Healthcare Professionals’ Cultural Competence in Diabetes Care: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Information Sources and Search Strategies
2.3. Search Keyword and Strategy
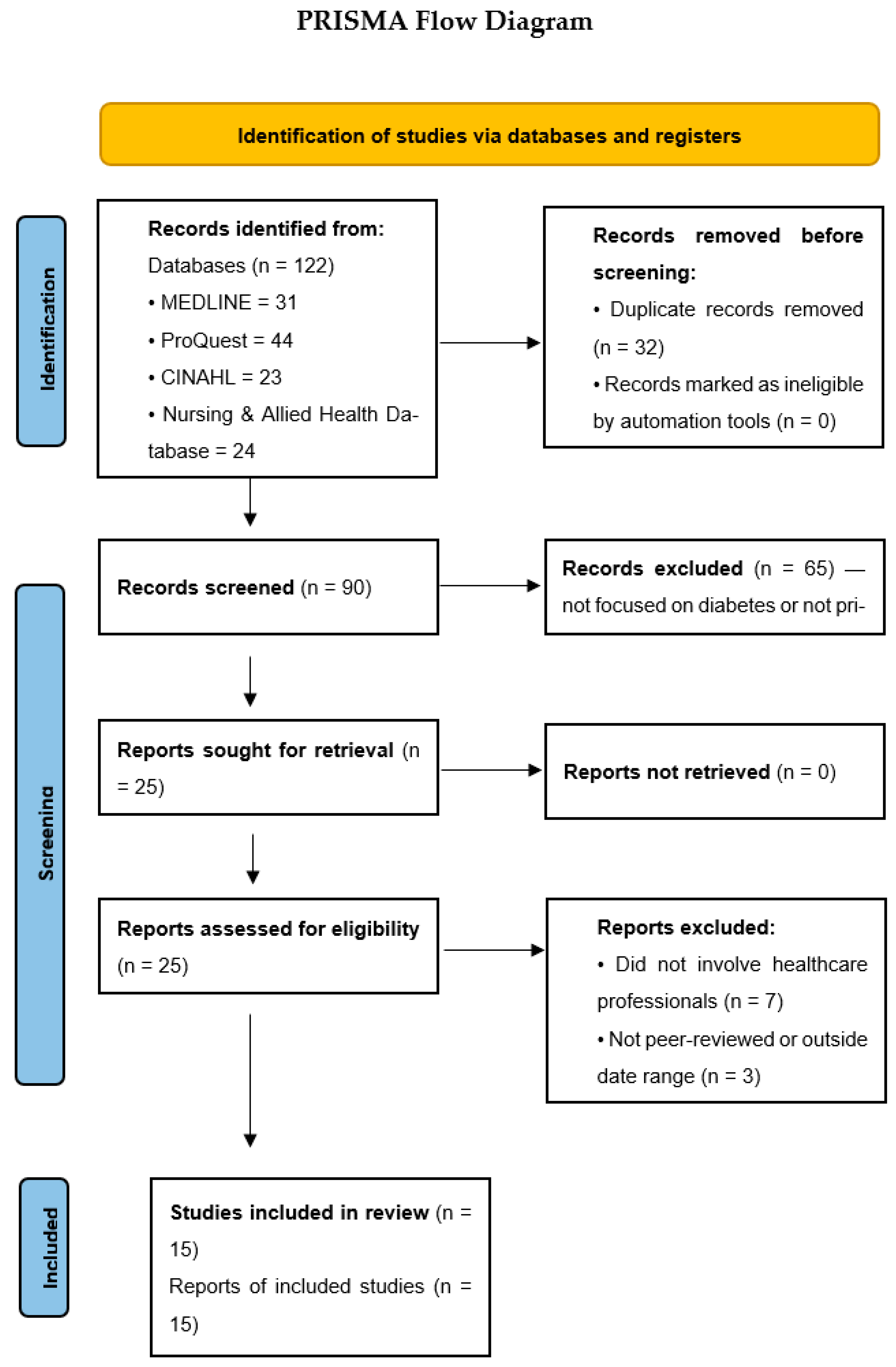
2.4. Study Selection Process
2.5. Data Collection Process
2.6. Data Items
2.7. Study Risk of Bias Assessment
2.8. Effect Measures
2.9. Synthesis Methods
2.10. Reporting Bias Assessment
3. Results
3.1. Study Selection
3.2. Study Characteristics
3.3. Risk of Bias in Studies
3.4. Result of Individual Studies
3.5. Results of Synthesis
3.5.1. Healthcare Professionals’ Cultural Competence in Diabetes Care
3.5.2. Barriers to Providing Culturally Competent Diabetes Care
3.5.3. Effectiveness of Trainings on Cultural Competence for Healthcare Professionals
3.6. Reporting Biases
3.7. Certainty of Evidence
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Appendix A
| Authors/Date | Aim | Methodology | Sample | Findings |
|---|---|---|---|---|
| Zeh et al. (2018) [16] | This study aims to assess the cultural competence of diabetes services provided to minority ethnic groups in a multicultural UK metropolis with a diabetes prevalence of 4.3% | The culturally competent assessment tool (CCAT) was used to evaluate the cultural competence of diabetes services. | The survey was sent to each senior general practitioner (GP) and practice manager of 66 general practices, but only 34 practices responded. | An assessment of cultural competence using CCAT revealed that 19 practices were highly culturally competent (90–100%), 9 moderately competent (70–89%), and 6 less competent (<70%) |
| Pettersson S et al. (2022) [17] | This study evaluates the cultural competence of Swedish healthcare professionals specialized in diabetes care and identifies factors influencing it. | The Swedish version of the Cultural Competence Assessment Instrument (CCAI-S) was employed to assess cultural competence. The instrument consists of 13 items, with responses measured on a 6-point scale. | 279 healthcare professionals responded to the questionnaire. The healthcare professionals consisted of 207 registered nurses, 37 general practitioners, 22 podiatrists, 8 dieticians, and 4 other professionals. | Overall, 61% felt confident in verbal communication across cultures, whereas 9% struggled with non-verbal communication and 10% with minority ethnic clients. |
| Çinar et al. (2022) [18] | The study investigates diabetes nurses’ cultural competence in educating and caring for patients with diabetes, taking into account their cultural characteristics. | A cross-sectional descriptive study was carried out, and data were obtained by using the introductory information Form and the Nurse Cultural Competence Scale (NCCS-T) | The study consisted of 183 diabetes nurses in Turkey | 63.9% of diabetes nurses identified language as a problem, and 60.15% had communication issues. According to the NCCS-T scores, all participants had cultural skills, knowledge, and sensitivity. 89.65% had an average level of cultural competence and a higher mean score in graduate and experienced nurses. |
| Ofosu et al. (2023) [24] | The study was carried out to understand primary health providers’ views on the challenges of providing intercultural diabetes and obesity care. | This research included 9 individual interviews and 4 focus groups with 6 to 12 participants. Semi-structured and open-ended questions that address how healthcare providers manage diabetes and obesity and the challenges they experience were used in the interview. | This study involved 37 healthcare professionals specialized in diabetes care. | Communication barriers between patients and providers, low literacy levels of migrants, and a lack of knowledge in addressing non-medical issues affected the health outcomes of migrant patients. |
| Jager M et al. (2020) [25] | to investigate dieticians’ experiences, knowledge, Attitudes, and abilities they consider crucial for effective dietetic diabetes care | A semi-structured interview was designed using Seeleman’s cultural competency model and the Dutch dietetic consultation model. | 12 dieticians of different ages, ethnic backgrounds and experience were involved | Dietitians were dissatisfied with their consultations with immigrants due to communication issues like difficulty in retrieving information and explaining how food and diabetes work. |
| Tremblay M et al. (2020) [26] | Aimed to find potential obstacles and facilitators of cultural safety in medical care provided to Indigenous people with diabetes. | Using a qualitative descriptive design, data were collected through three talking circles with three different groups of participants. | A total of 30 participants, including 10 healthcare professionals, 6 caregivers, and 14 people with diabetes | Health providers mentioned the congestion in the healthcare system, communication barriers, and lack of knowledge about the culture as hindrances to culturally safe care. |
| Crowshoe L et al. (2018) [27] | Aimed to describe the perspectives of Canadian physicians on diabetes management for Indigenous patients. | A semi-structured interview involving family physicians, specialists, and Aboriginal patients was carried out. | 28 individuals took part in this study. | Physicians acknowledged their limitations, linking them to inconsistent service, physician shortage, lack of trust, and discrimination by other health professionals. |
| Jager M et al. (2024) [19] | The purpose of this study was to present the pilot implementation and initial evaluation of a cultural competence program for dieticians. | Training was created based on Seeleman’s cultural competence framework. Evaluation was conducted using a Cultural Competence Questionnaire, an Experience Evaluation Questionnaire, and consultation observations. | 8 dieticians responded and participated in the research | There was an increase in self-perceived cultural competence and attitude, the use of teach-back methods and discussions of treatment options. Skills and knowledge were unchanged. |
| Movafagh S and Adams E (2024) [20] | This paper assesses the effect of pharmacist-led cultural competency training on provider self-perceived readiness and diabetes-related health outcomes in Asian patients. | A cross-sectional study, followed by a quasi-experimental Phase 1, evaluated the relationship between patients’ diabetes health and physicians’ CCCS scores. In phase two, surveys and patients’ diabetes indicators before and after training were used to assess pharmacist-led cultural competency training. | The first phase involved 9 healthcare providers. The second phase included 30 providers and 95 patients | Phase 1 demonstrated that providers’ baseline cross-cultural competence was insufficient, whereas Phase 2 found that training reduced their perceived unpreparedness. Only patients with uncontrolled diabetes showed a significant reduction in health parameters. |
| Kim K and Lee H (2016) [21] | This study used intervention mapping to assess the impact of a cultural competence training program for public health nurses (PHNs). | An embedded mixed-methods design was adopted, with professionals divided into experimental and control groups. The experimental group had four weeks of cultural competence training. Cultural competence was measured using the Koreans’ version of Jeffrey’s Transcultural Self-efficacy Tool (TSET). It also featured migrant women receiving treatment. | 41 public health nurses and 40 migrant women participated | The experimental group significantly improved Transcultural Self-efficacy (TSE), client-nurse trust, and satisfaction with nursing care compared to the control group. |
| Beck P et al. (2024) [23] | The study’s objective is to assess the efficacy of cross-cultural competence training for German healthcare professionals. | A quasi-experimental evaluation study was carried out at two German hospitals. The self-reported questionnaire Cross-Cultural Competence of Healthcare Professionals (CCCHP) was used to assess cross-cultural competence in both an intervention and control group, and the results were analyzed using SPSS Statistics 25. | 196 healthcare providers contributed to this research | Cross-cultural training increased knowledge, awareness, and attitudes while decreasing social desirability. Motivation and curiosity decreased, although empathy increased marginally. However, cross-cultural skills decreased after training, emphasizing the need for additional practical, long-term training. |
| Lin M and Hsu H (2020) [13] | This study aimed to examine the impact of a cultural competency educational course on nurses’ self-assessments of their cultural competence. | Attendees were randomly assigned to one of two groups: experimental or control. A four-week course was held, and pre-post data were collected with a two-month follow-up. Cultural competency was measured using the NCCS. | A total of 97 nurses were included | The experimental group scored lower on the total cultural competence and cultural action ability before intervention; however, the score was higher than that of the control group after a two-month follow-up. |
| Rissel C et al. (2022) [12] | This study aimed to assess the effectiveness of a Central Australian cultural awareness training program for healthcare professionals. | A case–control study was employed with a consecutive group pre-program, post-program, and follow-up evaluation. | Only 11 out of 124 participants responded to the two-month follow-up. | The scale mean score pre-program was 45.7, 47.3 post-program, and 42.2 after a two-month follow-up. Most participants found the course relevant to their work, and the qualitative feedback was positive. |
| McElfish P et al. (2017) [22] | The purpose of this study was to develop and evaluate a cultural training program to improve the delivery of culturally appropriate care in indigenous communities. | A mixed-methods evaluation based on the Kirkpatrick model was employed, with quantitative data collected after each session and qualitative data acquired from individuals and organizational units at two time points: immediately after each session and six months later. | 672 healthcare professionals participated in the research | Following training, 91.2% indicated more knowledge, 86.6% higher competence, and 87.2% better performance. At six months, the response rates were 17% for individuals and 28% for organizations. |
| Kaihlanen AM et al. (2019) [28] | This study investigates the nurses’ perceptions of the content and utility of cultural competence training, which focuses on developing awareness of one’s cultural differences. | A semi-structured interview was held in a hospital with a large number of immigrants. Invitations for cultural competence training and post-interview were sent via email and through the ward managers. | Only 20 registered nurses and practical nurses indicated interest, but only 10 attended the two sessions | Nurses acknowledged that the training raises understanding of patients’ cultural diversity, which fosters respect in treatment. It also promotes self-awareness and cognitive shifts and justifies using effective communication strategies. |
Appendix B
| Yes | No | Unclear | Not Applicable | |
|---|---|---|---|---|
| □ | □ | □ | □ |
| □ | □ | □ | □ |
| □ | □ | □ | □ |
| □ | □ | □ | □ |
| □ | □ | □ | □ |
| □ | □ | □ | □ |
| □ | □ | □ | □ |
| □ | □ | □ | □ |
References
- Hossain, M.J.; Al-Mamun, M.; Islam, M.R. Diabetes mellitus, the fastest growing global public health concern: Early detection should be focused. Health Sci. Rep. 2024, 7, e2004. [Google Scholar] [CrossRef]
- World Health Organization. Diabetes; WHO: Geneva, Switzerland, 2024; Available online: https://www.who.int/news-room/fact-sheets/detail/diabetes (accessed on 23 September 2025).
- Yapislar, H.; Gurler, E.B. Management of microcomplications of diabetes mellitus: Challenges, current trends, and future perspectives in treatment. Biomedicines 2024, 12, 1958. [Google Scholar] [CrossRef]
- Ahmad, F.J.; Joshi, S.H. Self-care practices and their role in the control of diabetes: A narrative review. Cureus 2023, 15, e41409. [Google Scholar] [CrossRef] [PubMed]
- International Organization for Migration. World Migration Report 2024; IOM: Geneva, Switzerland, 2024. [Google Scholar]
- Theodosopoulos, L.; Fradelos, E.C.; Panagiotou, A.; Dreliozi, A.; Tzavella, F. Delivering culturally competent care to migrants by healthcare personnel: A crucial aspect of culturally sensitive care. J. Nurs. Health Sci. 2024, 13, 530. [Google Scholar] [CrossRef]
- Stubbe, D.E. Practicing cultural competence and cultural humility in the care of diverse patients. Focus (Am. Phychiatr. Publ.) 2020, 18, 49–51. [Google Scholar] [CrossRef]
- Hassan, S.; Gujral, U.P.; Quarells, R.C.; Rhodes, E.C.; Shah, M.K.; Obi, J.; Lee, W.-H.; Shamambo, L.; Weber, M.B.; Narayan, K.M.V. Disparities in diabetes prevalence and management by race and ethnicity in the USA: Defining a path forward. Lancet Diabetes Endocrinol. 2023, 11, 509–524. [Google Scholar] [CrossRef]
- Taylor, Y.J.; Spencer, M.D.; Mahabaleshwarkar, R.; Ludden, T. Racial/ethnic differences in healthcare use among patients with uncontrolled and controlled diabetes. Ethn. Health 2017, 24, 245–256. [Google Scholar] [CrossRef]
- Cipta, D.A.; Andoko, D.; Theja, A.; Utama, A.V.E.; Hendrik, H.; William, D.G.; Reina, N.; Handoko, M.T.; Lumbuun, N. Culturally sensitive patient-centered healthcare: A focus on health behavior modification in low- and middle-income nations—Insights from Indonesia. Front. Med. 2024, 11, 1353037. [Google Scholar] [CrossRef]
- Rahimi, M.; Khodabandeh Shahraki, S.; Fatehi, F.; Farokhzadian, J. A virtual training program for improving cultural competence among academic nurse educators. BMC Med. Educ. 2023, 23, 4414. [Google Scholar] [CrossRef]
- Rissel, C.; Liddle, L.; Ryder, C.; Wilson, A.; Bower, M.; Richards, B. Impact evaluation of a Central Australian Aboriginal cultural awareness training program for health professionals and students. J. Aust. Indig. HealthInfoNet 2022, 3, 4. [Google Scholar] [CrossRef]
- Lin, M.H.; Hsu, H.C. Effects of a cultural competence education programme on clinical nurses: A randomised controlled trial. Nurse Educ. Today 2020, 88, 104385. [Google Scholar] [CrossRef]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Zeh, P.; Cannaby, A.M.; Sandhu, H.K.; Warwick, J.; Sturt, J.A. A cross-sectional survey of general practice health workers’ perceptions of their provision of culturally competent services to ethnic minority people with diabetes. Prim. Care Diabetes 2018, 12, 501–509. [Google Scholar] [CrossRef] [PubMed]
- Pettersson, S.; Holstein, J.; Jirwe, M.; Jaarsma, T.; Klompstra, L. Cultural competence in healthcare professionals specialised in diabetes working in primary healthcare: A descriptive study. Health Soc. Care Community 2022, 30, e13442. [Google Scholar] [CrossRef]
- Çınar, D.; Olgun, N.; Koyuncu, A. Investigation of the cultural competence levels of diabetes nurses. Clin. Exp. Health Sci. 2022, 12, 548–555. [Google Scholar] [CrossRef]
- Jager, M.; Leij-Halfwerk, S.; Akkermans, R.; Maria, R. Cultural competence training of dietitians: Development and preliminary evaluation. Prim. Health Care Res. Dev. 2024, 25, e48. [Google Scholar] [CrossRef]
- Movafagh, A.; Adams, S. The impact of a pharmacist-led cultural competence training on provider perceived preparedness and clinical care in patients with diabetes of Asian descent. J. Am. Pharm. Assoc. 2023, 25, e100912. [Google Scholar] [CrossRef]
- Kim, Y.K.; Lee, H. The effectiveness of a cultural competence training program for public health nurses using intervention mapping. J. Korean Acad. Community Health Nurs. 2016, 27, 410–418. [Google Scholar] [CrossRef]
- McElfish, P.A.; Long, C.R.; Rowland, B.; Moore, S.; Wilmoth, R.; Ayers, B. Improving culturally appropriate care using a community-based participatory research approach: Evaluation of a multicomponent cultural competency training program, Arkansas, 2015–2016. Prev. Chronic Dis. 2017, 14, E14. [Google Scholar] [CrossRef]
- Beck, P.; Matusiewicz, D.; Schouler-Ocak, M.; Khan, Z.; Peppler, L.; Schenk, L. Evaluation of cross-cultural competence among German healthcare professionals: A quasi-experimental study of training in two hospitals. Heliyon 2024, 10, e27331. [Google Scholar] [CrossRef]
- Ofosu, N.N.; Luig, T.; Mumtaz, N.; Chiu, Y.; Lee, K.K.; Yeung, R.O.; Campbell-Scherer, D.L. Health care providers’ perspectives on challenges and opportunities of intercultural health care in diabetes and obesity management: A qualitative study. Can. Med. Assoc. J. Open 2023, 11, E765–E773. [Google Scholar] [CrossRef] [PubMed]
- Jager, M.; den Boeft, A.; Leij-Halfwerk, S.; van der Sande, R.; van den Muijsenbergh, M. Cultural competency in dietetic diabetes care: A qualitative study of the dietitian’s perspective. Health Expect. 2020, 23, 540–548. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, M.; Bradette-Laplante, M.; Witteman, H.O.; Dogba, M.J.; Breault, P.; Paquette, J.; Careau, E.; Echaquan, S. Providing culturally safe care to Indigenous people living with diabetes: Identifying barriers and enablers from different perspectives. Health Expect. 2021, 24, 654–665. [Google Scholar] [CrossRef]
- Crowshoe, L.; Henderson, R.I.; Green, M.E.; Jacklin, K.M.; Walker, L.M.; Calam, B. Exploring Canadian physicians’ experiences with type 2 diabetes care for adult Indigenous patients. Can. J. Diabetes 2018, 42, 281–288. [Google Scholar] [CrossRef] [PubMed]
- Kaihlanen, A.M.; Hietapakka, L.; Heponiemi, T. Increasing cultural awareness: Qualitative study of nurses’ perceptions about cultural competence training. BMC Nurs. 2019, 18, 38. [Google Scholar] [CrossRef]
- Bhattacharyya, O.K.; Estey, E.A.; Rasooly, I.R.; Harris, S.; Zwarenstein, M.; Barnsley, J. Providers’ perceptions of barriers to the management of type 2 diabetes in remote Aboriginal settings. Int. J. Circumpolar Health 2011, 70, 552–563. [Google Scholar] [CrossRef]
- Caballero, A.E. Cultural competence in diabetes mellitus care: An urgent need. Insulin 2007, 2, 80–91. [Google Scholar] [CrossRef]
- McClimens, A.; Brewster, J.; Lewis, R. Recognising and respecting patients’ cultural diversity. Nurs. Stand. 2014, 28, 45–52. [Google Scholar] [CrossRef]
- Khanal, S.K. Language barriers and their consequences in healthcare: A qualitative case study of Nepali migrants in Finland. BMC Health Serv. Res. 2025, 25, 577. [Google Scholar] [CrossRef]
- Powell, D.L. Social determinants of health: Cultural competence is not enough. Creat. Nurs. 2016, 22, 5–10. [Google Scholar] [CrossRef]
- Horvat, L.; Horey, D.; Romios, P.; Kis-Rigo, J. Cultural competence education for health professionals. Cochrane Database Syst. Rev. 2014, 2014, CD009405. [Google Scholar] [CrossRef] [PubMed]
- Jettner, J.F.; Crawford, K.; Campbell, A.D.; Shackleford, K.; Bailey, B. Long-term effect on cultural competency: University study abroad service learning course in Belize. J. Soc. Work. Educ. 2025, 61, 424–440. [Google Scholar] [CrossRef]
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Articles published within the last ten years | Articles published more than ten years ago |
| Studies published in English | Studies issued in languages other than English |
| Research involving any health professionals | Research involving no health professional |
| Full-text articles that are available for review and analysis | Abstract-only publications or publications without access |
| Population | Interest | Context |
|---|---|---|
| (“healthcare professionals” OR “health workers” OR “nurses” OR “doctors” OR “clinicians” OR “medical staff”) | (“training” OR “education” OR “intervention” OR “program”) AND (“cultural competence” OR “cultural sensitivity” OR “cultural awareness” OR “cross-culture”) | (“diabetes” OR “diabetes mellitus” OR “diabetic care”) |
| Authors and Year | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 |
|---|---|---|---|---|---|---|---|---|
| Zeh, P., Cannaby, A.-M., Sandhu, H.K., Warwick, J. and Sturt, J.A. (2018) [16] | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | Yes |
| ÇINAR, D., OLGUN, N. and KOYUNCU, A. (2022) [18] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Pettersson, S., Holstein, J., Jirwe, M., Jaarsma, T. and Klompstra, L. (2022) [17] | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes |
| Jager, M., Leij-Halfwerk, S., Reinier Akkermans, Rob and Maria (2024) [19] | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | Yes |
| Movafagh, S and Adams. E (2024) [20] | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes |
| Authors and Year | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 |
|---|---|---|---|---|---|---|---|---|---|---|
| McElfish, P.A, Long, C.R, Rowland, B, Moore, S, R. Wilmoth, and B. Ayers (2017) [22] | Yes | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | Yes |
| Rissel, L. Liddle, C. Ryder, A. Wilson, M. Bower, and B. Richards (2022) [12] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Kim and H. Lee (2016) [21] | Yes | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | Yes |
| Authors and Year | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 |
|---|---|---|---|---|---|---|---|---|---|
| Beck P et al. (2024) [23] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes |
| Authors and Year | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lin M and Hsu H, (2020) [13] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes | Yes | Yes | Unclear |
| Authors and Year | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 |
|---|---|---|---|---|---|---|---|---|---|---|
| N. Ofosu, T. Luig, N. Mumtaz, Y. Chiu, K. Lee, R.O Yeung, and D.L. Campbell-Schere (2023) [24] | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | Yes | Yes |
| Jager M, den Boeft A, Leij-Halfwerk S, van der Sande R, van den Muijsenbergh M (2020) [25] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Tremblay, M., Bradette-Laplante, M., Witteman, H.O., Dogba, M.J., Breault, P., Paquette, J., Careau, E. and Echaquan, S. (2020) [26] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Kaihlanen, A.-M., Hietapakka, L. and Heponiemi, T. (2019) [28] | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | Yes | Yes |
| Crowshoe, L., Henderson, R.I., Green, M.E., Jacklin, K.M., Walker, L.M. and Calam, B. (2018) [27] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nikitara, M.; Mba, A.E.; Latzourakis, E.; Constantinou, C.S. Healthcare Professionals’ Cultural Competence in Diabetes Care: A Systematic Review. Healthcare 2025, 13, 2910. https://doi.org/10.3390/healthcare13222910
Nikitara M, Mba AE, Latzourakis E, Constantinou CS. Healthcare Professionals’ Cultural Competence in Diabetes Care: A Systematic Review. Healthcare. 2025; 13(22):2910. https://doi.org/10.3390/healthcare13222910
Chicago/Turabian StyleNikitara, Monica, Achonwa Esther Mba, Evangelos Latzourakis, and Costas S. Constantinou. 2025. "Healthcare Professionals’ Cultural Competence in Diabetes Care: A Systematic Review" Healthcare 13, no. 22: 2910. https://doi.org/10.3390/healthcare13222910
APA StyleNikitara, M., Mba, A. E., Latzourakis, E., & Constantinou, C. S. (2025). Healthcare Professionals’ Cultural Competence in Diabetes Care: A Systematic Review. Healthcare, 13(22), 2910. https://doi.org/10.3390/healthcare13222910







