Combining 675 nm Laser with Isotretinoin for Enhanced Acne Vulgaris Treatment Outcomes
Abstract
1. Introduction
2. Materials and Methods
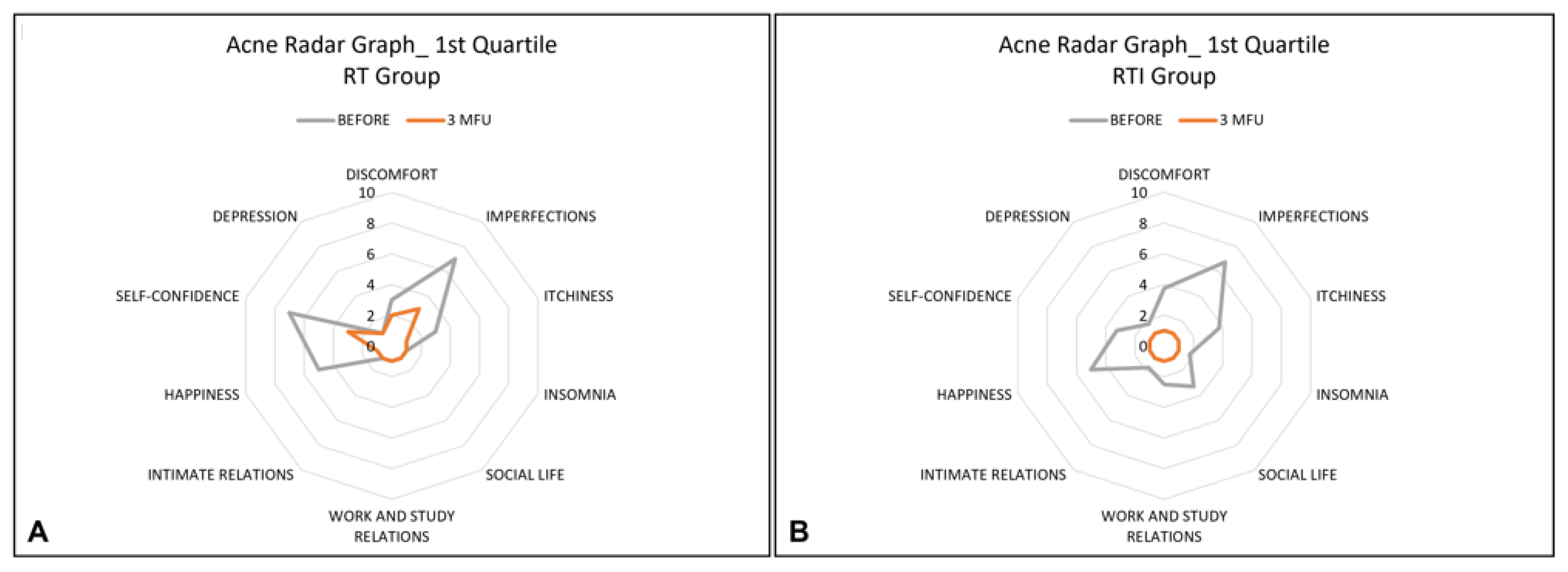
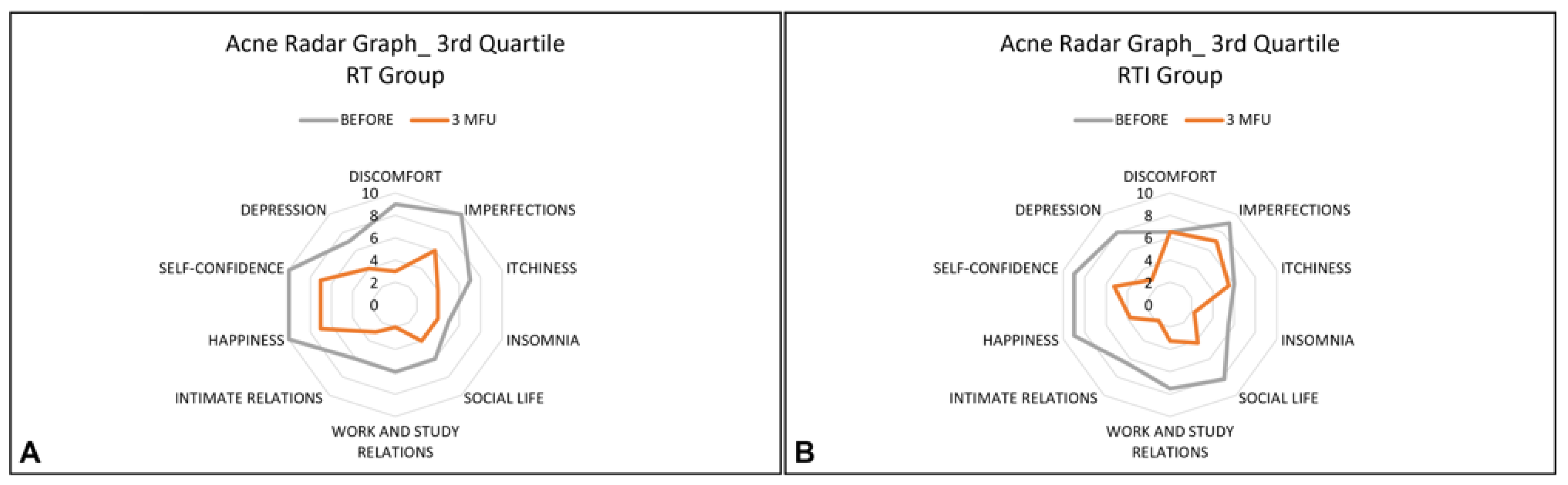
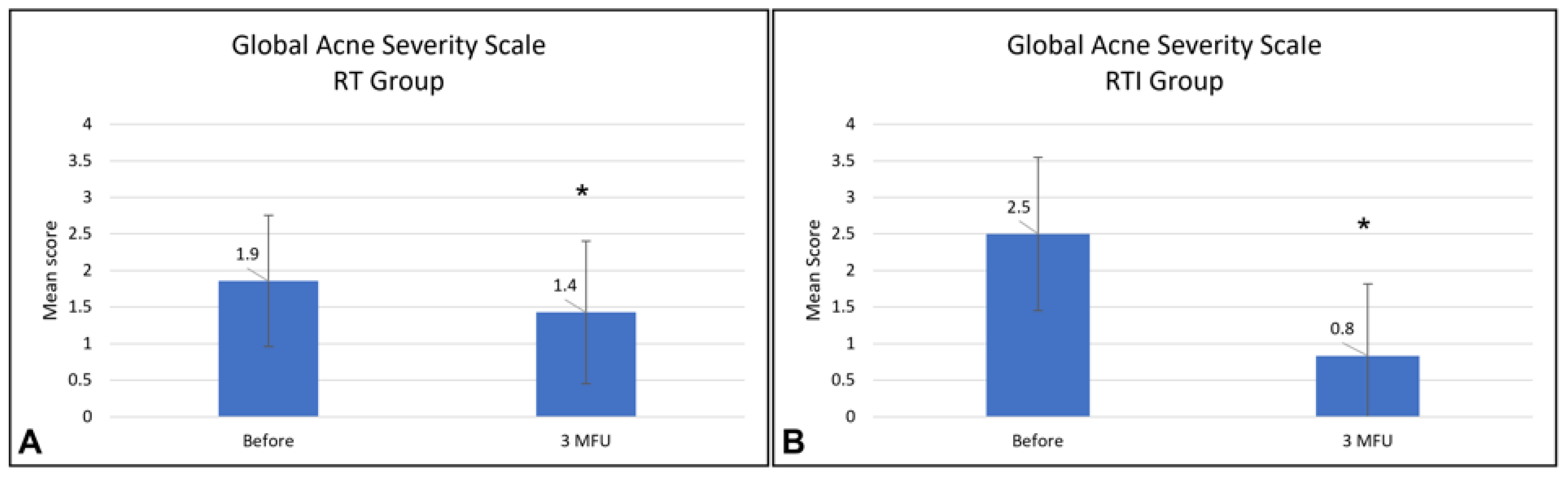
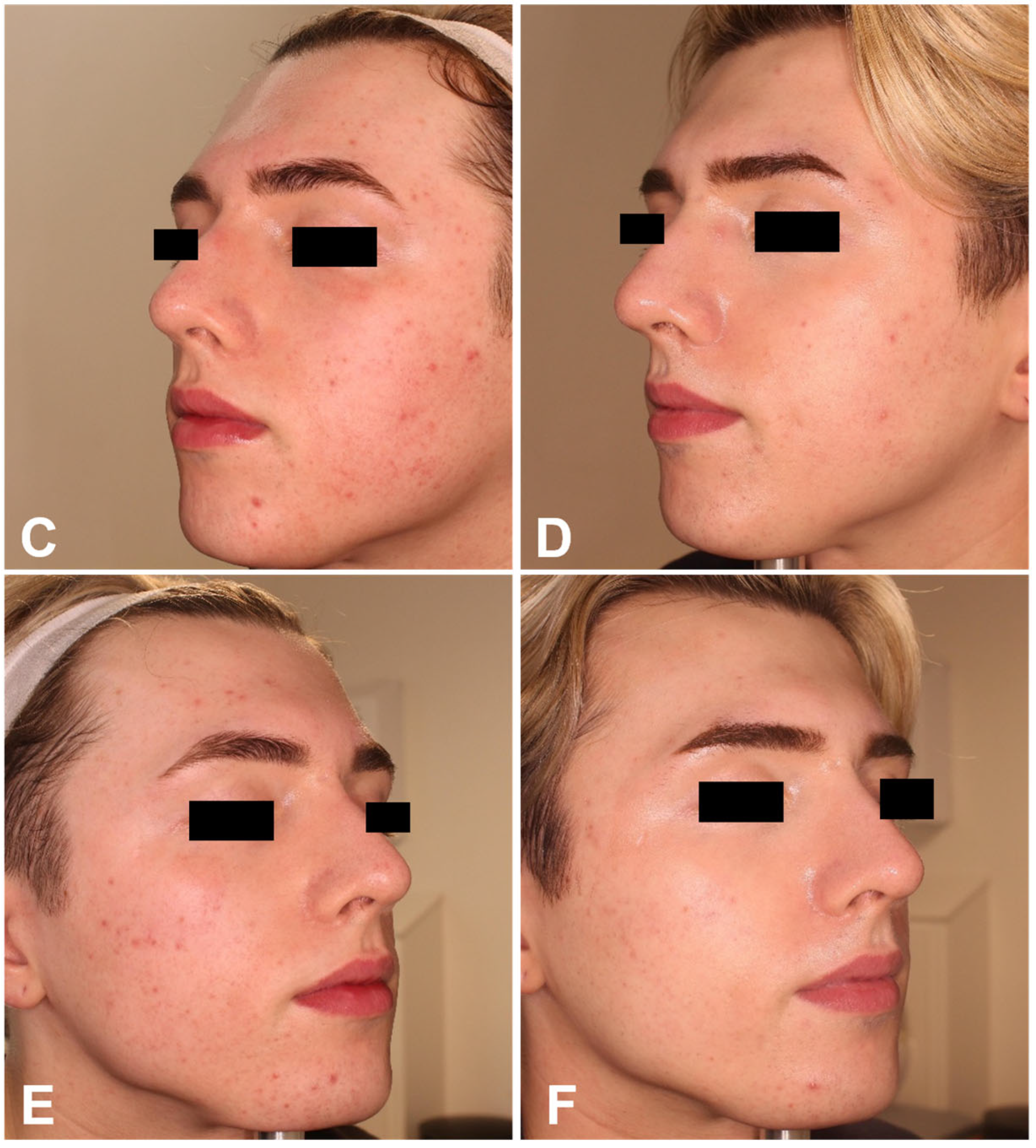
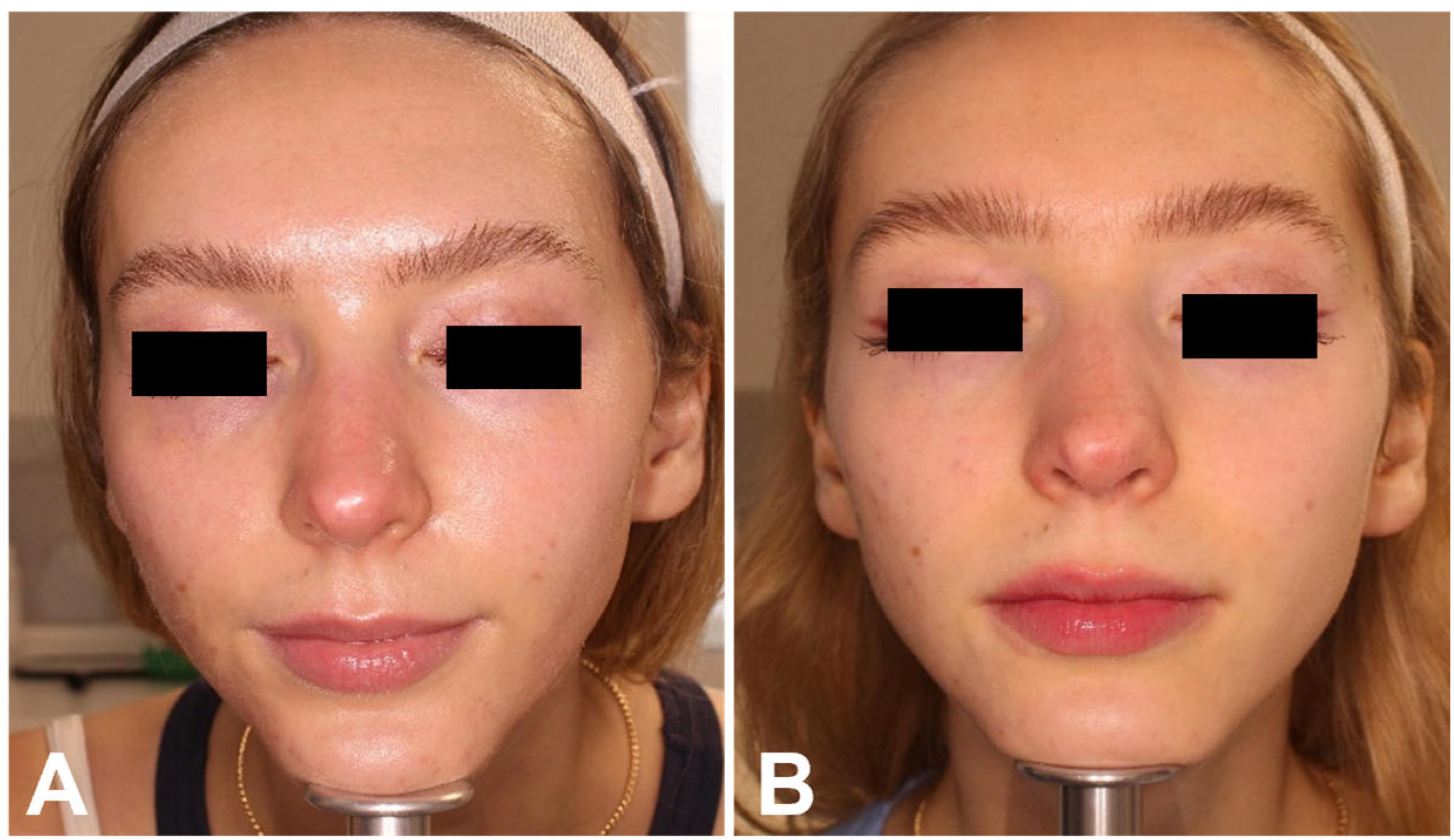
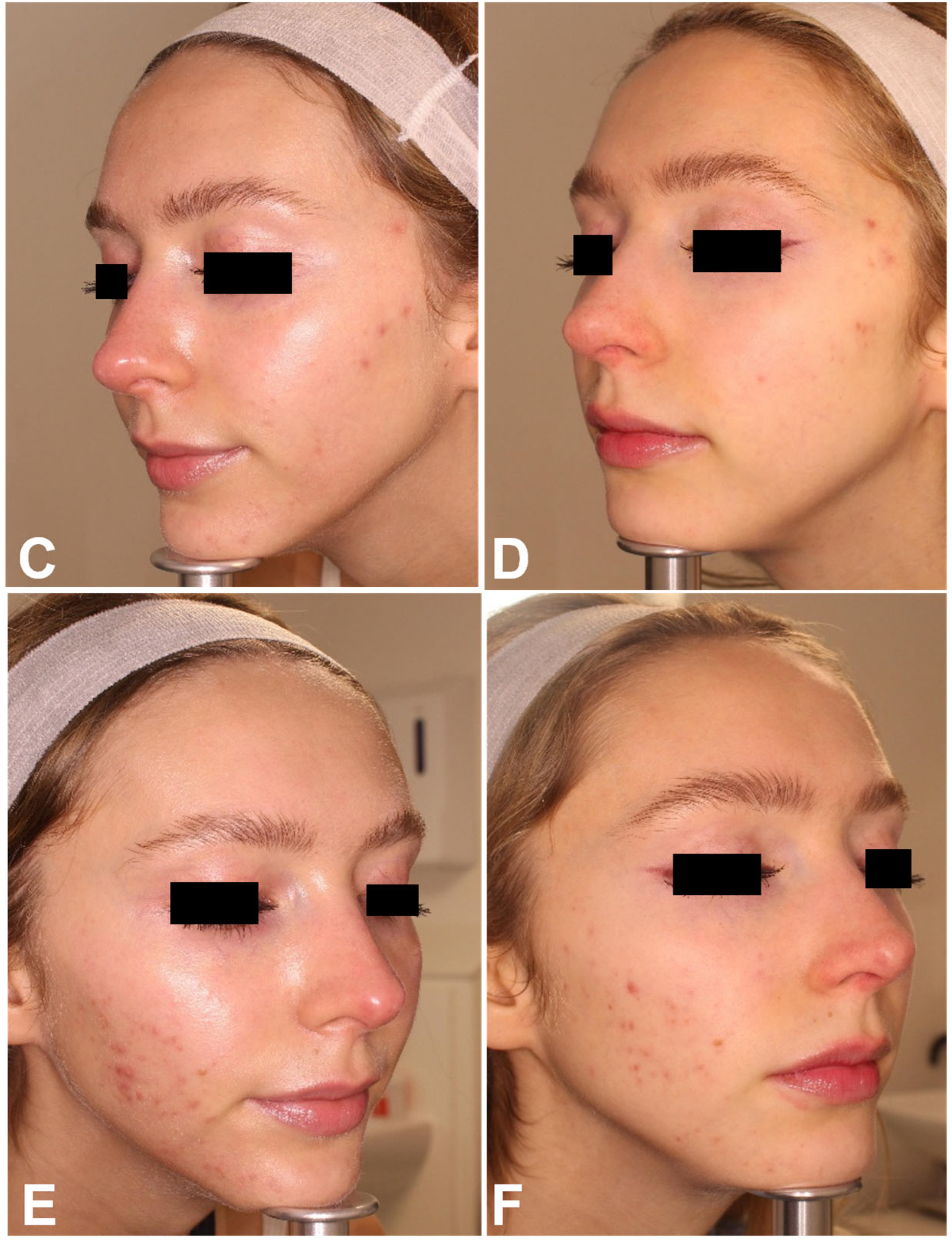
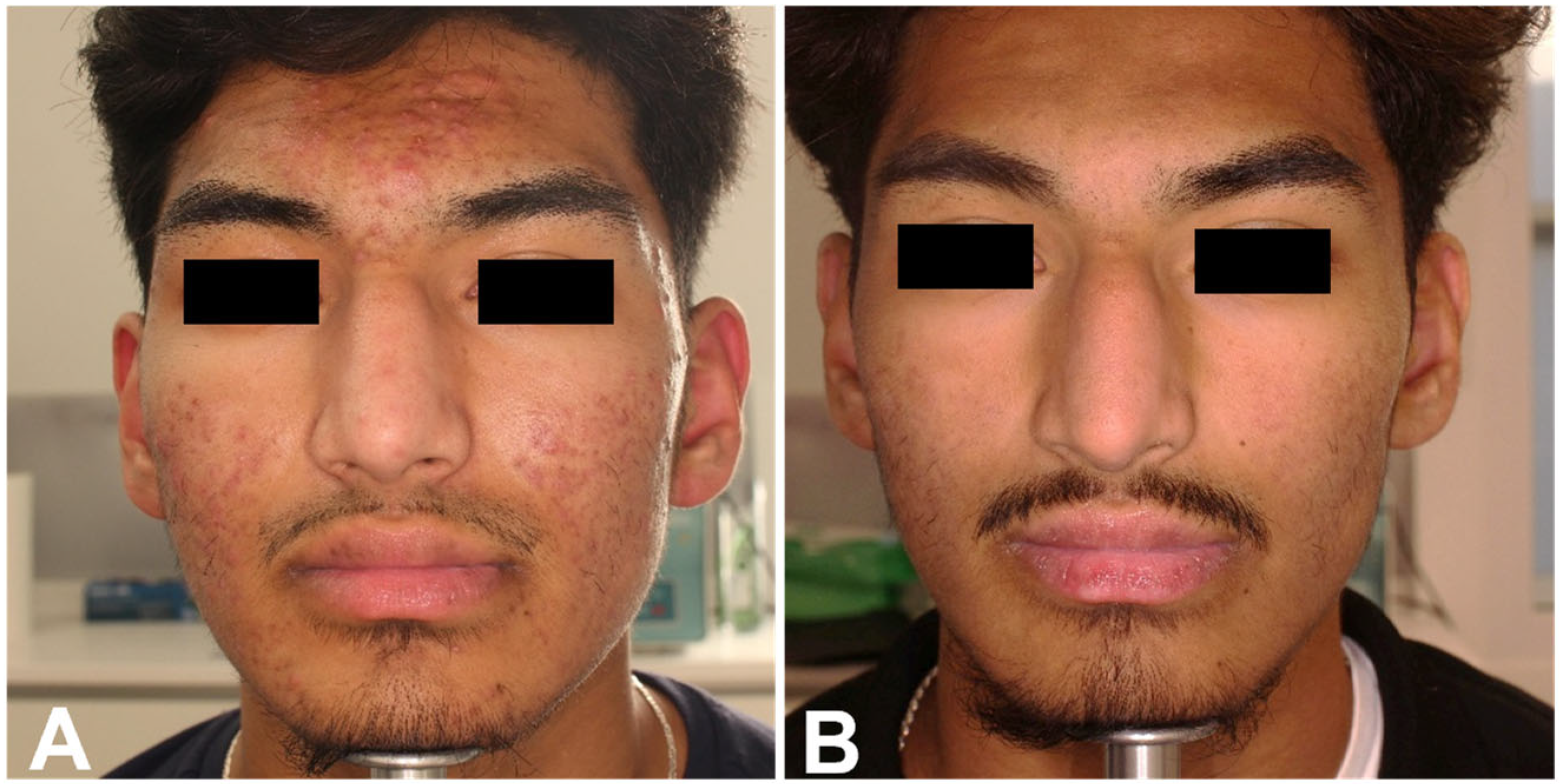
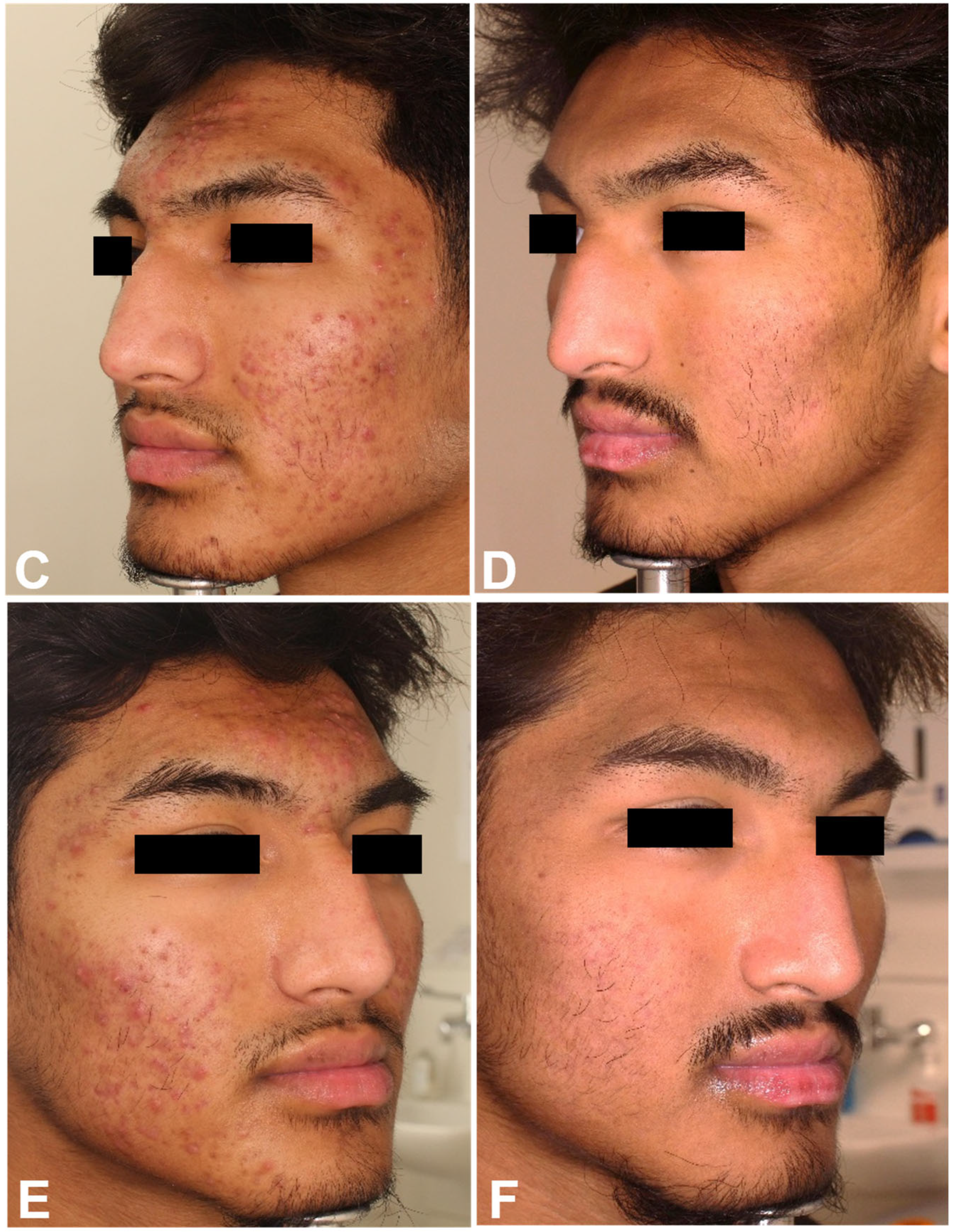
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tan, J.K.; Bhate, K. A global perspective on the epidemiology of acne. Br. J. Dermatol. 2015, 172, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, J.L.; Dabade, T.S.; Davis, S.A.; Feldman, S.R.; Krowchuk, D.P.; Fleischer, A.B. Changing age of acne vulgaris visits: Another sign of earlier puberty? Pediatr. Dermatol. 2011, 28, 645–648. [Google Scholar] [CrossRef] [PubMed]
- Williams, H.C.; Dellavalle, R.P.; Garner, S. Acne vulgaris. Lancet 2012, 379, 361–372. [Google Scholar] [CrossRef] [PubMed]
- Heng, A.H.S.; Chew, F.T. Systematic review of the epidemiology of acne. Sci. Rep. 2020, 10, 5754. [Google Scholar] [CrossRef]
- Sutaria, A.H.; Masood, S.; Saleh, H.M.; Schlessinger, J. Acne Vulgaris. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- Kurokawa, I.; Danby, F.W.; Ju, Q.; Wang, X.; Xiang, L.F.; Xia, L.; Chen, W.; Nagy, I.; Picardo, M.; Suh, D.H.; et al. New developments in our understanding of acne pathogenesis and treatment. Exp. Dermatol. 2009, 18, 821–832. [Google Scholar] [CrossRef]
- Heng, A.H.S.; Say, Y.-H.; Sio, Y.Y.; Ng, Y.T.; Chew, F.T. Epidemiological risk factors associated with acne vulgaris presentation, severity, and scar-ring in a Singapore Chinese population: A cross-sectional study. Dermatology 2022, 238, 226–235. [Google Scholar] [CrossRef]
- Dunn, L.K.; O’Neill, J.L.; Feldman, S.R. Acne in adolescents: Quality of life, self-esteem, mood, and psychological disorders. Dermatol. Online J. 2011, 17, 1. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, R.V.; Yeung, H.; Cheng, C.E.; Cook-Bolden, F.; Desai, S.R.; Druby, K.M.; Freeman, E.E.; Keri, J.E.; Gold, L.F.S.; Tan, J.K.; et al. Guidelines of care for the management of acne vulgaris. J. Am. Acad. Dermatol. 2024, 90, 1006.e1–1006.e30. [Google Scholar] [CrossRef]
- Alexiades, M.; Kothare, A.; Goldberg, D.; Dover, J.S. Novel 1726 nm laser demonstrates durable therapeutic outcomes and tolerability for moderate-to-severe acne across skin types. J. Am. Acad. Dermatol. 2023, 89, 703–710. [Google Scholar] [CrossRef]
- Shah, N.; Smith, E.; Czermak, J.; Ferris, M.; Kirkorian, A.Y. The administrative burden of prescribing and treating with isotretinoin. J. Am. Acad. Dermatol. 2022, 86, 1165–1167. [Google Scholar] [CrossRef]
- Clementi, A.; Cannarozzo, G.; Guarino, L.; Zappia, E.; Cassalia, F.; Alma, A.; Sannino, M.; Longo, C.; Nisticò, S.P. Sequential Fractional CO2 and 1540/1570 nm Lasers: A Narrative Review of Preclinical and Clinical Evidence. J. Clin. Med. 2025, 14, 3867. [Google Scholar] [CrossRef] [PubMed]
- Clementi, A.; Cannarozzo, G.; Amato, S.; Zappia, E.; Bennardo, L.; Michelini, S.; Morini, C.; Sannino, M.; Longo, C.; Nistico, S.P. Dye Laser Applications in Cosmetic Dermatology: Efficacy and Safety in Treating Vascular Lesions and Scars. Cosmetics 2024, 11, 227. [Google Scholar] [CrossRef]
- Clementi, A.; Cassalia, F.; Cannarozzo, G.; Guarino, L.; Zappia, E.; Bennardo, L.; Mazzetto, R.; Danese, A.; Longo, C.; Nisticò, S.P. Laser-Assisted Exosome Delivery (LAED) with Fractional CO2 Laser: A Pilot Two-Case Report and Narrative Re-view. Cosmetics 2025, 12, 199. [Google Scholar] [CrossRef]
- Yang, T.H.; Li, C.N.; Huang, Y.C. The Efficacy of Pulsed Dye Laser Treatment for Acne Vulgaris: A Systemic Review and Me-ta-Analysis. Dermatol. Surg. 2022, 48, 209–213. [Google Scholar] [CrossRef]
- Diogo, M.L.G.; Campos, T.M.; Fonseca, E.S.R.; Pavani, C.; Horliana, A.C.R.T.; Fernandes, K.P.S.; Bussadori, S.K.; Fantin, F.G.M.M.; Leite, D.P.V.; Yamamoto, Â.T.A.; et al. Effect of Blue Light on Acne Vulgaris: A Systematic Review. Sensors 2021, 21, 6943. [Google Scholar] [CrossRef]
- Piccolo, D.; Kostaki, D.; Dianzani, C.; Crisman, G.; Conforti, C. Effective Intense Pulsed Light Protocol in the Treatment of Moderate to Severe Acne Vulgaris of the Chest and Back. J. Clin. Aesthet. Dermatol. 2022, 15, 22–25. [Google Scholar] [PubMed]
- Domenico, P.; Dimitra, K.; Giuliana, C.; Caterina, D.; Gianluca, A.; Roberta, G.; Fabrizio, G.; Stefania, G.; Iris, Z.; Irene, F.; et al. Effective Intense Pulsed Light Protocol in the Treatment of Moderate to Severe Acne Vulgaris. Front. Med. 2022, 9, 946405. [Google Scholar] [CrossRef]
- Vitale, M.D.F.; Madeddu, F.; Fusco, I.; Pieri, L.; Bonan, P.; Zingoni, T.; Magni, G.; Rossi, F. High-powered 675-nm laser: Safety and efficacy in clinical evaluation and in vitro evidence for different skin disorders. Skin. Res. Technol. 2024, 30, e70019. [Google Scholar] [CrossRef]
- Hamblin, M.R. Mechanisms and Mitochondrial Redox Signaling in Photobiomodulation. Photochem. Photobiol. 2018, 94, 199–212. [Google Scholar] [CrossRef]
- Cannarozzo, G.; Silvestri, M.; Tamburi, F.; Sicilia, C.; Del Duca, E.; Scali, E.; Bennardo, L.; Nisticò, S.P. A new 675-nm laser device in the treatment of acne scars: An observational study. Lasers Med. Sci. 2021, 36, 227–231. [Google Scholar] [CrossRef]
- Kuppa, S.S.; Kang, J.Y.; Kim, J.-Y.; Sa, G.; Park, J.-H.; Kim, J.-H.; Ha, T.-S.; Seon, J.K.; Kim, H.K.; Lee, J.-B. Red-light LED therapy promotes wound regeneration by upregulating COL1A1, COL2A1, VEGF and reducing IL-1β for anti-inflammation. Lasers Med. Sci. 2025, 40, 171. [Google Scholar] [CrossRef] [PubMed]
- Alter, I.; Pennati, B.M.; Madeddu, F.; Zingoni, T. The 675 nm laser for the treatment of facial acne scars in dark skin type. Skin. Res. Technol. 2023, 29, e13514. [Google Scholar] [CrossRef] [PubMed]
- Islam, R.K.; Khachemoune, A. Exploring the potential of the emerging 675 nm laser across diverse skin pathologies: A compre-hensive review. J. Cosmet. Laser Ther. 2025, 27, 39–42. [Google Scholar] [CrossRef] [PubMed]
- Cannarozzo, G.; Bennardo, L.; Zingoni, T.; Pieri, L.; Del Duca, E.; Nisticò, S.P. Histological skin changes after treatment with 675 nm laser. Photobiomodul Photomed. Laser Surg. 2021, 39, 617–621. [Google Scholar] [CrossRef]
- Magni, G.; Pieri, L.; Fusco, I.; Madeddu, F.; Zingoni, T.; Rossi, F. Laser emission at 675 nm: In vitro study evidence of a promising role in skin rejuvenation. Regen. Ther. 2023, 22, 176–180. [Google Scholar] [CrossRef]
- Eichenfield, D.Z.; Sprague, J.; Eichenfield, L.F. Management of Acne Vulgaris: A Review. JAMA 2021, 326, 2055–2067. [Google Scholar] [CrossRef]
- Vitale, M.D.F.; Madeddu, F.; Fusco, I.; Bonan, P.; Gallo, G.; Zingoni, T.; Piccolo, D. Clinical evidence of high-power 675 nm laser system equipped with a faster treatment modality for the management of pigmented lesions and skin rejuvenation. JAAD Case Rep. 2025, 58, 93–98. [Google Scholar] [CrossRef]
- Fabbrocini, G.; Lauro, C.; Izzo, R.; Mazzella, C.; Di Bonito, M.; Piccolo, A.; Ricci, C.; Monfrecola, G. Acne radar: A new intuitive graphic visualization of quality of life in acne pa-tients. J. Plast. Dermatol. 2013, 9, 165–172. [Google Scholar]
- Dréno, B.; Poli, F.; Pawin, H.; Beylot, C.; Faure, M.; Chivot, M.; Auffret, N.; Moyse, D.; Ballanger, F.; Revuz, J. Development and evaluation of a Global Acne Severity Scale (GEA Scale) suitable for France and Europe. J. Eur. Acad. Dermatol. Venereol. 2011, 25, 43–48. [Google Scholar] [CrossRef]
- Bagatin, E.; Costa, C.S. The use of isotretinoin for acne—An update on optimal dosing, surveillance, and adverse effects. Expert Rev. Clin. Pharmacol. 2020, 13, 885–897. [Google Scholar] [CrossRef]
- Melnik, B.C. Isotretinoin and FoxO1: A scientific hypothesis. Dermato-endocrinology 2011, 3, 141–165. [Google Scholar] [CrossRef] [PubMed]
- Tsukada, M.; Schröder, M.; Orfanos, C.E.; Zouboulis, C.C.; Roos, T.C.; Chandraratna, R.A.; Reichert, U.; Merk, H.F. 13-cis retinoic acid exerts its specific activity on human sebocytes through selective intracellular isomerization to all-trans retinoic acid and binding to retinoid acid receptors. J. Investig. Dermatol. 2000, 115, 321–327. [Google Scholar] [CrossRef] [PubMed]
- Melnik, B.C. Pro-inflammatory sebocyte growth and survival signalling in acne vulgaris are reversed by pro-apoptotic isotret-inoin signalling. Exp. Dermatol. 2016, 25, 676–677. [Google Scholar] [CrossRef]
- Nelson, A.; Cong, Z.; Gilliland, K.; Thiboutot, D. TRAIL contributes to the apoptotic effect of 13-cis retinoic acid in human sebaceous gland cells. Br. J. Dermatol. 2011, 165, 526–533. [Google Scholar] [CrossRef]
- Mirdamadi, Y.; Thielitz, A.; Wiede, A.; Goihl, A.; Papakonstantinou, E.; Hartig, R.; Zouboulis, C.C.; Reinhold, D.; Simeoni, L.; Bommhardt, U.; et al. Insulin and insulin-like growth factor-1 can modulate the phosphoinosi-tide-3-kinase/Akt/FoxO1 pathway in SZ95 sebocytes in vitro. Mol. Cell Endocrinol. 2015, 415, 32–44. [Google Scholar] [CrossRef]
- Agamia, N.; Abdallah, D.; Sorour, O.S.; Mourad, B.; Younan, D.Y. Skin expression of mammalian target of rapamycin and forkhead box tran-scription factor O1, and serum insulin-like growth factor-1 in patients with acne vulgaris and their relationship with diet. Br. J. Dermatol. 2016, 174, 1299–1307. [Google Scholar] [CrossRef]
- Erkelens, M.N.; Mebius, R.E. Retinoic Acid and Immune Homeostasis: A Balancing Act. Trends Immunol. 2017, 38, 168–180. [Google Scholar] [CrossRef]
- AlJasser, R.N.; Alaqeely, R.S.; Al-Hoqail, I.A.; Al-Haddab, M.; AlQahtani, S.S.; AlKenani, M.E.; AlZahrani, A.M.; AlOraini, S. Association between isotretinoin (Roaccutanne) use and changes in perio-dontal clinical parameters and MMP-8 and MMP-9 salivary levels. Front. Biosci. 2021, 26, 191–197. [Google Scholar] [CrossRef]
- Sadeghzadeh-Bazargan, A.; Ghassemi, M.; Goodarzi, A.; Roohaninasab, M.; Nobari, N.N.; Behrangi, E. Systematic review of low-dose isotretinoin for treatment of acne vulgaris: Focus on indication, dosage, regimen, efficacy, safety, satisfaction, and follow up, based on clinical studies. Dermatol. Ther. 2021, 34, e14438. [Google Scholar] [CrossRef]
- Xu, Y.; Wang, H.; Guo, L.; Hamblin, M.R.; Wen, X. Combinations of Energy-based Devices plus isotretinoin for management of acne and acne scars: A systematic review. J. Cosmet. Dermatol. 2024, 23, 3090–3101. [Google Scholar] [CrossRef]
- Jarab, A.S.; Al-Azzam, S.; Almutairi, S.; Mukattash, T.L. Patients’ Knowledge and Information Needs about Isotretinoin Therapy Use in Jordan. Int. J. Clin. Pract. 2022, 2022, 9443884. [Google Scholar] [CrossRef]
- Spring, L.K.; Krakowski, A.C.; Alam, M.; Bhatia, A.; Brauer, J.; Cohen, J.; Del Rosso, J.Q.; Diaz, L.; Dover, J.; Eichenfield, L.F.; et al. Isotretinoin and Timing of Procedural Interventions: A Systematic Review with Consensus Recommendations. JAMA Dermatol. 2017, 153, 802–809. [Google Scholar] [CrossRef]
- Notari, L.; Pieri, L.; Cialdai, F.; Fusco, I.; Risaliti, C.; Madeddu, F.; Bacci, S.; Zingoni, T.; Monici, M. Laser Emission at 675 nm: Molecular Counteraction of the Aging Process. Biomedicines 2024, 12, 2713. [Google Scholar] [CrossRef]
- Hernández-Bule, M.L.; Naharro-Rodríguez, J.; Bacci, S.; Fernández-Guarino, M. Unlocking the Power of Light on the Skin: A Comprehensive Review on Photobiomodulation. Int. J. Mol. Sci. 2024, 25, 4483. [Google Scholar] [CrossRef]
- Thiboutot, D.M.; Weiss, J.; Bucko, A.; Eichenfield, L.; Jones, T.; Clark, S.; Liu, Y.; Graeber, M.; Kang, S.; Adapalene-BPO Study Group. Adapalene-benzoyl peroxide, a fixed-dose combination for the treatment of acne vulgaris: Results of a multicenter, randomized double-blind, controlled study. J. Am. Acad. Dermatol. 2007, 57, 791–799. [Google Scholar] [CrossRef]
- Cook, C.H.; Centner, R.L.; Michaels, S.E. An acne grading method using photographic standards. Arch. Dermatol. 1979, 115, 571–575. [Google Scholar] [CrossRef] [PubMed]


| Group | Sex | Age | Fitzpatrick Skin Type |
|---|---|---|---|
| RT group | 86% females 14% males | 28 ± 8.3 years | 29% type II 42% type III 29% type IV |
| RTI group | 33% females 67% males | 20.3 ± 2.9 years | 17% type I 66% type II 17% type V |
| Fitzpatrick Skin Type | Power (W) | Dwell Time (ms) | Spacing (μm) | SmartStack | Energy/DOT (J) | Number of Treatments | Time Interval Between Treatments |
|---|---|---|---|---|---|---|---|
| I | 10 | 150 | 1500 | 1 | 1.5 | 6 | 7 Days |
| II | 10 | 150 | 1500 | 1 | 1.5 | 6 | 7 Days |
| III | 5–10 | 125–150 | 1500–2000 | 1 | 0.625–1.5 | 6 | 7 Days |
| IV | 5–8 | 100–150 | 2000–2500 | 1 | 0.5–1.2 | 6 | 7 Days |
| V | 5 | 125 | 1500 | 1 | 0.625 | 6 | 7 Days |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haus, A.; Clementi, A.; Cannarozzo, G.; Guarino, L.; Zappia, E.; Gratteri, M.; Dattola, A.; Nisticò, S.P. Combining 675 nm Laser with Isotretinoin for Enhanced Acne Vulgaris Treatment Outcomes. Healthcare 2025, 13, 3068. https://doi.org/10.3390/healthcare13233068
Haus A, Clementi A, Cannarozzo G, Guarino L, Zappia E, Gratteri M, Dattola A, Nisticò SP. Combining 675 nm Laser with Isotretinoin for Enhanced Acne Vulgaris Treatment Outcomes. Healthcare. 2025; 13(23):3068. https://doi.org/10.3390/healthcare13233068
Chicago/Turabian StyleHaus, Ariel, Alessandro Clementi, Giovanni Cannarozzo, Luca Guarino, Elena Zappia, Marco Gratteri, Annunziata Dattola, and Steven Paul Nisticò. 2025. "Combining 675 nm Laser with Isotretinoin for Enhanced Acne Vulgaris Treatment Outcomes" Healthcare 13, no. 23: 3068. https://doi.org/10.3390/healthcare13233068
APA StyleHaus, A., Clementi, A., Cannarozzo, G., Guarino, L., Zappia, E., Gratteri, M., Dattola, A., & Nisticò, S. P. (2025). Combining 675 nm Laser with Isotretinoin for Enhanced Acne Vulgaris Treatment Outcomes. Healthcare, 13(23), 3068. https://doi.org/10.3390/healthcare13233068








