Influence of Hypnosis and Acupuncture on Perioperative Complications
Abstract
1. Introduction
2. Materials and Methods
- -
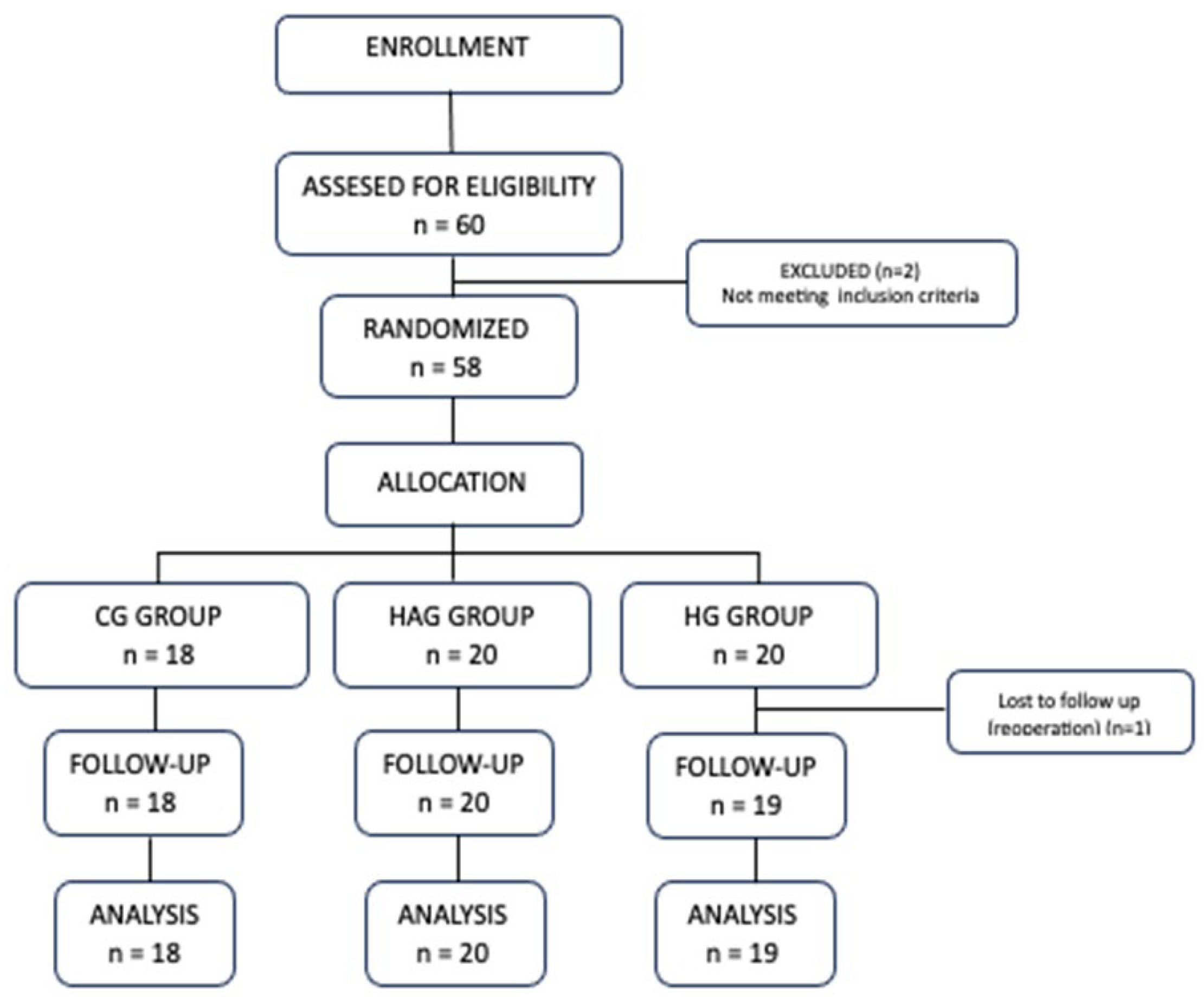
- HG (Hypno-acupuncture Group): Received hypnosis and acupuncture in addition to standard anaesthesia protocol, without ondansetron.
- -
- HAG (Hypno-acupuncture + Antiemetic Group): Received hypnosis, acupuncture and ondansetron with standard anaesthesia protocol.
- -
- CG (Control Group): Received standard premedication with midazolam and standard anaesthesia protocol with ondansetron, without hypnosis and acupuncture.
2.1. Perioperative Management
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Correction Statement
Abbreviations
| ASA | American Society of Anaesthesiologists |
| CS | Cervical Spine |
| LS | Lumbar Spine |
| PACU | Postoperative Care Unit |
| LOS | Length of the Day |
| PONV | Postoperative Nausea and Vomiting |
| HG | Hypno-acupuncture Group |
| HAG | Hypno-acupuncture Group with Antiemetic |
| CG | Control Group |
| UMC | University Medical Centre |
| ICU | Intensive Care Unit |
| LOS | Length of Stay |
| MMA | Multimodal Analgesia |
| TCI | Target-Controlled Infusion |
| TOF | Train-of-Four |
| NRS | Numerical Rating Scale |
| PCA | Patient-Controlled Analgesia |
References
- Lu, Z.; Dong, H.; Wang, Q.; Xiong, L. Perioperative acupuncture modulation: More than anaesthesia. Br. J. Anaesth. 2015, 115, 183–193. [Google Scholar] [CrossRef]
- Asmussen, S.; Maybauer, D.M.; Chen, J.D.; Fraser, J.F.; Toon, M.H.; Przkora, R.; Jennings, K.; Maybaur, M.O. Effects of acupuncture in anesthesia for craniotomy: A meta-analysis. J. Neurosurg. Anesthesiol. 2017, 29, 219–227. [Google Scholar] [CrossRef]
- Schug, S.A.; Palmer, G.M.; Scott, D.A.; Alcock, M.; Halliwell, R.; Mott, J.F. Acute Pain Management: Scientific Evidence, 5th ed.; ANZCA & FPM: Melbourne, VIC, Australia, 2020. [Google Scholar]
- Arnberger, M.; Stadelmann, K.; Alischer, P.; Ponert, R.; Melber, A.; Greif, R. Monitoring of meeting abstracts at the P6 acupuncture point reduces the incidence of postoperative nausea and vomiting. Anesthesiology 2007, 107, 903–908. [Google Scholar] [CrossRef]
- Cheong, K.B.; Zhang, J.-P.; Huang, Y.; Zhang, Z.-J. The effectiveness of acupuncture in prevention and treatment of postoperative nausea and vomiting: A systematic review and meta-analysis. PLoS ONE 2013, 8, e82474. [Google Scholar] [CrossRef] [PubMed]
- Elkins, G.R.; Barabasz, A.F.; Council, J.R.; Spiegel, D. Advancing research and practice: The revised APA Division 30 definition of hypnosis. Int. J. Clin. Exp. Hypn. 2015, 63, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Schnur, J.B.; Kafer, I.; Marcus, C.; Montgomery, G.H. Hypnosis to manage distress related to medical procedures: A meta-analysis. Contemp. Hypn. 2008, 25, 114–128. [Google Scholar] [CrossRef]
- Kekecs, Z.; Nagy, T.; Varga, K. The effectiveness of suggestive techniques in reducing postoperative side effects: A meta-analysis of randomized controlled trials. Anesth. Analg. 2014, 119, 1407–1419. [Google Scholar] [CrossRef] [PubMed]
- Markovič Božič, J.; Spindler Vesel, A. Perioperative use of medical hypnosis. Zdrav. Vestn. 2021, 90, 202–207. [Google Scholar] [CrossRef]
- Potié, A.; Roelants, F.; Pospiech, A.; Momeni, M.; Watremez, C. Hypnosis in the perioperative management of breast cancer surgery: Clinical benefits and potential implications. Anesthesiol. Res. Pract. 2016, 2016, 2942416. [Google Scholar] [CrossRef]
- Schnur, J.B.; Bovbjerg, D.H.; David, D.; Tatrow, K.; Goldfarb, A.B.; Silverstein, J.H.; Montgomery, G.H. Hypnosis decreases presurgical distress in excisional breast biopsy patients. Anesth. Analg. 2008, 106, 440–444. [Google Scholar] [CrossRef]
- Tefikow, S.; Barth, J.; Maichrowitz, S.; Beelmann, A.; Strauss, B.; Rosendahl, J. Efficacy of hypnosis in adults undergoing surgery or medical procedures: A meta-analysis of randomized controlled trials. Clin. Psychol. Rev. 2013, 33, 623–636. [Google Scholar] [CrossRef]
- Apfel, C.C.; Läärä, E.; Koivuranta, M.; Greim, C.-A.; Roewer, N. A simplified risk score for predicting postoperative nausea and vomiting: Conclusions from cross-validations between two centers. Anesthesiology 1999, 91, 693–700. [Google Scholar] [CrossRef] [PubMed]
- Gan, T.J.; Belani, K.G.; Bergese, S.; Chung, F.; Diemunsch, P.; Habib, A.S.; Jin, Z.; Kovac, A.L.; Meyer, T.A.; Urman, R.D.; et al. Fourth consensus guidelines for the management of postoperative nausea and vomiting. Anesth. Analg. 2020, 131, 411–448. [Google Scholar] [CrossRef] [PubMed]
- Janjua, M.S.; Spurling, B.C.; Arthur, M.E. Postoperative Delirium. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024; Updated 12 February 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK534831/ (accessed on 17 November 2025).
- Kalish, V.B.; Gillham, J.E.; Unwin, B.K. Delirium in older persons: Evaluation and management. Am. Fam. Physician 2014, 90, 150–158. [Google Scholar] [PubMed]
- Chaiwat, O.; Chanidnuan, M.; Pancharoen, W.; Vijitmala, K.; Danpornprasert, P.; Toadithep, P.; Thanakiattiwibun, C. Postoperative delirium in critically ill surgical patients: Incidence, risk factors, and predictive scores. BMC Anesthesiol. 2019, 19, 39. [Google Scholar] [CrossRef]
- Yoo, J.S.; Ahn, J.; Buvanendran, A.; Singh, K. Multimodal analgesia in pain management after spine surgery. J. Spine Surg. 2019, 5 (Suppl. S2), S154–S159. [Google Scholar] [CrossRef]
- Schwenk, E.S.; Mariano, E.R. Designing the ideal perioperative pain management plan starts with multimodal analgesia. Korean J. Anesthesiol. 2018, 71, 345352. [Google Scholar] [CrossRef]
- Wu, M.-S.; Chen, K.-H.; Chen, I.-F.; Huang, S.K.; Tzeng, P.-C.; Yeh, M.-L.; Lee, F.-P.; Lin, J.-G.; Chen, C. The efficacy of acupuncture in post-operative pain management: A systematic review and meta-analysis. PLoS ONE 2016, 11, e0150367. [Google Scholar] [CrossRef]
- Sun, Y.; Gan, T.J.; Dubose, J.W.; Habib, A.S. Acupuncture and related techniques for postoperative pain: A systematic review of randomized controlled trials. Br. J. Anaesth. 2008, 101, 151–160. [Google Scholar] [CrossRef]
- Halsband, U.; Wolf, T.G. Functional changes in brain activity after hypnosis in patients with dental phobia. J. Physiol. 2015, 109, 131–142. [Google Scholar] [CrossRef]
- Blankfield, R.P. Suggestion, relaxation, and hypnosis as adjuncts in the care of surgery patients: A review of the literature. Am. J. Clin. Hypn. 1991, 33, 172186. [Google Scholar] [CrossRef]
- Faymonville, M.-E.; Mambourg, P.H.; Joris, J.; Vrijens, B.; Fissette, J.; Albert, A.; Lamy, M. Psychological approaches during conscious sedation. Hypnosis versus stress reducing strategies: A prospective randomized study. Pain 1997, 73, 361–367. [Google Scholar] [CrossRef] [PubMed]
- Ginandes, C.; Brooks, P.; Sando, W.; Jones, C.; Aker, J. Can medical hypnosis accelerate post-surgical wound healing? Results of a clinical trial. Am. J. Clin. Hypn. 2003, 45, 333–351. [Google Scholar] [CrossRef]
- Vanhaudenhuyse, A.; Laureys, S.; Faymonville, M.E. Neurophysiology of hypnosis. Clin. Neurophysiol. 2014, 44, 343–353. [Google Scholar] [CrossRef]
- Markovits, J.; Blaha, O.; Zhao, E.; Spiegel, D. Effects of hypnosis versus enhanced standard of care on postoperative opioid use after total knee arthroplasty: The HYPNO-TKA randomized clinical trial. Reg. Anesth. Pain Med. 2022, 47, 534–540. [Google Scholar] [CrossRef]
- Shiao, S.Y.; Dune, L.S. Metaanalyses of acustimulations: Effects on nausea and vomiting in postoperative adult patients. Explore 2006, 2, 202–215. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.; Fan, L.T.Y. Stimulation of the wrist acupuncture point P6 for preventing postoperative nausea and vomiting. Cochrane Database Syst. Rev. 2009, 15, CD003281. [Google Scholar] [CrossRef]
- Cho, H.K.; Park, I.J.; Jeong, Y.M.; Lee, Y.J.; Hwang, S.H. Can perioperative acupuncture reduce the pain and vomiting experienced after tonsillectomy? Meta-analysis. Laryngoscope 2016, 126, 608–615. [Google Scholar] [CrossRef]
- Lee, S.; Lee, M.S.; Choi, D.H.; Lee, S.K. Electroacupuncture on PC6 prevents opioid-induced nausea and vomiting after laparoscopic surgery. Chin. J. Integr. Med. 2013, 19, 277–281. [Google Scholar] [CrossRef] [PubMed]
- Gan, T.J.; Jiao, K.R.; Zenn, M.; Georgiade, G. A randomized controlled comparison of electroacupoint stimulation or ondansetron versus placebo for the prevention of postoperative nausea and vomiting. Anesth. Analg. 2004, 99, 1070–1075. [Google Scholar] [CrossRef]
- Wang, S.M.; Kain, Z.N. P6 acupoint injections are as effective as droperidol in controlling early postoperative nausea and vomiting in children. Anesthesiology 2002, 97, 359–366. [Google Scholar] [CrossRef] [PubMed]
- Stein, D.J.; Birnbach, D.J.; Danzer, B.I.; Kuroda, M.M.; Grunebaum, A.; Thys, D.M. Acupressure versus intravenous metoclopramide to prevent nausea and vomiting during spinal anesthesia for cesarean section. Anesth. Analg. 1997, 84, 342–345. [Google Scholar] [CrossRef]
- Sessler, D.I.; Sigl, J.C.; Kelley, S.D.; Chamoun, N.G.; Manberg, P.J.; Saager, L.; Kurz, A.; Greenwald, S. Hospital stay and mortality are increased in patients having a “triple low” of low blood pressure, low bispectral index, and low minimum alveolar concentration of volatile anesthesia. Anesthesiology 2012, 116, 1195–1203. [Google Scholar] [CrossRef]
- Helander, E.M.; Menard, B.L.; Harmon, C.M.; Homra, B.K.; Allain, A.V.; Bordelon, G.J.; Wyche, M.Q.; Padnos, I.W.; Lavrova, A.; Kaye, A.D. Multimodal Analgesia, Current Concepts, and Acute Pain Considerations. Curr. Pain Headache Rep. 2017, 21, 3. [Google Scholar] [CrossRef] [PubMed]
- Kotani, N.; Hashimoto, H.; Sato, Y.; Sessler, D.I.; Yoshioka, H.; Kitayama, M.; Yasuda, T.; Matsuki, A. Preoperative intradermal acupuncture reduces postoperative pain, nausea and vomiting, analgesic requirement, and sympathoadrenal responses. Anesthesiology 2001, 95, 349–356. [Google Scholar] [CrossRef]
- Lin, J.G.; Lo, M.W.; Wen, Y.R.; Hsieh, C.L.; Tsai, S.K.; Sun, W.Z. The effect of high and low frequency electroacupuncture in pain after lower abdominal surgery. Pain 2002, 99, 509–514. [Google Scholar] [CrossRef]
- Stener-Victorin, E.; Waldenström, U.; Nilsson, L.; Janson, L.; Wikland, M. A prospective randomized study of electro-acupuncture versus alfentanil as anaesthesia during oocyte aspiration in in-vitro fertilization. Hum. Reprod. 1999, 14, 2480–2484. [Google Scholar] [CrossRef]
- Kho, H.G.; van Egmond, J.; Zhuang, C.F.; Cho, M.; Liu, C. Acupuncture anaesthesia. Observations on its use for removal of thyroid adenomata and influence on recovery and morbidity in a Chinese hospital. Anaesthesia 1990, 45, 480–485. [Google Scholar] [CrossRef]
- Christensen, P.A.; Noreng, M.; Andersen, P.E.; Nielsen, J.W. Electroacupuncture and postoperative pain. Br. J. Anaesth. 1989, 62, 258–262. [Google Scholar] [CrossRef]
- Gupta, S.; Francis, J.D.; Tillu, A.B.; Sattirajah, I.; Sizer, J. The effect of pre-emptive acupuncture treatment on analgesic requirements after day-case knee arthroscopy. Anaesthesia 1999, 54, 1204–1207. [Google Scholar] [CrossRef] [PubMed]
- Gilbey, P.; Bretler, S.; Avraham, Y.; Lazarovich, A.; Almogy, G.; Martinuzzi, A.; Mandel, M.; Victor, N.; Barak, Y. Acupuncture for posttonsillectomy pain in children: A randomized, controlled study. Pediatr. Anesth. 2015, 25, 603–609. [Google Scholar] [CrossRef]
- Usichenko, T.I.; Dinse, M.; Hermsen, M.; Witstruck, T.; Pavlovic, D.; Lehmann, C. Auricular acupuncture for pain relief after total hip arthroplasty—A randomized controlled study. Pain 2005, 114, 320–327. [Google Scholar] [CrossRef] [PubMed]
- El-Rakshy, M.; Clark, S.C.; Thompson, J.; Khan, Z.; Elshazly, M.; Smith, C. Effect of intraoperative electroacupuncture on postoperative pain, analgesic requirements, nausea and sedation: A randomized controlled trial. Acupunct. Med. 2009, 27, 9–12. [Google Scholar] [CrossRef] [PubMed]
- Cherynyak, G.V.; Sessler, D.I. Perioperative acupuncture and related techniques. Anesthesiology 2005, 102, 1031–1078. [Google Scholar] [CrossRef]
- Wang, S.M.; Kain, Z.N.; White, P.F. Acupuncture analgesia: II. Clinical considerations. Anesth. Analg. 2008, 106, 611–621. [Google Scholar] [CrossRef] [PubMed]
- Ulett, G.; Han, S.; Han, J. Electroacupuncture: Mechanisms and clinical application. Biol. Psychiatry 1998, 44, 129–138. [Google Scholar] [CrossRef]
- Huang, X.; Cai, J.; Lv, Z.; Zhou, Z.; Zhou, X.; Zhao, Q.; Sun, J.; Chen, L. Postoperative pain after different doses of remifentanil infusion during anaesthesia: A meta-analysis. BMC Anesthesiol. 2024, 24, 25. [Google Scholar] [CrossRef]
| GROUP | CG (n = 18) | HAG (n = 20) | HG (n = 19) | p |
|---|---|---|---|---|
| Age (years) | 60 ±12 | 60 ± 10 | 61 ± 13 | 0.9 |
| Gender (male/female) | 10/8 | 14/6 | 10/9 | 0.5 |
| Weight (kg) | 89 ± 15 | 87 ± 12 | 79 ± 13 | 0.1 |
| Height (cm) | 173 ± 8 | 175 ± 9 | 170 ± 11 | 0.2 |
| ASA (1/2/3) | 3/13/2 | 1/17/2 | 3/12/4 | 0.6 |
| Type of surgery (CS/LS) | 0/18 | 4/16 | 2/17 | 0.1 |
| GROUP | CG (n = 18) | HAG (n = 20) | HG (n = 19) | p |
|---|---|---|---|---|
| Additional analgesic PACU (yes/no) | 17/1 | 16/4 | 16/3 | 0.4 |
| Additional analgesic ICU (yes/no) | 2/16 | 1/19 | 2/17 | 0.8 |
| Additional antiemetic PACU (yes/no) | 0/18 | 0/20 | 1/18 | 0.4 |
| Additional antiemetic ICU (yes/no) | 0/18 | 0/20 | 1/18 | 0.4 |
| GROUP | CG (n = 18) | HAG (n = 20) | HG (n = 19) | p |
|---|---|---|---|---|
| Well-being (perfect/very good/good) | 9/9/0 | 10/6/4 | 9/7/3 | 0.4 |
| Satisfaction (perfect/very good/good) | 10/8/0 | 13/5/2 | 13/5/1 | 0.5 |
| LOS (days) | 3 ± 1 | 4 ± 2 | 4 ± 2 | 0.7 |
| Complications (no/yes) | 16/2 | 20/0 | 19/0 | 0.1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Markovič-Božič, J.; Gradišar, M.; Petovar, M.; Mušič, P.; Pirc, N.; Meyerson, J.; Tušak, M.; Lapoša, A.; Tušak, M.; Spindler-Vesel, A. Influence of Hypnosis and Acupuncture on Perioperative Complications. Healthcare 2025, 13, 2992. https://doi.org/10.3390/healthcare13222992
Markovič-Božič J, Gradišar M, Petovar M, Mušič P, Pirc N, Meyerson J, Tušak M, Lapoša A, Tušak M, Spindler-Vesel A. Influence of Hypnosis and Acupuncture on Perioperative Complications. Healthcare. 2025; 13(22):2992. https://doi.org/10.3390/healthcare13222992
Chicago/Turabian StyleMarkovič-Božič, Jasmina, Meta Gradišar, Mihela Petovar, Polona Mušič, Nina Pirc, Joseph Meyerson, Maks Tušak, Andrej Lapoša, Matej Tušak, and Alenka Spindler-Vesel. 2025. "Influence of Hypnosis and Acupuncture on Perioperative Complications" Healthcare 13, no. 22: 2992. https://doi.org/10.3390/healthcare13222992
APA StyleMarkovič-Božič, J., Gradišar, M., Petovar, M., Mušič, P., Pirc, N., Meyerson, J., Tušak, M., Lapoša, A., Tušak, M., & Spindler-Vesel, A. (2025). Influence of Hypnosis and Acupuncture on Perioperative Complications. Healthcare, 13(22), 2992. https://doi.org/10.3390/healthcare13222992







