Abstract
Objectives: Chronic dermatoses are extremely prevalent and can manifest in various forms across genders and ages. Faced with the symptoms experienced by these conditions and the patient’s perception of the disease and its manifestation, it often leads to isolation and difficulty in emotional regulation. All these symptoms are associated with low quality of life, resulting in depressive and anxious symptomatology. Methods: This systematic literature review aims to study psychosocial interventions with an impact on the treatment of patients with chronic dermatoses. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed, guiding a systematic search across PubMed, Google Scholar, and PsycNet databases. The considered studies reported the impact of interventions when applied to patients with chronic dermatoses. All the studies found were published in peer-reviewed journals. Results: The analysis revealed that interventions based on mindfulness, self-compassion, and self-help showed promise, with several studies reporting reductions in disease-related suffering and improvements in quality of life. However, the results were heterogeneous, with some interventions showing no significant benefit over control conditions for specific outcomes like anxiety or appearance-related distress. Conclusions: The development of research lines to enhance knowledge in this field will allow for significant improvements in therapeutic care for patients with chronic dermatoses, aiming to support professionals in the development of integrative therapeutic strategies for these patients in their clinical practice.
1. Introduction
Society is frequently exposed to live and virtual images that pose a threat to body image, images that are related to appearance and lead to a reduction in body satisfaction or a momentary decrease in evaluative attitude towards one’s own body or its parts. Another aspect can be defined as discomfort or apprehension about body parts falling short of culturally defined beauty standards. A positive body image does not imply the absence of a negative body image; it is a flexible, holistic, and protective construct that goes beyond mere appearance satisfaction to include respect, honor, love, and acceptance of the body, including its unique features that deviate from appearance ideals [1].
The skin, as the most visible organ, is central to body image and self-perception. However, many chronic skin conditions—such as psoriasis, atopic dermatitis, vitiligo, and chronic urticaria—can profoundly disrupt an individual’s relationship with their body [2]. Chronic dermatoses are extremely prevalent and, due to their visible nature, carry a significant psychosocial burden. The self-assessed implications by individuals with a skin condition are more strongly associated with psychological distress than the severity estimated by the physician, suggesting that individuals’ perceptions and emotions regarding their skin condition play a fundamental role in the development of related distress [3].
Broader surveys of conditions affecting appearance report findings where individuals with visible signs tend to experience above-average levels of psychological distress [4,5]. There is considerable individual variation in the psychosocial impact of an altered appearance, and mental health condition can therefore affect the burden, severity, and implications of physical conditions. This highlights the need for attention from healthcare professionals, especially those in the mental health field [3]. In fact, chronic dermatoses are conditions frequently associated with significant psychological impacts, including symptoms of anxiety, depression, and reduced quality of life, as evidenced in the literature emphasizes the importance of addressing these issues through integrated psychological interventions within the clinical management of such conditions, highlighting the need for multidisciplinary approaches that consider both the physical and psychological aspects of the disease [6].
This strong bidirectional link between psychological state and skin health is underpinned by well-characterized biological pathways. Psychological stress activates the hypothalamic–pituitary–adrenal (HPA) axis and the sympathetic nervous system (SNS), leading to the release of neuroendocrine mediators such as cortisol and catecholamines [7]. These substances can directly modulate immune function and promote inflammation, a key driver of many chronic dermatoses like psoriasis and atopic dermatitis [7]. Furthermore, stress can impair the skin’s barrier function and increase pruritus (itching), triggering a scratch-itch cycle that exacerbates lesions [8]. Therefore, psychological interventions that effectively reduce stress may not only alleviate psychological distress but also directly mitigate this neuroimmunocutaneous activity, potentially leading to disease modification.
Consequently, patients often experience symptoms such as shame, distress, frustration, lack of confidence, loss of self-esteem, and body image issues [9], which, combined with the patient’s perception of the illness and its manifestation, often leads to isolation, abandonment of activities, difficulties in relationships with others, and challenges in emotional regulation. In effect, all these symptoms are associated with elevated levels of low quality of life that generate depressive and anxiety-related symptoms [10].
In response to this complex biopsychosocial interplay, psychological interventions for the treatment of dermatoses have been developed, often based on principles of self-compassion, self-concept, and mindfulness, which are rooted in non-self-judgment and acceptance of inner experiences and physical sensations. Mindfulness-based therapies not only aim to increase body awareness and regulate suffering overall but also emphasize the fundamental role of self-compassion in the patient’s ability to be kind to oneself during moments of heightened distress [11]. In addition to these interventions, expressive writing based on self-compassion aims to stimulate self-compassion to improve body image, especially in situations of failure, humiliation, and feelings of loss. This approach seeks to prevent negative thoughts about oneself and one’s body [12]. This intervention has shown promise in other visible conditions; for example, in a study conducted by [13], when applied, expressive writing based on self-compassion in the post-cancer process, there was an observed increase in self-compassion, demonstrating an improvement in distress. The aim of this systematic literature review is to investigate the efficacy of these and other psychological interventions for patients with chronic dermatoses. Based on the existing literature, we expect to find that interventions focusing on mindfulness and self-compassion will be particularly effective in reducing psychological distress and improving quality of life in this patient population.
2. Materials and Methods
2.1. Search Strategy
This review was conducted by PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines (PRISMA check list are available in the Supplementary Materials—Table S1) and registered on the International Prospective Register of Systematic Reviews (PROSPERO) under the registration number 1170236. The databases selected were PubMed, Google Scholar and PsycNet. The keywords used were: “dermatoses”, “skin diseases”, “psychological intervention”, “self-compassion “, “body image”, “atopic dermatitis” and “psoriasis”. Some studies were obtained through the references of others. All the authors were actively involved in all stages of the review process.
The core search criteria, including the key concepts, search terms, and Boolean operators used, are detailed in Table 1. The search strategy was adapted for the specific syntax of each database.

Table 1.
Research strategy.
2.2. Inclusion Criteria
The titles and abstracts of the studies were evaluated and selected for inclusion following specific criteria: (a) complete studies (without protocols); (b) studies correlating dermatoses and psychological interventions; (c) involving specific interventions and their psychological and psychosocial outcomes; and (d) studies published in peer-reviewed journals. The articles considered are in English and Portuguese.
2.3. Exclusion Criteria
Studies were excluded if they focused only on dermatoses and excluded psychological interventions, or if they addressed only the dermatological or pharmacological aspects themselves and did not establish an association with the psychological dimensions. Studies that addressed interventions with the family were also excluded, as were case reports and studies that did not describe the results of the intervention and had a small sample size (<10 participants).
2.4. Screening
The title/summary of the studies was selected independently, always based on the inclusion and exclusion criteria.
2.5. Quality Assessment
The methodological quality and risk of bias of the included studies were critically appraised using the appropriate Joanna Briggs Institute (JBI) checklists for study design (2024) [14]. The appraisal was conducted independently by the review authors, with any discrepancies resolved through consensus. The results of this assessment are summarized in Table 2, Table 3, Table 4, Table 5 and Table 6. The overall risk of bias for each study, as determined by this appraisal, was considered when interpreting the results and drawing conclusions in this review.

Table 2.
Randomized Controlled Trials.
Table 2.
Randomized Controlled Trials.
| Authors | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 | % Yes | Risk of Bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (Adkins, 2021) [15] | Y | U | Y | U | NA | Y | Y | N | Y | Y | Y | Y | Y | 69.2 | Moderate |
| (Kelly et al., 2009) [16] | Y | U | Y | N | NA | NA | Y | Y | Y | Y | Y | Y | Y | 69.2 | Moderate |
| (D’Alton et al., 2019b) [17] | Y | U | N | N | U | U | Y | Y | U | Y | Y | Y | Y | 53.8 | Moderate |
| (Singh et al., 2017) [18] | Y | U | U | N | U | U | Y | Y | Y | Y | Y | Y | Y | 61.5 | Moderate |
| (Larsen et al., 2014b) [19] | Y | U | U | N | U | U | Y | Y | U | Y | Y | Y | Y | 53.8 | Moderate |
| (Kishimoto et al., 2023) [20] | Y | Y | Y | N | N | Y | Y | Y | Y | Y | Y | Y | Y | 84.6 | Low |
| (Hudson et al., 2020) [21] | Y | U | U | N | N | U | Y | N | Y | Y | Y | Y | Y | 53.8 | Moderate |
| (Mifsud et al., 2021b) [22] | Y | Y | Y | Y | NA | Y | Y | Y | Y | Y | Y | Y | Y | 92.3 | Low |
| (Muftin et al., 2022) [23] | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | 92.3 | Low |
| (Łakuta, 2022) [24] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 100 | Low |
| (Seekis et al., 2017b) [1] | Y | U | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | 84.6 | Low |
| (Sengupta et al., 2025) [25] | Y | U | U | N | N | U | Y | U | Y | Y | Y | Y | Y | 53.8 | Moderate |
| (Sherman et al., 2019) [26] | Y | U | Y | Y | NA | NA | Y | Y | Y | Y | Y | Y | Y | 76.9 | Low |
| (Borimnejad et al., 2015) [27] | Y | U | Y | N | N | Y | Y | Y | Y | Y | Y | Y | Y | 76.9 | Low |
| (Bundy et al., 2013) [28] | Y | U | Y | U | NA | NA | Y | Y | Y | Y | Y | Y | Y | 69.2 | Moderate |
| (Pascual-Sánchez et al., 2020) [29] | Y | U | Y | N | NA | U | Y | NA | Y | Y | Y | Y | Y | 61.5 | Moderate |
Note. 1. Was true randomization used for assignment of participants to treatment groups? 2. Was allocation to treatment groups concealed? 3. Were treatment groups similar at the baseline? 4. Were participants blind to treatment assignment? 5. Were those delivering treatment blind to treatment assignment? 6. Were outcomes assessors blind to treatment assignment? 7. Were treatment groups treated identically other than the intervention of interest? 8. Was follow-up complete and if not, were differences between groups in terms of their follow-up adequately described and analyzed? 9. Were participants analyzed in the groups to which they were randomized? 10. Were outcomes measured in the same way for treatment groups? 11. Were outcomes measured in a reliable way? 12. Was appropriate statistical analysis used? 13. Was the trial design appropriate, and any deviations from the standard RCT design (individual randomization, parallel groups) accounted for in the conduct and analysis of the trial?; U = Unclear; Y = Yes; N = No; NA = Not applicable.

Table 3.
Quasi-Experimental Studies.
Table 3.
Quasi-Experimental Studies.
| Authors | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | % Yes | Risk of Bias |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (Hedman-Lagerlöf et al., 2019) [30] | Y | N | NA | NA | Y | Y | U | Y | Y | 55 | Moderate |
| (Offenbächer et al., 2021) [31] | Y | N | NA | NA | Y | Y | Y | Y | Y | 66.6 | Moderate |
| (Harfensteller, 2022) [32] | Y | N | NA | NA | Y | Y | Y | Y | Y | 66.6 | Moderate |
| (Ridge et al., 2021) [33] | Y | N | Y | Y | Y | Y | Y | NA | Y | 77.7 | Low |
| (Latifi et al., 2020) [34] | Y | Y | Y | Y | Y | Y | Y | Y | Y | 100 | Low |
| (Li et al., 2020) [35] | Y | Y | Y | Y | Y | Y | Y | U | Y | 88.8 | Low |
Note. 1. Is it clear in the study what the “cause” and the “effect” are (i.e., there is no confusion about which variable comes first)? 2. Was there a control group? 3. Were participants included in any comparisons similar? 4. Were the participants included in any comparisons receiving similar treatment/care, other than the exposure or intervention of interest? 5. Were there multiple measurements of the outcome, both pre and post the intervention/exposure? 6. Were the outcomes of participants included in any comparisons measured in the same way? 7. Were outcomes measured in a reliable way? 8. Was follow-up complete and if not, were differences between groups in terms of their follow-up adequately described and analyzed? 9. Was appropriate statistical analysis used?; U = Unclear; Y = Yes; N = No; NA = Not applicable.

Table 4.
Qualitative Research.
Table 4.
Qualitative Research.
| Authors | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | % Yes | Risk of Bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (Da Silva et al., 2011) [36] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 100 | Low |
| (Zucchelli et al., 2021) [37] | Y | Y | Y | Y | Y | Y | U | Y | Y | Y | 90 | Low |
Note. 1. Is there congruity between the stated philosophical perspective and the research methodology? 2. Is there congruity between the research methodology and the research question or objectives? 3. Is there congruity between the research methodology and the methods used to collect data? 4. Is there congruity between the research methodology and the representation and analysis of data? 5. Is there congruity between the research methodology and the interpretation of results? 6. Is there a statement locating the researcher culturally or theoretically? 7. Is the influence of the researcher on the research, and vice versa, addressed? 8. Are participants, and their voices, adequately represented? 9. Is the research ethical according to current criteria or, for recent studies, and is there evidence of ethical approval by an appropriate body? 10. Do the conclusions drawn in the research report flow from the analysis, or interpretation, of the data?; U = Unclear; Y = Yes.

Table 5.
Systematic Review.
Table 5.
Systematic Review.
| Authors | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | % Yes | Risk of Bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (Bartholomew et al., 2022) [38] | Y | Y | Y | U | U | Y | Y | Y | N | Y | Y | 72.7 | Moderate |
| (Rafidi et al., 2022) [39] | Y | Y | Y | Y | Y | U | U | Y | N | Y | Y | 72.7 | Moderate |
Note. 1. Is the review question clearly and explicitly stated? 2. Were the inclusion criteria appropriate for the review question? 3. Was the search strategy appropriate? 4. Were the sources and resources used to search for studies adequate? 5. Were the criteria for appraising studies appropriate? 6. Was critical appraisal conducted by two or more reviewers independently? 7. Were there methods to minimize errors in data extraction? 8. Were the methods used to combine studies appropriate? 9. Was the likelihood of publication bias assessed? 10. Were recommendations for policy and/or practice supported by the reported data? 11. Were the specific directives for new research appropriate?; U = Unclear; Y = Yes; N = No.

Table 6.
Textual Evidence: Expert Opinion.
Table 6.
Textual Evidence: Expert Opinion.
| Authors | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | % Yes | Risk of Bias |
|---|---|---|---|---|---|---|---|---|
| (Yosipovitch et al., 2024) [8] | Y | Y | Y | U | Y | Y | 83.3 | Low |
Note. 1. Is the source of the opinion clearly identified? 2. Does the source of the opinion have standing in the field of expertise? 3. Are the interests of the relevant population the central focus of the opinion? 4. Does the opinion demonstrate a logically defended argument to support the conclusions drawn? 5. Is there reference to the extant literature? 6. Is any incongruence with the literature/sources logically defended?; U = Unclear; Y = Yes.
3. Results
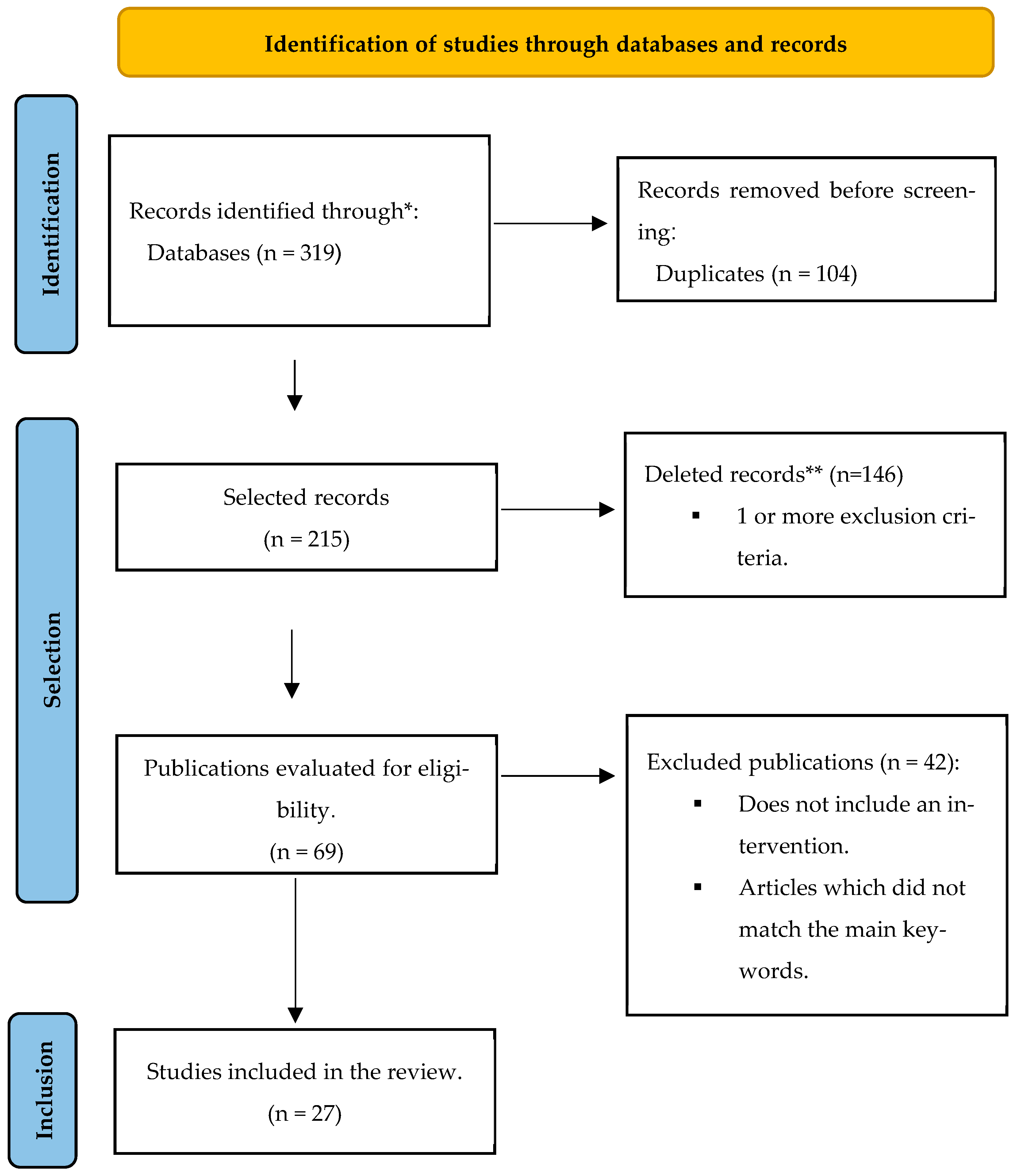
The initial searches in the databases yielded a total of 319 articles, of which 104 (32.60%) were removed due to duplication. The abstracts of the remaining 215 (67.39%) studies were analyzed, and 146 (45.77%) were excluded. Among the remaining 69 (21.63%) full-text articles, 42 (13.17%) were excluded, resulting in 27 (8.46%) articles for review (Figure 1).
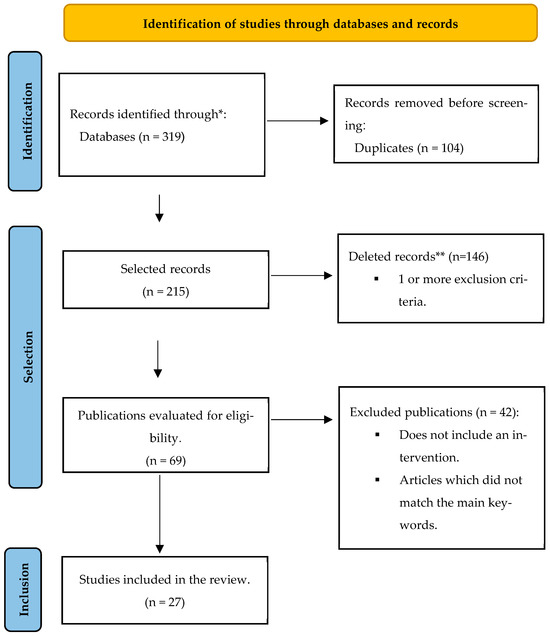
Figure 1.
PRISMA flow diagram comprising the different phases of this systematic review. * Refers to records identified through database searching (PubMed, Google Scholar, PsycNet). ** Records deleted for meeting one or more predefined exclusion criteria.
3.1. Studies’ Characteristics
The characteristics of the studies (n = 27) are presented in Table 7. Three studies (11.11%) included cancer survivors, twenty-three studies (85.19%) focused on patients with dermatological conditions, predominantly psoriasis, and one study (3.70%) addressed the role of negative body image in individuals with dermatoses. Of the 27 studies, four (14.81%) applied the intervention of expressive writing based on self-compassion, and nineteen (70.37%) applied interventions based on mindfulness therapy. Regarding methodology, twelve (44.44%) were randomized controlled trials, five (18.52%) randomized study, two (7.41%) were pilot studies, five (7.41%) were qualitative studies, one (3.70%) was a prospective study; one (3.70%) was a prospective cutting study, and one (3.70%) was an open trial.

Table 7.
Resume of the studies reviewed for this literature review.
3.2. Studies’ Results Summary
In the analysis of the tables (Table 8 and Table 9), we observe that the selected studies present a similar methodology, twelve (44.44%) were randomized controlled trials, five (18.52%) randomized study, two (7.41%) were pilot studies, five (7.41%) were qualitative studies, one (3.70%) was a prospective study; one (3.70%) was a prospective cutting study, and one (3.70%) was an open trial. As seen in Table 9, despite the variations in the instruments used to assess the effectiveness of interventions across different studies, they generally evaluated depression and anxiety [12,16,17,18,20,22,25,28,29,31,33,35], quality of life [17,18,20,23,24,25,28,29,31,35,38], self-compassion [12,20,22,26,27], and body appreciation [1,12,22,24,26,34]. The most studied variables included sociodemographic characteristics, with individuals diagnosed with chronic dermatoses, predominantly psoriasis and vitiligo (Table 8). The articles are grounded in aspects related to self-compassion, self-help, body image, and quality of life in patients with dermatoses. Most of the studies are classified as Q1 and Q2 metrics, indicating the significance and recognition of research on the subject.
The evidence for expressive writing was mixed. While a general writing intervention on body functionality showed no significant effects on appearance anxiety or skin-related quality of life [15,26], writing tasks specifically designed to cultivate self-compassion demonstrated more consistent benefits for body appreciation and satisfaction [1,15] compared to control conditions. These data can be explained by the fact that expressive writing based on self-compassion requires more awareness, greater self-reflection, and a stronger self-connection [32], as kindness and unconditional acceptance are also important for body acceptance. These results can be useful for clinical use since cultivating a self-compassionate attitude toward stressors can promote better coping and improve mood [32].
Mind–Body therapies (MBT) in atopic dermatitis (AD) demonstrated promising effects on both physical and psychological outcomes. Studies reported reductions in pruritus, scratching behaviors, and overall disease severity, alongside improvements in anxiety, stress, depressive symptoms, and quality of life. Interventions including mindfulness, cognitive–behavioral therapy, hypnotherapy, relaxation techniques, biofeedback, and therapeutic massage showed beneficial effects as adjuncts to conventional treatment [8]. Mindfulness and self-compassion–based interventions significantly reduced psychological distress in individuals with chronic skin conditions. Improvements were observed in depression, anxiety, stress, self-esteem, dermatology-related quality of life, and overall well-being. Mindfulness enhanced emotional regulation and reduced rumination, self-judgment, and experiential avoidance. Self-compassion promoted acceptance, self-kindness, and recognition of the universality of negative experiences. These findings suggest that such interventions may be effective as adjuncts in psychodermatological care [25,40].
In mindfulness-based interventions [3,17,25,31,32,33,38], a decrease in the severity of symptomatology, as well as emotional suffering caused by the physical effects of dermatoses, was observed. Improvements in stress, changes in depressive symptomatology (but not anxiety), and enhanced coping with the disease were also noted. The studies reported that mindfulness led to improvements in symptoms, coping mechanisms, a deeper understanding of emotions, increased awareness of impulses, and enhancements in positive psychological attributes. In another study comparing mindfulness-based interventions such as Mindfulness-Based Cognitive Therapy, Mindfulness-Based Self-Compassion Therapy, and self-help to usual treatment, despite the beneficial aspects of these interventions, they were not significant for psychological well-being. The evidence on meditation and mindfulness practices in psoriasis is promising, but still limited by the small number of RCTs and short follow-up periods. Most studies reported improvements in psoriasis severity measured by the saPASI, while only a few demonstrated significant effects on quality of life. These interventions may also address psychological comorbidities, such as anxiety, depression, and worry, providing additional benefits beyond physical symptom relief [38].
In two studies, Cognitive–Behavioral Therapy (CBT) was used; in one, exposure-based CBT involving mindfulness practice was employed [30], and in another, general CBT was applied to dermatosis [28]. In both studies, a reduction in anxiety and improvements in quality of life were observed, but there were no changes in the depressive component. In mindfulness-based CBT, quality of life underwent changes during the intervention, while in the study of general CBT applied to dermatosis, the results regarding quality of life were more significant. Perhaps this difference is due to the latter intervention having a greater focus on overall disease management rather than specifically targeting the treatment of suffering for psoriasis. In both studies, careful consideration is warranted when analyzing results due to the potentially limiting small sample size for interventions based on self-compassion and Mindfulness [20,22,26,27,34], various studies reported significant effects on stress, self-compassion, anxiety, and depression [21]. These interventions assisted in the acceptance of altered appearance [37], reduction in shame and skin complaints, and a greater reduction in depression was observed in individuals with higher levels of self-criticism [16]. In one study [31], with a similar intervention basis, an increase in anxiety and depression levels was reported; however, caution is advised due to the small sample size, which prevents definitive conclusions.
Finally, in a study where individual motivational interviewing was used [19], significant changes were observed in lifestyle and overall positive changes. However, this intervention is recommended as a potential complement to medical management and for patient education regarding the condition. In a self-affirmation intervention [24], despite significant results for depressive symptoms, anxiety, and well-being, no differences were observed in mental health. The conclusion reached was that self-affirmation is not a pathway to improving psychological functioning in patients with dermatoses.

Table 8.
Variables, analysis, and statistical methods used in the studies reviewed for this literature.
Table 8.
Variables, analysis, and statistical methods used in the studies reviewed for this literature.
| Reference | Analysis and Statistical Methods | Variables |
|---|---|---|
| (Adkins, 2021) [15] | ANCOVA; Cronbach’s alphas | Age; gender; ethnicity, educational; dermatological condition that affects their body image; language |
| (Ahmed et al., 2018) [9] | Independent t-tests | People with vitiligo; age (>18) |
| (Bartholomew et al., 2022) [38] | Qualitative synthesis | Type of intervention; psoriasis; Psoriasis Area and Severity Index; Dermatology Life Quality Index; Perceived stress |
| (Borimnejad et al., 2015) [27] | Student’s t-tests; | Age; diagnosis of vitiligo confirmed; ability to read and write |
| (Bundy et al., 2013) [28] | Analise of covariance (ANCOVA), intention-to treat (ITT), multiple imputation, multivariate logistic regression, Shapiro–Wilk test, Stata v12 | |
| (Clarke et al., 2020b) [3] | SPSS 26; multiple regression; bivariate correlations; independent t-tests | Dermatology patients; age; gender; ethnicity; employment status; marital status; education level |
| (D’Alton et al., 2019b) [17] | Not discriminated | Age; diagnosis of psoriasis; systemic medication for 6 months or more |
| (Da Silva et al., 2011) [36] | Not discriminated | People with psychodermatoses; age; gender |
| (Galhardo et al., 2022) [7] | SPSS, v. 27; Pearson’s correlation; hierarchical multiple linear regression; Durbin–Watson statistics; | People with a diagnosis of psoriasis; age; gender |
| (Harfensteller, 2022) [32] | Spearman’s correlation coefficient; SPSS IBM 26; t-tests; Cohen’s d; | Patients with diagnosed Atopic dermatitis (AD); age (18–65); language |
| (Hedman-Lagerlöf et al., 2019) [30] | STATA version 14.2; t-tests; | Age (18–65); adults with Atopic dermatitis; duration of AD for at least 6 months; language |
| (Hewitt et al., 2022) [41] | NVivo 12 Pro; | Age; self-diagnosed dermatological condition |
| (Hudson et al., 2020) [21] | Independent samples t-tests; chi square tests | Age (16); English-speaking; diagnosis of a skin condition; |
| (Hughes et al., 2023) [42] | Thematic analysis | 8–11 years of age; diagnosed with any skin condition and English-language speakers; eligible parents were 18 years of age or over; the child’s main caregiver |
| (Kelly et al., 2009) [16] | ANOVAs; | Age; facial acne; prescribed acne treatment perceived to be ineffective |
| (Kishimoto et al., 2023) [20] | Mixed model for repeated measures (MMRM), adjusting for age, sex, and baseline DLQI, to assess within- and between-group differences. Additional DLQI analyses included: (1) percentage of patients with >4-point improvement, (2) subgroup analysis by sex, age, and baseline DLQI, and (3) per-protocol comparisons. All analyses used SAS 9.4 with standard corrections | Age, sex, education, marital status, living situation, working situation Disease duration, dermatologic treatment |
| (Łakuta, 2022) [24] | Six linear mixed models (LMMs); PROCESS macro version 3.5.3; | Age; physician-diagnosed psoriasis |
| (Larsen et al., 2014b) [19] | SPSS version 19; t-tests; qui 2 statistics, or Mann–Whitney U tests; ANOVA; Cohen’s d; ANCOVAs; | Age; gender; educational level; health status; disease duration |
| (Latifi et al., 2020) [34] | Descriptive statistics (frequency, percentage, mean, and standard deviation) and inferential statistics (repeated-measures ANOVA and Kruskal–Wallis test) | Women with skin cancer; age; children; education. Checklist of physiological symptoms related to skin cancer: skin changes, unreasonable weight loss, bloating, change in the chest, abnormal bleeding, trouble with swallowing, blood in the stool, abdominal pain, depression, mouth infections, persistent and unspecified pain, changes in lymph nodes, fever, fatigue, persistent cough, and indigestion. Three scales (severe, partial, and never) to assess the symptoms, and patients reported changes and a lack of changes in their status. |
| (Li et al., 2020) [35] | SPSS Statistics for Windows, Version 17.0. Student’s t-tests and the chi-square tests; hospitalization length and patient satisfaction between the different groups. | Age, gender, mean time from diagnosis to treatment initiation, and family history of psoriasis |
| (Melissant et al., 2021b) [12] | SPSS version 26; Multiple regression model; Linear mixed; | Head and neck cancer (HNC) survivors |
| (Mifsud et al., 2021b) [22] | c2 tests of Independence; ANOVA; chi-square tests; Shapiro–Wilk’s; Levene’s Test of Homogeneity of Variance; SPSS version 23; | Age; gender; diagnosed with stage I to III breast cancer, ductal carcinoma in situ (DCIS) and/or lobular carcinoma in situ (LCIS); experienced at least one negative event related to the changes that have occurred to their body after breast cancer; language |
| (Muftin et al., 2022) [23] | SPSS Statistics; intention-to-treat (ITT); v2-tests; MANOVA; ANOVA; | Gender; age; ethnicity; education |
| (Offenbächer et al., 2021) [31] | SPSS; t-test; per-protocol analysis (PPA); | Age; diagnosis of AD; |
| (Pascual-Sánchez et al., 2020) [29] | IBM SPSS Statistics for Macintosh, Version 21.0; t-test for independent sample; Pearson correlation | Women with AAU; age; time of disease; number of received treatments |
| (Rafidi et al., 2022) [39] | Qualitative synthesis | Type of intervention; dermatologic disease; treatment outcomes |
| (Ridge et al., 2021) [33] | GraphPad Prism software; version 9.3.1. | Age; diagnosis of chronic urticaria |
| (Seekis et al., 2017b) [1] | MANOVA; one-way ANOVA; | Age (17–25); language |
| (Sengupta et al., 2025) [25] | SPSS version 27; ANCOVAs | Age; Depression; Anxiety; Stress; Dermatology-specific quality of life; Self-esteem; Well-being |
| (Sherman et al., 2019) [26] | SPSS version 25.0; Chi-square; t-test; R statistics software version 4.5.2; ANCOVAs | Age, gender, education level, skin condition type, time since skin condition onset; whether treatment was received for the skin condition |
| (Singh et al., 2017) [18] | SPSS version 18; Wilcoxon signed-rank test | Age (>15); moderate and severe chronic plaque psoriasis |
| (Yosipovitch et al., 2024) [8] | Focused literature review of mind–body therapies | Pruritus/itch; pain; stress; sleep disturbances; anxiety; depressive symptoms; dermatology-specific quality of life; scratching behavior |
| (Zucchelli et al., 2021) [37] | NVivo© version 15.3.0 software; | Age; gender; participants with a range of appearance-affecting conditions; language |

Table 9.
Instruments used in the studies reviewed for this review.
Table 9.
Instruments used in the studies reviewed for this review.
| Reference | Instruments |
|---|---|
| (Borimnejad et al., 2015) [27] | General Health Questionnaire-28 (GHQ-28); |
| (Bundy et al., 2013) [28] | Hospital Anxiety Depression Scale (HADS) Self-Administered Psoriasis Area and Severity Index (SAPASI) Dermatology Life Quality Index (DLQI) Illness Perception Questionnaire |
| (D’Alton et al., 2019b) [17] | The Hospital Anxiety and Depression Scale (HADS); The Penn State Worry Questionnaire (PSWQ); The Five Facet Mindfulness Questionnaire (FFMQ); The Fears of Compassion Scales (FCS); The World Health Organization Quality of Life-BREF (WHOQOLBREF); The Dermatology Life Quality Index (DLQI); The Psoriasis Area and Severity Index (PASI); |
| (Kelly et al., 2009) [16] | Depressive Experiences Questionnaire (DEQ); The Beck Depression Inventory (BDI); Experiences of Shame Scale (ESS); SKINDEX-16; |
| (Kishimoto et al., 2023) [20] | Dermatology Life Quality Index—Japanese version (DLQI-J) Patient-Oriented Eczema Measure (POEM) Japanese version Evaluation of itching Self-Compassion Scale—Japanese version SCS-J Japanese version of the Freiburg Mindfulness Inventory (FMI) Hospital anxiety and depression scale (HADS)—Japanese version Japanese version of the Internalized Shame Scale (Japanese version of the ISS) Dermatological treatment adherence Home practice record |
| (Łakuta, 2022) [24] | Health Questionnaire [PHQ-9]; Mental Health Continuum—Short Form [MHCSF]; Self-Affirming Implementation Intention (S-AII); Body-Related Self-Affirming Implementation Intention (BS-AII); |
| (Larsen et al., 2014b) [19] | Self-Administered Psoriasis Area and Severity Index (SAPASI); Self-management measured (heiQ); The Psoriasis Knowledge Questionnaire (PKQ); The Brief Illness Perception Questionnaire (BIPQ); |
| (Latifi et al., 2020) [34] | Self-compassion scale (SCS) Body Image Concern Inventory (BICI) |
| (Li et al., 2020) [35] | Symptom Checklist-90 (SCL-90) Self-Rating Depression Scale (SDS) Self-Rating Anxiety Scale (SAS) The Generic Quality of Life Inventory (GQOLI) |
| (Melissant et al., 2021b) [12] | Body Image Scale (BIS); Body Appreciation Scale (BAS-2); Self-Compassion Scale—Short Form (SCS-SF); Hospital Anxiety and Depression Scale (HADS), (HADS-A), (HADS-D); Female Sexual Function Index (FSFI-6); International Index of Erectile Function (IIEF-5); |
| (Mifsud et al., 2021b) [22] | Body Image Scale (BIS: [43]); The Body Appreciation Scale; Self-compassionate attitude (SCA); Self-Compassion Scale—Short Form (SCS-SF); Positive and Negative Affect Schedule (PANAS); Short form of the Depression, Anxiety and Stress Scale (DASS21); |
| (Muftin et al., 2022) [23] | Other as Shamer Scale (OAS); The Forms of Self-Criticizing/Attacking & Self-Reassuring Scale (FSCRS); The Dermatology Life Quality Index (DLQI); |
| (Offenbächer et al., 2021) [31] | Score of Atopic Dermatitis (SCORAD); Patient Oriented Eczema Measure (POEM); Dermatology Life Quality Index (DLQI); Hospital Anxiety and Depression Scale (HADS); Perceived Stress Questionnaire (PSQ); Freiburger Mindfulness Inventory (FMI); Mindful Attention Awareness Scale (MAAS); Global Transition Items; |
| (Pascual-Sánchez et al., 2020) [29] | Dermatology Life Quality Index—DLQI Beck Depression Inventory—BDI State-trait Anxiety Inventory—STAI Rosenberg Self-esteem Scale—RSES Toronto Alexithymia Scale—TAS-20 |
| (Ridge et al., 2021) [33] | Depression and Anxiety Stress Scale (DASS 21); the Five Facets of Mindfulness Questionnaire (FFMQ); Urticaria Control Test; PERMA profiler; |
| (Seekis et al., 2017b) [1] | State Body Appreciation Scale-2 (SBAS-2); Body Image States Scale (BISS); |
| (Sengupta et al., 2025) [25] | Dermatology Life Quality Index (DLQI) Rosenberg Self-Esteem Scale (RSES) World Health Organization Well-Being Index (WHO-5) Depression, Anxiety, and Stress Scale (DASS-21) |
| (Sherman et al., 2019) [26] | Self-Compassion Scale—Short Form (SCS-SF); Positive and Negative Affect Schedule (PANAS); Body Image Disturbance Questionnaire; |
| (Singh et al., 2017) [18] | Psoriasis Area Severity Index (PASI); Dermatology Life Quality Index (DLQI); WHO-5 well-being index (WHO-5); Patient health questionnaire (PHQ); Generalized anxiety disorder (GAD)-7; |
| (Zucchelli et al., 2021) [37] | Not discriminated |
4. Discussion
The objective of this literature review is to investigate psychological interventions for the treatment of chronic dermatoses. Chronic dermatoses, especially psoriasis and vitiligo, have a significant impact on an individual’s life, leading to depression, anxiety, an increased risk of suicide, experiences of stigma, tendencies towards isolation, and negative body image [44]. All these factors can affect the individual’s quality of life [45] and may pose a risk of psychiatric morbidity [9]. The difficulties faced by individuals with dermatoses regarding their self-image and social life are mentioned [46]. In this sense, psychological intervention is essential.
Among the interventions used in different articles, expressive writing-based intervention has the potential to promote a positive body image and increase self-compassion. Interventions based on Mindfulness, self-compassion, and self-help demonstrate greater efficacy in the treatment of chronic dermatoses and can be a complementary tool for intervention [47]. They are promising in addressing the psychological stress generated by the effects of chronic dermatoses on the skin, mitigating negative thoughts about body image, reducing feelings of shame, skin complaints, depression, and self-criticism, and improving quality of life levels [48]. These interventions were also reported with higher participant satisfaction. While interventions based on Cognitive–Behavioral Therapy (CBT) show positive results, their practice is general and non-specific, demonstrating significant effects only when applied in conjunction with mindfulness practices.
The success of mindfulness-based and self-compassion interventions in reducing disease-related suffering and improving quality of life can be understood within the context of the neuroimmunocutaneous framework discussed in the introduction. By fostering a non-judgmental awareness of thoughts and sensations (mindfulness) and cultivating self-kindness during distress (self-compassion), these techniques can downregulate the maladaptive stress response [49,50]. This psychophysiological shift likely leads to a reduction in pro-inflammatory signaling and a break in the stress-itch cycle [8,39]. Consequently, the observed benefits of these interventions may extend beyond the psychological realm, contributing to a direct, positive impact on disease activity—such as reducing flare-ups, severity of lesions, and pruritus—by modulating the very biological pathways that link the mind and the skin. This underscores the potential of psychosocial strategies as integral components of a treatment plan aimed at comprehensive disease management.
A critical appraisal of the evidence base reveals several recurrent limitations within the included studies, which consequently inform the constraints of the present review. The primary literature is frequently characterized by modest sample sizes and notable attrition rates, which challenge the statistical power and generalizability of the findings. Furthermore, the context of participant recruitment introduces potential bias; for instance, individuals recruited in clinical settings may present with lower symptom severity and demonstrate reduced post-treatment improvement, suggesting that interventions might yield different effects for those experiencing higher levels of distress. The interpretability of results is also complicated by confounding variables, such as the concurrent use of antidepressant medication and the fluctuating nature of dermatoses, where the level of disease exacerbation at the time of assessment can significantly influence outcomes. An additional methodological concern across studies is the predominant reliance on self-report measures for psychological outcomes, which inherently carries the potential for bias. These inherent limitations in the primary literature directly shape the constraints of this review. While conducted according to PRISMA guidelines, the present synthesis was limited by its search strategy, being restricted to three databases and including only English and Portuguese publications, which may have led to the omission of pertinent research. The significant heterogeneity observed in the interventions, methodological designs (ranging from RCTs to qualitative studies), and outcome measures precluded a quantitative meta-analysis, thereby limiting the ability to draw definitive conclusions regarding efficacy. Finally, the broad focus on chronic dermatoses as a whole means the findings may not be uniformly applicable to each specific condition. Collectively, these factors underscore that the conclusions drawn here, while promising, should be viewed as indicative of a rapidly evolving field rather than as definitive evidence.
Considering the objective of this study, the analysis of the articles easily reveals the understanding and knowledge that experts have regarding the physical, psychological, and social impact of chronic dermatoses on an individual’s life. However, the therapists’ knowledge for assisting these patients is limited when it comes to determining the most suitable intervention. Despite the promising results observed in the studies, it would be important to develop more objective research with conclusive outcomes to enable better adaptation to the characteristics of the patient, as well as the use of feasible interventions.
The purpose of this literature review was to clarify which interventions demonstrate effectiveness in the treatment of patients with chronic dermatoses, with the aim of increasing knowledge in this field.
In future research, it would be important to conduct comparative studies between different psychological interventions to determine relative effectiveness, patient acceptability, and long-term outcomes. Evaluating the effectiveness of different intervention formats, such as in-person sessions, online videos, and remote interventions, is crucial to understanding the feasibility and efficacy of these approaches in different contexts and populations. Given the limited sample sizes and high dropout rates, it would be important to investigate factors influencing patient acceptance and participation in psychological interventions, considering barriers such as stigma, accessibility, and individual preferences. Finally, delving deeper into the relationship between improvements in dermatoses severity measures and the reduction in psychological distress would be a valuable avenue for exploration. Furthermore, the emergence of telehealth and digital health platforms presents a transformative prospect for expanding the reach and accessibility of psychological interventions. Future research should rigorously evaluate the efficacy and long-term adherence of interventions delivered remotely via videoconferencing, mobile applications, and structured online programs. Investigating how these digital formats compare to traditional in-person therapy in terms of clinical outcomes, patient engagement, and economic feasibility will be crucial. Embracing telemedicine could ultimately help overcome barriers such as geographic limitations, mobility issues, and stigma, making integrative psychodermatological care available to a broader and more diverse patient population.
5. Conclusions
The psychological impact of chronic dermatoses is well-documented in the literature, significantly affecting patients’ self-esteem, body image, and overall quality of life. In this context, psychological interventions that address not only the physical symptoms but also the emotional and social consequences of skin disorders are essential.
The evidence reviewed in this study suggests that therapeutic approaches based on mindfulness, self-compassion, and self-help are promising but heterogeneous. While they show potential for managing psychological distress and improving quality of life in patients with chronic dermatoses, their effectiveness varies across specific outcomes, conditions, and intervention formats. Future research should aim to identify the most effective components of these interventions and the patient populations most likely to benefit. Additionally, expressive writing interventions focused on self-compassion have shown potential in promoting body image acceptance and reducing self-critical thoughts.
In summary, this review contributes to the growing body of knowledge on psychological interventions for chronic dermatoses and underscores the importance of an interdisciplinary approach that integrates both physical and psychological aspects in the care of dermatological patients.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/healthcare13222947/s1, Table S1: PRISMA 2020 Checklist.
Author Contributions
Conceptualization, A.T. and V.A.; methodology, A.T., V.A., R.R. and A.V.; formal analysis, Â.L., A.T. and V.A.; investigation, A.T., V.A., Â.L. and Â.F.; data curation, A.T., Â.L. and Â.F.; writing—original draft preparation, R.R., A.V. and Â.L.; writing—review and editing, A.T., Â.L. and Â.F.; supervision, Â.L., A.T. and V.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The original contributions presented in this study are included in the article/Supplementary Materials. Further inquiries can be directed to the corresponding authors.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviation
| CBT | Cognitive–Behavioral Therapy |
References
- Seekis, V.; Bradley, G.L.; Duffy, A. The effectiveness of self-compassion and self-esteem writing tasks in reducing body image concerns. Body Image 2017, 23, 206–213. [Google Scholar] [CrossRef]
- Ücker Calvetti, P.; Rivas, R.; Coser, J.; Barbosa, A.; Ramos, D. Biopsychosocial aspects and quality of life of people with chronic dermatoses. Psicol. Saúde Doença 2017, 18, 297–307. [Google Scholar] [CrossRef]
- Clarke, E.N.; Thompson, A.R.; Norman, P. Depression in people with skin conditions: The effects of disgust and self-compassion. Br. J. Health Psychol. 2020, 25, 540–557. [Google Scholar] [CrossRef]
- Rumsey, N.; Harcourt, D. Body image and disfigurement: Issues and interventions. Body Image 2004, 1, 83–97. [Google Scholar] [CrossRef] [PubMed]
- Thompson, A.; Kent, G. Adjusting to disfigurement: Processes involved in dealing with being visibly different. Clin. Psychol. Rev. 2001, 21, 663–682. [Google Scholar] [CrossRef] [PubMed]
- Misery, L.; Schut, C.; Balieva, F.; Bobko, S.; Reich, A.; Sampogna, F.; Altunay, I.; Dalgard, F.; Gieler, U.; Kupfer, J.; et al. White paper on psychodermatology in Europe: A position paper from the EADV Psychodermatology Task Force and the European Society for Dermatology and Psychiatry (ESDaP). J. Eur. Acad. Dermatol. Venereol. 2023, 37, 2419–2427. [Google Scholar] [CrossRef]
- Chen, Y.; Lyga, J. Brain-skin connection: Stress, inflammation and skin aging. Inflamm. Allergy-Drug Targets 2014, 13, 177–190. [Google Scholar] [CrossRef]
- Yosipovitch, G.; Bernhard, J.D. Chronic pruritus. N. Engl. J. Med. 2013, 368, 1625–1634. [Google Scholar] [CrossRef]
- Ahmed, A.; Steed, L.; Burden-Teh, E.; Shah, R.; Sanyal, S.; Tour, S.; Dowey, S.; Whitton, M.; Batchelor, J.M.; Bewley, A.P. Identifying key components for a psychological intervention for people with vitiligo—A quantitative and qualitative study in the United Kingdom using web-based questionnaires of people with vitiligo and healthcare professionals. J. Eur. Acad. Dermatol. Venereol. 2018, 32, 2275–2283. [Google Scholar] [CrossRef]
- Galhardo, A.; Mendes, R.; Massano-Cardoso, I.; Cunha, M. Processos relacionados com a regulação emocional e vergonha e sua associação com os sintomas de depressão, ansiedade e stresse em pessoas com psoríase. Psychologica 2022, 65, e065004. [Google Scholar] [CrossRef]
- Berry, M.P.; Lutz, J.; Schuman-Olivier, Z.; Germer, C.; Pollak, S.; Edwards, R.R.; Gardiner, P.; Desbordes, G.; Napadow, V. Brief Self-Compassion Training Alters Neural Responses to Evoked Pain for Chronic Low Back Pain: A Pilot Study. Pain Med. 2020, 21, 2172–2185. [Google Scholar] [CrossRef] [PubMed]
- Melissant, H.C.; Jansen, F.; Eerenstein, S.E.J.; Cuijpers, P.; Lissenberg-Witte, B.I.; Sherman, K.A.; Laan, E.T.M.; Leemans, C.R.; Verdonck-de Leeuw, I.M. A structured expressive writing activity targeting body image-related distress among head and neck cancer survivors: Who do we reach and what are the effects? Support. Care Cancer 2021, 29, 5763–5776. [Google Scholar] [CrossRef]
- Sherman, K.A.; Przezdziecki, A.; Alcorso, J.; Kilby, C.J.; Elder, E.; Boyages, J.; Koelmeyer, L.; Mackie, H. Reducing Body Image–Related Distress in Women with Breast Cancer Using a Structured Online Writing Exercise: Results from the My Changed Body Randomized Controlled Trial. J. Clin. Oncol. 2018, 36, 1930–1940. [Google Scholar] [CrossRef]
- Joanna Briggs Institute. JBI Critical Appraisal Tools: Checklists for Assessing the Trustworthiness, Relevance and Results of Published Papers. 2024. Available online: https://jbi.global/critical-appraisal-tools (accessed on 2 March 2024).
- Adkins, K.V.; Overton, P.G.; Thompson, A.R. A brief online writing intervention improves positive body image in adults living with dermatological conditions. Front. Med. 2022, 9, 1064012. [Google Scholar] [CrossRef] [PubMed]
- Kelly, A.C.; Zuroff, D.C.; Shapira, L.B. Soothing Oneself and Resisting Self-Attacks: The Treatment of Two Intrapersonal Deficits in Depression Vulnerability. Cogn. Ther. Res. 2009, 33, 301–313. [Google Scholar] [CrossRef]
- D’Alton, P.; Kinsella, L.; Walsh, O.; Sweeney, C.; Timoney, I.; Lynch, M.; O’Connor, M.; Kirby, B. Mindfulness-Based Interventions for Psoriasis: A Randomized Controlled Trial. Mindfulness 2019, 10, 288–300. [Google Scholar] [CrossRef]
- Singh, S.M.; Narang, T.; Vinay, K.; Sharma, A.; Satapathy, A.; Handa, S.; Dogra, S. Clinic-based group multi-professional education causes significant decline in psoriasis severity: A randomized open label pilot study. Ind. Dermatol. Online J. 2017, 8, 454–459. [Google Scholar] [CrossRef]
- Larsen, M.H.; Krogstad, A.L.; Aas, E.; Moum, T.; Wahl, A.K. A telephone-based motivational interviewing intervention has positive effects on psoriasis severity and self-management: A randomized controlled trial. Br. J. Dermatol. 2014, 171, 1458–1469. [Google Scholar] [CrossRef] [PubMed]
- Kishimoto, S.; Watanabe, N.; Yamamoto, Y.; Imai, T.; Aida, R.; Germer, C.; Tamagawa-Mineoka, R.; Shimizu, R.; Hickman, S.; Nakayama, Y.; et al. Efficacy of integrated online mindfulness and self-compassion training for adults with atopic dermatitis: A randomized clinical trial. JAMA Dermatol. 2023, 159, 628–636. [Google Scholar] [CrossRef]
- Hudson, M.P.; Thompson, A.R.; Emerson, L.-M. Compassion-focused self-help for psychological distress associated with skin conditions: A randomized feasibility trial. Psychol. Health 2020, 35, 1095–1114. [Google Scholar] [CrossRef]
- Mifsud, A.; Pehlivan, M.J.; Fam, P.; O’Grady, M.; van Steensel, A.; Elder, E.; Gilchrist, J.; Sherman, K.A. Feasibility and pilot study of a brief self-compassion intervention addressing body image distress in breast cancer survivors. Health Psychol. Behav. Med. 2021, 9, 498–526. [Google Scholar] [CrossRef]
- Muftin, Z.; Gilbert, P.; Thompson, A.R. A randomized controlled feasibility trial of online compassion—focused self-help for psoriasis. Br. J. Dermatol. 2022, 186, 955–962. [Google Scholar] [CrossRef]
- Łakuta, P. A Factorial Randomized Controlled Trial of Implementation-Intention-Based Self-Affirmation Interventions: Findings on Depression, Anxiety, and Well-being in Adults with Psoriasis. Front. Psychiatry 2022, 13, 795055. [Google Scholar] [CrossRef]
- Sengupta, A.; Wagani, R. Mindful self-compassion for psychological distress associated with skin conditions: An online intervention study. Ind. J. Dermatol. Venereol. Leprol. 2024, 91, 71–75. [Google Scholar] [CrossRef]
- Sherman, K.A.; Roper, T.; Kilby, C.J. Enhancing self-compassion in individuals with visible skin conditions: Randomised pilot of the ‘My Changed Body’ self-compassion writing intervention. Health Psychol. Behav. Med. 2019, 7, 62–77. [Google Scholar] [CrossRef]
- Borimnejad, L.; Firooz, A.; Mortazavi, H.; Aghazadeh, N.; Halaji, Z. The Effect of Expressive Writing on Psychological Distress in Patients with Vitiligo: A Randomized Clinical Trial. J. Client-Centered Nurs. Care 2015, 1, 3–8. [Google Scholar]
- Bundy, C.; Pinder, B.; Bucci, S.; Reeves, D.; Griffiths, C.E.M.; Tarrier, N. A novel, web-based, psychological intervention for people with psoriasis: The electronic Targeted Intervention for Psoriasis (eTIPs) study. Br. J. Dermatol. 2013, 169, 329–336. [Google Scholar] [CrossRef] [PubMed]
- Pascual-Sánchez, A.; Fernández-Martín, P.; Saceda-Corralo, D.; Vañó-Galván, S. Impact of psychological intervention in women with alopecia areata universalis: A pilot study. Actas Dermo-Sifiliogr. 2020, 111, 694–696. [Google Scholar] [CrossRef]
- Hedman-Lagerlöf, E.; Bergman, A.; Lindefors, N.; Bradley, M. Exposure-based cognitive behavior therapy for atopic dermatitis: An open trial. Cogn. Behav. Ther. 2019, 48, 300–310. [Google Scholar] [CrossRef] [PubMed]
- Offenbächer, M.; Seitlinger, M.; Münch, D.; Schnopp, C.; Darsow, U.; Harfensteller, J.; Schmid-Grendelmeier, P.; Ring, J.; Kohls, N. A Pilot Study of a Mindfulness-Based Stress Reduction Programme in Patients Suffering from Atopic Dermatitis. Psych 2021, 3, 663–672. [Google Scholar] [CrossRef]
- Harfensteller, J. An Open Trial on the Feasibility and Efficacy of a Mindfulness-Based Intervention with Psychoeducational Elements on Atopic Eczema and Chronic Itch. Psych 2022, 4, 160–172. [Google Scholar] [CrossRef]
- Ridge, K.; Conlon, N.; Hennessy, M.; Dunne, P.J. Feasibility assessment of an 8-week attention-based training programme in the management of chronic spontaneous urticaria. Pilot Feasibility Stud. 2021, 7, 103. [Google Scholar] [CrossRef]
- Latifi, Z.; Soltani, M.; Mousavi, S. Evaluation of the effectiveness of self-healing training on self-compassion, body image concern, and recovery process in patients with skin cancer. Complement. Ther. Clin. Pract. 2020, 40, 101180. [Google Scholar] [CrossRef]
- Li, X.; Liu, L.; Zhang, Y.; Li, L. Efficacy of psychological intervention for patients with psoriasis vulgaris: A prospective study. J. Int. Med. Res. 2020, 48, 0300060520961674. [Google Scholar] [CrossRef]
- Da Silva, A.; Castoldi, L.; Kijner, L. A pele expressando o afeto: Uma intervenção grupal com pacientes portadores de psicodermatoses. Contextos Clínicos 2011, 4, 53–63. [Google Scholar] [CrossRef][Green Version]
- Zucchelli, F.A.; Donnelly, O.; Sharratt, N.D.; Hooper, N.; Williamson, H.M. Patients’ Experiences of an Acceptance and Commitment Therapy-Based Approach for Psychosocial Difficulties Relating to an Appearance-Affecting Condition. Eur. J. Couns. Psychol. 2021, 9, 29–40. [Google Scholar] [CrossRef]
- Bartholomew, E.; Chung, M.; Yeroushalmi, S.; Hakimi, M.; Bhutani, T.; Liao, W. Mindfulness and meditation for psoriasis: A systematic review. Dermatol. Ther. 2022, 12, 2273–2283. [Google Scholar] [CrossRef] [PubMed]
- Rafidi, B.; Kondapi, K.; Beestrum, M.; Basra, S.; Lio, P. Psychological therapies and mind–body techniques in the management of dermatologic diseases: A systematic review. Am. J. Clin. Dermatol. 2022, 23, 755–773. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.T.; Jensen, C.G.; Khoury, L.; Deleuran, B.; Blom, E.S.; Breinholt, T.; Christensen, R.; Skov, L. Effectiveness of mind–body intervention for inflammatory conditions: Results from a 26-week randomized, non-blinded, parallel-group trial. J. Clin. Med. 2021, 10, 3107. [Google Scholar] [CrossRef]
- Hewitt, R.M.; Ploszajski, M.; Purcell, C.; Pattinson, R.; Jones, B.; Wren, G.H.; Hughes, O.; Ridd, M.J.; Thompson, A.R.; Bundy, C. A mixed methods systematic review of digital interventions to support the psychological health and well-being of people living with dermatological conditions. Front. Med. 2022, 9, 1024879. [Google Scholar] [CrossRef]
- Hughes, O.; Shelton, K.H.; Penny, H.; Thompson, A.R. Parent and child experience of skin conditions: Relevance for the provision of mindfulness-based interventions. Br. J. Dermatol. 2023, 188, 514–523. [Google Scholar] [CrossRef]
- Hopwood, P.; Fletcher, I.; Lee, A.; Al Ghazal, S. A body image scale for use with cancer patients. Eur. J. Cancer 2001, 37, 189–197. [Google Scholar] [CrossRef]
- Fried, R.G.; Gupta, M.A.; Gupta, A.K. Depression and skin disease. Dermatol. Clin. 2005, 23, 657–664. [Google Scholar] [CrossRef] [PubMed]
- Almeida, V.; Leite, Â.; Constante, D.; Correia, R.; Almeida, I.F.; Teixeira, M.; Vidal, D.G.; e Sousa, H.F.P.; Dinis, M.A.P.; Teixeira, A. The Mediator Role of Body Image-Related Cognitive Fusion in the Relationship between Disease Severity Perception, Acceptance and Psoriasis Disability. Behav. Sci. 2020, 10, 142. [Google Scholar] [CrossRef]
- Ziemer, K.S.; Lamphere, B.R.; Raque-Bogdan, T.L.; Schmidt, C.K. A randomized controlled study of writing interventions on college women’s positive body image. Mindfulness 2019, 10, 66–77. [Google Scholar] [CrossRef]
- Türk, K.E.; Yılmaz, M. The effect on quality of life and body image of mastectomy among breast cancer survivors. Eur. J. Breast Health 2018, 14, 205. [Google Scholar] [CrossRef] [PubMed]
- Birdi, G.; Cooke, R.; Knibb, R.C. Impact of atopic dermatitis on quality of life in adults: A systematic review and meta-analysis. Int. J. Dermatol. 2020, 59, e75–e91. [Google Scholar] [CrossRef]
- Black, D.S.; Slavich, G.M. Mindfulness meditation and the immune system: A systematic review of randomized controlled trials. Ann. N. Y. Acad. Sci. 2016, 1373, 13–24. [Google Scholar] [CrossRef]
- Dunn, T.J.; Dimolareva, M. The effect of mindfulness-based interventions on immunity-related biomarkers: A comprehensive meta-analysis of randomised controlled trials. Clin. Psychol. Rev. 2022, 92, 102124. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).