Competency Profile for Primary Health Care Managers in Chile: Mixed-Methods Validation Through Expert Judgment
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
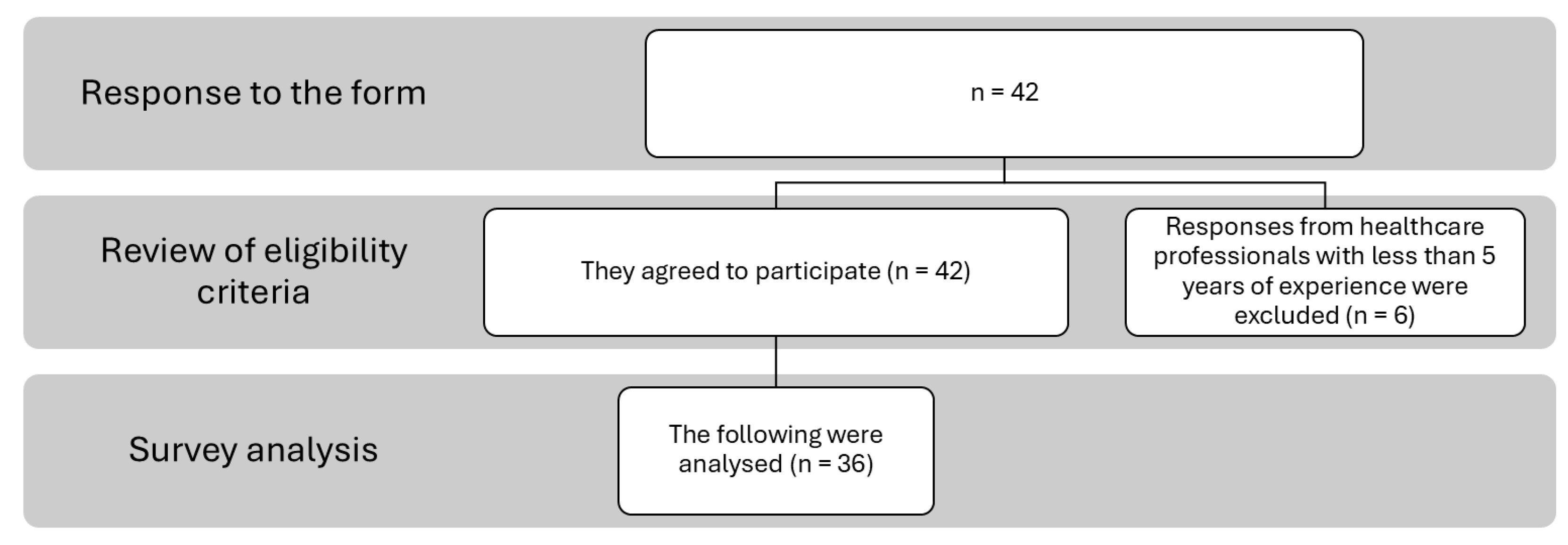
2.2. Participants
- –
- Professionals who are currently serving as PHC directors for at least two years or who have held this position within the past five years.
- –
- Professionals currently working in PHC roles, with a minimum of five years’ experience.
- –
- Academics or researchers whose teaching or publications focused on PHC.
Instruments
2.3. Procedure
2.4. Data Analysis
2.5. Ethical Considerations
3. Results
3.1. Participants
3.2. Descriptive Analysis and Normality
3.3. Content Validity
3.4. Qualitative Analysis
3.4.1. Knowledge
3.4.2. Skills
3.4.3. Attitudes
4. Discussion
Limitations and Future Lines of Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Knowledge | Skills | Attitudes |
|---|---|---|
| Initial competencies | ||
| Previous in health/PHC | Leadership | Autonomy |
| Healthcare network | Teamwork | Resilience |
| Health administration and management | Crisis management | Neutrality |
| Management and use of indicators | Institutional alignment | Coping skills |
| Health personnel management | Strategic vision | Creativity |
| Workflows and processes | Effective communication | Motivation |
| Planning, monitoring and evaluation | Flexibility | |
| Recognising skills in others | Professionalism | |
| Conflict management | Proactivity | |
| Negotiation | Empathy | |
| Delegation | Professional self-realisation | |
| Decision-making | Acting ethically and responsibly | |
| Articulation skills | Self-criticism | |
| Change management | Initiative | |
| Persuasion | ||
| Relationship building | ||
| Analytical thinking | ||
| Innovative thinking | ||
| Performance evaluation | ||
| Team building | ||
| Added competencies | ||
| Regulatory and legislative framework for PHC | Institutional support | Positive and proactive attitude |
| Quality management and accreditation | Team well-being management | Territorial management |
| Emotional Intelligence | ||
Appendix B
Appendix B.1. Knowledge
- Previous in health/PHC: Understanding of the principles, structures, and practices related to health promotion, prevention, and comprehensive care at the community and family levels.
- Healthcare network: In-depth understanding of how the health system operates and how the different levels of care (primary, secondary, tertiary) are integrated, as well as the processes that ensure continuity and efficiency in patient care.
- Health administration and management: Understanding principles and practices for organizing, directing, and coordinating human, financial, technological, and material resources within the health system to ensure effective and efficient service delivery.
- Management and use of indicators: Ability to identify, analyse, and apply key metrics to assess service performance, quality of care, and population health outcomes.
- Health personnel management: Competencies required to effectively manage human resources in the health sector, particularly in PHC, ensuring that teams operate efficiently and in line with strategic objectives.
- Workflows and processes: Understanding and ability to manage, design, and optimize the sequence of activities and operations within a health organization or system, with a focus on PHC.
- Regulatory and legislative framework for PHC: Ability to understand, interpret, and apply the laws, policies, and regulations governing Primary Health Care.
- Quality management and accreditation: Conceptual and practical understanding of principles, tools, and processes associated with continuous quality improvement in health services.
Appendix B.2. Skills
- Leadership: Ability to influence, motivate, and guide others toward shared goals—not limited to formal authority, but also including positive influence and inspiring commitment.
- Teamwork: Capacity to collaborate effectively with individuals of diverse skills and backgrounds, coordinating efforts and responsibilities to achieve common goals.
- Crisis management: Set of actions and strategies to anticipate, address, and resolve critical situations that may endanger an organisation or system, requiring rapid and effective responses.
- Institutional alignment: The extent to which an organization’s goals, strategies, values, and actions are aligned, ensuring coherence across departments and personnel.
- Strategic vision: Ability to anticipate and plan by identifying long-term objectives, emerging trends, and necessary changes, guiding present actions toward sustainable success.
- Effective communication: Skill to convey messages clearly and accurately, ensuring mutual understanding and facilitating agreements and actions—includes verbal and non-verbal communication.
- Planning, monitoring, and evaluation: Ability to define objectives, set goals and deadlines, assign tasks, monitor progress, and evaluate outcomes to ensure successful implementation.
- Recognising skills in others: Ability to identify and value the strengths and talents of others, assigning responsibilities or guiding development accordingly.
- Conflict management: Skill to identify, address, and resolve disputes constructively, understanding root causes and maintaining relationships while promoting performance.
- Negotiation: Process through which parties with shared or conflicting interests reach mutually beneficial agreements. It is key to problem-solving and achieving organisational goals.
- Delegation: Ability to assign responsibilities to others effectively, granting the necessary authority and resources while maintaining adequate supervision.
- Decision-making: Capacity to choose the best course of action among alternatives by weighing risks, benefits, and consequences in the short and long term.
- Coordination skills: Ability to integrate and align different services, care levels, stakeholders, and resources to ensure comprehensive, continuous, and accessible care.
- Change management: Skill to lead and support organisational transitions, addressing resistance, maintaining motivation, and achieving desired outcomes with minimal negative impact.
- Persuasion: Ability to influence ideas or behaviours through logical argumentation and emotional connection, building trust and credibility.
- Relationship building: Ability to establish and maintain positive, productive relationships with colleagues, supervisors, clients, and other stakeholders.
- Analytical thinking: Ability to break down complex issues into components, evaluate information, and draw logical conclusions using critical and systematic reasoning.
- Innovative thinking: Ability to generate new ideas and approaches, challenge conventional thinking, and propose creative solutions that add value.
- Performance evaluation: Ability to assess individual or team performance objectively, based on clear criteria, and provide constructive feedback for improvement.
- Team building: Ability to select, organize, and motivate team members to work collaboratively and efficiently toward common objectives.
- Emotional intelligence: Ability to recognize, understand, and manage one’s own emotions and those of others, fostering effective relationships and a healthy work environment.
- Institutional support: The managers’ role in backing their team during pressure or conflict, especially when staff act according to regulations.
- Team well-being management: Ability to promote healthy work conditions, detect signs of stress or burnout, and implement preventive strategies to maintain team well-being.
Appendix B.3. Attitudes
- Autonomy: Willingness to make decisions and act independently, with self-regulation and responsibility in fulfilling tasks.
- Resilience: Ability to adapt to and recover from adversity, learning and growing from challenges without lasting harm.
- Neutrality: Attitude of impartiality in conflict resolution and decision-making, relying on facts and avoiding personal bias.
- Coping skills: Proactive and effective approach to dealing with challenges, maintaining emotional control and seeking constructive solutions.
- Creativity: Disposition to generate new ideas and approaches to improve processes and decision-making.
- Motivation: Internal drive to pursue goals and achieve fulfilment, influencing engagement and persistence at work.
- Flexibility: Readiness to adapt to changes or new demands with agility and effectiveness.
- Professionalism: Commitment to ethical, respectful, and responsible behaviour, aligned with the expectations of the professional role.
- Proactivity: Tendency to anticipate situations, take initiative, and seek improvement without waiting for instructions.
- Empathy: Active disposition to understand and connect with others’ feelings and perspectives, showing genuine interest and sensitivity.
- Professional self-realisation: Commitment to personal growth, striving for satisfaction and meaning in work through development and purpose.
- Acting ethically and responsibly: Commitment to integrity, justice, and community welfare, with awareness of the impact of one’s actions.
- Self-criticism: Willingness to evaluate oneself honestly, acknowledging strengths and areas for improvement to foster continuous learning.
- Initiative: Internal drive to act independently, recognize opportunities, and take responsibility without external prompting.
- Positive and proactive attitude: Orientation toward continuous improvement, problem-solving, and constructive engagement.
- Territorial management: Ability to act with awareness of the political and social context of the local territory, aligning institutional management with local realities and PHC strategies.
Appendix C
| Decision | Competence (Final) | Expert Statements (Verbatim, Translated) |
|---|---|---|
| Not added | — | “No” (33.33%, 12 of 36 responses) |
| Reorganized | Previous in health/PHC | “Knowledge of the Family Health Model and Quality and Safety of health care”; “Having knowledge of newly implemented strategies such as ECICEP”; “Health information systems or digital platforms”; “experience and cross-cutting knowledge of programs”; “Social determinants”; “Knowledge of the municipal role in PHC”; “Knowing all the possible programs that can be carried out in PHC in order to expand the portfolio of services of the facility (e.g., Vida Sana, Más AMA, Friendly Spaces, etc.)”; “Family Medicine and knowledge of the family and community health model. Health information systems or digital platforms. In terms of service delivery, some level of knowledge in chronic disease management and, in my opinion, it would be desirable to have basic training in the management of institutions for older adults.” |
| Added | Regulatory and legislative framework for PHC | “Knowledge of Laws 19,378, 18,883, 21,188, 21,643, 16,744, 20,545, 20,609, the Labor Code, the local regulation of the civil service career and the internal regulations”; “health legislative framework” |
| Added | Quality management and accreditation | “Knowledge in quality management and accreditation”; “Knowledge about public bidding processes”; “Knowledge of the PHC accreditation system”; “Knowledge of quality and accreditation” |
| Reallocated → Skills | Planning, monitoring and evaluation/Effective communication | “Health planning and programming, and strategic management of health information and communication” |
| Reallocated → Skills | Leadership | “Competencies and knowledge in organizational leadership” |
| Reallocated → Attitudes | Professionalism | “A manager must guarantee the delivery of a comprehensive, quality, and timely health service” |
| Decision | Competence (Final) | Expert statements (Verbatim, Translated) |
|---|---|---|
| Not added | — | “No” (63.89%, 23 of 36 responses) |
| Reorganized | Existing categories (Effective communication, empathy, self-criticism, conflict management) | “Soft skills such as empathy, emotional intelligence, resilience, tolerance to stress and frustration, among others”; “Active and empathetic listening” |
| Added | Emotional intelligence | “Soft skills such as empathy, emotional intelligence, resilience, tolerance to stress and frustration, among others” |
| Added | Institutional support | “Empathy to understand the difficulties people face and the problems they encounter, since many times their work or conflicts are minimized, especially frontline staff dealing with demanding users. I don’t know how to call the skill of backing up staff when they give a correct instruction to a user and the user does not accept it (to prevent the staff member from feeling unprotected, without support).” |
| Added | Team well-being management | “Promoting good practices, knowledge and skill in caring for the mental health of health workers, prevention of burnout, flexibility in decision-making.” |
| Decision | Competence (Final) | Expert Statements (Verbatim, Translated) |
|---|---|---|
| Not added | — | “No” (72.22%, 26 of 36 responses) |
| Refined | Neutrality | “Fairness in the treatment of staff” |
| Refined | Self-criticism | “Being consistent, humility in recognizing when they have been wrong” |
| Not added | — | “Public service vocation does not constitute an observable skill…” |
| Added | Positive and proactive attitude | “Positivism”; “Positive and proactive attitude” |
| Added | Territorial management | “I would add strategic territorial thinking” |
References
- Organización Panamericana de la Salud. Avances Hacia La Salud Universal En La Región de Las Américas: Abordar Las Necesidades Insatisfechas de Atención de Salud, Las Brechas En La Cobertura y La Falta de Protección Financiera Mediante La Atención Primaria de Salud; Organización Panamericana de la Salud: Washington, DC, USA, 2024; ISBN 9789275329474. [Google Scholar]
- Owens, B.P.; Hekman, D.R. How Does Leader Humility Influence Team Performance? Exploring the Mechanisms of Contagion and Collective Promotion Focus. Acad. Manag. J. 2016, 59, 1088–1111. [Google Scholar] [CrossRef]
- Montano, D.; Reeske, A.; Franke, F.; Hüffmeier, J. Leadership, Followers’ Mental Health and Job Performance in Organizations: A Comprehensive Meta-Analysis from an Occupational Health Perspective. J. Organ. Behav. 2017, 38, 327–350. [Google Scholar] [CrossRef]
- Atun, R.; de Andrade, L.O.M.; Almeida, G.; Cotlear, D.; Dmytraczenko, T.; Frenz, P.; Garcia, P.; Gómez-Dantés, O.; Knaul, F.M.; Muntaner, C.; et al. Health-System Reform and Universal Health Coverage in Latin America. Lancet 2015, 385, 1230–1247. [Google Scholar] [CrossRef]
- World Health Organization; UNICEF. A Vision for Primary Health Care in the 21st Century; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Organización Mundial de la Salud Atención Primaria de Salud. Available online: https://www.who.int/es/news-room/fact-sheets/detail/primary-health-care (accessed on 17 May 2025).
- Organization for Economic Co-operation and Development. Primary Health Care for Resilient Health Systems in Latin America; OECD: Paris, France, 2022; ISBN 9789264724877. [Google Scholar]
- Cerda, A.A.; García, L.Y.; Rivera-Arroyo, J.; Riquelme, A.; Teixeira, J.P.; Jakovljevic, M. Comparison of the Healthcare System of Chile and Brazil: Strengths, Inefficiencies, and Expenditures. Cost Eff. Resour. Alloc. 2022, 20, 71. [Google Scholar] [CrossRef]
- Giovanella, L.; de Almeida, P.F.; Vega Romero, R.; Oliveira, S.; Tejerina Silva, H. Panorama de La Atención Primaria de Salud En Suramérica: Concepciones, Componentes y Desafíos. Saúde Debate 2015, 39, 300–322. [Google Scholar] [CrossRef]
- Bernales, M.; Cabieses, B.; McIntyre, A.M.; Chepo, M. Desafíos En La Atención Sanitaria de Migrantes Internacionales En Chile. Rev. Peru. Med. Exp. Salud Publica 2017, 34, 167–175. [Google Scholar] [CrossRef]
- Abashidze-Gabaidze, G.; Khurtsia, L.; Gabaidze, M.; Loria, L. Primary Health Care as the Main Guarantor of a Healthy Population in the Country and a Global Challenge in the World: A Systematic Review. F1000Research 2024, 13, 38. [Google Scholar] [CrossRef]
- Heidemann, I.T.S.B.; Durand, M.K.; de Souza, J.B.; Arakawa-Belaunde, A.M.; Macedo, L.C.; Correa, S.M.; de Araujo, L.M.C.; Maciel, K.S. Potentialities and Challenges for Care in the Primary Health Care Context. Texto Contexto—Enferm. 2023, 32, e20220333. [Google Scholar] [CrossRef]
- Villarroel González, S.R. Health Workforce Planning: Brief Historic Route of Chilean Policies. Medwave 2016, 16, e6611. [Google Scholar] [CrossRef]
- Pesse-Sorensen, K.; Fuentes-García, A.; Ilabaca, J. Estructura y Funciones de La Atención Primaria de Salud Según El Primary Care Assessment Tool Para Prestadores En La Comuna de Conchalí—Santiago de Chile. Rev. Med. Chil. 2019, 147, 305–313. [Google Scholar] [CrossRef]
- Da Silva, L.B.; Sousa, M.H.O.; Íñiguez-Rueda, L. Managers’ Views on Professional Competencies for Primary Health Care. Sage Open 2022, 12, 215824402211382. [Google Scholar] [CrossRef]
- Puertas, E.B.; Sotelo, J.M.; Ramos, G. Liderazgo y Gestión Estratégica En Sistemas de Salud Basados En Atención Primaria de Salud. Rev. Panam. Salud Pública 2020, 44, e124. [Google Scholar] [CrossRef]
- Soto-Schulz, K.; Herrera-Echenique, R.; Brito-Díaz, R.; Pérez-Romero, N. Competencies Required for the Performance of Primary Health Care Managers: A Systematic Review. Cad. Saude Publica 2025, 41, e00092624. [Google Scholar] [CrossRef]
- Dikic, M.; Nikolic, D.; Todorovic, J.; Terzic-Supic, Z.; Kostadinovic, M.; Babic, U.; Gacevic, M.; Santric-Milicevic, M. Alignment of Perceived Competencies and Perceived Job Tasks among Primary Care Managers. Healthcare 2020, 8, 9. [Google Scholar] [CrossRef]
- Fernandes, J.C.; Cordeiro, B.C. Gerência de Unidade Básica de Saúde: Discutindo Competências Gerenciais Com o Enfermeiro Gerente. Rev. APS 2021, 22, 833–848. [Google Scholar] [CrossRef]
- André, A.M.; Ciampone, M.H.T.; Santelle, O. Tendências de Gerenciamento de Unidades de Saúde e de Pessoas. Rev. Saude Publica 2013, 47, 158–163. [Google Scholar] [CrossRef][Green Version]
- Farah, B.F.; Dutra, H.S.; Sanhudo, N.F.; Costa, L.M. Percepção de Enfermeiros Supervisores Sobre Liderança Na Atenção Primária. Rev. Cuid. 2017, 8, 1638–1655. [Google Scholar] [CrossRef]
- Mesa Oliveros, O.L.; Murillo, L.D.; Osorio Henao, F. Atención Primaria En Salud, Un Análisis Desde Los Determinantes Sociales de La Salud. Rev. Salud Pública 2021, 23, 1–2. [Google Scholar] [CrossRef]
- Sallam, M.; Stanley, A.; Snygg, J.; Jelley, D.; Sajwani, A. Empowering Healthcare Leadership Through Facilitators of Evidence-Based Management: A Narrative Review and Proposed Conceptual Framework. Front. Manag. Sci. 2025, 4, 39–63. [Google Scholar] [CrossRef]
- Anusi, H.I.; Boboye, O.; Nwankwo Ezeanyim, E.E. Review of Leadership Styles: An Exploration of Approaches Used by Hospital Administrators: A Systematic Review of Literature. Int. J. Sci. Res. Arch. 2025, 16, 123–131. [Google Scholar] [CrossRef]
- Restivo, V.; Minutolo, G.; Battaglini, A.; Carli, A.; Capraro, M.; Gaeta, M.; Odone, A.; Trucchi, C.; Favaretti, C.; Vitale, F.; et al. Leadership Effectiveness in Healthcare Settings: A Systematic Review and Meta-Analysis of Cross-Sectional and Before–After Studies. Int. J. Environ. Res. Public Health 2022, 19, 10995. [Google Scholar] [CrossRef]
- Batt, A.M.; Tavares, W.; Williams, B. The Development of Competency Frameworks in Healthcare Professions: A Scoping Review. Adv. Health Sci. Educ. 2020, 25, 913–987. [Google Scholar] [CrossRef]
- MacKay, M.; Ford, C.; Grant, L.E.; Papadopoulos, A.; McWhirter, J.E. Developing Competencies in Public Health: A Scoping Review of the Literature on Developing Competency Frameworks and Student and Workforce Development. Front. Public Health 2024, 12, 1332412. [Google Scholar] [CrossRef]
- Kakemam, E.; Liang, Z.; Janati, A.; Arab-Zozani, M.; Mohaghegh, B.; Gholizadeh, M. Leadership and Management Competencies for Hospital Managers: A Systematic Review and Best-Fit Framework Synthesis. J. Healthc. Leadersh. 2020, 12, 59–68. [Google Scholar] [CrossRef]
- Dois, A.; Bravo, P.; Contreras, A.; Soto, M.G.; Mora, I. Formación y Competencias Para Los Equipos de Atención Primaria Desde La Mirada de Expertos Chilenos. Rev. Panam. Salud Pública 2018, 42, e147. [Google Scholar] [CrossRef]
- del Campo, C.B.; Contreras, M.R. Identificación de Factores Relacionados Con La Rotación Laboral de Los Médicos Que Trabajan En Centros de Salud de Atención Primaria Del Gran Santiago; Sociedad Chilena de Políticas Públicas, Centro de Políticas Públicas UC: Santiago, Chile, 2010. [Google Scholar]
- Rebolledo Díaz, C.A. Propuesta de Un Modelo Explicativo Para La Decisión de Permanencia de Los Médicos Generales En Los Establecimientos de Atención Primaria. Ph.D. Thesis, Universidad de Chile, Santiago, Chile, 2022. [Google Scholar]
- Roberto, S.; Paulina, M.T.C. Metodologίa de La Investigación: Las Rutas Cuantitativa, Cualitativa y Mixta; Editorial Mc Graw Hill Education: Columbus, OH, USA, 2018. [Google Scholar]
- Tamayo, M.; Aguirre, M.; Besoain, A. Aproximación al Perfil de Los Directores de Centros de Salud de Atención Primaria En Chile Description Directors of Health Centers of Primary Care in Chile. Cuad. Médicos Soc. 2012, 52, 156–163. [Google Scholar]
- Yusoff, M.S.B. ABC of Content Validation and Content Validity Index Calculation. Educ. Med. J. 2019, 11, 49–54. [Google Scholar] [CrossRef]
- de Souza, A.C.; Alexandre, N.M.C.; de Brito Guirardello, E. Propriedades Psicométricas Na Avaliação de Instrumentos: Avaliação Da Confiabilidade e Da Validade. Epidemiol. Serviços Saúde 2017, 26, 649–659. [Google Scholar] [CrossRef]
- Department of Health Education and Welfare. The Belmont Report: Ethical Principles and Guidelines for the Protection of Human Subjects of Research; DHEW Publication: Washington, DC, USA, 1979. [Google Scholar]
- Dorji, K.; Tejativaddhana, P.; Siripornpibul, T.; Cruickshank, M.; Briggs, D. Leadership and Management Competencies Required for Bhutanese Primary Health Care Managers in Reforming the District Health System. J. Healthc. Leadersh. 2019, 11, 13–21. [Google Scholar] [CrossRef]
- Suárez Conejero, J.E.; Listovsky, G.; Magaña Valladares, L.; Duré, M.I.; García Gutiérrez, J.F.; van Olphen, M. Competencias Esenciales Para La Docencia En Salud Pública: Marco Regional Para Las Américas. Rev. Panam. Salud Pública 2023, 47, e137. [Google Scholar] [CrossRef]
- Astier-Peña, M.P.; Martínez-Bianchi, V.; Torijano-Casalengua, M.L.; Ares-Blanco, S.; Bueno-Ortiz, J.M.; Férnandez-García, M. The Global Patient Safety Action Plan 2021–2030: Identifying Actions for Safer Primary Health Care. Aten. Primaria 2021, 53, 102224. [Google Scholar] [CrossRef]
- Coss-Mandiola, J.; Vanegas-López, J.; Rojas, A.; Dubó, P.; Campillay-Campillay, M.; Carrasco, R. Accreditation of Quality in Primary Health Care in Chile: Perception of the Teams from Accredited Family Healthcare Centers. Int. J. Environ. Res. Public Health 2023, 20, 2477. [Google Scholar] [CrossRef]
- Bronkhorst, B.; Tummers, L.; Steijn, B.; Vijverberg, D. Organizational Climate and Employee Mental Health Outcomes. Health Care Manag. Rev. 2015, 40, 254–271. [Google Scholar] [CrossRef] [PubMed]
- Amoadu, M.; Agyare, D.F.; Doe, P.F.; Abraham, S.A. Examining the Impact of Psychosocial Safety Climate on Working Conditions, Well-Being and Safety of Healthcare Providers: A Scoping Review. BMC Health Serv. Res. 2025, 25, 90. [Google Scholar] [CrossRef] [PubMed]
- Kohnen, D.; De Witte, H.; Schaufeli, W.B.; Dello, S.; Bruyneel, L.; Sermeus, W. Engaging Leadership and Nurse Well-Being: The Role of the Work Environment and Work Motivation—A Cross-Sectional Study. Hum. Resour. Health 2024, 22, 8. [Google Scholar] [CrossRef]
- Paes, L.G.; Fermo, V.C.; de Figueiredo, M.D.C.A.B.; de Mello, A.L.S.F. Care Management in Primary Health Care: A Constructivist Grounded Theory. Texto Contexto—Enferm. 2021, 30, e20200578. [Google Scholar] [CrossRef]
- Yan, Z.; Hong, S.; Liu, F.; Su, Y. A Meta-analysis of the Relationship between Empathy and Executive Function. Psych. J. 2020, 9, 34–43. [Google Scholar] [CrossRef]
- Doǧru, Ç. A Meta-Analysis of the Relationships Between Emotional Intelligence and Employee Outcomes. Front. Psychol. 2022, 13, 611348. [Google Scholar] [CrossRef]
- Chen, Y.-C.; Chiang, Y.-C.; Chu, H.-C. Comprehensive Meta-Analysis of Emotional Intelligence. Work 2025, 80, 548–566. [Google Scholar] [CrossRef]
- World Health Organization; Regional Office for Europe; Association of Schools of Public Health in the European Region (ASPHER). WHO-ASPHER Competency Framework for the Public Health Workforce in the European Region. In WHO-ASPHER Competency Framework for the Public Health Workforce in the European Region; WHO Regional Office for Europe UN City: Copenhagen, Denmark, 2020. [Google Scholar]
| Age | Years of Experience in PHC | Years of Experience in Current Position | Years of Experience at Current Institution | |
|---|---|---|---|---|
| North | 0.728 * | 0.763 * | 0.877 | 0.895 |
| Centre | 0.951 | 0.922 * | 0.919 * | 0.973 |
| South | 0.863 | 0.860 | 0.869 | 0.869 |
| North (n = 5) Arica to Coquimbo | Centre (n = 26) Valparaíso to Biobío | South (n = 5) La Araucanía to Magallanes | |
|---|---|---|---|
| Age M (SD)/Mn (Q1–Q3) | 35 (32–35) | 39.89 (7.20) | 37.40 (4.62) |
| Gender (Women/Men) | 4/1 (80%/20%) | 15/11 (57.69%/42.31%) | 3/2 (60%/40%) |
| Position | |||
| Care role in primary care/teacher/researcher | 0 (0%) | 1 (3.85%) | 0 (0%) |
| Care role in primary care/teacher | 0 (0%) | 6 (23.08%) | 0 (0%) |
| Care role in primary care | 3 (60%) | 9 (34.62%) | 4 (80%) |
| Manager in primary care | 0 (0%) | 8 (30.77%) | 1 (20%) |
| Manager in primary care/care role in primary care | 2 (40%) | 2 (7.69%) | 0 (0%) |
| Educational Level | |||
| Doctorate | 0 (0%) | 1 (3.85%) | 0 (0%) |
| Master’s degree | 1 (20%) | 13 (50%) | 3 (60%) |
| Diploma | 3 (60%) | 11 (42.31%) | 2 (40%) |
| Bachelor’s degree | 1 (20%) | 1 (3.85%) | 0 (0%) |
| Years of experience in PHC M (SD)/Mn (Q1–Q3) | 9 (9–11) | 12 (12–15) | 12.80 (4.49) |
| Years of experience at the current position M (SD)/Mn (Q1–Q3) | 9 (8) | 6.50 (4–10) | 9.80 (4.44) |
| Years of experience in the institution M (SD)/Mn (Q1–Q3) | 9.20 (7.92) | 10.15 (4.31) | 9.80 (4.44) |
| Competency training (yes/no/don’t remember) | 3 (60%)/2 (40%)/0 (0%) | 24 (92.31%)/1 (3.85%)/1 (3.85%) | 5 (100%)/0 (0%)/0 (0%) |
| Knowledge (6 Competences) | Skills (20 Competences) | Attitudes (14 Competences) | |||
|---|---|---|---|---|---|
| 1 | 0.97 | 0.99 | |||
| Previous in health/aps | 1 | Leadership | 1 | Autonomy | 1 |
| Healthcare network | 1 | Teamwork | 1 | Resilience | 1 |
| Health administration and management | 1 | Crisis management | 0.94 | Neutrality | 1 |
| Management and use of indicators | 1 | Institutional alignment | 0.97 | Coping skills | 0.97 |
| Health personnel management | 0.97 | Strategic vision | 0.94 | Creativity | 0.97 |
| Workflows and processes | 1 | Effective communication | 1 | Motivation | 1 |
| Planning, monitoring and evaluation | 1 | Flexibility | 1 | ||
| Recognising skills in others | 0.94 | Professionalism | 1 | ||
| Conflict management | 0.97 | Proactivity | 1 | ||
| Negotiation | 0.97 | Empathy | 1 | ||
| Delegation | 1 | Professional self-realisation | 1 | ||
| Decision-making | 1 | Acting ethically and responsibly | 0.97 | ||
| Articulation skills | 1 | Self-criticism | 1 | ||
| Change management | 0.97 | Initiative | 1 | ||
| Persuasion | 0.94 | ||||
| Relationship building | 0.94 | ||||
| Analytical thinking | 0.97 | ||||
| Innovative thinking | 0.92 | ||||
| Performance evaluation | 0.97 | ||||
| Team building | 0.94 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Soto-Schulz, K.; Herrera-Echenique, R.; Pérez-Romero, N. Competency Profile for Primary Health Care Managers in Chile: Mixed-Methods Validation Through Expert Judgment. Healthcare 2025, 13, 3277. https://doi.org/10.3390/healthcare13243277
Soto-Schulz K, Herrera-Echenique R, Pérez-Romero N. Competency Profile for Primary Health Care Managers in Chile: Mixed-Methods Validation Through Expert Judgment. Healthcare. 2025; 13(24):3277. https://doi.org/10.3390/healthcare13243277
Chicago/Turabian StyleSoto-Schulz, Katherine, Raúl Herrera-Echenique, and Nuria Pérez-Romero. 2025. "Competency Profile for Primary Health Care Managers in Chile: Mixed-Methods Validation Through Expert Judgment" Healthcare 13, no. 24: 3277. https://doi.org/10.3390/healthcare13243277
APA StyleSoto-Schulz, K., Herrera-Echenique, R., & Pérez-Romero, N. (2025). Competency Profile for Primary Health Care Managers in Chile: Mixed-Methods Validation Through Expert Judgment. Healthcare, 13(24), 3277. https://doi.org/10.3390/healthcare13243277






