Socially Sustainable Interventions for Childhood Obesity Management: A Scoping Review of Randomized Controlled Trials
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Search Strategy
2.3. Study Coding and Data Extraction
2.4. Methodological Quality Assessment
3. Results
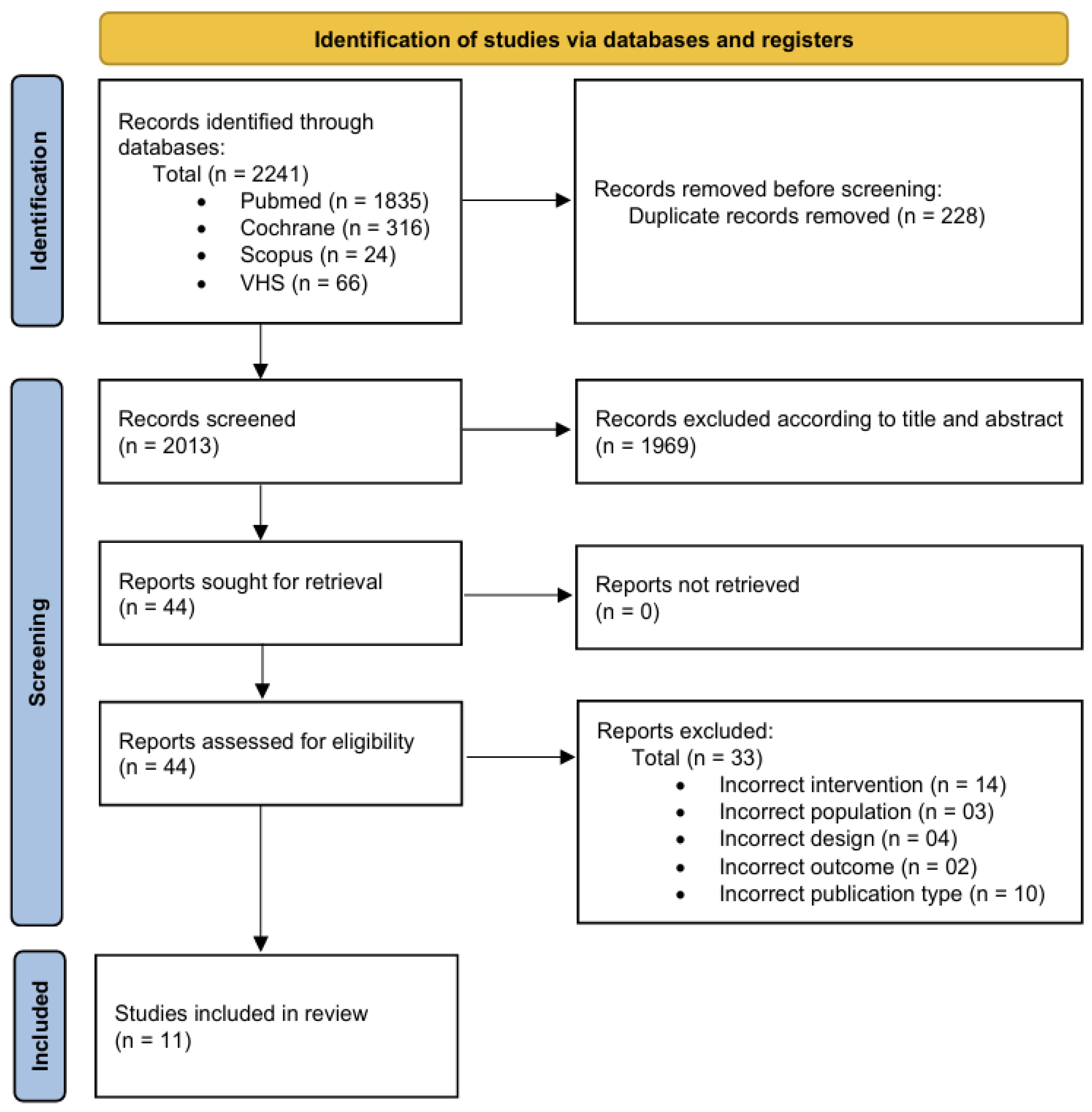
3.1. Search Results
3.2. Studies’ Description
3.3. Methodological Quality
4. Discussion
4.1. School- and Community-Based Environmental Interventions
4.2. Family-Based Interventions
4.3. General Overview
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BMI | Body Mass Index |
| WHO | World Health Organization |
| CDC | Centers for Disease Control and Prevention |
| RCT | Randomized Controlled Trial |
| PRISMA-ScR | Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews |
| VHL | Virtual Health Library |
| PedsQL | Pediatric Quality of Life Inventory |
| PEDro | Physiotherapy Evidence Database Scale |
| SBP | Systolic Blood Pressure |
| DBP | Diastolic Blood Pressure |
| SDQ | Strengths and Difficulties Questionnaire |
References
- World Health Organization. Obesity and Overweight. 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 27 September 2025).
- Zhang, X.; Liu, J.; Ni, Y.; Yi, C.; Fang, Y.; Ning, Q.; Shen, B.; Zhang, K.; Liu, Y.; Yang, L.; et al. Global Prevalence of Overweight and Obesity in Children and Adolescents: A Systematic Review and Meta-Analysis. JAMA Pediatr. 2024, 178, 800–813. [Google Scholar] [CrossRef]
- Garrido-Miguel, M.; Oliveira, A.; Cavero-Redondo, I.; Álvarez-Bueno, C.; Pozuelo-Carrascosa, D.P.; Soriano-Cano, A.; Martínez-Vizcaíno, V. Prevalence of Overweight and Obesity among European Preschool Children: A Systematic Review and Meta-Regression by Food Group Consumption. Nutrients 2019, 11, 1698. [Google Scholar] [CrossRef] [PubMed]
- Karnik, S.; Kanekar, A. Childhood obesity: A global public health crisis. Int. J. Prev. Med. 2012, 3, 1–7. [Google Scholar]
- Sahoo, K.; Sahoo, B.; Choudhury, A.K.; So, N.Y.; Kumar, R.; Bhadoria, A.S. Childhood obesity: Causes and consequences. J. Fam. Med. Prim. Care 2015, 4, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Mond, J.; Van den Berg, P.; Boutelle, K.; Hannan, P.; Neumark-Sztainer, D. Obesity, body dissatisfaction, and emotional well-being in early and late adolescence: Findings from the project EAT study. J. Adolesc. Health 2011, 48, 373–378. [Google Scholar] [CrossRef] [PubMed]
- Hagman, E.; Danielsson, P.; Brandt, L.; Svensson, V.; Ekbom, A.; Marcus, C. Childhood obesity, obesity treatment outcome, and achieved education: A prospective cohort study. J. Adolesc. Health 2017, 61, 508–513. [Google Scholar] [CrossRef]
- Biro, F.M.; Wien, M. Childhood obesity and adult morbidities. Am J Clin Nutr. 2010, 91, 1499–1505. [Google Scholar] [CrossRef]
- Angoorani, P.; Heshmat, R.; Ejtahed, H.S.; Motlagh, M.E.; Ziaodini, H.; Taheri, M.; Aminaee, T.; Shafiee, G.; Godarzi, A.; Qorbani, M.; et al. The association of parental obesity with physical activity and sedentary behaviors of their children: The CASPIAN-V study. J. Pediatr. 2018, 94, 410–418. [Google Scholar] [CrossRef]
- An, R.; Shen, J.; Yang, Q.; Yang, Y. Impact of built environment on physical activity and obesity among children and adolescents in China: A narrative systematic review. J. Sport Health Sci. 2019, 8, 153–169. [Google Scholar] [CrossRef]
- Braithwaite, I.; Stewart, A.W.; Hancox, R.J.; Beasley, R.; Murphy, R.; Mitchell, E.A.; ISAAC Phase Three Study Group. The worldwide association between television viewing and obesity in children and adolescents: Cross sectional study. PLoS ONE. 2013, 8, e74263. [Google Scholar] [CrossRef]
- He, G.; Cerin, E.; Huang, W.Y.; Wong, S.H. Understanding neighborhood environment related to Hong Kong children’s physical activity: A qualitative study using nominal group technique. PLoS ONE. 2014, 9, e106578. [Google Scholar] [CrossRef]
- Skouteris, H.; Cox, R.; Huang, T.; Rutherford, L.; Edwards, S.; Cutter-Mackenzie, A. Promoting obesity prevention together with environmental sustainability. Health Promot. Int. 2014, 29, 454–462. [Google Scholar] [CrossRef]
- Sacher, P.M.; Kolotourou, M.; Chadwick, P.M.; Cole, T.J.; Lawson, M.S.; Lucas, A.; Singhal, A. Randomized controlled trial of the MEND program: A family-based community intervention for childhood obesity. Obesity 2010, 18, 62–68. [Google Scholar] [CrossRef] [PubMed]
- Benjamin Neelon, S.E.; Namenek Brouwer, R.J.; Østbye, T.; Evenson, K.R.; Neelon, B.; Martinie, A.; Bennett, G. A community-based intervention increases physical activity and reduces obesity in school-age children in North Carolina. Child. Obes. 2015, 11, 297–303. [Google Scholar] [CrossRef] [PubMed]
- Narayanan, N.; Nagpal, N.; Zieve, H.; Vyas, A.; Tatum, J.; Ramos, M.; Team KiPOW!; McCarter, R., Jr.; Lucas, C.T.; Mietus-Snyder, M. A School-Based Intervention Using Health Mentors to Address Childhood Obesity by Strengthening School Wellness Policy. Prev. Chronic Dis. 2019, 16, 154. [Google Scholar] [CrossRef]
- Ernest, D.K.; Onugha, E.A.; Singh, B.; Sharma, S.V.; Dave, J.M. A Scoping Review of the Social Determinants of Pediatric and Adolescent Obesity. Int. J. Pediatr. 2025, 28, 8871022. [Google Scholar] [CrossRef] [PubMed]
- Brown, V.; Moodie, M.; Sultana, M.; Hunter, K.E.; Byrne, R.; Zarnowiecki, D.; Seidler, A.L.; Golley, R.; Taylor, R.W.; Hesketh, K.D.; et al. A scoping review of outcomes commonly reported in obesity prevention interventions aiming to improve obesity-related health behaviors in children to age 5 years. Obes. Rev. 2022, 23, e13427. [Google Scholar] [CrossRef]
- Chia, A.; Ong, J.; Bundele, A.; Lim, Y.W. Social entrepreneurship in obesity prevention: A scoping review. Obes. Rev. 2022, 23, e13378. [Google Scholar] [CrossRef]
- Wang, X.; Ammerman, A.; Orr, C.J. Family-based interventions for preventing overweight or obesity among preschoolers from racial/ethnic minority groups: A scoping review. Obes. Sci. Pract. 2021, 8, 371–386. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- De Morton, N.A. The PEDro scale is a valid measure of the methodological quality of clinical trials: A demographic study. Aust. J. Physiother. 2009, 55, 129–133. [Google Scholar] [CrossRef]
- Warren, J.M.; Henry, C.J.; Lightowler, H.J.; Bradshaw, S.M.; Perwaiz, S. Evaluation of a pilot school programme aimed at the prevention of obesity in children. Health Promot. Int. 2003, 18, 287–296. [Google Scholar] [CrossRef]
- Economos, C.D.; Hyatt, R.R.; Goldberg, J.P.; Must, A.; Naumova, E.N.; Collins, J.J.; Nelson, M.E. A community intervention reduces BMI z-score in children: Shape Up Somerville first year results. Obesity 2007, 15, 1325–1336. [Google Scholar] [CrossRef]
- de Silva-Sanigorski, A.M.; Bell, A.C.; Kremer, P.; Nichols, M.; Crellin, M.; Smith, M.; Sharp, S.; de Groot, F.; Carpenter, L.; Boak, R.; et al. Reducing obesity in early childhood: Results from Romp & Chomp, an Australian community-wide intervention program. Am. J. Clin. Nutr. 2010, 91, 831–840. [Google Scholar] [CrossRef] [PubMed]
- Story, M.; Hannan, P.J.; Fulkerson, J.A.; Rock, B.H.; Smyth, M.; Arcan, C.; Himes, J.H. Bright Start: Description and main outcomes from a group-randomized obesity prevention trial in American Indian children. Obesity 2012, 20, 2241–2249. [Google Scholar] [CrossRef]
- Williamson, D.A.; Champagne, C.M.; Harsha, D.W.; Han, H.; Martin, C.K.; Newton, R.L., Jr.; Sothern, M.S.; Stewart, T.M.; Webber, L.S.; Ryan, D.H. Effect of an environmental school-based obesity prevention program on changes in body fat and body weight: A randomized trial. Obesity 2012, 20, 1653–1661. [Google Scholar] [CrossRef] [PubMed]
- Butte, N.F.; Hoelscher, D.M.; Barlow, S.E.; Pont, S.; Durand, C.; Vandewater, E.A.; Liu, Y.; Adolph, A.L.; Pérez, A.; Wilson, T.A.; et al. Efficacy of a Community- Versus Primary Care-Centered Program for Childhood Obesity: TX CORD RCT. Obesity 2017, 25, 1584–1593. [Google Scholar] [CrossRef]
- Taveras, E.M.; Marshall, R.; Sharifi, M.; Avalon, E.; Fiechtner, L.; Horan, C.; Gerber, M.W.; Orav, E.J.; Price, S.N.; Sequist, T.; et al. Comparative Effectiveness of Clinical-Community Childhood Obesity Interventions: A Randomized Clinical Trial. JAMA Pediatr. 2017, 171, e171325. [Google Scholar] [CrossRef] [PubMed]
- Waters, E.; Gibbs, L.; Tadic, M.; Ukoumunne, O.C.; Magarey, A.; Okely, A.D.; de Silva, A.; Armit, C.; Green, J.; O’Connor, T.; et al. Cluster randomised trial of a school-community child health promotion and obesity prevention intervention: Findings from the evaluation of fun ‘n healthy in Moreland! BMC Public Health 2017, 18, 92. [Google Scholar] [CrossRef]
- Wilfley, D.E.; Saelens, B.E.; Stein, R.I.; Best, J.R.; Kolko, R.P.; Schechtman, K.B.; Wallendorf, M.; Welch, R.R.; Perri, M.G.; Epstein, L.H. Dose, Content, and Mediators of Family-Based Treatment for Childhood Obesity: A Multisite Randomized Clinical Trial. JAMA Pediatr. 2017, 171, 1151–1159. [Google Scholar] [CrossRef] [PubMed]
- Novotny, R.; Davis, J.; Butel, J.; Boushey, C.J.; Fialkowski, M.K.; Nigg, C.R.; Braun, K.L.; Leon Guerrero, R.T.; Coleman, P.; Bersamin, A.; et al. Effect of the Children’s Healthy Living Program on Young Child Overweight, Obesity, and Acanthosis Nigricans in the US-Affiliated Pacific Region: A Randomized Clinical Trial. JAMA Netw. Open 2018, 1, e183896. [Google Scholar] [CrossRef] [PubMed]
- Novotny, R.; Yamanaka, A.B.; Butel, J.; Boushey, C.J.; Dela Cruz, R.; Aflague, T.; Coleman, P.; Shallcross, L.; Fleming, T.; Wilkens, L.R. Maintenance Outcomes of the Children’s Healthy Living Program on Overweight, Obesity, and Acanthosis Nigricans Among Young Children in the US-Affiliated Pacific Region: A Randomized Clinical Trial. JAMA Netw. Open 2022, 5, e2214802. [Google Scholar] [CrossRef] [PubMed]
- Baskin, M.L.; Tipre, M.; Richardson, M. Culturally-Relevant Obesity Interventions: African American Children and Adolescents. In Families, Food, and Parenting; Francis, L.A., McHale, S.M., King, V., Glick, J.E., Eds.; National Symposium on Family Issues; Springer: Cham, Switzerland, 2021; Volume 11. [Google Scholar]
- Chen, J.L.; Weiss, S.; Heyman, M.B.; Cooper, B.; Lustig, R.H. The efficacy of the Web-based childhood obesity prevention program in Chinese American adolescents: Web ABC Study. J. Adolesc. Health 2011, 49, 148–154. [Google Scholar] [CrossRef]
| Element | Description | Application in the Review |
|---|---|---|
| Population (P) | Children aged 2–12 years who are overweight or obese | The review included studies with pediatric participants (2–12 years old) classified as overweight or obese according to age- and sex-specific BMI criteria. |
| Concept (C) | Socially sustainable interventions designed to prevent or treat childhood obesity. | Interventions that incorporate elements promoting equity, inclusivity, community engagement, and long-term social well-being, such as family-, school-, or community-based programs aimed at fostering sustainable health-related behaviors. |
| Context (C) | Family, school, and community environments where health promotion and obesity prevention occur. | Studies were included if they evaluated interventions implemented in real-world social settings (home, schools, or community programs) and assessed anthropometric outcomes within those contexts. |
| Keywords | ||||
|---|---|---|---|---|
| P (Population) | Intervention | Outcome | ||
| “child nutrition disorders” [Mesh] OR “pediatric obesity” [Mesh] | AND | “sustainable development” [Mesh] OR “sustainable development indicators” OR “social environment” [Mesh] OR “social sustainability” | AND | “body weight” [Mesh] OR “body mass index” [Mesh] OR “waist circumference” [Mesh] OR “anthropometric outcome” |
| Authors | Participants’ Characteristics | Design | Results |
|---|---|---|---|
| Butte et al. [29] | 549 North American obese (BMI ≥ 85th percentile) children from 12 primary care clinics stratified in 3 age groups (2–5 y; 6–8 y; 9–12 y) | 12-month (Intensive Phase = 3 months; Transition Phase = 9 months) community-centered weight management program (Intervention group; n = 315) vs. primary care-centered program (Control group; n = 234) | Intervention group (including 2–5 y, 6–8 y and 9–12 y), Intensive Phase: ↓BMI (p < 0.05), ↓%fat mass (p < 0.05), ↑PedsQL (p < 0.05), ↓SDQ (p < 0.05) Intervention group (including 2–5 y, 6–8 y and 9–12 y), Transition Phase: ↔BMI (p > 0.05), ↑%fat mass (p < 0.05), ↔PedsQL (p > 0.05), ↔SDQ (p > 0.05) Control group (including 2–5 y, 6–8 y and 9–12 y), Intensive Phase: ↔BMI (p > 0.35), ↔%fat mass (p > 0.05), ↑PedsQL (p < 0.05), ↓SDQ (p < 0.05) Control group (including 2–5 y, 6–8 y and 9–12 y), Transition Phase: ↑BMI (p < 0.05), ↑%fat mass (p < 0.05), ↑PedsQL (p < 0.05), ↔SDQ (p > 0.05) |
| de Silva-Sanigorski et al. [26] | 26,664 Australian children from local government areas in Victoria (0–5 y) | 4-year community-wide, multisetting, multistrategy program in CoGG and BoQ (0–2 y, n = 1457; 3.5–5 y, n = 1082) vs. LGA across the rest of Victoria (0–2 y, n = 14,924; 3–5 y, n = 9201) | Intervention group: ↓weight (p < 0.05), ↓BMI (p < 0.05), ↓BMI z-score (p < 0.05), ↓%overweight/obese children (p < 0.05) (both 0–2 y and 3.5–5 y), ↑fruit ingestion (p = 0.03), ↑vegetable ingestion (p < 0.001), ↓sugar-sweetened beverages (p = 0.005) Control group: ↔weight (p > 0.05), ↔BMI (p > 0.05), ↔BMI z-score (p > 0.05), ↔%overweight/obese children (p > 0.05) (both 0–2 y and 3.5–5 y), ↑fruit ingestion (p = 0.03), ↑vegetable ingestion (p < 0.001), ↓sugar-sweetened beverages (p = 0.005) |
| Economos et al. [25] | 1178 North American Grade 1, 2, and 3 public school children from 3 communities in Somerville (6–9 y) | 8-month community-, family and school-centered weight gain prevention program (Intervention group; n = 385) vs. Control communities (Control group; n = 793) | Intervention group: ↓BMI z-score (p = 0.001) Control group: ↔BMI z-score (p > 0.05) |
| Novotny et al. [33] | 4042 US-Affiliated Pacific region overweight (BMI ≥ 85th–94th percentile), obese (BMI ≥ 95th percentile), and acanthosis nigricans children (2–8 y) | 24-month multijurisdictional, multilevel, multicomponent community-based program (n = 1342) vs. control group (n = 1295) vs. Temporal group (n = 1405) | Intervention group: ↓BMI z-score (p = 0.006), ↓waist circumference (p = 0.02), ↓%overweight/obese children (p = 0.02), ↔fruit ingestion (p = 0.07), ↔vegetable ingestion (p = 0.73), ↔sugar-sweetened beverages (p = 0.09) Control group: ↔BMI z-score (p = 0.84), ↑waist circumference (p < 0.001), ↔%overweight/obese children (p = 0.35), ↔fruit ingestion (p = 0.09), ↔vegetable ingestion (p = 0.89), ↔sugar-sweetened beverages (p = 0.40) Temporal group: ↔BMI z-score (p = 0.42), ↔waist circumference (p = 0.06), ↔%overweight/obese children (p = 0.84), fruit ingestion (not measured), vegetable ingestion (not measured), sugar-sweetened beverages (not measured) |
| Novotny et al. [34] | 1469 US-Affiliated Pacific region overweight (BMI ≥ 85th–94th percentile), obese (BMI ≥ 95th percentile), and acanthosis nigricans children (2–8 y) | 6-year multijurisdictional, multilevel, multicomponent community-based program (n = 500) vs. control group (n = 479) vs. Temporal group (n = 490) | Intervention group: ↓BMI z-score (p = 0.02), ↔waist circumference (p = 0.06), ↓%overweight/obese children (p = 0.05), ↔fruit ingestion (p = 0.71), ↔vegetable ingestion (p = 0.99), ↔sugar-sweetened beverages (p = 0.51) Control group: ↑BMI z-score (p = 0.05), ↑waist circumference (p < 0.0001), ↑%overweight/obese children (p = 0.009), ↔fruit ingestion (p = 0.08), ↔vegetable ingestion (p = 0.13), ↔sugar-sweetened beverages (p = 0.10) Temporal group: ↔BMI z-score (p = 0.16), ↑waist circumference (p = 0.0005), ↔%overweight/obese children, fruit ingestion (not measured), vegetable ingestion (not measured), sugar-sweetened beverages (not measured). |
| Story et al. [27] | 454 North American kindergarten children (5–6 y) from 14 schools on the Pine Ridge Reservation in South Dakota | 14-week family- and school-centered weight gain prevention program (Intervention group; n = 267) vs. Control group (n = 187) | Intervention group: ↔BMI (p = 0.057), ↔BMI z-score (p = 0.90), ↔%fat mass (p = 0.12), ↓%overweight children (p = 0.01), ↔obese children (p = 0.50), ↓sugar-sweetened beverages (p = 0.02), ↓fat ingestion (p = 0.004). Control group: ↔BMI (p > 0.05), ↔BMI z-score (p > 0.05), ↔%fat mass (p > 0.05), ↑%overweight children (p > 0.05), ↔obese children (p > 0.05), ↔sugar-sweetened beverages (p > 0.05), ↔fat ingestion (p > 0.05). |
| Taveras et al. [30] | 664 North American overweight and obese (BMI ≥ 85th percentile) children (2–12.9 y) | 1-year enhanced primary care plus family- and contextually centered individual health coaching (Intervention group; n = 336) vs. enhanced primary care (Control group; n = 328) | Intervention group: ↓BMI z-score (p < 0.05), ↓%overweight children (p < 0.05), ↓%obese children (p < 0.05), ↑PedsQL (p < 0.05), ↑Parenteral resource empowerment (p < 0.05). Control group: ↓BMI z-score (p < 0.05), ↓%overweight children (p < 0.05), ↓%obese children (p < 0.05), ↔PedsQL (p > 0.05), ↔Parenteral resource empowerment (p > 0.05). |
| Warren et al. [24] | 218 British children (5–7 y) from 3 primary schools in Oxford | 20-week school-centered weight gain prevention program through Nutrition (Intervention group 1; n = 56) vs. Physical activity (Intervention group 2; n = 54) vs. Physical activity plus Nutrition (Intervention group 3; n = 54) vs. Education (Control group; n = 54) | Intervention group 1: ↔BMI (p > 0.05), ↔%overweight children (p > 0.05), ↔obese children (p > 0.05), ↑fruit ingestion (p < 0.05), ↔physical activity (p > 0.05). Intervention group 2: ↔BMI (p > 0.05), ↔%overweight children (p > 0.05), ↔obese children (p > 0.05), ↔fruit ingestion (p > 0.05), ↑physical activity (p < 0.05). Intervention group 3: ↔BMI (p > 0.05), ↔%overweight children (p > 0.05), ↔obese children (p > 0.05), ↔fruit ingestion (p > 0.05), ↑physical activity (p < 0.05). Control group: ↔BMI (p > 0.05), ↔%overweight children (p > 0.05), ↔obese children (p > 0.05), ↑fruit ingestion (p < 0.05), ↔physical activity (p > 0.05) |
| Waters et al. [31] | 2806 Australian children (5–12 y) from 22 primary schools in Moreland | 3.5-year school-centered weight gain prevention program (Intervention group; n = 1346) vs. normal school programs (Control group; n = 1460) | Intervention group: ↔BMI (p > 0.05), ↓BMI z-score (p < 0.05), ↔waist circumference (p > 0.05), ↓%overweight children (p < 0.05), ↓obese children (p < 0.05), ↑fruit ingestion (p < 0.05), ↔physical activity (p > 0.05) Control group: ↔BMI (p > 0.05), ↓BMI z-score (p < 0.05), ↔waist circumference (p > 0.05), ↓%overweight children (p < 0.05), ↓obese children (p < 0.05), ↔fruit ingestion (p > 0.05), ↔physical activity (p > 0.05) |
| Wilfley et al. [32] | 160 North American overweight or obese (BMI ≥ 85th percentile) children (7–11 y) | 12-month family-based behavioral weight loss program of low (Intervention group 1; n = 54) and high dose (Intervention group 2; n = 55) vs. weight-control education program (Control group; n = 51) | Intervention group 1: ↔BMI z-score (p = 0.24), ↓%overweight children (p < 0.001) Intervention group 2: ↔BMI z-score (p = 0.81), ↓%overweight children (p = 0.02) Control group: ↔BMI z-score (p > 0.05), ↔%overweight children (p > 0.05) |
| Williamson et al. [28] | 1697 North American Grades 4–6 children from 17 school systems in Louisiana (9–11 y) | 28-month school-centered healthy habits program (Intervention group 1; n = 612) vs. school-centered healthy habits program + internet-based educational approach (Intervention group 2; n = 638) vs. Control group (n = 447) | Intervention group 1: ↔BMI z-score (p > 0.05), ↔%fat mass (p > 0.05), ↔food intake (p > 0.05), ↔physical activity (p > 0.05), ↔sedentary behaviour (p > 0.05) Intervention group 2: ↔BMI z-score (p > 0.05), ↔%fat mass (p > 0.05), ↔food intake (p > 0.05), ↔physical activity (p > 0.05), ↔sedentary behaviour (p > 0.05) Control group: ↔BMI z-score (p > 0.05), ↔%fat mass (p > 0.05), ↔food intake (p > 0.05), ↔physical activity (p > 0.05), ↔sedentary behaviour (p > 0.05) |
| Reference | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Butte et al. [29] | Yes | ✔ | ✔ | ✔ | X | X | X | X | ✔ | ✔ | ✔ | 6 |
| De Silva-Sanigorski et al. [26] | No | ✔ | X | X | X | X | X | X | ✔ | ✔ | ✔ | 4 |
| Economos et al. [25] | Yes | ✔ | X | ✔ | X | X | X | X | ✔ | ✔ | ✔ | 5 |
| Novotny et al. [33] | Yes | ✔ | X | ✔ | X | X | X | ✔ | ✔ | ✔ | ✔ | 6 |
| Novotny et al. [34] | Yes | ✔ | X | ✔ | X | X | X | X | ✔ | ✔ | ✔ | 5 |
| Story et al. [27] | No | ✔ | X | ✔ | X | X | X | X | ✔ | ✔ | ✔ | 5 |
| Taveras et al. [30] | Yes | ✔ | ✔ | ✔ | X | X | X | ✔ | ✔ | ✔ | ✔ | 7 |
| Warren et al. [24] | No | ✔ | X | ✔ | X | X | X | X | ✔ | ✔ | ✔ | 5 |
| Waters et al. [31] | Yes | ✔ | ✔ | ✔ | X | X | ✔ | ✔ | ✔ | ✔ | ✔ | 8 |
| Wilfley et al. [32] | Yes | ✔ | ✔ | ✔ | X | X | X | ✔ | ✔ | ✔ | ✔ | 7 |
| Williamson et [28] | Yes | ✔ | X | ✔ | X | X | X | X | ✔ | ✔ | ✔ | 5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Paula, R.; de Salles Painelli, V.; Andreato, L.V.; Magnani Branco, B.H.; Corrêa, R.G. Socially Sustainable Interventions for Childhood Obesity Management: A Scoping Review of Randomized Controlled Trials. Healthcare 2025, 13, 2932. https://doi.org/10.3390/healthcare13222932
de Paula R, de Salles Painelli V, Andreato LV, Magnani Branco BH, Corrêa RG. Socially Sustainable Interventions for Childhood Obesity Management: A Scoping Review of Randomized Controlled Trials. Healthcare. 2025; 13(22):2932. https://doi.org/10.3390/healthcare13222932
Chicago/Turabian Stylede Paula, Regiane, Vitor de Salles Painelli, Leonardo Vidal Andreato, Braulio Henrique Magnani Branco, and Rúbia Gomes Corrêa. 2025. "Socially Sustainable Interventions for Childhood Obesity Management: A Scoping Review of Randomized Controlled Trials" Healthcare 13, no. 22: 2932. https://doi.org/10.3390/healthcare13222932
APA Stylede Paula, R., de Salles Painelli, V., Andreato, L. V., Magnani Branco, B. H., & Corrêa, R. G. (2025). Socially Sustainable Interventions for Childhood Obesity Management: A Scoping Review of Randomized Controlled Trials. Healthcare, 13(22), 2932. https://doi.org/10.3390/healthcare13222932







