef]
- Stefanidis, D.; Hope, W.W.; Korndorffer, J.R., Jr.; Markley, S.; Scott, D.J. Initial laparoscopic basic skills training shortens the learning curve of laparoscopic suturing and is cost-effective. J. Am. Coll. Surg. 2010, 210, 436–440. [Google Scholar] [CrossRef]
- Perumalla, C.; Kearse, L.; Peven, M.; Laufer, S.; Goll, C.; Wise, B.; Yang, S.; Pugh, C. AI-based video segmentation: Procedural steps or basic maneuvers? J. Surg. Res. 2023, 283, 500–506. [Google Scholar] [CrossRef]
- Yang, Y.-Y.; Shulruf, B. An expert-led and artificial intelligence system-assisted tutoring course to improve the confidence of Chinese medical interns in suturing and ligature skills: A prospective pilot study. J. Educ. Eval. Health Prof. 2019, 16, 7. [Google Scholar] [CrossRef]
- Sirajudeen, N.; Boal, M.; Anastasiou, D.; Xu, J.; Stoyanov, D.; Kelly, J.; Collins, J.W.; Sridhar, A.; Mazomenos, E.; Francis, N.K. Deep learning prediction of error and skill in robotic prostatectomy suturing. Surg. Endosc. 2024, 38, 7663–7671. [Google Scholar] [CrossRef]
- Levin, I.; Ferman, J.R.; Bar, O.; Ayoun, D.B.; Cohen, A.; Wolf, T. Introducing surgical intelligence in gynecology: Automated identification of key steps in hysterectomy. Int. J. Gynecol. Obstet. 2024, 166, 1273–1278. [Google Scholar] [CrossRef] [PubMed]
- Postema, R.R.; van Gastel, L.A.; Hardon, S.F.; Bonjer, H.J.; Horeman, T. Haptic exploration improves performance of a laparoscopic training task. Surg. Endosc. 2021, 35, 4175–4182. [Google Scholar] [CrossRef] [PubMed]
- Wong, E.Y.; Knudsen, J.E.; Ma, R.; Chu, T.N.; Lo, E.; Cen, S.; Hung, A.J. Randomized Control Trial Evaluating Different Modalities of Real-Time Surgical Feedback. Curr. Probl. Surg. 2025, 62, 101666. [Google Scholar] [CrossRef] [PubMed]
- Howard, T.; Szewczyk, J. Improving precision in navigating laparoscopic surgery instruments toward a planar target using haptic and visual feedback. Front. Robot. AI 2016, 3, 37. [Google Scholar] [CrossRef]
- Alaker, M.; Wynn, G.R.; Arulampalam, T. Virtual reality training in laparoscopic surgery: A systematic review & meta-analysis. Int. J. Surg. 2016, 29, 85–94. [Google Scholar]
- Kowalewski, K.-F.; Garrow, C.R.; Schmidt, M.W.; Benner, L.; Müller-Stich, B.P.; Nickel, F. Sensor-based machine learning for workflow detection and as key to detect expert level in laparoscopic suturing and knot-tying. Surg. Endosc. 2019, 33, 3732–3740. [Google Scholar] [CrossRef]
- Dayan, D.; Dvir, N.; Agbariya, H.; Nizri, E. Implementation of artificial intelligence-based computer vision model in laparoscopic appendectomy: Validation, reliability, and clinical correlation. Surg. Endosc. 2024, 38, 3310–3319. [Google Scholar] [CrossRef]

| Author(s), Year | Title | Research Design | Study Location | Key Findings |
|---|---|---|---|---|
| Runzhuo Ma et al., 2023 [23] | AI-based Video Feedback on Robotic Suturing Tasks | Randomized Controlled Trial | United States of America (USA) | AI feedback improved needle handling in underperformers; significant but selective performance improvement for suturing skill acquisition. |
| Naik et al., 2017 [24] | Personalized video feedback improves suturing skills of incoming general surgery trainees | Nonrandomized study: video feedback vs. no feedback | USA | The feedback group had higher completion rates and faster performance. Significant improvement in suturing time for the feedback group. Higher global ratings for feedback group. No difference in OSATS scores. |
| Xuemei Huang et al., 2024 [25] | Force-Feedback-Enabled Laparoscopic Grasper for Skill Improvement | Pre-experiment Training Program | China | Force feedback reduced the learning curve for novices and improved grip control. |
| Benjamin Gautier et al., 2021 [26] | Real-Time 3D Tracking System for Instrument Feedback in Laparoscopy | Algorithm Development | United Kingdom (UK) | Cost-effective, automated feedback system preserving physical interaction during training. |
| Ryder et al., 2023 [27] | Using Artificial Intelligence to Gauge Competency on a Novel Laparoscopic Training System | Experimental Study | Ethiopia, Cameroon, Kenya, and USA | AI-based scoring of laparoscopic simulation videos matched human assessments ~72.4% of the time. AI can help address training gaps in LMICs. |
| Montoya-Alvarez et al., 2024 [28] | Real-Time Feedback’s Impact on Laparoscopic Suturing Skills | Randomized Controlled Trial | Mexico | Visual feedback enhanced suturing proficiency and shortened the learning curve compared to haptic feedback or no feedback. |
| Matsumoto et al., 2024 [29] | Kinematic Analysis of Gastrectomy Using AI | Retrospective Video Analysis | Japan | AI revealed differences in efficiency between novice and expert surgeons, suggesting application for real-time evaluation. |
| Xue et al., 2023 [30] | Pass/Fail Evaluation System for Fundamentals of Surgery (FLS) | Experimental Video Analysis | USA | AI achieved 78.6% accuracy in real-time assessment, improving feedback and training efficiency. |
| Mohaidat et al., 2024 [31] | AI-Driven Deep Learning for Peg Transfer and Suturing Assessment | Developmental Study with Computer Vision | USA (Multiple Centers) | Deep learning models provided high precision in peg transfer tasks, offering potential for standardized training evaluation. |
| Bogar et al., 2024 [18] | Comparison of VR Simulators vs. Box Trainers for Laparoscopic Training | Randomized Controlled Study | Hungary | VR simulators were equally effective as box trainers; AI reduced assessment time by 30%, maintaining 95% accuracy. |
| Zuluaga et al., 2024 [32] | Real-Time AI Annotations for Robotic Surgery | Symposium and Live Demonstration | Palo Alto, USA | AI annotated key steps and safety milestones during live surgeries, demonstrating potential for intraoperative decision-making. |
| Rashidi Fathabadi et al., 2023 [33] | Multi-Camera AI-Based Assessment for Peg Transfer Tasks | Experimental Study with Deep Learning | USA | High-precision assessment model for peg transfer tasks, eliminating the need for manual evaluation. |
| Belmar et al., 2023 [34] | AI-Expert Agreement on Remote Training Platforms | Observational Study | Latin America | AI showed 93% agreement with expert evaluations, indicating reliability for large-scale training assessment. |
| Alonso-Silverio et al., 2018 [35] | Affordable AI-Powered Laparoscopic Trainer | Experimental Design | Mexico | The AI-powered system improved accessibility and confidence in skill acquisition in resource-limited settings. |
| Kiyasseh et al., 2023 [36] | Reliability of AI Feedback in Surgical Video Explanations | Multi-Institutional AI Feedback Study | Multiple Locations | AI feedback often aligned with human evaluations, with improvements via explanation strategies like TWIX. |
| Xiaoyu Tan et al., 2019 [37] | Robot-Assisted Training System with Deep Reinforcement Learning | Experimental Robot-Assisted Training Study | Singapore | Reinforcement learning significantly improved laparoscopic training outcomes, providing tailored feedback and action simulation. |
| Takeoka et al., 2017 [38] | Assessment potential of a new suture simulator in laparoscopic surgical skills training | Pre- and post-training evaluation using a hybrid simulator | Japan | Significant improvement in air pressure leakage, number of full-thickness sutures, suture tension, wound area, and performance time. Performance was significantly better post-training. |
| Ko et al., 2017 [39] | Randomized Controlled Trial Comparing Trainee-Directed Virtual Reality Simulation Training and Box Trainer on the Acquisition of Laparoscopic Suturing Skills | Randomized Controlled Trial (RCT) | China | No significant difference in successful task completion, suturing time, or assessment scores between virtual reality simulator, box trainer, and control groups. Novices required longer training time to master suturing. Trainees had difficulty accurately assessing their own skill level. |
| Kuzminsky et al., 2023 [40] | Comparing AI and Traditional Assessments in Veterinary Suturing Skills | Comparative Observational Study | USA | AI showed higher reliability in skill differentiation, suggesting potential for objective assessment in surgical education. |
| Ebina et al., 2022 [41] | AI for Objective Surgical Skill Assessment in Wet Lab Training | Experimental Study with Motion Analysis | Japan | AI and motion capture metrics correlated with expert ratings, demonstrating potential for automated skill credentialing. |
| Oquendo et al., 2018 [42] | Paediatrics Laparoscopic Suturing Evaluation with AI | Experimental Study with Motion Tracking | USA | AI achieved 71% alignment with human expert ratings, enhancing feedback for pediatric surgical training. |
| Reynolds et al., 2023 [43] | Evidence Supporting Performance Measures of Laparoscopic Appendectomy Through a Novel Surgical Proficiency Assessment Tool and Low-Cost Laparoscopic Training System | Pilot Study | Ethiopia, Cameroon, and USA | The APPY-VOP tool effectively distinguished skill levels in laparoscopic appendectomy. Peer rating showed consistent evaluations. Promising for training scalability. |
| Kitaguchi et al., 2023 [44] | Suturing Skill Assessment in Trans-anal Total Meso-rectal Excision Using Deep Learning | Retrospective Video Analysis Study | Japan | AI scoring correlated with manual assessments, supporting its use in skill evaluation for advanced surgical tasks. |
| Laca et al., 2023 [45] | AI-Based Video Feedback to Improve Novice Performance on a Robotic Suturing Task | Randomized Controlled Trial (RCT) | USA | AI-based feedback improved needle handling and driving skills, with underperformers benefiting the most, demonstrating the potential of personalized AI feedback in training. |
| Ebina et al., 2022 [46] | Machine Learning Credentialing System for Porcine Organ Simulations | Experimental Study | Japan | Machine learning demonstrated 70% accuracy in assessing laparoscopic competence, supporting scalable skill assessments. |
| Verhoeven et al., 2022 [47] | Assessment of Minimally Invasive Suturing Skills | Experimental Study | Netherlands | Instrument tracking showed skill improvement but had weak correlation with expert assessments. |
| Sung et al., 2020 [48] | Intelligent Haptic Virtual Simulation for Suture Surgery | Experimental Study | Republic of Korea | Developed an AI-assisted haptic VR simulation for suturing, reducing surgical training costs and time. |
| Cheng et al., 2021 [49] | AI-based Automated Laparoscopic Cholecystectomy Analysis | Cohort Study | China (Multiple Centers) | The deep learning model identified surgical phases with high accuracy; accuracy varied with case complexity. |
| Stefanidis et al., 2009 [50] | Initial Laparoscopic Basic Skills Training Shortens the Learning Curve of Laparoscopic Suturing and Is Cost-Effective | Randomized Controlled Trial (RCT) | USA | Basic laparoscopic skills training before suturing reduces learning time and cost. Group I (basic skills training) had a shorter suturing learning curve and needed less active instruction. Cost savings of USD 148 per trainee. |
| Perumalla et al., 2022 [51] | AI-Based Video Segmentation: Procedural Steps or Basic Manoeuvres | Deep Learning Algorithm Study | USA | The AI algorithm achieved 84% accuracy in differentiating basic maneuvers (suturing, knot tying, and suture cutting). Precision: 87.9% for suture throws, 60% for knot ties, and 90.9% for suture cutting. Basic maneuvers aid in error management and skill assessment. |
| Yang and Shulruf, 2019 [52] | An Expert-Led and Artificial Intelligence System-Assisted Tutoring Course to Improve the Confidence of Chinese Medical Interns in Suturing and Ligature Skills: A Prospective Pilot Study | Pilot Study | China | Compared regular training, expert-led tutoring, and expert-led + AI tutoring, with the AI-integrated group showing the best OSCE performance and confidence, especially after three AI sessions, underscoring AI’s value in surgical education. |
| Sirajudeen et al., 2024 [53] | Deep Learning Prediction of Errors in Robotic Suturing | Observational Study | UK | The AI model predicted surgical errors with strong correlations to human assessments in robotic prostatectomy. |
| Levin et al., 2024 [54] | Automated Identification of Key Steps in Hysterectomy | Retrospective Study | Israel (Five Medical Centers) | AI accurately identified surgical steps in hysterectomy with high precision; further research is needed for clinical application. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ogbonnaya, C.N.; Li, S.; Tang, C.; Zhang, B.; Sullivan, P.; Erden, M.S.; Tang, B. Exploring the Role of Artificial Intelligence (AI)-Driven Training in Laparoscopic Suturing: A Systematic Review of Skills Mastery, Retention, and Clinical Performance in Surgical Education. Healthcare 2025, 13, 571. https://doi.org/10.3390/healthcare13050571
Ogbonnaya CN, Li S, Tang C, Zhang B, Sullivan P, Erden MS, Tang B. Exploring the Role of Artificial Intelligence (AI)-Driven Training in Laparoscopic Suturing: A Systematic Review of Skills Mastery, Retention, and Clinical Performance in Surgical Education. Healthcare. 2025; 13(5):571. https://doi.org/10.3390/healthcare13050571
Chicago/Turabian StyleOgbonnaya, Chidozie N., Shizhou Li, Changshi Tang, Baobing Zhang, Paul Sullivan, Mustafa Suphi Erden, and Benjie Tang. 2025. "Exploring the Role of Artificial Intelligence (AI)-Driven Training in Laparoscopic Suturing: A Systematic Review of Skills Mastery, Retention, and Clinical Performance in Surgical Education" Healthcare 13, no. 5: 571. https://doi.org/10.3390/healthcare13050571
APA StyleOgbonnaya, C. N., Li, S., Tang, C., Zhang, B., Sullivan, P., Erden, M. S., & Tang, B. (2025). Exploring the Role of Artificial Intelligence (AI)-Driven Training in Laparoscopic Suturing: A Systematic Review of Skills Mastery, Retention, and Clinical Performance in Surgical Education. Healthcare, 13(5), 571. https://doi.org/10.3390/healthcare13050571





