Mini-Basketball for Preschool and School-Aged Children with Autism Spectrum Disorder: A Systematic Review of Randomized Controlled Trials
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Study Selection and Data Extraction
2.4. Quality Assessment
3. Results
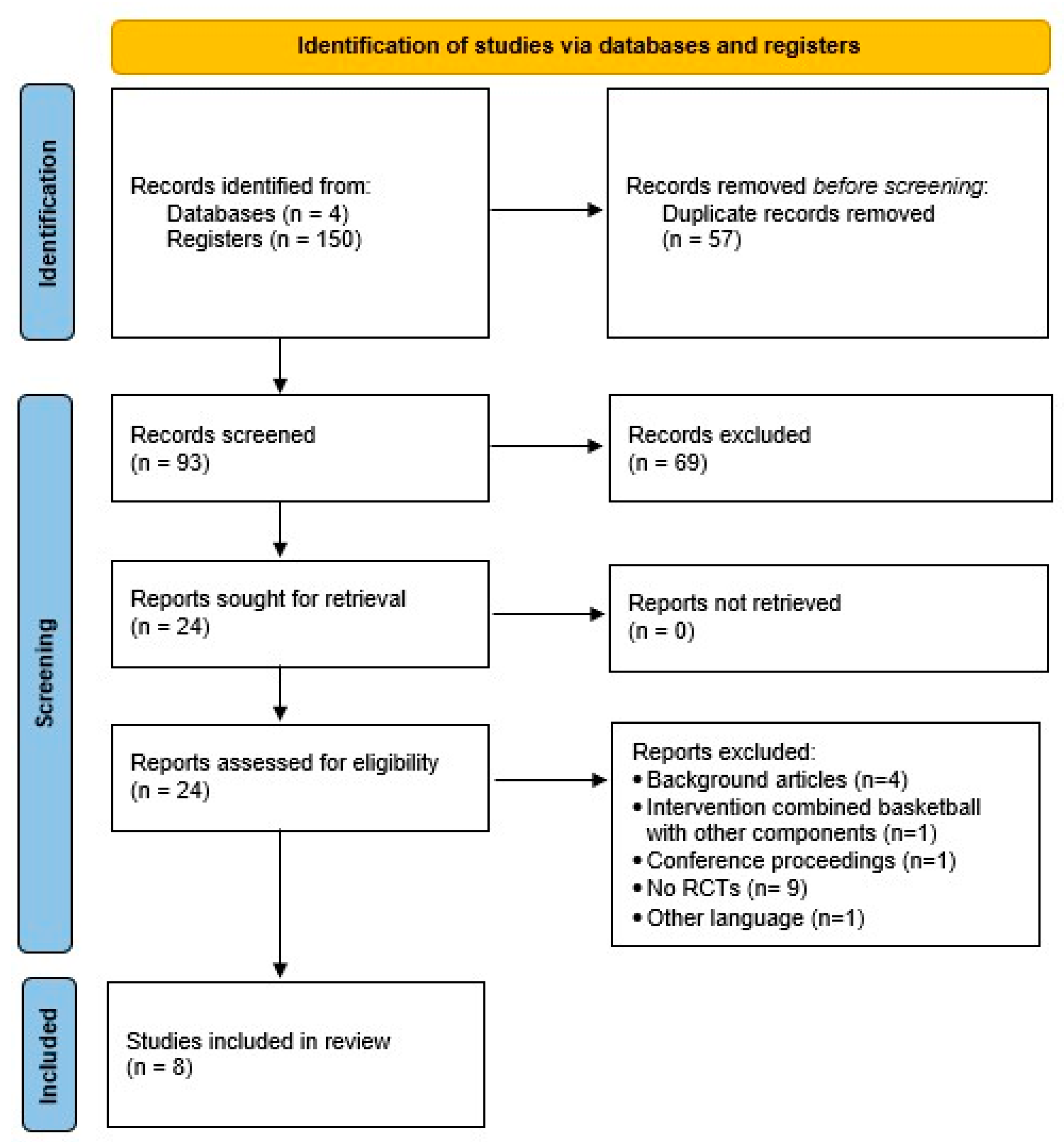
3.1. Study Selection and Screening Results
3.2. Quality Assessment Results
3.3. Study Design and Samples
3.4. Characteristics of Interventions
3.5. Main Results
3.5.1. Social Responsiveness
| First Author (Year), Design | Sample | Intervention | Outcomes | Results | Dropouts and Adverse Events |
|---|---|---|---|---|---|
| Zhang et al. (2025) [39] Country: China | Participants (n): 57 (30EG; 27CON) Final sample (n): 28 (15EG; 13CON) Sex: M Age, years (mean; SD): EG: 4.90 ± 0.66 CON: 4.77 ± 0.70 | Duration: 12 weeks Frequency: 5 days/week Volume: 40 min Intensity: Moderate EG: Mini-basketball program + ABA Activities: Typical exercise session had four sequential components, including introduction, warm-up activity, mini-basketball, and relaxation. CON: Maintained their regular routine + ABA. | Behavioral outcome measures:
| Intra-group (p < 0.05): ↑ Repetitive behavior scale (total score) in CON ↑ Restricted behavior in CON Inter-group (p < 0.05): EG < Repetitive behavior scale (total score) than CON EG < Self-injurious behavior than CON EG < Restricted behavior than CON | Dropouts: 29 EG: 15 did not complete the experiment CON: 12 did not complete the experiment; 2 missing T1-MPRAGE data Adverse events: NR |
| Yang et al. (2024) [34] Country: China | Participants (n): 59 (30EG; 29CON) Final sample (n): 30 (15EG; 15CON) Sex: EG: 13M/2F CON: 13M/2F Age, years (mean; SD): EG: 5.17 ± 0.72 CON: 4.67 ± 0.70 | Duration: 12 weeks Frequency: 5 days/week Volume: 40 min Intensity: Moderate; 128–148 bpm EG: Mini-basketball program + ABA Activities: Introduction, warm-up exercises, basketball intervention, and relaxation. CON: Maintained their regular routine + ABA. | Social Responsiveness:
| Intra-group (p < 0.05): ↓ Social responsiveness (total score) in EG ↓ Social communication (score) in EG ↓ Behavior pattern (score) in EG ↑ Social responsiveness (total score) in CON ↑ Social communication (score) in CON ↑ Behavior pattern (score) in CON Inter-group (p < 0.05): EG < Social responsiveness (total score) than CON EG < Social cognition (score) than CON EG < Social communication (score) than CON EG < Behavior pattern (score) than CON | Dropouts: 29 EG: 14 did not complete behavioral assessment 1 Did not complete rs-fMRI scan CON: 13 did not complete behavioral assessment 1 Did not complete rs-fMRI scan Adverse events: NR |
| Qi et al. (2024) [35] Country: China | Participants (n): 63 (20EG1; 23EG2; 20CON) Final sample (n): 41 (13EG1; 14EG2; 14CON) Sex: EG1: 10M/3F EG1: 12M/2F CON: 13M/1F Age, years (mean; SD): 4.99 ± 0.76 | Duration: 12 weeks Frequency: 5 days/week Volume: 40–45 min Intensity: Moderate; 128–148 bpm EG1: Ball combination training program + ABA Activities: Phases I–II: mini-basketball. Late Phase II: introduces soccer. Phase III: group games combining mini-basketball + soccer EG2: Mini-basketball program + ABA Activities: Exercise session had four sequential components, including introduction, warm-up, mini-basketball intervention, and cool-down. CON: Maintained their regular routine + ABA. | Social Responsiveness:
| Intra-group (p < 0.05): ↓ Social responsiveness (total score) in EG1 ↓ Social awareness (score) in EG1 ↓ Behavior pattern (score) in EG1 ↓ Social responsiveness (total score) in EG2 ↓ Social communication (score) in EG2 ↓ Social cognition (score) in EG2 ↑ Social responsiveness (total score) in CON ↑ Behavior pattern (score) in CON Inter-group (p < 0.05): EG1 and EG2 < Social responsiveness (total score) than CON EG1 < Social awareness (score) than CON EG1 < Behavior pattern (score) than CON EG2 < Social communication (score) than CON EG2 < Social cognition (score) than CON | Dropouts: 22 lost to follow-up EG1: 7 EG2: 9 CON: 6 Adverse events: NR |
| Ge et al. (2024) [41] Country: China | Participants (n): 49 (23EG; 26CON) Final sample (n): 30 (16EG; 14CON) Sex: EG: 15M/1F CON: 12M/2F Age, years (mean; SD): EG: 7.50 ± 2.19 CON: 6.64 ± 1.45 | Duration: 12 weeks Frequency: 5 days/week Volume: 40 min Intensity: Moderate; 128–148 bpm EG: Mini-basketball program + ABA Activities: 10 min warm-up with short games, a 25 min combining mini-basketball skills and fitness, and a 5 min cool-down. CON: Maintained their regular routine + ABA. | Joint Attention:
| Intra-group (p < 0.05): ↑ Time to first fixation in CON ↓ Accurate gaze shifts count in CON Inter-group (p < 0.05): EG > AOI fixation count than CON EG < Time to first fixation than CON EG > Accurate gaze shifts count than CON EG > Accurate-to-inaccurate gaze shift ratio than CON | Dropouts: 19 EG: 1 did not complete post-test 3 missing MRI data 1 excessive head motion 2 missing behavioral data CON: 7 due to the impact of COVID-19 epidemic 4 missing MRI data 1 excessive head motion Adverse events: NR |
| Yu et al. (2021) [36] Country: China | Participants (n): 40 (20EG; 20CON) Final sample (n): 31 (17EG; 14CON) Sex: EG: 15M/2F CON: 13M/2F Age, years (mean; SD): EG: 4.89 ± 0.80 CON: 4.75 ± 0.62 | Duration: 12 weeks Frequency: 5 days/week Volume: 40 min Intensity: 136.97 ± 7.45 bpm EG: Mini-basketball program Activities: Including a 2 min classroom routine preparation, then 8 min warm-up activities, followed by a 25 min mini-basketball training and a 5 min cool-down. CON: Maintained their regular routine. | Social Responsiveness:
| Intra-group (p < 0.05): ↓ Social responsiveness (total score) in EG ↓ Social cognition (score) in EG ↓ Social communication (score) in EG ↑ Social responsiveness (total score) in CON ↑ Social communication (score) in CON ↑ Behavior pattern (score) in CON Inter-group (p < 0.05): EG < Social responsiveness (total score) than CON EG < Social communication (score) than CON EG < Social cognition (score) than CON EG < Behavior pattern (score) than CON | Dropouts: 9 6 missing MRI data 3 inferior images not suitable for analysis EG: 3 CON: 6 Adverse events: NR |
| Yang et al. (2021) [38] Country: China | Participants (n): 59 (30EG; 29CON) Final sample (n): 30 (15EG; 15CON) Sex: EG: 13M/2F CON: 12M/3F Age, years (mean; SD): EG: 4.67 ± 0.70 CON: 5.03 ± 0.55 | Duration: 12 weeks Frequency: 5 days/week Volume: 40 min Intensity: 60–69% HRpeak EG: Mini-basketball program Activities: Start (lining up, roll call, and greetings), warm-up (light jogging, stretching, and general limb mobility), intervention—comprising three consecutive stages: (1) basic basketball training, (2) instruction in specific mini-basketball skills, and (3) a mini-basketball game—and cool-down. CON: Maintained their regular routine and usual care. | Social Responsiveness:
| Intra-group (p < 0.05): ↓ Social cognition (score) in EG ↑ Social responsiveness (total score) in CON ↑ Social communication (score) in CON Inter-group (p < 0.05): EG < Social responsiveness (total score) than CON EG < Social communication (score) than CON EG < Social cognition (score) than CON | Dropouts: 29 lost to follow-up EG: 15 CON: 14 Adverse events: NR |
| Cai et al. (2019) [37] Country: China | Participants (n): 59 (30EG; 29CON) Final sample (n): 30 (15EG; 15CON) Sex: EG: 12M/3F CON: 14M/1F Age, years (mean; SD): EG: 5.03 ± 0.64 CON: 4.56 ± 0.84 | Duration: 12 weeks Frequency: 5 days/week Volume: 40 min Intensity: NR EG: Mini-basketball program Activities: 5 min warm-up; (b) 20 min basic basketball skill instruction; (c) 10 min basketball game; (d) 5 min cool-down. CON: Maintained their regular routine. | Social Responsiveness:
| Intra-group (p < 0.05): ↓ Social responsiveness (total score) in EG ↓ Social cognition (score) in EG ↓ Social communication (score) in EG ↑ Social responsiveness (total score) in CON ↑ Social communication (score) in CON ↑ Behavior pattern (score) in CON ↓ 2 × 10 m shuttle run time in EG ↑ Standing long jump in EG Inter-group (p < 0.05): EG < Social responsiveness (total score) than CON EG < Social awareness (score) than CON EG < Social communication (score) than CON EG < Social cognition (score) than CON EG < Behavior pattern (score) than CON EG < 2 × 10 m shuttle run time than CON EG ˃ Standing long jump than CON | Dropouts: 29 lost to follow-up EG: 15 CON: 14 Adverse events: NR |
| Tse et al. (2019) [40] Country: China | Participants (n): 50 (25EG; 25CON) Final sample (n): 40 (19EG; 21CON) Sex: EG: 14M/5F CON: 18M/3F Age, years (mean; SD): EG: 10.11 ± 1.20 CON: 9.81 ± 1.17 | Duration: 12 weeks Frequency: 2 days/week Volume: 44 min Intensity: NR EG: Basketball skill-learning intervention Activities: Warm-up (10 min); basketball instruction (30 min) to learn different basketball skills; cool-down (5 min). CON: Did not receive any intervention and were asked to follow their daily routine without taking part in any additional physical exercise program. | Self-reported sleep quality (parent-reported sleep log):
| Intra-group (p < 0.05) ↑ Sleep duration after intervention on weekday (actigraphy and sleep log) and weekend (actigraphy) in EG ↓ Sleep duration after intervention on weekday (actigraphy and sleep log) and weekend (sleep log) in CON ↑ Sleep efficiency after intervention on weekday and weekend in EG (actigraphy and sleep log) ↓ Sleep efficiency after intervention on weekday (actigraphy) and weekend (sleep log) in CON ↓ Wake after sleep onset after intervention on weekday and weekend in EG (actigraphy and sleep log) ↑ Wake after sleep onset after intervention on weekday in CON (actigraphy) ↓ Inhibition control (false alarm error) in EG Inter-group (p < 0.05) EG > Sleep duration compared to CON after intervention on weekday (actigraphy) and weekend (actigraphy and sleep log) EG > Sleep efficiency in compared to CON after intervention on weekday and weekend (actigraphy and sleep log) EG < Wake after sleep onset compared to CON after intervention on weekday and weekend (actigraphy and sleep log) EG < Inhibition control (false alarm error) than CON | Dropouts: 10 Due to incompletion of assessments EG: 6 CON: 4 Adverse events: NR |
3.5.2. Behavioral Outcome Measures
3.5.3. Joint Attention (Eye-Tracking)
3.5.4. Physical Fitness
3.5.5. Neuropsychological Measures
3.5.6. Sleep Quality
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Washington, DC, USA, 2013. [Google Scholar]
- Wilson, A.C. Cognitive Profile in Autism and ADHD: A Meta-Analysis of Performance on the WAIS-IV and WISC-V. Arch. Clin. Neuropsychol. 2024, 39, 498–515. [Google Scholar] [CrossRef] [PubMed]
- Donovan, A.P.A.; Basson, M.A. The Neuroanatomy of Autism—A Developmental Perspective. J. Anat. 2017, 230, 4–15. [Google Scholar] [CrossRef] [PubMed]
- O’Reilly, C.; Lewis, J.D.; Elsabbagh, M. Is Functional Brain Connectivity Atypical in Autism? A Systematic Review of EEG and MEG Studies. PLoS ONE 2017, 12, e0175870. [Google Scholar] [CrossRef]
- Zhou, M.S.; Nasir, M.; Farhat, L.C.; Kook, M.; Artukoglu, B.B.; Bloch, M.H. Meta-Analysis: Pharmacologic Treatment of Restricted and Repetitive Behaviors in Autism Spectrum Disorders. J. Am. Acad. Child Adolesc. Psychiatry 2021, 60, 35–45. [Google Scholar] [CrossRef]
- Alfageh, B.H.; Wang, Z.; Mongkhon, P.; Besag, F.M.C.; Alhawassi, T.M.; Brauer, R.; Wong, I.C.K. Safety and Tolerability of Antipsychotic Medication in Individuals with Autism Spectrum Disorder: A Systematic Review and Meta-Analysis. Pediatr. Drugs 2019, 21, 153–167. [Google Scholar] [CrossRef]
- Salazar De Pablo, G.; Pastor Jordá, C.; Vaquerizo-Serrano, J.; Moreno, C.; Cabras, A.; Arango, C.; Hernández, P.; Veenstra-VanderWeele, J.; Simonoff, E.; Fusar-Poli, P.; et al. Systematic Review and Meta-Analysis: Efficacy of Pharmacological Interventions for Irritability and Emotional Dysregulation in Autism Spectrum Disorder and Predictors of Response. J. Am. Acad. Child Adolesc. Psychiatry 2023, 62, 151–168. [Google Scholar] [CrossRef]
- Chen, Y.-C.B.; Lin, H.-Y.; Wang, L.-J.; Hung, K.-C.; Brunoni, A.R.; Chou, P.-H.; Tseng, P.-T.; Liang, C.-S.; Tu, Y.-K.; Lin, P.-Y.; et al. A Network Meta-Analysis of Non-Invasive Brain Stimulation Interventions for Autism Spectrum Disorder: Evidence from Randomized Controlled Trials. Neurosci. Biobehav. Rev. 2024, 164, 105807. [Google Scholar] [CrossRef]
- Huang, J.; Du, C.; Liu, J.; Tan, G. Meta-Analysis on Intervention Effects of Physical Activities on Children and Adolescents with Autism. IJERPH 2020, 17, 1950. [Google Scholar] [CrossRef]
- Healy, S.; Nacario, A.; Braithwaite, R.E.; Hopper, C. The Effect of Physical Activity Interventions on Youth with Autism Spectrum Disorder: A Meta-analysis. Autism Res. 2018, 11, 818–833. [Google Scholar] [CrossRef]
- Monteiro, C.E.; Da Silva, E.; Sodré, R.; Costa, F.; Trindade, A.S.; Bunn, P.; Costa E Silva, G.; Di Masi, F.; Dantas, E. The Effect of Physical Activity on Motor Skills of Children with Autism Spectrum Disorder: A Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 14081. [Google Scholar] [CrossRef]
- Liang, X.; Haegele, J.A.; Healy, S.; Tse, A.C.-Y.; Qiu, H.; Zhao, S.; Li, C. Age-Related Differences in Accelerometer-Assessed Physical Activity and Sleep Parameters Among Children and Adolescents With and Without Autism Spectrum Disorder: A Meta-Analysis. JAMA Netw. Open 2023, 6, e2336129. [Google Scholar] [CrossRef]
- Liang, X.; Haegele, J.A.; Tse, A.C.-Y.; Li, M.; Zhang, H.; Zhao, S.; Li, S.X. The Impact of the Physical Activity Intervention on Sleep in Children and Adolescents with Autism Spectrum Disorder: A Systematic Review and Meta-Analysis. Sleep Med. Rev. 2024, 74, 101913. [Google Scholar] [CrossRef] [PubMed]
- Tao, R.; Yang, Y.; Wilson, M.; Chang, J.R.; Liu, C.; Sit, C.H.P. Comparative Effectiveness of Physical Activity Interventions on Cognitive Functions in Children and Adolescents with Neurodevelopmental Disorders: A Systematic Review and Network Meta-Analysis of Randomized Controlled Trials. Int. J. Behav. Nutr. Phys. Act. 2025, 22, 6. [Google Scholar] [CrossRef] [PubMed]
- Sung, M.-C.; Ku, B.; Leung, W.; MacDonald, M. The Effect of Physical Activity Interventions on Executive Function Among People with Neurodevelopmental Disorders: A Meta-Analysis. J. Autism Dev. Disord. 2022, 52, 1030–1050. [Google Scholar] [CrossRef]
- Wang, S.; Chen, D.; Yang, Y.; Zhu, L.; Xiong, X.; Chen, A. Effectiveness of Physical Activity Interventions for Core Symptoms of Autism Spectrum Disorder: A Systematic Review and Meta-analysis. Autism Res. 2023, 16, 1811–1824. [Google Scholar] [CrossRef]
- Ferreira, J.P.; Ghiarone, T.; Cabral Júnior, C.R.; Furtado, G.E.; Moreira Carvalho, H.; Machado-Rodrigues, A.M.; Andrade Toscano, C.V. Effects of Physical Exercise on the Stereotyped Behavior of Children with Autism Spectrum Disorders. Medicina 2019, 55, 685. [Google Scholar] [CrossRef]
- Kou, R.; Li, Z.; Li, M.; Zhou, R.; Zhu, F.; Ruan, W.; Zhang, J. Comparative Effectiveness of Physical Exercise Interventions on Sociability and Communication in Children and Adolescents with Autism: A Systematic Review and Network Meta-Analysis. BMC Psychol. 2024, 12, 712. [Google Scholar] [CrossRef]
- Rosales, M.R.; Butera, C.D.; Wilson, R.B.; Zhou, J.; Maus, E.; Zhao, H.; Chow, J.C.; Dao, A.; Freeman, J.; Dusing, S.C. Systematic Review and Meta-Analysis of the Effect of Motor Intervention on Cognition, Communication, and Social Interaction in Children with Autism Spectrum Disorder. Phys. Occup. Ther. Pediatr. 2025, 45, 688–710. [Google Scholar] [CrossRef]
- He, J.; Gong, Y.; Yin, M.; Zhang, L.; Wu, X. Optimal Dosage of Group-Based Organized Physical Activity for Enhancing Social Abilities in Autistic Children: Insights from a Multilevel Meta-Analysis. Int. J. Behav. Nutr. Phys. Act. 2025, 22, 87. [Google Scholar] [CrossRef]
- Howells, K.; Sivaratnam, C.; May, T.; Lindor, E.; McGillivray, J.; Rinehart, N. Efficacy of Group-Based Organised Physical Activity Participation for Social Outcomes in Children with Autism Spectrum Disorder: A Systematic Review and Meta-Analysis. J. Autism Dev. Disord. 2019, 49, 3290–3308. [Google Scholar] [CrossRef]
- O’Flahert, M.; Hill, J.; Bourke, M.; Gomersall, L.; Tweedy, S.; Cairney, J. Comparing Trajectories of Sport Participation for Autistic- and Non-Autistic-Youth: A Group-Based Multi-Trajectory Modelling Approach. Autism 2025, 29, 2575–2587. [Google Scholar] [CrossRef] [PubMed]
- Vetri, L.; Roccella, M. On the Playing Field to Improve: A Goal for Autism. Medicina 2020, 56, 585. [Google Scholar] [CrossRef] [PubMed]
- Howells, K.; Sivaratnam, C.; Lindor, E.; Hyde, C.; McGillivray, J.; Whitehouse, A.; Rinehart, N. Can Participation in a Community Organized Football Program Improve Social, Behavioural Functioning and Communication in Children with Autism Spectrum Disorder? A Pilot Study. J. Autism Dev. Disord. 2020, 50, 3714–3727. [Google Scholar] [CrossRef] [PubMed]
- Howells, K.; Sivaratnam, C.; Lindor, E.; He, J.; Hyde, C.; McGillivray, J.; Wilson, R.B.; Rinehart, N. Can a Community-Based Football Program Benefit Motor Ability in Children with Autism Spectrum Disorder? A Pilot Evaluation Considering the Role of Social Impairments. J. Autism Dev. Disord. 2022, 52, 402–413. [Google Scholar] [CrossRef]
- Hou, Y.; Wang, Y.; Deng, J.; Song, X. Effects of Different Exercise Interventions on Executive Function in Children with Autism Spectrum Disorder: A Network Meta-Analysis. Front. Psychiatry 2024, 15, 1440123. [Google Scholar] [CrossRef]
- Stachura, K.; Emich-Widera, E.; Kazek, B.; Stania, M. Coordination, Balance and Fine Motor Skills Deficities in Children with Autism Spectrum Disorder Without Co-Occuring Conditions-Application of MABC-2 Test in Pilot Study Among Polish Children. J. Clin. Med. 2025, 14, 4946. [Google Scholar] [CrossRef]
- Wang, J.-G.; Cai, K.-L.; Liu, Z.-M.; Herold, F.; Zou, L.; Zhu, L.-N.; Xiong, X.; Chen, A.-G. Effects of Mini-Basketball Training Program on Executive Functions and Core Symptoms among Preschool Children with Autism Spectrum Disorders. Brain Sci. 2020, 10, 263. [Google Scholar] [CrossRef]
- Fotrousi, F.; Bagherly, J.; Ghasemi, A. The Compensatory Impact of Mini-Basketball Skills on the Progress of Fundamental Movements in Children. Procedia—Soc. Behav. Sci. 2012, 46, 5206–5210. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Rico-González, M.; Pino-Ortega, J.; Clemente, F.M.; Los Arcos, A. Guidelines for Performing Systematic Reviews in Sports Science. Biol. Sport. 2022, 39, 463–471. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a Web and Mobile App for Systematic Reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Silverman, S.R.; Schertz, L.A.; Yuen, H.K.; Lowman, J.D.; Bickel, C.S. Systematic Review of the Methodological Quality and Outcome Measures Utilized in Exercise Interventions for Adults with Spinal Cord Injury. Spinal Cord 2012, 50, 718–727. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Chen, D.; Cai, K.; Zhu, L.; Shi, Y.; Dong, X.; Sun, Z.; Qiao, Z.; Yang, Y.; Zhang, W.; et al. Effects of Mini-Basketball Training Program on Social Communication Impairments and Regional Homogeneity of Brain Functions in Preschool Children with Autism Spectrum Disorder. BMC Sports Sci. Med. Rehabil. 2024, 16, 92. [Google Scholar] [CrossRef] [PubMed]
- Qi, K.; Liu, Y.; Wang, Z.; Xiong, X.; Cai, K.; Xu, Y.; Shi, Y.; Sun, Z.; Dong, X.; Chen, A. Recreational Ball Games Are Effective in Improving Social Communication Impairments among Preschoolers Diagnosed with Autism Spectrum Disorder: A Multi-Arm Controlled Study. BMC Sports Sci. Med. Rehabil. 2024, 16, 176. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Qu, H.; Chen, A.; Du, Y.; Liu, Z.; Wang, W. Alteration of Effective Connectivity in the Default Mode Network of Autism After an Intervention. Front. Neurosci. 2021, 15, 796437. [Google Scholar] [CrossRef]
- Cai, K.L.; Wang, J.G.; Liu, Z.M.; Zhu, L.N.; Xiong, X.; Klich, S.; Maszczyk, A.; Chen, A.G. Mini-Basketball Training Program Improves Physical Fitness and Social Communication in Preschool Children with Autism Spectrum Disorders. J. Hum. Kinet. 2020, 73, 267–278. [Google Scholar] [CrossRef]
- Yang, S.; Liu, Z.; Xiong, X.; Cai, K.; Zhu, L.; Dong, X.; Wang, J.; Zhu, H.; Shi, Y.; Chen, A. Effects of Mini-Basketball Training Program on Social Communication Impairment and Executive Control Network in Preschool Children with Autism Spectrum Disorder. Int. J. Environ. Res. Public Health 2021, 18, 5132. [Google Scholar] [CrossRef]
- Zhang, W.; Cai, K.; Xiong, X.; Zhu, L.; Sun, Z.; Yang, S.; Cheng, W.; Mao, H.; Chen, A. Alterations of Triple Network Dynamic Connectivity and Repetitive Behaviors after Mini-Basketball Training Program in Children with Autism Spectrum Disorder. Sci. Rep. 2025, 15, 2629. [Google Scholar] [CrossRef]
- Tse, C.Y.A.; Lee, H.P.; Chan, K.S.K.; Edgar, V.B.; Wilkinson-Smith, A.; Lai, W.H.E. Examining the Impact of Physical Activity on Sleep Quality and Executive Functions in Children with Autism Spectrum Disorder: A Randomized Controlled Trial. Autism 2019, 23, 1699–1710. [Google Scholar] [CrossRef]
- Ge, L.K.; Man, X.; Cai, K.; Liu, Z.; Tsang, W.W.; Chen, A.; Wei, G.X. Sharing Our World: Impact of Group Motor Skill Learning on Joint Attention in Children with Autism Spectrum Disorder. J. Autism Dev. Disord. 2024. [Google Scholar] [CrossRef]
- Wang, Y.; Qian, G.; Mao, S.; Zhang, S. The Impact of Physical Exercise Interventions on Social, Behavioral, and Motor Skills in Children with Autism: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Front. Pediatr. 2025, 13, 1475019. [Google Scholar] [CrossRef]
- Ruggeri, A.; Dancel, A.; Johnson, R.; Sargent, B. The Effect of Motor and Physical Activity Intervention on Motor Outcomes of Children with Autism Spectrum Disorder: A Systematic Review. Autism 2020, 24, 544–568. [Google Scholar] [CrossRef]
| Data Base | Search Strategy | Results |
|---|---|---|
| Web Of Science | TS ((“basketball” OR “mini-basketball”) AND (“autis*” OR “autism spectrum disorder” OR “ASD” OR “autist*”)) | 44 |
| Scopus | TITLE-ABS-KEY ((“basketball” OR “mini-basketball”) AND (“autis*” OR “autism spectrum disorder” OR “ASD” OR “autist*”)) | 49 |
| SPORTDiscus | (“basketball” OR “mini-basketball”) AND (“autis*” OR “autism spectrum disorder” OR “ASD” OR “autist*”) | 32 |
| MEDLINE/ PubMed | (“basketball” OR “mini-basketball”) AND (“autis*” OR “autism spectrum disorder” OR “ASD” OR “autist*”) | 25 |
| TOTAL | 150 | |
| Authors (Year) | Items | Quality Rating | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Score | ||
| Yang et al. (2024) [34] | Y | + | − | + | − | − | − | − | − | + | + | 4/10 | Fair |
| Qi et al. (2024) [35] | Y | + | − | + | − | − | + | − | − | + | + | 5/10 | Fair |
| Yu et al. (2021) [36] | Y | + | − | + | − | − | − | − | − | + | + | 4/10 | Fair |
| Cai et al. (2019) [37] | Y | + | − | + | − | − | − | − | − | + | + | 4/10 | Fair |
| Yang et al. (2021) [38] | Y | + | − | + | − | − | − | − | − | + | + | 4/10 | Fair |
| Zhang et al. (2025) [39] | Y | + | − | + | − | − | − | − | − | + | + | 4/10 | Fair |
| Tse et al. (2019) [40] | Y | + | − | + | − | − | + | + | − | + | + | 6/10 | Good |
| Ge et al. (2024) [41] | Y | + | + | + | − | − | + | − | − | + | + | 6/10 | Good |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
González-Devesa, D.; Zhou, R.; Rico-González, M.; Gómez-Carmona, C.D. Mini-Basketball for Preschool and School-Aged Children with Autism Spectrum Disorder: A Systematic Review of Randomized Controlled Trials. Healthcare 2025, 13, 2861. https://doi.org/10.3390/healthcare13222861
González-Devesa D, Zhou R, Rico-González M, Gómez-Carmona CD. Mini-Basketball for Preschool and School-Aged Children with Autism Spectrum Disorder: A Systematic Review of Randomized Controlled Trials. Healthcare. 2025; 13(22):2861. https://doi.org/10.3390/healthcare13222861
Chicago/Turabian StyleGonzález-Devesa, Daniel, Rui Zhou, Markel Rico-González, and Carlos D. Gómez-Carmona. 2025. "Mini-Basketball for Preschool and School-Aged Children with Autism Spectrum Disorder: A Systematic Review of Randomized Controlled Trials" Healthcare 13, no. 22: 2861. https://doi.org/10.3390/healthcare13222861
APA StyleGonzález-Devesa, D., Zhou, R., Rico-González, M., & Gómez-Carmona, C. D. (2025). Mini-Basketball for Preschool and School-Aged Children with Autism Spectrum Disorder: A Systematic Review of Randomized Controlled Trials. Healthcare, 13(22), 2861. https://doi.org/10.3390/healthcare13222861







