Influence of Internet-Based Health Management on Control of Blood Glucose in Patients with Type 2 Diabetes: A Four-Year Longitudinal Study
Abstract
1. Introduction
2. Methods
2.1. Study Design
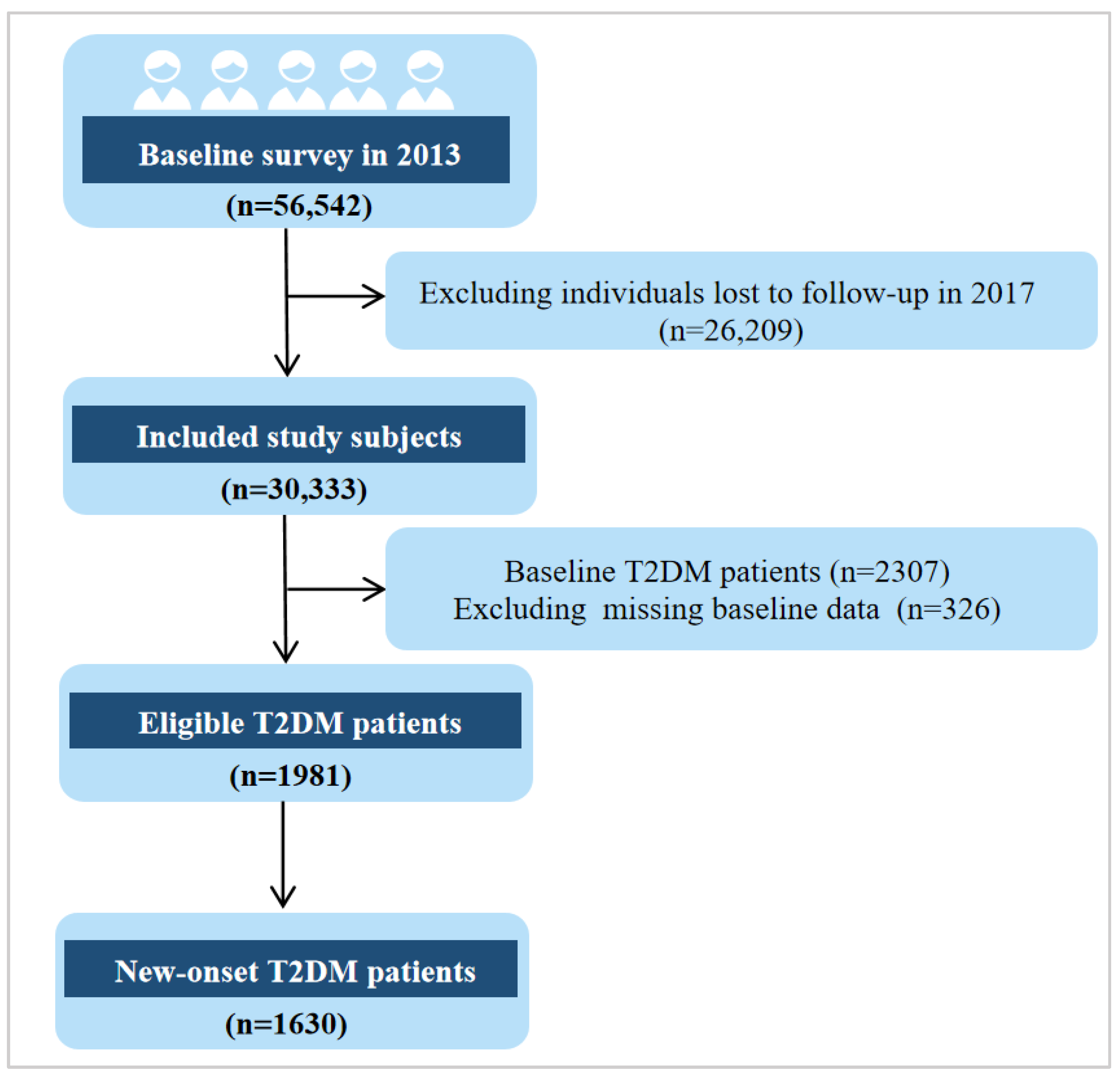
2.2. Participants
2.3. Setting
2.4. Self-Health Management Platform
2.5. Dietary Management
2.6. Exercise Management
2.7. Clinical Parameter Measurements
2.8. Questionnaire Survey
2.9. Statistical Analysis
3. Results
3.1. Basic Characteristics of Eligible Participants in 2013
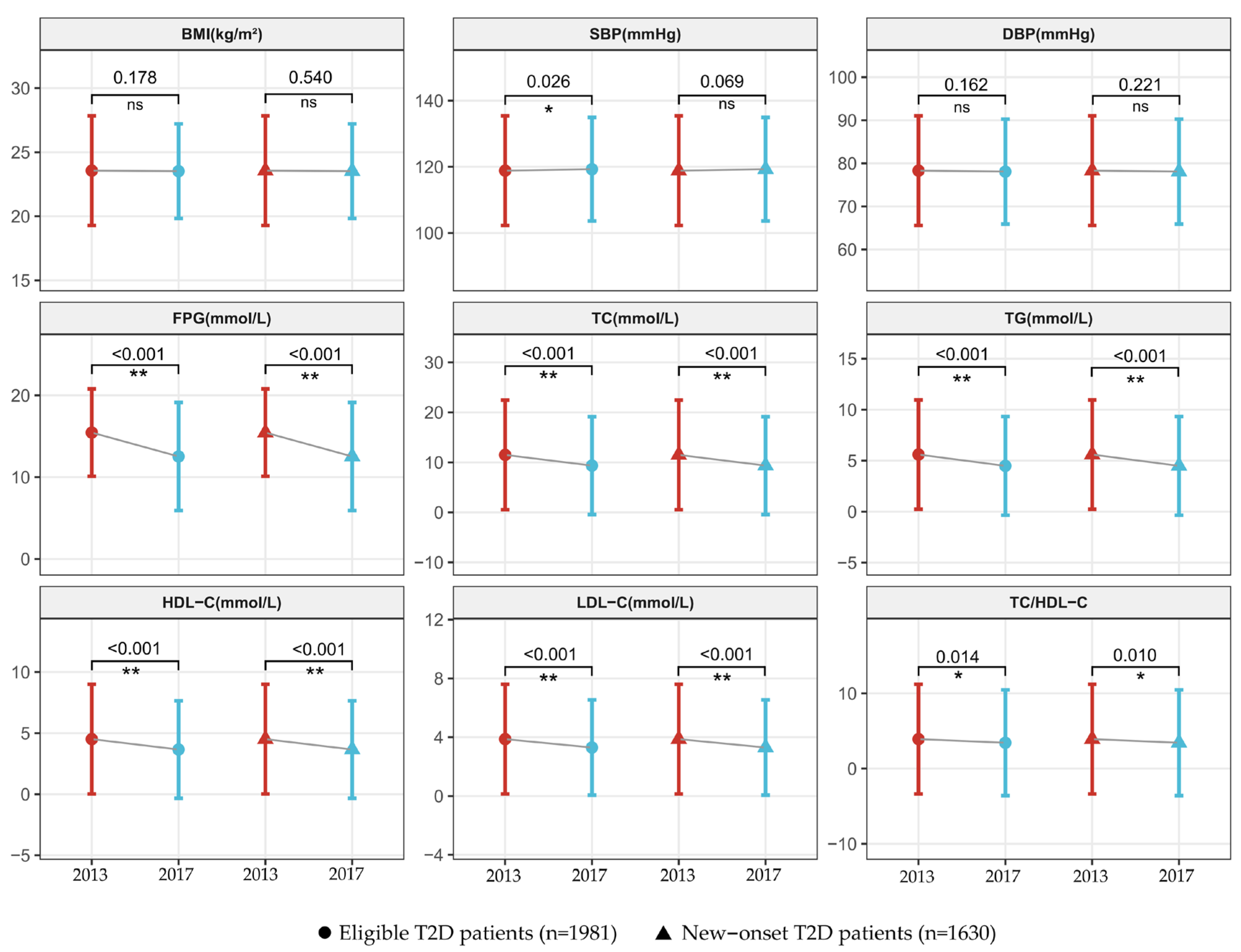
3.2. Change in Self-Management and Clinical Parameters of Eligible T2D Patients
3.3. Changes in Self-Management and Clinical Parameters of Participants with New-Onset Diabetes
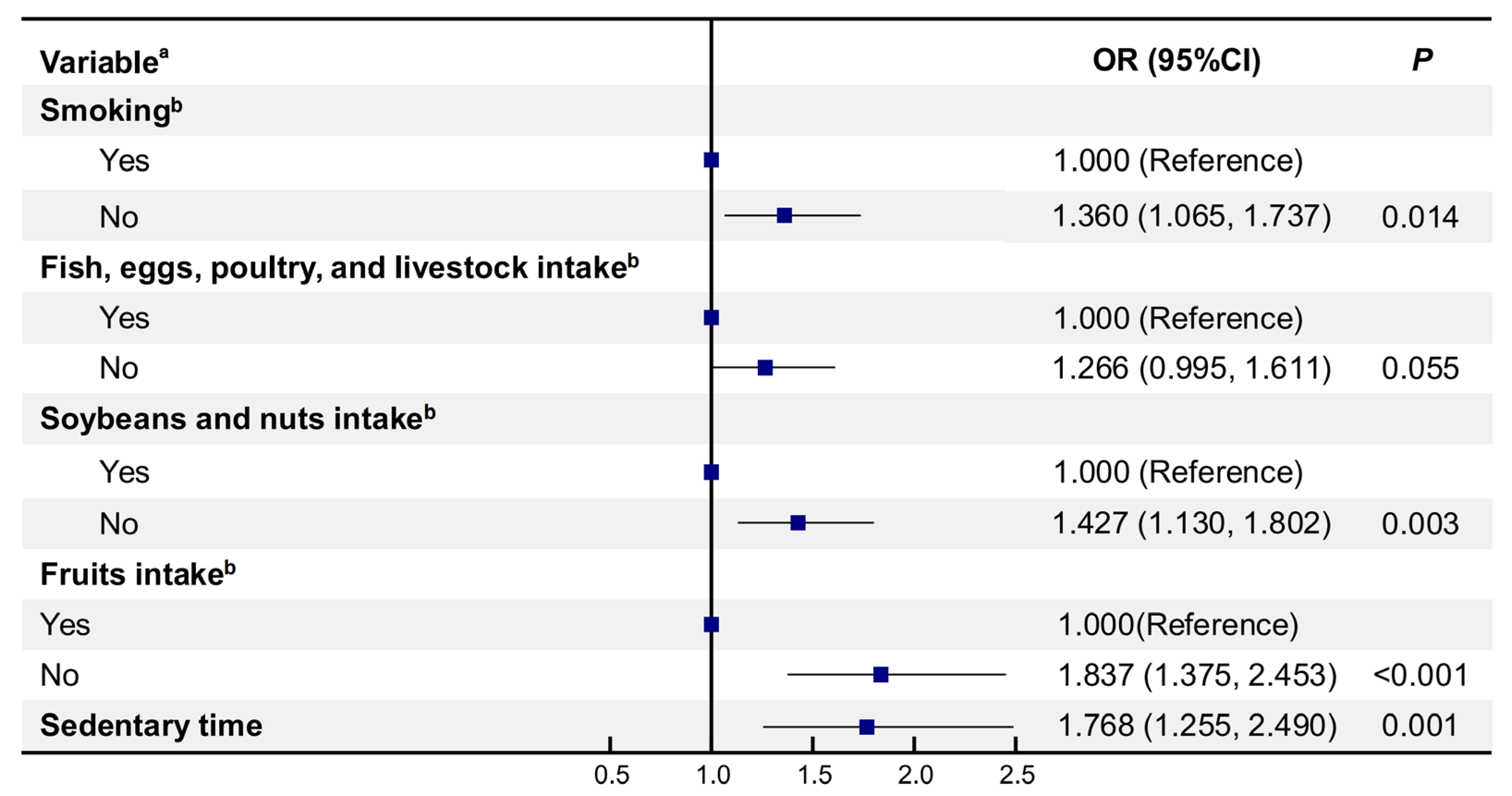
3.4. Factors Related to Blood Glucose Control in Participants with New-Onset Diabetes
3.5. Binary Logistic Regression Model of Factors Associated with Blood Glucose Control in New-Onset Patients
4. Discussion
4.1. Strengths and Limitations
4.2. The New Directions for Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Li, D.; Luo, M.; Liu, Y.; Dong, J.; Geng, W.; Li, X.; Yang, L.; Wang, J.; Cao, P. Increased Rates of Health Management and Health Education on Hypertension and Diabetes in Inner Mongolia, China: 10-Year Population Level Trends (2009–2018). Int. J. Environ. Res. Public Health 2022, 19, 13048. [Google Scholar] [CrossRef] [PubMed]
- Espinoza, P.; Varela, C.A.; Vargas, I.E.; Ortega, G.; Silva, P.A.; Boehmer, K.B.; Montori, V.M. The burden of treatment in people living with type 2 diabetes: A qualitative study of patients and their primary care clinicians. PLoS ONE 2020, 15, e0241485. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Wang, S.; Han, X.; Zhang, G.; Zhao, M.; Ma, L. Spatiotemporal trends and influence factors of global diabetes prevalence in recent years. Soc. Sci. Med. 2020, 256, 113062. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Hu, W.; Ye, S.; Deng, D.; Chen, M. The Description and Prediction of Incidence, Prevalence, Mortality, Disability-Adjusted Life Years Cases, and Corresponding Age-Standardized Rates for Global Diabetes. J. Epidemiol. Glob. Health 2023, 13, 566–576. [Google Scholar] [CrossRef]
- Shi, G.; Zhu, N.; Qiu, L.; Yan, H.; Zeng, L.; Wang, D.; Dang, S.; Li, Z.; Kang, Y.; Chen, T.; et al. Impact of the 2020 China Diabetes Society Guideline on the Prevalence of Diabetes Mellitus and Eligibility for Antidiabetic Treatment in China. Int. J. Gen. Med. 2021, 14, 6639–6645. [Google Scholar] [CrossRef]
- Wang, L.; Peng, W.; Zhao, Z.; Zhang, M.; Shi, Z.; Song, Z.; Zhang, X.; Li, C.; Huang, Z.; Sun, X.; et al. Prevalence and Treatment of Diabetes in China, 2013–2018. JAMA 2021, 326, 2498–2506. [Google Scholar] [CrossRef]
- Zhao, X.; Zhang, Y.; Yang, Y.; Pan, J. Diabetes-related avoidable hospitalisations and its relationship with primary healthcare resourcing in China: A cross-sectional study from Sichuan Province. Health Soc. Care Community 2022, 30, e1143–e1156. [Google Scholar] [CrossRef]
- Liang, F.; Yang, X.; Liu, F.; Li, J.; Xiao, Q.; Chen, J.; Liu, X.; Cao, J.; Shen, C.; Yu, L.; et al. Long-term exposure to ambient fine particulate matter and incidence of diabetes in China: A cohort study. Environ. Int. 2019, 126, 568–575. [Google Scholar] [CrossRef]
- Cho, N.H.; Shaw, J.E.; Karuranga, S.; Huang, Y.; da Rocha Fernandes, J.D.; Ohlrogge, A.W.; Malanda, B. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res. Clin. Pract. 2018, 138, 271–281. [Google Scholar] [CrossRef]
- Lee, M.K. Blood glucose control: Where are we? J. Diabetes Investig. 2021, 12, 1762–1764. [Google Scholar] [CrossRef]
- Awotidebe, T.O.; Adedoyin, R.A.; Afolabi, M.A.; Opiyo, R. Knowledge, attitude and practice of exercise for plasma blood glucose control among patients with type-2 diabetes. Diabetes Metab. Syndr. 2016, 10, S1–S6. [Google Scholar] [CrossRef] [PubMed]
- Aloke, C.; Egwu, C.O.; Aja, P.M.; Obasi, N.A.; Chukwu, J.; Akumadu, B.O.; Ogbu, P.N.; Achilonu, I. Current Advances in the Management of Diabetes Mellitus. Biomedicines 2022, 10, 2436. [Google Scholar] [CrossRef] [PubMed]
- Salama, I.I.; Sami, S.M.; Salama, S.I.; Abdel-Latif, G.A.; Aboulghate, A.; Raslan, H.M.; Mohsen, A.; Rasmy, H.; Ibrahim, M.H.; Ganem, M.M.; et al. Impact of lifestyle modification on glycemic control and cognitive function among Type II diabetes mellitus patients. Future Sci. OA 2023, 9, FSO835. [Google Scholar] [CrossRef] [PubMed]
- Uusitupa, M.; Khan, T.A.; Viguiliouk, E.; Kahleova, H.; Rivellese, A.A.; Hermansen, K.; Pfeiffer, A.; Thanopoulou, A.; Salas-Salvado, J.; Schwab, U.; et al. Prevention of Type 2 Diabetes by Lifestyle Changes: A Systematic Review and Meta-Analysis. Nutrients 2019, 11, 2611. [Google Scholar] [CrossRef]
- Wang, L.; Gao, P.; Zhang, M.; Huang, Z.; Zhang, D.; Deng, Q.; Li, Y.; Zhao, Z.; Qin, X.; Jin, D.; et al. Prevalence and Ethnic Pattern of Diabetes and Prediabetes in China in 2013. JAMA 2017, 317, 2515–2523. [Google Scholar] [CrossRef]
- Yoon, S.; Ng, J.H.; Kwan, Y.H.; Low, L.L. Healthcare Professionals’ Views of Factors Influencing Diabetes Self-Management and the Utility of a mHealth Application and Its Features to Support Self-Care. Front. Endocrinol. 2022, 13, 793473. [Google Scholar] [CrossRef]
- Hurst, C.P.; Rakkapao, N.; Hay, K. Impact of diabetes self-management, diabetes management self-efficacy and diabetes knowledge on glycemic control in people with Type 2 Diabetes (T2D): A multi-center study in Thailand. PLoS ONE 2020, 15, e0244692. [Google Scholar] [CrossRef]
- Yang, N.; Masingboon, K.; Samartkit, N. Factors influencing diabetes self-management among adults with type 2 diabetes mellitus in China. Belitung Nurs. J. 2022, 8, 389–395. [Google Scholar] [CrossRef]
- Pong, C.; Tseng, R.; Tham, Y.C.; Lum, E. Current Implementation of Digital Health in Chronic Disease Management: Scoping Review. J. Med. Internet Res. 2024, 26, e53576. [Google Scholar] [CrossRef]
- Appuswamy, A.V.; Desimone, M.E. Managing Diabetes in Hard to Reach Populations: A Review of Telehealth Interventions. Curr. Diabetes Rep. 2020, 20, 28. [Google Scholar] [CrossRef]
- Fitzner, K.K.; Heckinger, E.; Tulas, K.M.; Specker, J.; McKoy, J. Telehealth technologies: Changing the way we deliver efficacious and cost-effective diabetes self-management education. J. Health Care Poor Underserved 2014, 25, 1853–1897. [Google Scholar] [CrossRef] [PubMed]
- McDonnell, M.E. Telemedicine in Complex Diabetes Management. Curr. Diabetes Rep. 2018, 18, 42. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.Y.; Lee, S.W.H. Telemedicine Cost-Effectiveness for Diabetes Management: A Systematic Review. Diabetes Technol. Ther. 2018, 20, 492–500. [Google Scholar] [CrossRef] [PubMed]
- Whitehead, L.; Seaton, P. The Effectiveness of Self-Management Mobile Phone and Tablet Apps in Long-term Condition Management: A Systematic Review. J. Med. Internet Res. 2016, 18, e97. [Google Scholar] [CrossRef]
- Lim, S.L.; Ong, K.W.; Johal, J.; Han, C.Y.; Yap, Q.V.; Chan, Y.H.; Chooi, Y.C.; Zhang, Z.P.; Chandra, C.C.; Thiagarajah, A.G.; et al. Effect of a Smartphone App on Weight Change and Metabolic Outcomes in Asian Adults with Type 2 Diabetes: A Randomized Clinical Trial. JAMA Netw. Open 2021, 4, e2112417. [Google Scholar] [CrossRef]
- Hong, D.; Stoecker, C.; Shao, Y.; Nauman, E.; Fonseca, V.; Hu, G.; Bazzano, A.N.; Kabagambe, E.K.; Shi, L. Effects of Non-Face-to-Face Chronic Care Management on Service Utilization and Outcomes Among US Medicare Beneficiaries with Diabetes. J. Gen. Intern. Med. 2024, 39, 1985–1992. [Google Scholar] [CrossRef]
- Block, G.; Azar, K.M.; Romanelli, R.J.; Block, T.J.; Hopkins, D.; Carpenter, H.A.; Dolginsky, M.S.; Hudes, M.L.; Palaniappan, L.P.; Block, C.H. Diabetes Prevention and Weight Loss with a Fully Automated Behavioral Intervention by Email, Web, and Mobile Phone: A Randomized Controlled Trial Among Persons with Prediabetes. J. Med. Internet Res. 2015, 17, e240. [Google Scholar] [CrossRef]
- Dou, Y.; Chen, B.; Yu, X.; Ma, D. Effectiveness of Internet-based health management in patients with dyslipidemia: A four-year longitudinal study. Atherosclerosis 2023, 376, 34–42. [Google Scholar] [CrossRef]
- Hallal, P.C.; Victora, C.G. Reliability and Validity of the International Physical Activity Questionnaire (Ipaq). Med. Sci. Sports Exerc. 2004, 36, 7161. [Google Scholar] [CrossRef]
- Du, Z.; Wang, G.; Yan, D.; Yang, F.; Bing, D. Relationships between the Pittsburgh Sleep Quality Index (PSQI) and vertigo outcome. Neurol. Res. 2023, 45, 291–299. [Google Scholar] [CrossRef]
- Wang, S.-S.; Lay, S.; Yu, H.-N.; Shen, S.-R. Dietary Guidelines for Chinese Residents (2016): Comments and comparisons. J. Zhejiang Univ. Sci. B 2016, 17, 649–656. [Google Scholar] [CrossRef] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Ann. Intern. Med. 2007, 147, 573–577. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Chuang, L.M.; Chang, C.H.; Wang, C.S.; Wang, I.C.; Chung, Y.; Peng, H.Y.; Chen, H.C.; Hsu, Y.L.; Lin, Y.S.; et al. Evaluating self-management behaviors of diabetic patients in a telehealthcare program: Longitudinal study over 18 months. J. Med. Internet Res. 2013, 15, e266. [Google Scholar] [CrossRef] [PubMed]
- Park, G.; Lee, H.; Lee, Y.; Kim, M.S.; Jung, S.; Khang, A.R.; Yi, D. Automated Personalized Self-care Program for Patients with Type 2 Diabetes Mellitus: A Pilot Trial. Asian Nurs. Res. (Korean Soc. Nurs. Sci.) 2024, 18, 114–124. [Google Scholar] [CrossRef]
- Ruiz-Leon, A.M.; Casas, R.; Castro-Barquero, S.; Alfaro-Gonzalez, S.; Radeva, P.; Sacanella, E.; Casanovas-Garriga, F.; Perez-Gesali, A.; Estruch, R. Efficacy of a Mobile Health-Based Behavioral Treatment for Lifestyle Modification in Type 2 Diabetes Self-Management: Greenhabit Randomized Controlled Trial. J. Med. Internet Res. 2025, 27, e58319. [Google Scholar] [CrossRef]
- Sjoblom, L.; Hantikainen, E.; Dahlgren, A.; Trolle Lagerros, Y.; Bonn, S.E. The effect of an app-based dietary education on dietary intake and cardiometabolic risk markers in people with type 2 diabetes: Results from a randomized controlled trial. Nutr. J. 2025, 24, 2. [Google Scholar] [CrossRef]
- Wang, C.; Wang, Y.; Wu, J.; Liu, S.; Zhu, Y.; Lv, S.; Lin, P.; Wang, X.; Xu, Y.; Yu, S.; et al. Current Smoking Dose-Dependently Associated with Decreased beta-Cell Function in Chinese Men without Diabetes. J. Diabetes Res. 2015, 2015, 841768. [Google Scholar] [CrossRef]
- Durlach, V.; Verges, B.; Al-Salameh, A.; Bahougne, T.; Benzerouk, F.; Berlin, I.; Clair, C.; Mansourati, J.; Rouland, A.; Thomas, D.; et al. Smoking and diabetes interplay: A comprehensive review and joint statement. Diabetes Metab. 2022, 48, 101370. [Google Scholar] [CrossRef]
- Luque-Ramirez, M.; Sanz de Burgoa, V. Impact of smoking cessation on estimated cardiovascular risk in Spanish type 2 diabetes mellitus patients: The DIABETES study. Rev. Clin. Esp. 2018, 218, 391–398. [Google Scholar] [CrossRef]
- Muley, A.; Fernandez, R.; Ellwood, L.; Muley, P.; Shah, M. Effect of tree nuts on glycemic outcomes in adults with type 2 diabetes mellitus: A systematic review. JBI Evid. Synth. 2021, 19, 966–1002. [Google Scholar] [CrossRef]
- Dai, B.; Wu, Q.; Zeng, C.; Zhang, J.; Cao, L.; Xiao, Z.; Yang, M. The effect of Liuwei Dihuang decoction on PI3K/Akt signaling pathway in liver of type 2 diabetes mellitus (T2DM) rats with insulin resistance. J. Ethnopharmacol. 2016, 192, 382–389. [Google Scholar] [CrossRef] [PubMed]
- Liang, J.; He, Y.; Huang, C.; Ji, F.; Zhou, X.; Yin, Y. The Regulation of Selenoproteins in Diabetes: A New Way to Treat Diabetes. Curr. Pharm. Des. 2024, 30, 1541–1547. [Google Scholar] [CrossRef] [PubMed]
- Poolsup, N.; Suksomboon, N.; Paw, N.J. Effect of dragon fruit on glycemic control in prediabetes and type 2 diabetes: A systematic review and meta-analysis. PLoS ONE 2017, 12, e0184577. [Google Scholar] [CrossRef]
- Cheng, X.; Huang, J.; Li, H.; Zhao, D.; Liu, Z.; Zhu, L.; Zhang, Z.; Peng, W. Quercetin: A promising therapy for diabetic encephalopathy through inhibition of hippocampal ferroptosis. Phytomedicine 2024, 126, 154887. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Geng, J.; Zhang, S.; Zhang, K.; Yang, L.; Li, J.; Li, J. A Mobile-Based Intervention for Dietary Behavior and Physical Activity Change in Individuals at High Risk for Type 2 Diabetes Mellitus: Randomized Controlled Trial. JMIR Mhealth Uhealth 2020, 8, e19869. [Google Scholar] [CrossRef]
- Ryan, B.J.; Schleh, M.W.; Ahn, C.; Ludzki, A.C.; Gillen, J.B.; Varshney, P.; Van Pelt, D.W.; Pitchford, L.M.; Chenevert, T.L.; Gioscia-Ryan, R.A.; et al. Moderate-Intensity Exercise and High-Intensity Interval Training Affect Insulin Sensitivity Similarly in Obese Adults. J. Clin. Endocrinol. Metab. 2020, 105, e2941–e2959. [Google Scholar] [CrossRef]
- Kruse, C.S.; Betancourt, J.A.; Gonzales, M.; Dickerson, K.; Neer, M. Leveraging Mobile Health to Manage Mental Health/Behavioral Health Disorders: Systematic Literature Review. JMIR Ment. Health 2022, 9, e42301. [Google Scholar] [CrossRef]
- Friggi Sebe Petrelluzzi, K.; Garcia, M.C.; Petta, C.A.; Ribeiro, D.A.; de Oliveira Monteiro, N.R.; Cespedes, I.C.; Spadari, R.C. Physical therapy and psychological intervention normalize cortisol levels and improve vitality in women with endometriosis. J. Psychosom. Obstet. Gynaecol. 2012, 33, 191–198. [Google Scholar] [CrossRef]
- Armani Kian, A.; Vahdani, B.; Noorbala, A.A.; Nejatisafa, A.; Arbabi, M.; Zenoozian, S.; Nakhjavani, M. The Impact of Mindfulness-Based Stress Reduction on Emotional Wellbeing and Glycemic Control of Patients with Type 2 Diabetes Mellitus. J. Diabetes Res. 2018, 2018, 1986820. [Google Scholar] [CrossRef]
- Umar, A.; Khan, M.S.; Sehgal, S.A.; Jafar, K.; Ahmad, S.; Waheed, A.; Aslam, M.W.; Wajid, M.; Rehman, T.U.; Khan, T.; et al. Epidemiological studies of sleep disorder in educational community of Pakistani population, its major risk factors and associated diseases. PLoS ONE 2022, 17, e0266739. [Google Scholar] [CrossRef]
- Hamine, S.; Gerth-Guyette, E.; Faulx, D.; Green, B.B.; Ginsburg, A.S. Impact of mHealth chronic disease management on treatment adherence and patient outcomes: A systematic review. J. Med. Internet Res. 2015, 17, e52. [Google Scholar] [CrossRef] [PubMed]
- Bonn, S.E.; Hummel, M.; Peveri, G.; Eke, H.; Alexandrou, C.; Bellocco, R.; Lof, M.; Trolle Lagerros, Y. Effectiveness of a Smartphone App to Promote Physical Activity Among Persons with Type 2 Diabetes: Randomized Controlled Trial. Interact. J. Med. Res. 2024, 13, e53054. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Leng, Y.; Huo, D.; Zhao, D.; Zheng, J.; Zhao, P.; Yang, H.; Li, F.; Hou, C. A portable sensor for glucose detection in Huangshui based on blossom-shaped bimetallic organic framework loaded with silver nanoparticles combined with machine learning. Food Chem. 2023, 429, 136850. [Google Scholar] [CrossRef] [PubMed]
| Characteristic |
Total (n = 30,333) |
Non-T2DM (n = 28,026) |
T2DM (n = 2307) | p |
|---|---|---|---|---|
| Age, mean ± SD | 35.71 ± 8.17 | 35.64 ± 8.08) | 36.61 ± 9.15 | <0.001 |
| Gender, n (%) | <0.001 | |||
| Male | 19,236 (63.42) | 17,558 (62.65) | 1678 (72.74) | |
| Female | 11,097 (36.58) | 10,468 (37.35) | 629 (27.26) | |
| Family history of diabetes (father), n (%) | 1368 (4.51) | 1200 (4.28) | 168 (7.28) | <0.001 |
| Family history of diabetes (mother), n (%) | 1080 (3.56) | 953 (3.40) | 127 (5.50) | <0.001 |
| Tobacco use, n (%) | <0.001 | |||
| Non-smoking | 19,358 (63.85) | 18,105 (64.64) | 1253 (54.31) | |
| Current smoking | 10,075 (33.23) | 9143 (32.64) | 932 (40.40) | |
| Quit smoking | 885 (2.92) | 763 (2.72) | 122 (5.29) | |
| Alcohol consumption, n (%) | 0.001 | |||
| No alcoholic beverages | 18,635 (65.45) | 17,215 (65.72) | 1420 (62.42) | |
| Drinking | 9835 (34.55) | 8980 (34.28) | 855 (37.58) | |
| Cereals and potato intake, n (%) | 0.339 | |||
| Below | 13,119 (43.25) | 12,077 (43.09) | 1042 (45.17) | |
| Moderate | 8675 (28.60) | 8067 (28.78) | 608 (26.35) | |
| Higher | 8539 (28.15) | 7882 (28.12) | 657 (28.48) | |
| Fish, eggs, poultry, and livestock meat intake, n (%) | 0.011 | |||
| Below | 15,246 (50.26) | 14,030 (50.06) | 1216 (52.71) | |
| Moderate | 7600 (25.06) | 7039 (25.12) | 561 (24.32) | |
| Higher | 7487 (24.68) | 6957 (24.82) | 530 (22.97) | |
| Milk and dairy products intake, n (%) | 0.002 | |||
| Below | 26,839 (88.48) | 24,844 (88.65) | 1995 (86.48) | |
| Moderate | 3494 (11.52) | 3182 (11.35) | 312 (13.52) | |
| Soybeans and nuts intake, n (%) | <0.001 | |||
| Below | 20,058 (66.13) | 18,422 (65.73) | 1636 (70.91) | |
| Moderate | 1793 (5.91) | 1699 (6.06) | 94 (4.07) | |
| Higher | 8482 (27.96) | 7905 (28.21) | 577 (25.01) | |
| Vegetables intake, n (%) | <0.001 | |||
| Below | 22,798 (75.16) | 20,975 (74.84) | 1823 (79.02) | |
| Moderate | 5180 (17.08) | 4851 (17.31) | 329 (14.26) | |
| Higher | 2355 (7.76) | 2200 (7.85) | 155 (6.72) | |
| Fruits intake, n (%) | 0.002 | |||
| Below | 26,322 (86.78) | 24,258 (86.56) | 2064 (89.47) | |
| Moderate | 2994 (9.87) | 2826 (10.08) | 168 (7.28) | |
| Higher | 1017 (3.35) | 942 (3.36) | 75 (3.25) | |
| Quality of sleep, n (%) | <0.001 | |||
| Very good | 6922 (22.84) | 6447 (23.03) | 475 (20.59) | |
| Fair | 18,410 (60.75) | 17,133 (61.19) | 1277 (55.35) | |
| Not good | 4066 (13.42) | 3644 (13.01) | 422 (18.29) | |
| Very bad | 908 (3.00) | 775 (2.77) | 133 (5.77) | |
| Physical activity, n (%) | 0.011 | |||
| Low | 8983 (29.61) | 8213 (29.30) | 770 (33.38) | |
| Medium | 13,771 (45.40) | 12,811 (45.71) | 960 (41.61) | |
| High | 7579 (24.99) | 7002 (24.98) | 577 (25.01) | |
| Sleeping time, mean ± SD | 7.23 ± 1.18 | 7.23 ± 1.17 | 7.12 ± 1.33 | <0.001 |
| Psychological score, mean ± SD | 17.87 ± 5.10 | 17.80 ± 5.08 | 18.63 ± 5.32 | <0.001 |
| Sedentary time, mean ± SD | 5.11 ± 2.78 | 5.12 ± 2.75 | 4.98 ± 3.10 | 0.018 |
| Parameter | Eligible T2D Patients (n = 1981) | p | New-Onset T2D Patients (n = 1630) | p | ||
|---|---|---|---|---|---|---|
| 2013 | 2017 | 2013 | 2017 | |||
| Health behaviors | ||||||
| Quit smoking, n (%) | 106 (5.35) | 143 (7.22) | <0.001 | 63 (3.87) | 95 (5.83) | <0.001 |
| Sufficient exercise, n (%) | 1337 (67.49) | 1430 (72.19) | <0.001 | 1064 (65.28) | 1151 (70.61) | <0.001 |
| Sufficient cereal and potato intake, n (%) | 1094 (55.22) | 1116 (56.34) | 0.071 | 852 (52.27) | 875 (53.68) | 0.048 |
| Sufficient fish, eggs, poultry, and livestock meat intake, n (%) | 929 (46.90) | 965 (48.71) | 0.005 | 757 (46.44) | 793 (48.65) | 0.002 |
| Sufficient milk and dairy intake, n (%) | 272 (13.73) | 271 (13.68) | 0.904 | 236 (14.48) | 235 (14.42) | 0.898 |
| Sufficient soybeans and nuts intake, n (%) | 594 (29.98) | 998 (50.38) | <0.001 | 467 (28.65) | 786 (48.22) | <0.001 |
| Sufficient vegetables intake, n (%) | 411 (20.75) | 442 (22.31) | <0.001 | 304 (18.65) | 329 (20.18) | 0.002 |
| Sufficient fruits intake, n (%) | 203 (10.25) | 220 (11.11) | 0.024 | 170 (10.43) | 190 (11.66) | 0.006 |
| Times of drinking per week, mean ± SD | 0.96 ± 2.05 | 1.00 ± 2.11 | 0.533 | 0.50 ± 1.53 | 0.50 ± 1.46 | 0.932 |
| Sleep and psychological condition | ||||||
| Quality of sleep, n (%) | 0.140 | 0.090 | ||||
| Very good | 410 (20.73) | 346 (17.50) | 349 (21.44) | 290 (17.82) | ||
| Fair | 1082 (54.66) | 1098 (55.45) | 883 (54.17) | 897 (55.06) | ||
| Not good | 373 (18.84) | 428 (21.65) | 300 (18.42) | 350 (21.52) | ||
| Very bad | 114 (5.77) | 106 (5.40) | 97 (5.97) | 91.28 (5.60) | ||
| Sleeping time, mean ± SD | 7.13 ± 1.33 | 7.07 ± 1.25 | 1.162 | 7.15 ± 1.34 | 7.09 ± 1.25 | 0.209 |
| Psychological score, mean ± SD | 18.72 ± 5.31 | 18.69 ± 5.19 | 0.833 | 18.80 ± 5.29 | 18.8 ± 5.16 | 0.993 |
| Factors |
Well Controlled (n = 397) |
Poorly Controlled (n = 1233) | p |
|---|---|---|---|
| Age (years), mean ± SD | 37.97 ± 7.84 | 37.91 ± 8.45 | 0.890 |
| Gender, n (%) | 0.003 | ||
| Male | 245 (22.17) | 860 (77.83) | |
| Female | 152 (28.95) | 373 (71.05) | |
| Family history of diabetes (father), n (%) | 0.535 | ||
| Yes | 30 (27.79) | 82 (72.21) | |
| No | 367 (24.18) | 1151 (75.82) | |
| Family history of diabetes (mother), n (%) | 0.447 | ||
| Yes | 18 (20.93) | 68 (79.07) | |
| No | 379 (24.55) | 1165 (75.45) | |
| Changes in behavioral factors according to the guidance of health management, n (%) | |||
| Smoking | 0.002 | ||
| Yes | 270 (26.95) | 732 (73.05) | |
| No | 127 (20.22) | 501 (79.78) | |
| Drinking | 0.964 | ||
| Yes | 250 (24.32) | 778 (75.68) | |
| No | 147 (24.42) | 455 (75.58) | |
| Cereals and potato intake | 0.231 | ||
| Yes | 167 (25.93) | 477 (74.07) | |
| No | 230 (23.33) | 756 (76.67) | |
| Fish, eggs, poultry, and livestock meat intake | 0.001 | ||
| Yes | 169 (28.89) | 416 (71.11) | |
| No | 228 (21.82) | 817 (78.18) | |
| Milk and dairy products intake | 0.731 | ||
| Yes | 84 (25.07) | 251 (74.93) | |
| No | 313 (24.17) | 982 (75.83) | |
| Soybeans and nuts intake | <0.001 | ||
| Yes | 216 (28.99) | 529 (71.01) | |
| No | 181 (20.45) | 704 (79.55) | |
| Vegetables intake | 0.019 | ||
| Yes | 103 (29.10) | 251 (70.90) | |
| No | 294 (23.04) | 982 (76.96) | |
| Fruits intake | <0.001 | ||
| Yes | 101 (37.69) | 167 (62.31) | |
| No | 296 (21.73) | 1066 (78.27) | |
| Physical activity | 0.037 | ||
| Yes | 242 (26.30) | 678 (73.70) | |
| No | 155 (21.83) | 555 (78.17) | |
| Sedentary time | <0.001 | ||
| Yes | 63 (37.06) | 107 (62.94) | |
| No | 334 (22.88) | 1126 (77.12) | |
| Sleeping time | 0.698 | ||
| Yes | 253 (24.05) | 799 (75.95) | |
| No | 144 (24.91) | 434 (75.09) | |
| Sleeping quality | 0.790 | ||
| Yes | 89 (23.67) | 287 (76.33) | |
| No | 308 (24.56) | 946 (75.44) | |
| Psychological state | 0.022 | ||
| Yes | 89 (29.47) | 213 (70.53) | |
| No | 308 (23.19) | 1020 (76.81) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Y.; Hu, Q.; Chen, B.; Dai, L.; Chang, C.; Ma, D. Influence of Internet-Based Health Management on Control of Blood Glucose in Patients with Type 2 Diabetes: A Four-Year Longitudinal Study. Healthcare 2025, 13, 553. https://doi.org/10.3390/healthcare13050553
Wang Y, Hu Q, Chen B, Dai L, Chang C, Ma D. Influence of Internet-Based Health Management on Control of Blood Glucose in Patients with Type 2 Diabetes: A Four-Year Longitudinal Study. Healthcare. 2025; 13(5):553. https://doi.org/10.3390/healthcare13050553
Chicago/Turabian StyleWang, Yuyang, Qiang Hu, Botian Chen, Lingfeng Dai, Chun Chang, and Defu Ma. 2025. "Influence of Internet-Based Health Management on Control of Blood Glucose in Patients with Type 2 Diabetes: A Four-Year Longitudinal Study" Healthcare 13, no. 5: 553. https://doi.org/10.3390/healthcare13050553
APA StyleWang, Y., Hu, Q., Chen, B., Dai, L., Chang, C., & Ma, D. (2025). Influence of Internet-Based Health Management on Control of Blood Glucose in Patients with Type 2 Diabetes: A Four-Year Longitudinal Study. Healthcare, 13(5), 553. https://doi.org/10.3390/healthcare13050553









