Type-D Personality as a Predictor of Postoperative Pain, Recovery, and Clinical Outcomes After Spine Surgery: Implications for Chronic Pain Management
Abstract
1. Introduction
1.1. Type-D Personality
1.2. Relevance to Spine Surgery
1.3. Study Objective and Hypothesis
2. Materials and Methods
2.1. Participants
2.2. Assessment of Type-D Personality
2.3. Postoperative Outcomes
2.4. Statistical Analysis
2.5. Ethical Approval
3. Results
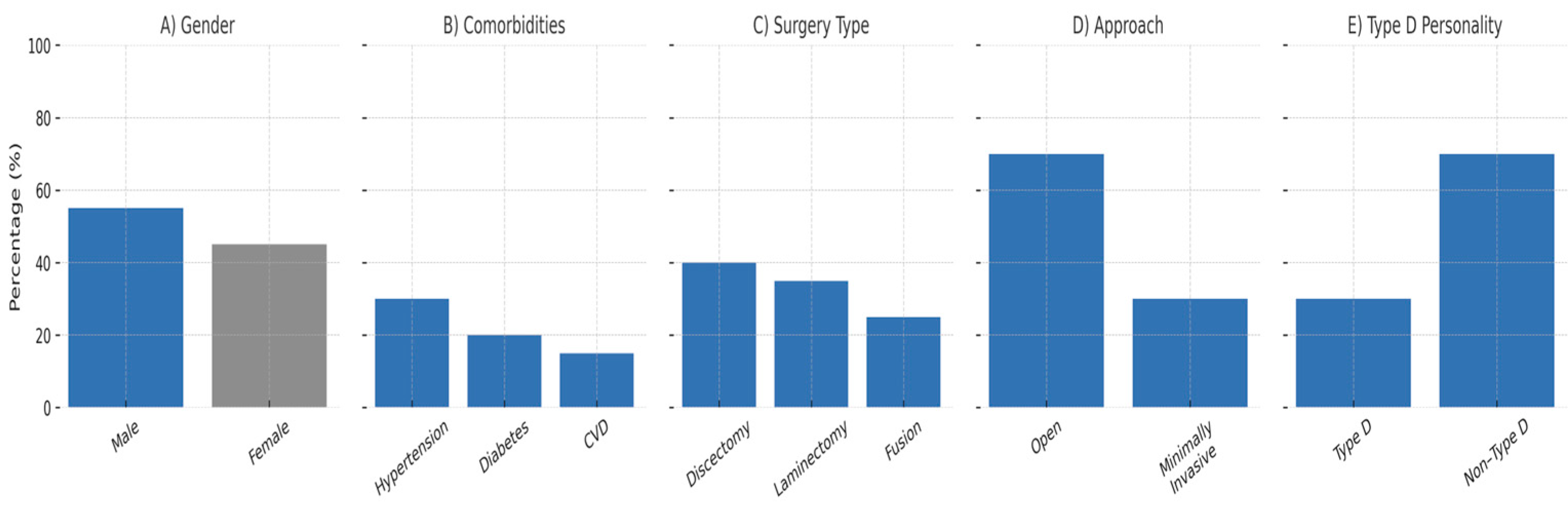
3.1. Patient Characteristics
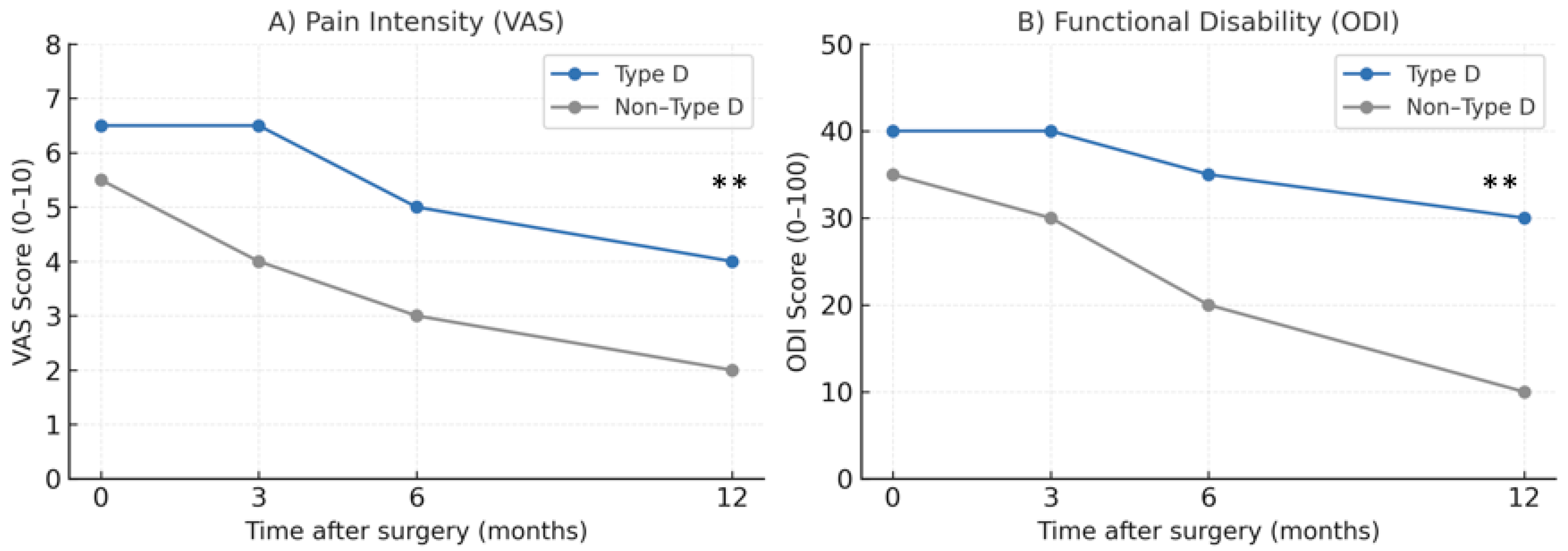
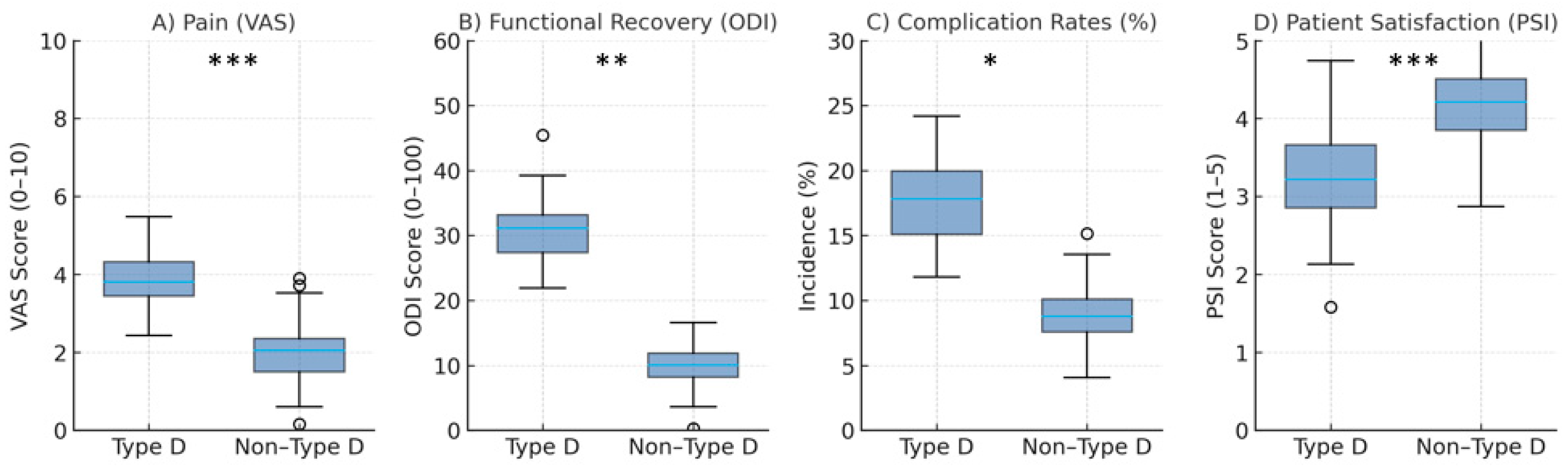
3.2. Pain and Functional Recovery
3.3. Complication Rates
3.4. Patient Satisfaction
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Denollet, J. DS14: Standard assessment of negative affectivity, social inhibition, and Type-D personality. Psychosom. Med. 2005, 67, 89–97. [Google Scholar] [CrossRef]
- Denollet, J.; Pedersen, S.S.; Ong, A.T.; Erdman, A.M.R.; Serruys, P.W.; Domburg, R.T.V. Social inhibition modulates the effect of negative emotions on cardiac prognosis following percutaneous coronary intervention in the drug-eluting stent era. Eur. Heart J. 2006, 27, 171–177. [Google Scholar] [CrossRef] [PubMed]
- Habra, M.E.; Linden, W.; Anderson, J.C.; Weinberg, J. Type D personality is related to cardiovascular and neuroendocrine reactivity to acute stress. J. Psychosom. Res. 2003, 55, 235–245. [Google Scholar] [CrossRef]
- Alshammari, H.S.; Alshammari, A.S.; Alshammari, S.A.; Ahamed, S.S. Prevalence of chronic pain after spinal surgery: A systematic review and meta-analysis. Cureus 2023, 15, e41841. [Google Scholar] [CrossRef]
- Ji, W.; Sang, C.; Zhang, X.; Zhu, K.; Bo, L. Personality, preoperative anxiety, and postoperative outcomes: A review. Int. J. Environ. Res. Public Health 2022, 19, 12162. [Google Scholar] [CrossRef]
- Hawker, G.A.; Mian, S.; Kendzerska, T.; French, M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res. 2011, 63, S240–S252. [Google Scholar] [CrossRef]
- Fairbank, J.C.; Couper, J.; Davies, J.B.; O’Brien, J.P. The Oswestry low back pain disability questionnaire. Physiotherapy 1980, 66, 271–273. [Google Scholar]
- Hinshaw, A.S.; Atwood, J.R. A Patient Satisfaction Instrument: Precision by replication. Nurs. Res. 1982, 31, 170–175, 191. [Google Scholar] [CrossRef]
- Vogel, M.; Riediger, C.; Krippl, M.; Frommer, J.; Lohmann, C.; Illiger, S. Negative affect, Type-D personality, quality of life, and dysfunctional outcomes of total knee arthroplasty. Pain. Res. Manag. 2019, 2019, 6393101. [Google Scholar] [CrossRef] [PubMed]
- Andersson, G.B. Epidemiological features of chronic low-back pain. Lancet 1999, 354, 581–585. [Google Scholar] [CrossRef] [PubMed]
- Sariyildiz, A.; Coskun Benlidayi, I.; Olmez Engizek, S.; Deniz, V. The relation of psychological status and Type-D personality with central sensitization in knee osteoarthritis: Everything is in your mind! Rheumatol. Int. 2023, 43, 2261–2269. [Google Scholar] [CrossRef] [PubMed]
- Denollet, J.; Conraads, V. Type-D personality and vulnerability to adverse outcomes in heart disease. Cleve Clin. J. Med. 2011, 78, 13–19. [Google Scholar] [CrossRef]
- Williams, L.; O’Connor, R.C.; Grubb, N.; O’Carroll, R.E. Type D personality and three-month psychosocial outcomes among patients post-myocardial infarction. J. Psychosom. Res. 2012, 72, 422–426. [Google Scholar] [CrossRef]
- Montfort van, E.; Mommersteeg, P.; Spek, V.; Kupper, N. Latent profiles of early trauma & Type D personality: Sex differences in cardiovascular risk markers. Compr. Psychiatry 2018, 83, 38–45. [Google Scholar] [CrossRef]
- Segerstrom, S.C.; Miller, G.E. Psychological stress and the human immune system: A meta-analytic study of 30 years of inquiry. Psychol. Bull. 2004, 130, 601–630. [Google Scholar] [CrossRef]
- Alanko, O.M.E.; Svedström-Oristo, A.L.; Tuomisto, M.T. Patients’ perceptions of orthognathic treatment, well-being, and psychological or psychiatric status: A systematic review. Acta Odontol. Scand. 2010, 68, 249–260. [Google Scholar] [CrossRef]
- Schiffer, A.A.; Denollet, J.; Widdershoven, J.W.; Hendriks, E.H.; Smith, O.R.F. Failure to consult for symptoms of heart failure in patients with a type-D personality. Heart 2007, 93, 814–818. [Google Scholar] [CrossRef]
- Linton, S.J.; Shaw, W.S. Impact of psychological factors in the experience of pain. Phys. Ther. 2011, 91, 700–711. [Google Scholar] [CrossRef]
- Majeed, M.H.; Ali, A.A.; Sudak, D.M. Mindfulness-based interventions for chronic pain: Evidence and applications. Asian J. Psychiatr. 2018, 32, 79–83. [Google Scholar] [CrossRef] [PubMed]
- Asadullah, H.; Abbasi, S.U.A.M.; Nabi, R. Integrating Mental Health in Perioperative Care: Addressing the Overlooked Impact of Chronic Stress and Depression on Surgical Outcomes. Can. J. Psychiatry 2025, 19, 07067437251340667. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Wang, L.Y.; Chen, Z.L.; Cao, X.Y.; Chen, B.Y. Cognitive behavioral therapy achieves better benefits in relieving postoperative pain and improving joint function: A systematic review and meta-analysis of randomized controlled trials. J. Orthop. Sci. 2024, 29, 681–689. [Google Scholar] [CrossRef] [PubMed]
- Sturgeon, J.A.; Zautra, A.J. Resilience: A new paradigm for adaptation to chronic pain. Curr. Pain Headache Rep. 2010, 14, 105–112. [Google Scholar] [CrossRef] [PubMed]
| Timepoint | Type-D (Mean ± SD) | Non-Type-D (Mean ± SD) | Difference/β | 95% CI | p-Value | Cohen’s d |
|---|---|---|---|---|---|---|
| Preoperative | 6.5 ± 1.0 | 5.5 ± 0.9 | β = 0.20 | −0.02–0.42 | 0.074 | 0.35 |
| 3 months | 6.5 ± 1.2 | 4.0 ± 1.0 | β = 0.38 | 0.22–0.55 | 0.001 | 0.72 |
| 6 months | 5.0 ± 1.1 | 3.0 ± 0.8 | β = 0.36 | 0.19–0.52 | 0.002 | 0.66 |
| 12 months | 4.0 ± 1.0 | 2.0 ± 0.7 | β = 0.34 | 0.18–0.52 | 0.004 | 0.61 |
| Timepoint | Type-D (Mean ± SD) | Non-Type-D (Mean ± SD) | Difference/β | 95% CI | p-Value | Cohen’s d |
|---|---|---|---|---|---|---|
| Preoperative | 40 ± 5 | 35 ± 5 | β = 0.15 | −0.05–0.34 | 0.142 | 0.30 |
| 3 months | 40 ± 6 | 30 ± 4 | β = 0.33 | 0.15–0.50 | 0.003 | 0.60 |
| 6 months | 35 ± 5 | 20 ± 3 | β = 0.32 | 0.14–0.49 | 0.004 | 0.59 |
| 12 months | 30 ± 4 | 10 ± 2 | β = 0.31 | 0.12–0.48 | 0.006 | 0.58 |
| Domain | Type-D (Mean ± SD) | Non-Type-D (Mean ± SD) | Difference/β | 95% CI | p-Value | Cohen’s d |
|---|---|---|---|---|---|---|
| Overall satisfaction | 3.2 ± 0.8 | 4.2 ± 0.6 | β = −0.36 | −0.49–−0.20 | <0.001 | 0.66 |
| Satisfaction with pain relief | 3.0 ± 0.8 | 4.0 ± 0.7 | β = −0.34 | −0.47–−0.18 | 0.001 | 0.62 |
| Satisfaction with functional recovery | 3.1 ± 0.7 | 4.1 ± 0.6 | β = −0.33 | −0.46–−0.17 | 0.002 | 0.60 |
| Satisfaction with surgical outcome | 3.3 ± 0.7 | 4.3 ± 0.6 | β = −0.35 | −0.48–−0.19 | 0.001 | 0.63 |
| Willingness to undergo surgery again | 3.2 ± 0.8 | 4.2 ± 0.7 | β = −0.34 | −0.47–−0.18 | 0.004 | 0.62 |
| Recommendation to others | 3.4 ± 0.8 | 4.4 ± 0.6 | β = −0.35 | −0.48–−0.19 | 0.002 | 0.63 |
| Dependent Variable | β (Type-D) | 95% CI | p | Adj. R2 | Covariates |
|---|---|---|---|---|---|
| Pain (VAS 12 mo) | 0.34 | 0.18–0.52 | 0.004 | 0.29 | Age, sex, comorbidities, surgery type |
| Function (ODI 12 mo) | 0.31 | 0.12–0.48 | 0.006 | 0.26 | Age, sex, comorbidities, surgery type |
| Satisfaction (PSI 12 mo) | −0.36 | −0.49–−0.20 | <0.001 | 0.31 | Age, sex, comorbidities, surgery type |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Riediger, C.; Ferl, M.; Lohmann, C.H.; Schönrogge, M.; Halm-Pozniak, A. Type-D Personality as a Predictor of Postoperative Pain, Recovery, and Clinical Outcomes After Spine Surgery: Implications for Chronic Pain Management. Healthcare 2025, 13, 2909. https://doi.org/10.3390/healthcare13222909
Riediger C, Ferl M, Lohmann CH, Schönrogge M, Halm-Pozniak A. Type-D Personality as a Predictor of Postoperative Pain, Recovery, and Clinical Outcomes After Spine Surgery: Implications for Chronic Pain Management. Healthcare. 2025; 13(22):2909. https://doi.org/10.3390/healthcare13222909
Chicago/Turabian StyleRiediger, Christian, Mark Ferl, Christoph H. Lohmann, Maria Schönrogge, and Agnieszka Halm-Pozniak. 2025. "Type-D Personality as a Predictor of Postoperative Pain, Recovery, and Clinical Outcomes After Spine Surgery: Implications for Chronic Pain Management" Healthcare 13, no. 22: 2909. https://doi.org/10.3390/healthcare13222909
APA StyleRiediger, C., Ferl, M., Lohmann, C. H., Schönrogge, M., & Halm-Pozniak, A. (2025). Type-D Personality as a Predictor of Postoperative Pain, Recovery, and Clinical Outcomes After Spine Surgery: Implications for Chronic Pain Management. Healthcare, 13(22), 2909. https://doi.org/10.3390/healthcare13222909








