Movement-Based Mindfulness vs. Attention Control for Modifying Physiological Risk in Chronic Stroke: Evidence from a Feasibility Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Trial Design and Ethics
2.2. Participants
2.3. Inclusion and Exclusion Criteria
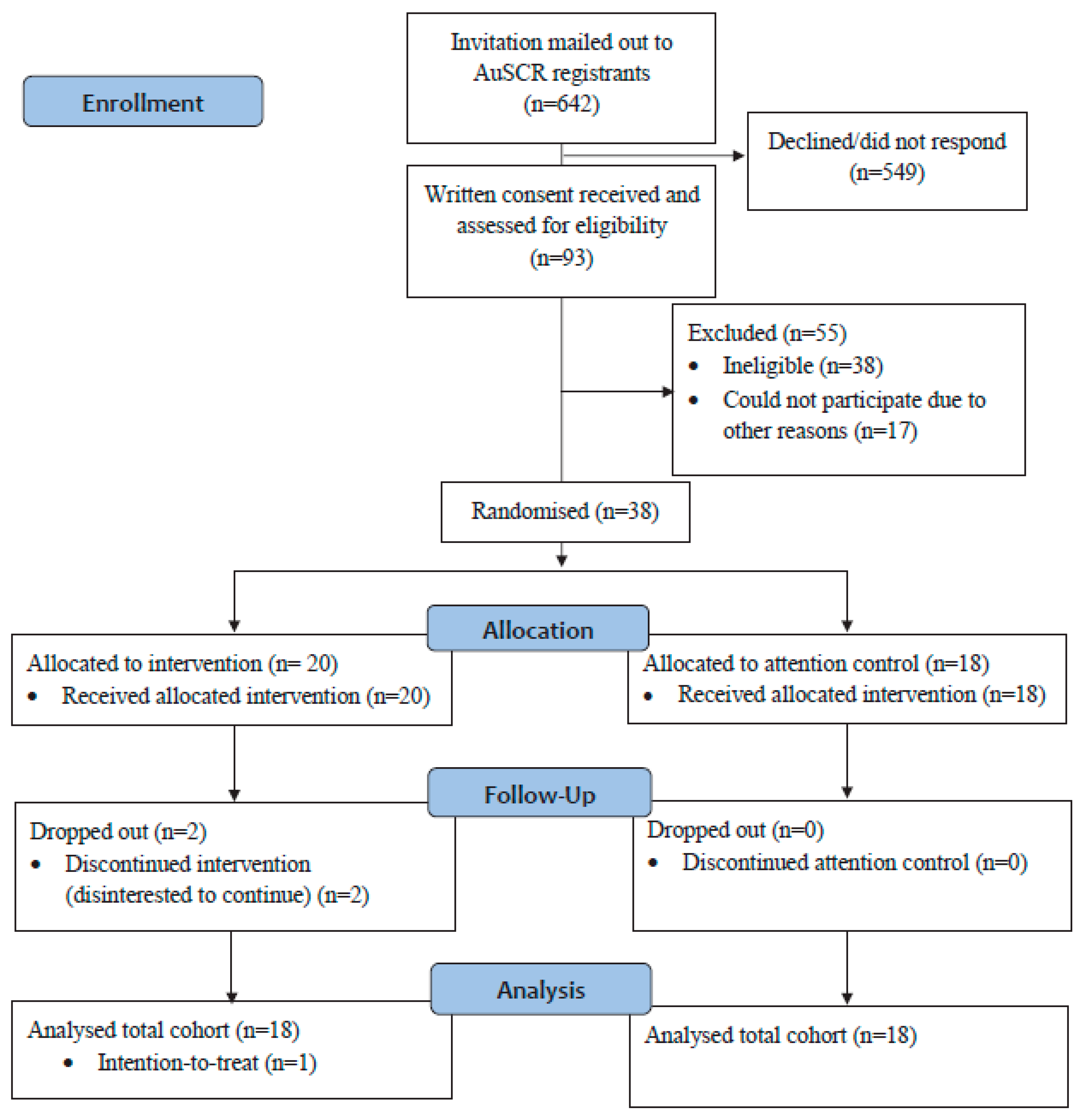
2.4. Recruitment and Informed Consent Process
2.5. Randomization
2.6. Intervention
2.7. Attention Control
2.8. Sub-Study Outcomes
2.9. Blood Pressure
2.10. Blood Lipids and Glycated Hemoglobin (HbA1c)
2.11. Stress
2.12. Sample Size
2.13. Statistical Analysis
3. Results
4. Discussion
4.1. Blood Pressure
4.2. Blood Lipids
4.3. Glycated Hemoglobin
4.4. Stress
4.5. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Glossary
| AuSCR | The Australian Stroke Clinical Registry |
| BMI | Body mass index |
| HbA1C | Glycated hemoglobin |
| HDL | High-density lipoprotein |
| ICMJE | International Committee of Medical Journal Editors |
| LDL | Low-density lipoprotein |
| MBI | Mindfulness-based intervention |
| MUHREC | Monash University Human Research Ethics Committee |
| PSS | Perceived Stress Scale |
| RCT | Randomized controlled trial |
| SMS | Short message service |
| TC | Total cholesterol |
| TG | Triglyceride |
References
- Deloitte Access Economics. The Economic Impact of Stroke in Australia; National Stroke Foundation: Melbourne, Australia, 2013. [Google Scholar]
- Flach, C.; Muruet, W.; Wolfe, C.D.A.; Bhalla, A.; Douiri, A. Risk and Secondary Prevention of Stroke Recurrence: A Population-Base Cohort Study. Stroke 2020, 51, 2435–2444. [Google Scholar] [CrossRef]
- Hankey, G.J. Secondary stroke prevention. Lancet Neurol. 2014, 13, 178–194. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, M.J.; Chin, S.L.; Rangarajan, S.; Xavier, D.; Liu, L.; Zhang, H.; Rao-Melacini, P.; Zhang, X.; Pais, P.; Agapay, S.; et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): A case-control study. Lancet 2016, 388, 761–775. [Google Scholar] [CrossRef] [PubMed]
- Mohan, K.M.; Wolfe, C.D.A.; Rudd, A.G.; Heuschmann, P.U.; Kolominsky-Rabas, P.L.; Grieve, A.P. Risk and Cumulative Risk of Stroke Recurrence. Stroke 2011, 42, 1489. [Google Scholar] [CrossRef]
- Walter, A.A.; Van Puymbroeck, M.; Bosch, P.; Schmid, A.A. Complementary and integrative health interventions in post-stroke rehabilitation: A systematic PRISMA review. Disabil. Rehabil. 2022, 44, 2223–2232. [Google Scholar] [CrossRef]
- Thayabaranathan, T.; Immink, M.A.; Stevens, P.; Hillier, S.; Thrift, A.G.; Brodtmann, A.; Carey, L.; Kilkenny, M.F.; Cadilhac, D.A. Understanding the potential for yoga and tai chi interventions to moderate risk factors for stroke—A scoping review. Future Neurol. 2018, 13, 239–252. [Google Scholar] [CrossRef]
- Hagins, M.; States, R.; Selfe, T.; Innes, K. Effectiveness of Yoga for Hypertension: Systematic Review and Meta-Analysis. Evid.-Based Complement. Altern. Med. 2013, 2013, 13. [Google Scholar] [CrossRef]
- McDermott, K.A.; Rao, M.R.; Nagarathna, R.; Murphy, E.J.; Burke, A.; Nagendra, R.H.; Hecht, F.M. A yoga intervention for type 2 diabetes risk reduction: A pilot randomized controlled trial. BMC Complement. Altern. Med. 2014, 14, 212. [Google Scholar] [CrossRef]
- Malinowski, P. Neural mechanisms of attentional control in mindfulness meditation. Front. Neurosci. 2013, 7, 35772. [Google Scholar] [CrossRef] [PubMed]
- Pascoe, M.C.; Thompson, D.R.; Ski, C.F. Yoga, mindfulness-based stress reduction and stress-related physiological measures: A meta-analysis. Psychoneuroendocrinology 2017, 86, 152–168. [Google Scholar] [CrossRef]
- Brenner, J.; LeBlang, S.; Lizotte-Waniewski, M.; Schmidt, B.; Espinosa, P.S.; DeMets, D.L.; Newberg, A.; Hennekens, C.H. Mindfulness with paced breathing reduces blood pressure. Med. Hypotheses 2020, 142, 109780. [Google Scholar] [CrossRef]
- Pal, A.; Srivastava, N.; Tiwari, S.; Verma, N.S.; Narain, V.S.; Agrawal, G.G.; Natu, S.M.; Kumar, K. Effect of yogic practices on lipid profile and body fat composition in patients of coronary artery disease. Complement. Ther. Med. 2011, 19, 122–127. [Google Scholar] [CrossRef]
- Manchanda, S.C.; Madan, K. Yoga and meditation in cardiovascular disease. Clin. Res. Cardiol. 2014, 103, 675–680. [Google Scholar] [CrossRef]
- Bhardwaj, P.; Kaur, N.; Malik, N.; Singh, G.; Pathania, M. Yoga and Mindfulness in the Prevention of Metabolic Diseases. In Neuroscience of Yoga: Theory and Practice: Part II; Anand, A., Ed.; Springer Nature Singapore: Singapore, 2024; pp. 1–24. [Google Scholar]
- Lawrence, M.; Booth, J.; Mercer, S.; Crawford, E. A Systematic Review of the Benefits of Mindfulness-Based Interventions following Transient Ischemic Attack and Stroke. Int. J. Stroke 2013, 8, 465–474. [Google Scholar] [CrossRef]
- Thayabaranathan, T.; Andrew, N.E.; Immink, M.A.; Hillier, S.; Stevens, P.; Stolwyk, R.; Kilkenny, M.; Cadilhac, D.A. Determining the potential benefits of yoga in chronic stroke care: A systematic review and meta-analysis. Top. Stroke Rehabil. 2017, 24, 279–287. [Google Scholar] [CrossRef]
- Abbott, R.A.; Whear, R.; Rodgers, L.R.; Bethel, A.; Thompson Coon, J.; Kuyken, W.; Stein, K.; Dickens, C. Effectiveness of mindfulness-based stress reduction and mindfulness based cognitive therapy in vascular disease: A systematic review and meta-analysis of randomised controlled trials. J. Psychosom. Res. 2014, 76, 341–351. [Google Scholar] [CrossRef]
- Priya, G.; Kalra, S. Mind-Body Interactions and Mindfulness Meditation in Diabetes. Eur. Endocrinol. 2018, 14, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Zhang, C.; Sun, M.; Zhang, D.; Luo, Y.; Liang, K.; Xu, T.; Pan, X.; Zheng, R.; Shangguan, F.; et al. Effectiveness of mindfulness training on pregnancy stress and the hypothalamic-pituitary-adrenal axis in women in China: A multicenter randomized controlled trial. Front. Psychol. 2023, 14, 1073494. [Google Scholar] [CrossRef]
- Lee, S.Y.; Gathright, E.C.; Wu, W.-C.; Salmoirago-Blotcher, E. Mindfulness-Based Interventions for Patients with Cardiovascular Disease: A Focused Review for Practicing Clinicians. Curr. Cardiol. Rep. 2023, 25, 185–191. [Google Scholar] [CrossRef] [PubMed]
- Immink, M.A.; Hillier, S.; Petkov, J. Randomised Controlled Trial of Yoga for Chronic Poststroke Hemiparesis: Motor Function, Mental Health, and Quality of Life Outcomes. Top. Stroke Rehabil. 2014, 21, 256–271. [Google Scholar] [CrossRef] [PubMed]
- Thayabaranathan, T.; Immink, M.A.; Hillier, S.; Stolwyk, R.; Andrew, N.E.; Stevens, P.; Kilkenny, M.F.; Gee, E.; Carey, L.; Brodtmann, A.; et al. Co-Designing a New Yoga-Based Mindfulness Intervention for Survivors of Stroke: A Formative Evaluation. Neurolology Int. 2021, 14, 1–10. [Google Scholar] [CrossRef]
- Hancock, S.; Thayabaranathan, T.; Stolwyk, R.; Cameron, J.; Immink, M.A.; Hillier, S.; Kilkenny, M.F.; Brodtmann, A.; Carey, L.M.; Olaiya, M.; et al. Anxiety, Depression, Fatigue, and Quality of Life Outcomes Following a Movement-Based Mindfulness or Social Group Program for Chronic Stroke: A Sub-Study of a Phase II Feasibility Randomised Controlled Trial. Mindfulness 2025, 16, 1612–1623. [Google Scholar] [CrossRef]
- Sandra, M.E.; Claire, L.C.; Michael, J.C.; Christine, M.B.; Sally, H.; Lehana, T.; Gillian, A.L. CONSORT 2010 statement: Extension to randomised pilot and feasibility trials. BMJ 2016, 355, i5239. [Google Scholar] [CrossRef]
- Orkin, A.M.; Gill, P.J.; Ghersi, D.; Campbell, L.; Sugarman, J.; Emsley, R.; Steg, P.G.; Weijer, C.; Simes, J.; Rombey, T.; et al. Guidelines for Reporting Trial Protocols and Completed Trials Modified Due to the COVID-19 Pandemic and Other Extenuating Circumstances: The CONSERVE 2021 Statement. JAMA 2021, 326, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Cadilhac, D.A.; Dalli, L.L.; Morrison, J.; Paice, K.; Carter, H.; Campbell, B.C.V.; Cloud, G.C.; Kilkenny, M.F.; Faux, S.; Hill, K.; et al. The Australian Stroke Clinical Registry Annual Report 2022; The Florey Institute of Neuroscience and Mental Health: Heidelberg, Australia, 2023; 72p. [Google Scholar] [CrossRef]
- Lannin, N.A.; Anderson, C.; Lim, J.; Paice, K.; Price, C.; Faux, S.; Levi, C.; Donnan, G.; Cadilhac, D. Telephone follow-up was more expensive but more efficient than postal in a national stroke registry. J. Clin. Epidemiol. 2013, 66, 896–902. [Google Scholar] [CrossRef] [PubMed]
- Gyawali, P.; Chow, W.Z.; Hinwood, M.; Kluge, M.; English, C.; Ong, L.K.; Nilsson, M.; Walker, F.R. Opposing Associations of Stress and Resilience With Functional Outcomes in Stroke Survivors in the Chronic Phase of Stroke: A Cross-Sectional Study. Front. Neurol. 2020, 11, 230. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Prather, J.G.; Stanfill, A.G. An Integrative Review of the Utilization of the Perceived Stress Scale in Stroke Recovery. J. Neurosci. Nurs. 2023, 55, 65–71. [Google Scholar] [CrossRef]
- Julious, S.A. Sample size of 12 per group rule of thumb for a pilot study. Pharm. Stat. 2005, 4, 287–291. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: London, UK, 1988. [Google Scholar] [CrossRef]
- Detry, M.A.; Ma, Y. Analyzing Repeated Measurements Using Mixed Models. JAMA 2016, 315, 407–408. [Google Scholar] [CrossRef]
- Lee, E.C.; Whitehead, A.L.; Jacques, R.M.; Julious, S.A. The statistical interpretation of pilot trials: Should significance thresholds be reconsidered? BMC Med. Res. Methodol. 2014, 14, 41. [Google Scholar] [CrossRef]
- Lancaster, G.A. Pilot and feasibility studies come of age! Pilot Feasibility Stud. 2015, 1, 1. [Google Scholar] [CrossRef]
- Kandzari, D.E.; Mahfoud, F.; Weber, M.A.; Townsend, R.; Parati, G.; Fisher, N.D.L.; Lobo, M.D.; Bloch, M.; Böhm, M.; Sharp, A.S.P.; et al. Clinical Trial Design Principles and Outcomes Definitions for Device-Based Therapies for Hypertension: A Consensus Document From the Hypertension Academic Research Consortium. Circulation 2022, 145, 847–863. [Google Scholar] [CrossRef]
- Intarakamhang, U.; Macaskill, A.; Prasittichok, P. Mindfulness interventions reduce blood pressure in patients with non-communicable diseases: A systematic review and meta-analysis. Heliyon 2020, 6, e03834. [Google Scholar] [CrossRef]
- Amarenco, P.; Labreuche, J. Lipid management in the prevention of stroke: Review and updated meta-analysis of statins for stroke prevention. Lancet Neurol. 2009, 8, 453–463. [Google Scholar] [CrossRef]
- Loucks, E.B.; Britton, W.B.; Howe, C.J.; Eaton, C.B.; Buka, S.L. Positive Associations of Dispositional Mindfulness with Cardiovascular Health: The New England Family Study. Int. J. Behav. Med. 2015, 22, 540–550. [Google Scholar] [CrossRef]
- Ismond, K.P.; Bukutu, C.; Vohra, S. Chapter 23—Mindfulness-Based Therapy and Heart Health. In Lifestyle in Heart Health and Disease; Watson, R.R., Zibadi, S., Eds.; Academic Press: Cambridge, MA, USA, 2018; pp. 275–283. [Google Scholar]
- Gentile, C.; Starnino, L.; Dupuis, G.; D’Antono, B. Mindfulness-Based Stress Reduction in Older Adults at Risk for Coronary Artery Disease: A Pilot Randomized Trial. Clin. Gerontol. 2022, 45, 272–286. [Google Scholar] [CrossRef] [PubMed]
- Chu, P.; Gotink, R.A.; Yeh, G.Y.; Goldie, S.J.; Hunink, M.G. The effectiveness of yoga in modifying risk factors for cardiovascular disease and metabolic syndrome: A systematic review and meta-analysis of randomized controlled trials. Eur. J. Prev. Cardiol. 2016, 23, 291–307. [Google Scholar] [CrossRef] [PubMed]
- Scott-Sheldon, L.A.J.; Gathright, E.C.; Donahue, M.L.; Balletto, B.; Feulner, M.M.; DeCosta, J.; Cruess, D.G.; Wing, R.R.; Carey, M.P.; Salmoirago-Blotcher, E. Mindfulness-Based Interventions for Adults with Cardiovascular Disease: A Systematic Review and Meta-Analysis. Ann. Behav. Med. 2020, 54, 67–73. [Google Scholar] [CrossRef]
- Sanogo, F.; Xu, K.; Cortessis, V.K.; Weigensberg, M.J.; Watanabe, R.M. Mind- and Body-Based Interventions Improve Glycemic Control in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis. J. Integr. Complement. Med. 2023, 29, 69–79. [Google Scholar] [CrossRef] [PubMed]
- Love, M.F.; Sharrief, A.; Chaoul, A.; Savitz, S.; Beauchamp, J.E.S. Mind-Body Interventions, Psychological Stressors, and Quality of Life in Stroke Survivors. Stroke 2019, 50, 434–440. [Google Scholar] [CrossRef] [PubMed]
| Variables | Intervention N = 18 n (%) | Control N = 18 n (%) | p-Value |
|---|---|---|---|
| Demographics | |||
| Age, median (Q1, Q3) | 69 (64, 76) | 73 (65, 78) | 0.67 |
| Female | 5 (25) | 5 (28) | 0.85 |
| Stroke type | |||
| Ischemic | 18 (90) | 18 (100) | |
| Hemorrhagic | 2 (10) | 0 (0) | 0.17 |
| Stroke Severity | |||
| NIHSS in hospital, median (Q1, Q3) | 5 (3, 19) | 4 (1, 14) | 0.34 |
| Able to walk during admission | 10 (50) | 9 (56) * | 0.19 |
| Slight to severe disability (mRS 2–4) | 7 (37) | 6 (35) | 0.92 |
| Outcome Measure | Within-Group Differences | Between-Groups Differences * | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Attention Control | MBI | |||||||||
| Sample Size (n) | Baseline Mean (SD) | Post-Intervention Mean (SD) | Cohen’s d * | Sample Size (n) | Baseline Mean (SD) | Post-Intervention Mean (SD) | Cohen’s d * | β Coefficient (95% CI) | p-Value | |
| Blood pressure | ||||||||||
| Systolic (mmHg) | 18 | 140 (16.9) | 139 (16.4) | 0.10 | 18 | 136 (14.4) | 131 (14.0) | 0.34 | −3.3 (−11.4, 4.8) | 0.421 |
| Diastolic (mmHg) | 18 | 82 (8.4) | 81 (7.6) | 0.11 | 18 | 82 (8.2) | 78 (11) | 0.41 | −3.2 (−8.7, 2.3) | 0.249 |
| Stress | ||||||||||
| Perceived Stress Scale | 18 | 14 (9.1) | 14 (8.6) | 0 | 18 | 12 (5.8) | 11 (6.6) | 0.12 | −0.8 (−4.3, 2.8) | 0.667 |
| Hair cortisol (pg/mg) | 7 | 15 (6.9) | 13 (5.2) | 0.34 | 8 | 15 (9.6) | 11 (1.2) | 0.52 | −1.5 (−10.5, 7.5) | 0.743 |
| Blood glucose | ||||||||||
| HBA1c (%) | 7 | 6.3 (1.1)) | 6.5 (1.1) | −0.22 | 10 | 5.8 (0.6) | 6.1 (0.8) | −0.30 | 0.2 (−0.2, 0.6) | 0.393 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thayabaranathan, T.; Paul, M.; Walker, F.R.; Hancock, S.; Allan, L.; Immink, M.A.; Hillier, S.; Kilkenny, M.F.; Brodtmann, A.; Gee, E.; et al. Movement-Based Mindfulness vs. Attention Control for Modifying Physiological Risk in Chronic Stroke: Evidence from a Feasibility Trial. Healthcare 2025, 13, 2940. https://doi.org/10.3390/healthcare13222940
Thayabaranathan T, Paul M, Walker FR, Hancock S, Allan L, Immink MA, Hillier S, Kilkenny MF, Brodtmann A, Gee E, et al. Movement-Based Mindfulness vs. Attention Control for Modifying Physiological Risk in Chronic Stroke: Evidence from a Feasibility Trial. Healthcare. 2025; 13(22):2940. https://doi.org/10.3390/healthcare13222940
Chicago/Turabian StyleThayabaranathan, Tharshanah, Marina Paul, Frederick R. Walker, Shaun Hancock, Liam Allan, Maarten A. Immink, Susan Hillier, Monique F. Kilkenny, Amy Brodtmann, Emma Gee, and et al. 2025. "Movement-Based Mindfulness vs. Attention Control for Modifying Physiological Risk in Chronic Stroke: Evidence from a Feasibility Trial" Healthcare 13, no. 22: 2940. https://doi.org/10.3390/healthcare13222940
APA StyleThayabaranathan, T., Paul, M., Walker, F. R., Hancock, S., Allan, L., Immink, M. A., Hillier, S., Kilkenny, M. F., Brodtmann, A., Gee, E., Carey, L. M., Stolwyk, R., Bernhardt, J., Nilsson, M., & Cadilhac, D. A. (2025). Movement-Based Mindfulness vs. Attention Control for Modifying Physiological Risk in Chronic Stroke: Evidence from a Feasibility Trial. Healthcare, 13(22), 2940. https://doi.org/10.3390/healthcare13222940








