Environment Disaster: A Cross-Sectional Study of the Determinants for the Preparation of Azorean Nurses
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Population and Sample
2.3. Instrument
- Post-disaster management: 21 items assessing how nurses perceive their ability to manage activities after a disaster.
- Competencies: 11 items focusing on the skills needed to act effectively in disaster scenarios.
- Knowledge: 13 items measuring nurses’ theoretical and practical understanding of disasters.
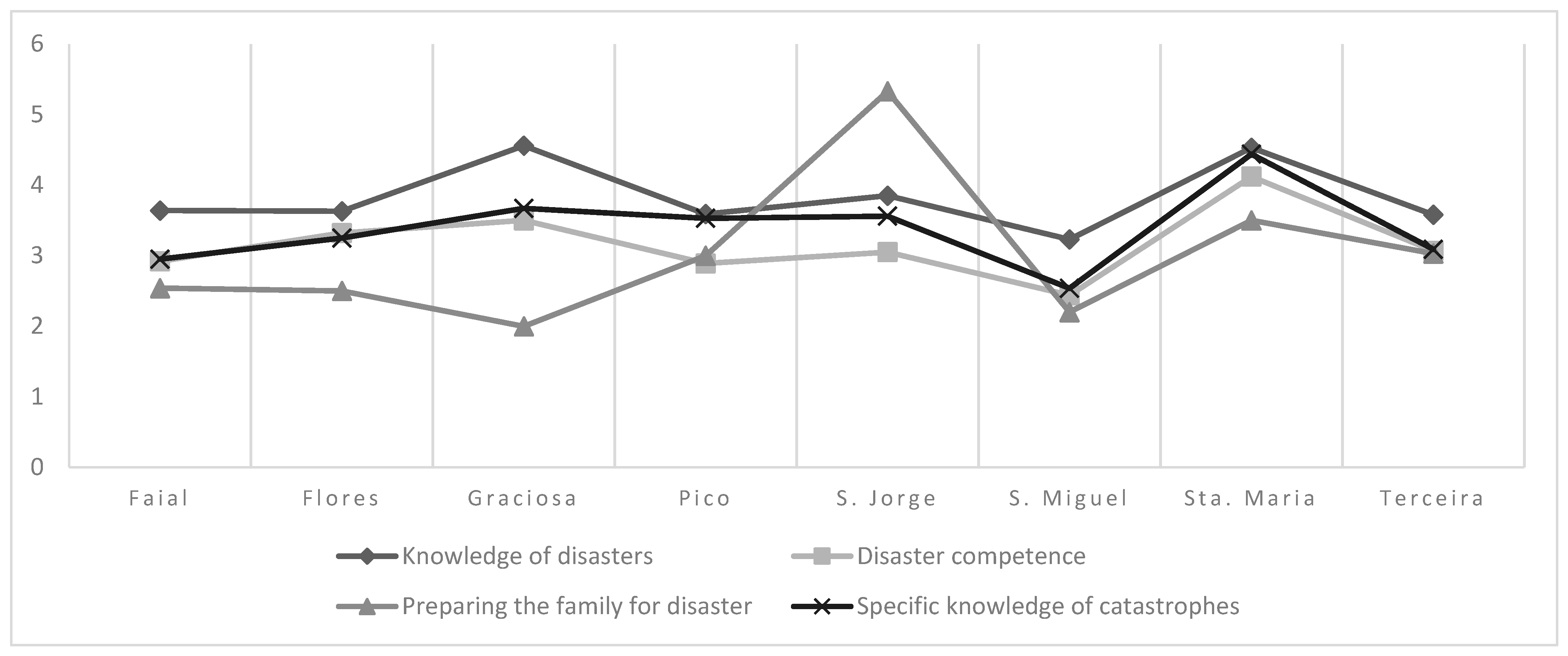
- Knowledge of disasters;
- Competence in disasters;
- Preparing the family for disasters;
- Specific knowledge of disasters;
- Patient management during disaster response;
- Knowledge about recovery;
- Recovery management.
2.4. Statistical Analysis
3. Results
3.1. Characterization of the Sample
3.2. Descriptive Analysis of the Disaster Preparedness Level (DPL) of Nurses in the Azores (N = 230)
3.3. Inferential Analysis (Hypothesis Testing)
3.4. Differences Between Professional Categories
3.5. Differences Between Professional Roles
3.6. Differences Between the Islands
3.7. Differences Between Islands with and Without a Hospital
3.8. Factors That Can Contribute to the Difference Between Islands with a Hospital and Islands Without a Hospital
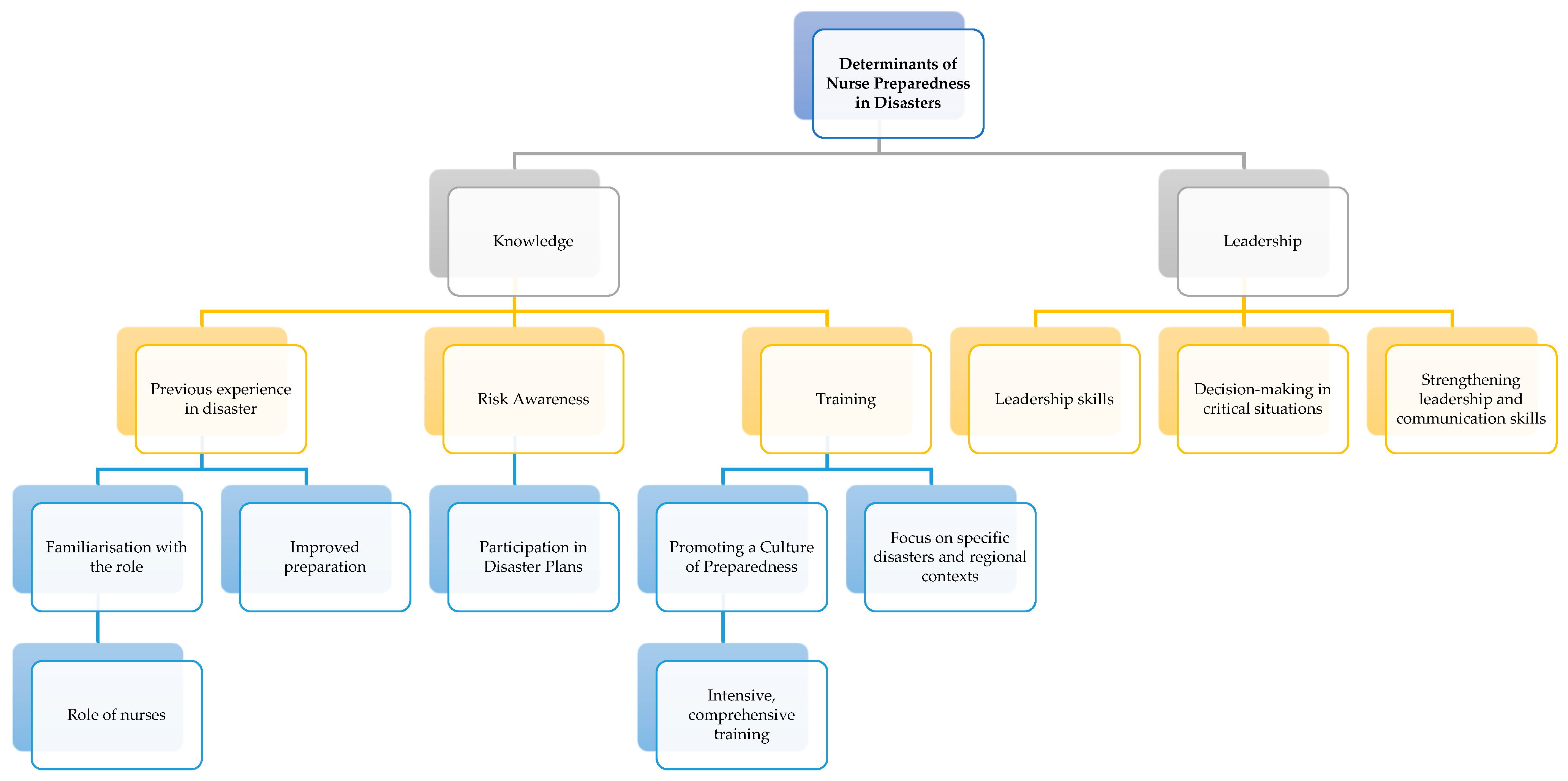
- Developing Resilience: The lack of a hospital in the community can promote greater awareness of the need to prepare themselves, their families, and the community to face disasters. Nurses working in environments without hospitals tend to develop high levels of resilience, creating adaptability and the ability to self-manage in challenging situations. The research by [22] highlights that nurses can develop resilience to cope with clinical pressures and demands in extreme conditions through emotional adaptation and innovation in care.
- Innovative Capacities: The absence of hospitals forces nurses to develop innovative practices in crisis care. They need to deal with the situation creatively and effectively to respond to the needs of the victim, family, and community [22].
- Importance of Planning: The literature emphasizes that planning and preparation must occur before disasters occur. This study highlights that more than half of the nurses know their unit’s disaster plan, associated with a better perception of preparedness. Awareness of the protocols and participation in training programs on disasters are essential factors that contribute to the adequate preparation of nurses [23].
3.9. Differences Between Specialties (Nursing Specialization Area)
3.10. The Role of Experience and Training
3.11. Effect of Length of Experience
4. Discussion
4.1. Determinants of Disaster Preparedness
4.2. Disaster Advanced Nursing
4.3. Implications and Limitations of This Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Secretaria Regional do Ambiente e Ação Climática, Direção Regional do Ambiente e Ação Climática. Relatório do Estado do Ambiente dos Açores 2020–2022; Secretaria Regional do Ambiente e Ação Climática, Direção Regional do Ambiente e Ação Climática: Ponta Delgada, Portugal, 2020. [Google Scholar]
- ICN. Core Competencies in Disaster Nursingversion 2.0; International Council of Nurses: Geneva, Switzerland, 2019; pp. 1–14. [Google Scholar]
- Fletcher, K.A.; Reddin, K.; Tait, D. The history of disaster nursing: From Nightingale to nursing in the 21st century. J. Res. Nurs. 2022, 27, 257–272. [Google Scholar] [CrossRef] [PubMed]
- Ziapour, A.; Darabi, F.; Rostami, F.; Motevaseli, S.; Sharma, M.; Chaboksavar, F.; Yildirim, M.; Kianipour, N. Investigating perceived core disaster competencies of nurses in Iran: A case study of northwest hospitals. Public Health Nurs. 2024, 41, 970–978. [Google Scholar] [CrossRef]
- Santos, P.A.F.d.; Rabiais, I.C.M.; Frade, J.M.; Coutinho, V.R.D.; Baptista, R.C.N. General nurse competencies in disaster: A delphi study. Nurse Educ. Pract. 2024, 79, 104037. [Google Scholar] [CrossRef]
- Labrague, L.J.; Hammad, K. Disaster preparedness among nurses in disaster-prone countries: A systematic review. Australas. Emerg. Care 2024, 27, 88–96. [Google Scholar] [CrossRef]
- Setyawati, A.D.; Lu, Y.Y.; Liu, C.Y.; Liang, S.Y. Disaster knowledge, skills, and preparedness among nurses in Bengkulu, Indonesia: A descriptive correlational survey study. J. Emerg. Nurs. 2021, 46, 633–641. [Google Scholar] [CrossRef]
- Tichy, M.; Bond, A.E.; Beckstrand, R.L.; Heise, B. Ps’ Perceptions of Disaster Preparedness Education: NPs’ Perceptions of Disaster Preparedness Education: Quantitative Survey Research. Am. J. Nurse Pract. 2009, 13, 10–22. [Google Scholar]
- Al Khalaileh, M.A.; Bond, A.E.; Beckstrand, R.L.; Al-Talafha, A. The Disaster Preparedness Evaluation Tool: Psychometric testing of the Classical Arabic version. J. Adv. Nurs. 2010, 66, 664672. [Google Scholar] [CrossRef]
- Thobaity, A.A.; Plummer, V.; Innes, K.; Copnell, B. Perceptions of knowledge of disaster management among military and civilian nurses in Saudi Arabia. Australas. Emerg. Nurs. J. 2015, 18, 156–164. [Google Scholar] [CrossRef] [PubMed]
- Younos, T.B.; Hasan, M.K.; Nasreen, M. Are nurses ready? Bangladeshi nurses’ perceived preparedness for disasters: A mixed-methods approach. Int. J. Disaster Risk Reduct. 2021, 58, 102195. [Google Scholar] [CrossRef]
- Aqtam, I.; Shouli, M.; Al-qoroum, S.; Shouli, K.; Ayed, A. Evaluating Disaster Management Preparedness among Healthcare Professionals During Pandemics: Palestinian Context. SAGE Open Nurs. 2024, 10, 1–9. [Google Scholar] [CrossRef]
- Usher, K.; Mills, J.; West, C.; Casella, E.; Dorji, P.; Guo, A.; Koy, V.; Pego, G.; Phanpaseuth, S.; Phouthavong, O.; et al. Cross-sectional survey of the disaster preparedness of nurses across the Asia–Pacific region. Nurs. Health Sci. 2015, 17, 434–443. [Google Scholar] [CrossRef] [PubMed]
- Oztekin, S.D.; Larson, E.E.; Akahoshi, M.; Oztekin, I. Japanese nurses’ perception of their preparedness for disasters: Quantitative survey research on one prefecture in Japan. Jpn. J. Nurs. Sci. 2016, 13, 391–401. [Google Scholar] [CrossRef] [PubMed]
- Rizqillaha, A.F.; Sunaa, J. Indonesian emergency nurses’ preparedness to respond to disaster: A descriptive survey. Australas. Emerg. Care 2018, 21, 64–68. [Google Scholar] [CrossRef]
- Han, S.J.; Chun, J. Validation of the Disaster Preparedness Evaluation Tool for Nurses—The Korean Version. Int. J. Environ. Res. Public Health 2021, 18, 1348. [Google Scholar] [CrossRef]
- Hasan, K.; Younos, T.B.; Farid, Z.I. Nurses’ knowledge, skills and preparedness for disaster management of a Megapolis: Implications for nursing disaster education. Nurse Educ. Today 2021, 107, 105–122. [Google Scholar] [CrossRef]
- Wang, J.; Sun, X.; Lu, S.; Wang, F.; Wan, M.; Chen, H.; Tan, Y. Disaster Preparedness and Associated Factors Among Emergency Nurses in Guangdong Province, China: A Descriptive Cross-Sectional Study; Disaster Medicine and Public Health Preparedness: Cambridge, UK, 2021. [Google Scholar]
- Santos, C.R.; Dixe, M.d.A.C.R. VALIDAÇÃO CULTURAL DO “DISASTER PREPAREDNESS EVALUATION TOOL (DPET©)”– PREPARAÇÃO DOS ENFERMEIROS PERANTE UMA SITUAÇÃO DE CATÁSTROFE. M. Dixe; P. Sousa & P. Gaspar (Coords.), Construindo Conhecimento em Enfermagem à Pessoa em Situação Crítica: Instituto Politécnico de Leiria, Unidade de Investigação em Saúde, Escola Superior de Saúde de Leiria; 2017. Available online: https://iconline.ipleiria.pt/bitstream/10400.8/2881/1/cap-4.pdf (accessed on 28 January 2025).
- Marôco, J. Análise Estatística Com o SPSS Statistics 5ª ed2011; SPSS, Inc.: Chicago, IL, USA, 2011. [Google Scholar]
- Hair, J.F.; Black, W.C.; Anderson, R.E. Multivariate Data Analysis 8ª; Cengage Learning EMEA: London, UK, 2019. [Google Scholar]
- Xue, C.-L.; Shu, Y.-S.; Hayter, M.; Lee, A. Experiences of nurses involved in natural disaster relief: A meta-synthesis of qualitative literature. J. Clin. Nurs. 2020, 29, 4514–4531. [Google Scholar] [CrossRef] [PubMed]
- Koçak, H.S.; Serin, E.K. Are Nurses Ready for a Disaster in Turkey? A Hospital Case. Disaster Med. Public Health Prep. 2023, 17, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Mamalova, K.; Galazova, Z.; Gafarov, E. Climate agenda: The role of international agreements in combating global warming. Reliab. Theory Appl. 2024, 19, 669–677. [Google Scholar]
- Harris, O.O.; Bialous, S.A.; Muench, U.; Chapman, S.; Dawson-Rose, C. Climate Change, Public Health, Health Policy, and Nurses Training. Am. J. Public Health 2022, 112, S321. [Google Scholar] [CrossRef]
- Baack, S.; Alfred, D. Nurses’ preparedness and perceived competence in managing disasters. J. Nurs. Scholarsh. 2013, 45, 281–287. [Google Scholar] [CrossRef]
- Alzahrani, F.; Kyratsis, Y. Emergency nurse disaster preparedness during mass gatherings: A cross-sectional survey of emergency nurses’ perceptions in hospitals in Mecca, Saudi Arabia. BMJ Open 2017, 7, e013563. [Google Scholar] [CrossRef] [PubMed]
- Brewer, C.A.; Hutton, A.; Hammad, K.S.; Geale, S.K. A feasibility study on disaster preparedness in regional and rural emergency departments in New South Wales: Nurses self-assessment of knowledge, skills and preparation for disaster management. Australas. Emerg. Care 2020, 23, 29–36. [Google Scholar] [CrossRef]
- Hossain, B.; Shi, G.; Ajiang, C.; Sarker, M.N.I.; Sohel, M.S.; Sun, Z.; Hamza, A. Impact of climate change on human health: Evidence from riverine island dwellers of Bangladesh. Int. J. Environ. Health Res. 2022, 32, 2359–2375. [Google Scholar] [CrossRef]
- Hassan, S.; Philippe, C.; West, R.M.; McFarlane, S.; Polson-Edwards, K.; Gordon-Strachan, G.; Hospedales, C.J.; Dubrow, R.; Allen, C.F. Development of an agenda for research and action on climate change and health in the Caribbean. Panam. Salud Publica 2025, 49, e4. [Google Scholar] [CrossRef]
- Anderson, G.B.; Schumacher, A.; Done, J.M.; Hurrell, J.W. Projecting the Impacts of a Changing Climate: Tropical Cyclones and Flooding. Curr. Environ. Health Rep. 2022, 9, 244–262. [Google Scholar] [CrossRef] [PubMed]
- Kassaw, G.M.; Malede, A.; Gebrehiwot, M. Livelihood vulnerability to climate change health impacts among Amhara Sayint district community, northeastern Ethiopia: A composite index approach. Heliyon 2024, 10, e38166. [Google Scholar] [CrossRef]
- AlOtaibi, S.S.; Almutairi, H.A.; Alotaibi, M.K.; Alharbi, K.; Bahari, G. Enhancing Nurses’ Disaster Management and Preparedness: Evaluating the Effectiveness of an Online Educational Program Through a QuasiExperimental Study. Risk Manag. Healthc. Policy 2024, 17, 101–111. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.; Wen, G.; Gu, C.; Ma, C.; Chen, H.; Xiang, J. The core competencies in disaster nursing of new graduate nurses in Guangdong, China: A cross-sectional study. Nurse Educ. Pract. 2024, 77, 103987. [Google Scholar] [CrossRef] [PubMed]
- Chisholm, L.J.; Hale, R.L.; Knight, S.L. Community Resilience After Hurricanes: Can Neuman’s Systems Theory Guide Public Health Nursing? Res. Theory Nurs. Pract. 2023, 37, 84–100. [Google Scholar] [CrossRef]
- Olímpio, J.d.A.; Araújo, J.N.d.M.; Pitombeira, D.O.; Enders, B.C.; Sonenberg, A.; Vitor1, A.F. Advanced practice nursing: A concept analysis. Acta Paul. Enferm. 2018, 31, 674–680. [Google Scholar] [CrossRef]

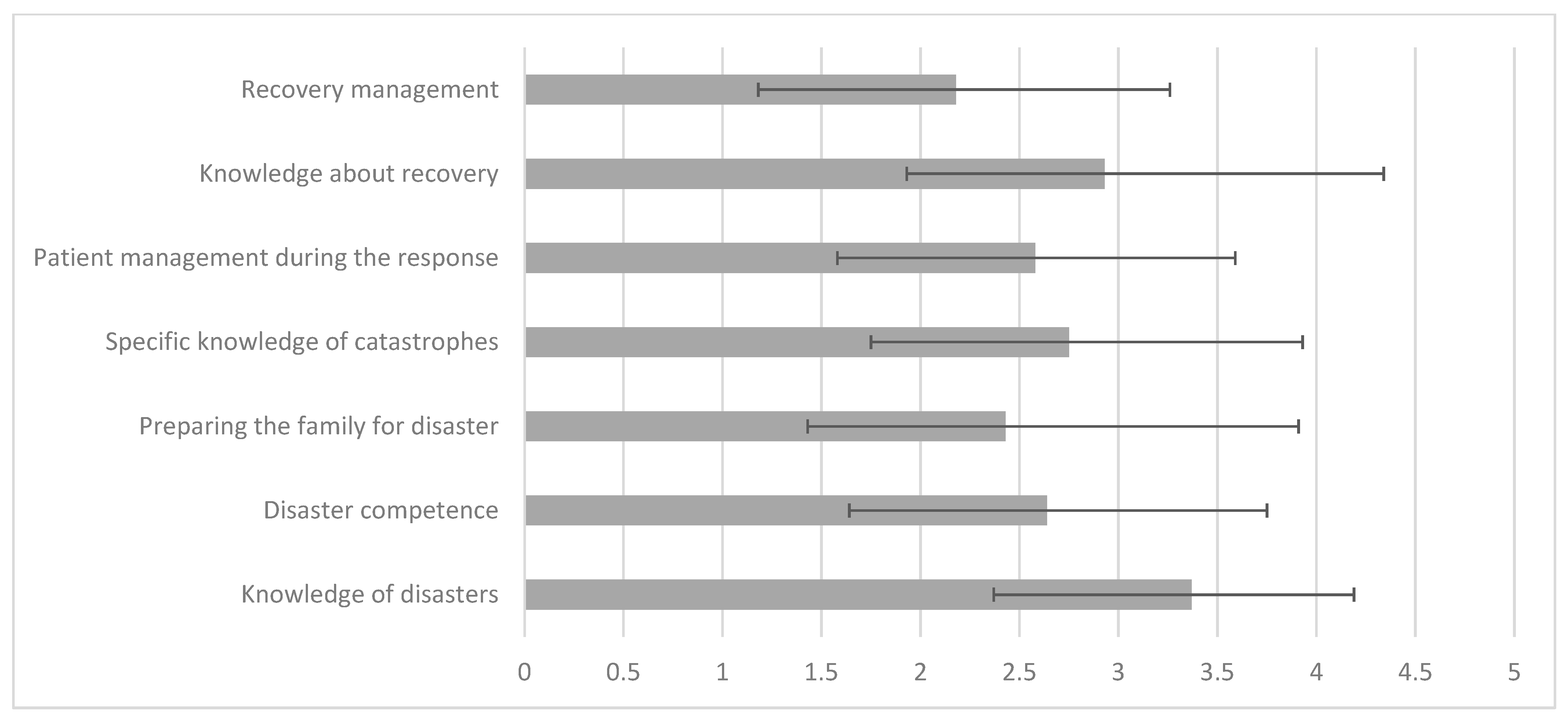
| Island with Hospital | n | Average | Standard Deviation | t (gl) p-Value | |
|---|---|---|---|---|---|
| Knowledge of disasters | No | 20 | 4.02 | 0.91 | t (228) = 3.771 p-value = 0.000 |
| Yes | 210 | 3.31 | 0.79 | ||
| Disaster competence | No | 20 | 3.43 | 0.92 | t (228) = 3.390 p-value = 0.001 |
| Yes | 210 | 2.57 | 1.10 | ||
| Preparing the family for disaster | No | 20 | 3.30 | 1.94 | t (20,95) = 2.147 p-value = 0.044 |
| Yes | 210 | 2.35 | 1.40 | ||
| Specific knowledge of catastrophes | No | 20 | 3.77 | 1.25 | t (228) = 4.174 p-value = 0.000 |
| Yes | 210 | 2.65 | 1.13 | ||
| Patient management during the response | No | 20 | 3.21 | 0.94 | t (228) = 2.969 p-value = 0.003 |
| Yes | 210 | 2.52 | 1.00 | ||
| Knowledge about recovery | No | 20 | 3.80 | 1.28 | t (228) = 2.948 p-value = 0.004 |
| Yes | 210 | 2.84 | 1.40 | ||
| Recovery management | No | 20 | 2.86 | 1.19 | t (228) = 2.983 p-value = 0.003 |
| Yes | 210 | 2.12 | 1.05 |
| Average | DP | Years of Professional Experience | Years of Professional Experience in the Current Unit | |
|---|---|---|---|---|
| Knowledge of disasters | 3.37 | 0.82 | 0.076 | 0.085 |
| Disaster competence | 2.64 | 1.11 | −0.043 | −0.017 |
| Preparing the family for disaster | 2.43 | 1.48 | 0.146 * | 0.133 * |
| Specific knowledge of catastrophes | 2.75 | 1.18 | −0.082 | −0.042 |
| Patient management during the response | 2.58 | 1.01 | −0.036 | 0.020 |
| Knowledge about recovery | 2.93 | 1.41 | −0.040 | −0.011 |
| Recovery management | 2.18 | 1.08 | −0.007 | 0.005 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pires, E.G.; Nogueira, P.; Henriques, M.A.; Arriaga, M.; Costa, A.S. Environment Disaster: A Cross-Sectional Study of the Determinants for the Preparation of Azorean Nurses. Healthcare 2025, 13, 303. https://doi.org/10.3390/healthcare13030303
Pires EG, Nogueira P, Henriques MA, Arriaga M, Costa AS. Environment Disaster: A Cross-Sectional Study of the Determinants for the Preparation of Azorean Nurses. Healthcare. 2025; 13(3):303. https://doi.org/10.3390/healthcare13030303
Chicago/Turabian StylePires, Eunice Gatinho, Paulo Nogueira, Maria Adriana Henriques, Miguel Arriaga, and Andreia Silva Costa. 2025. "Environment Disaster: A Cross-Sectional Study of the Determinants for the Preparation of Azorean Nurses" Healthcare 13, no. 3: 303. https://doi.org/10.3390/healthcare13030303
APA StylePires, E. G., Nogueira, P., Henriques, M. A., Arriaga, M., & Costa, A. S. (2025). Environment Disaster: A Cross-Sectional Study of the Determinants for the Preparation of Azorean Nurses. Healthcare, 13(3), 303. https://doi.org/10.3390/healthcare13030303










