Spinal Cord Injury Epidemiology and Causes: A Worldwide Analysis with 2050 Projections
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Overview
2.2. Data Sources and Collection
2.3. Definition of Case and Causes
2.4. Modeling and Data Processing
2.5. Risk Estimation
2.6. Estimation of Future Prevalence
3. Results
3.1. Global Prevalence in 2021
3.2. Regional Variation in Prevalence
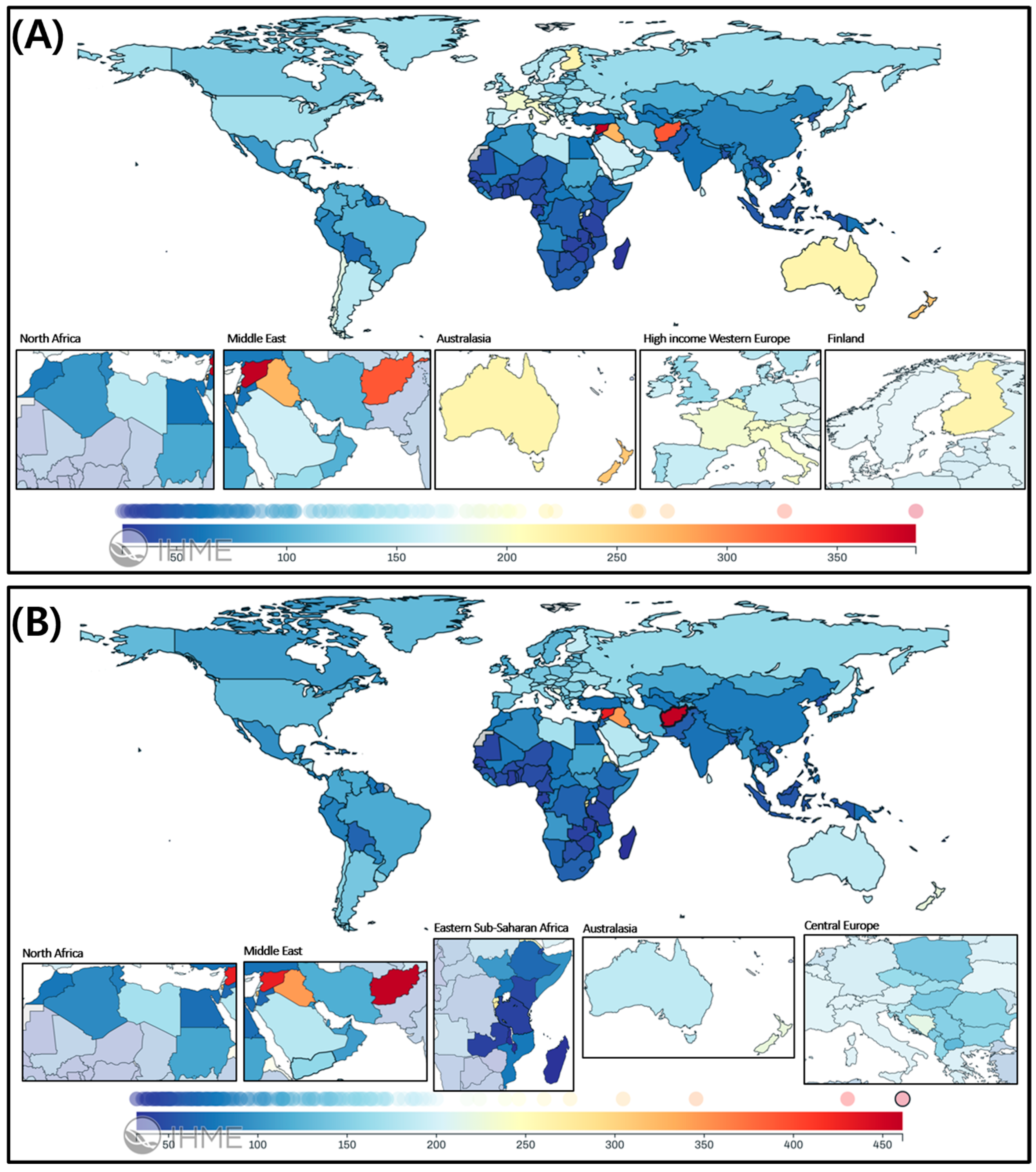
3.2.1. Neck-Level SCI
3.2.2. Below-Neck-Level SCI
3.2.3. Country-Level Prevalence and YLDs for SCI
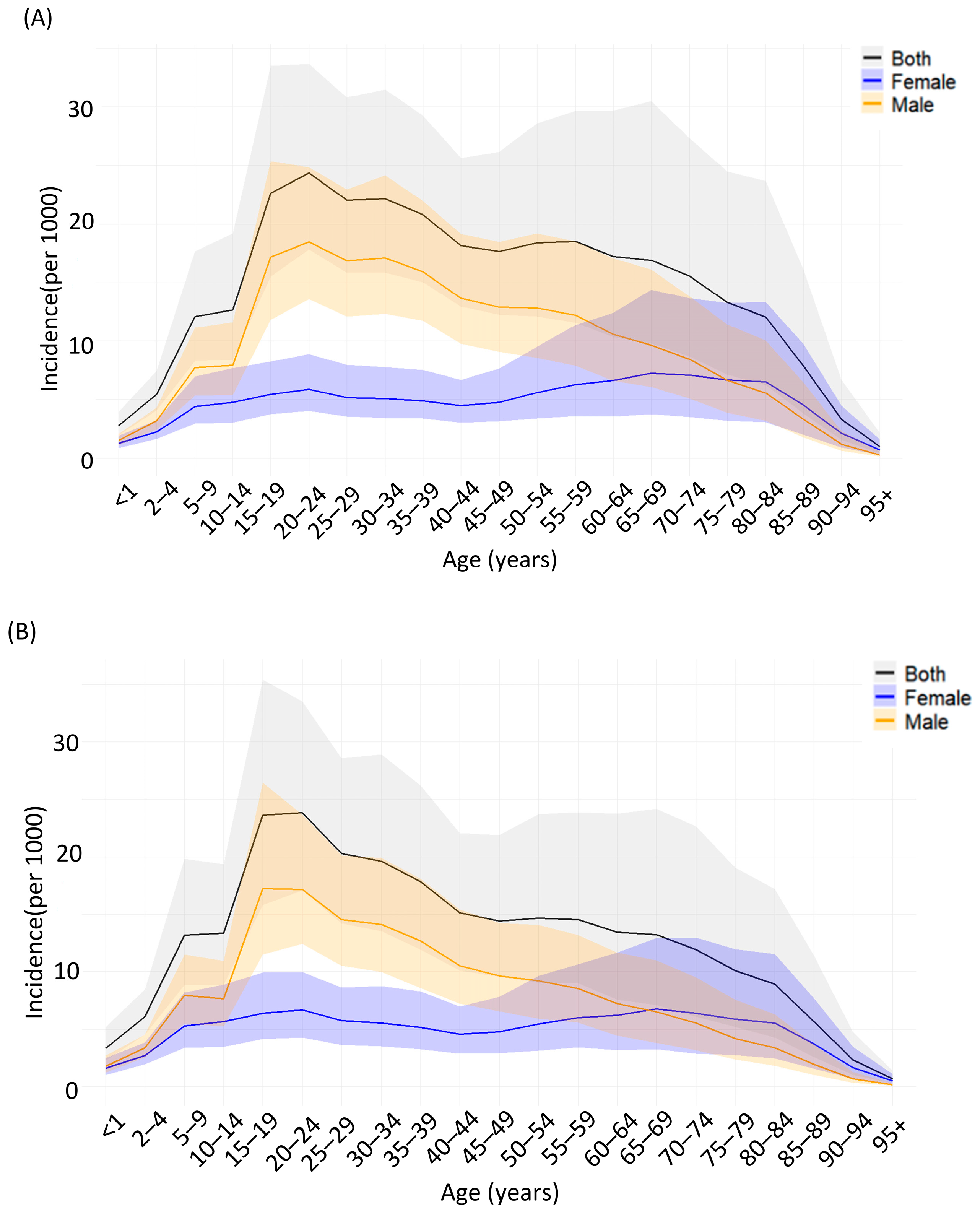
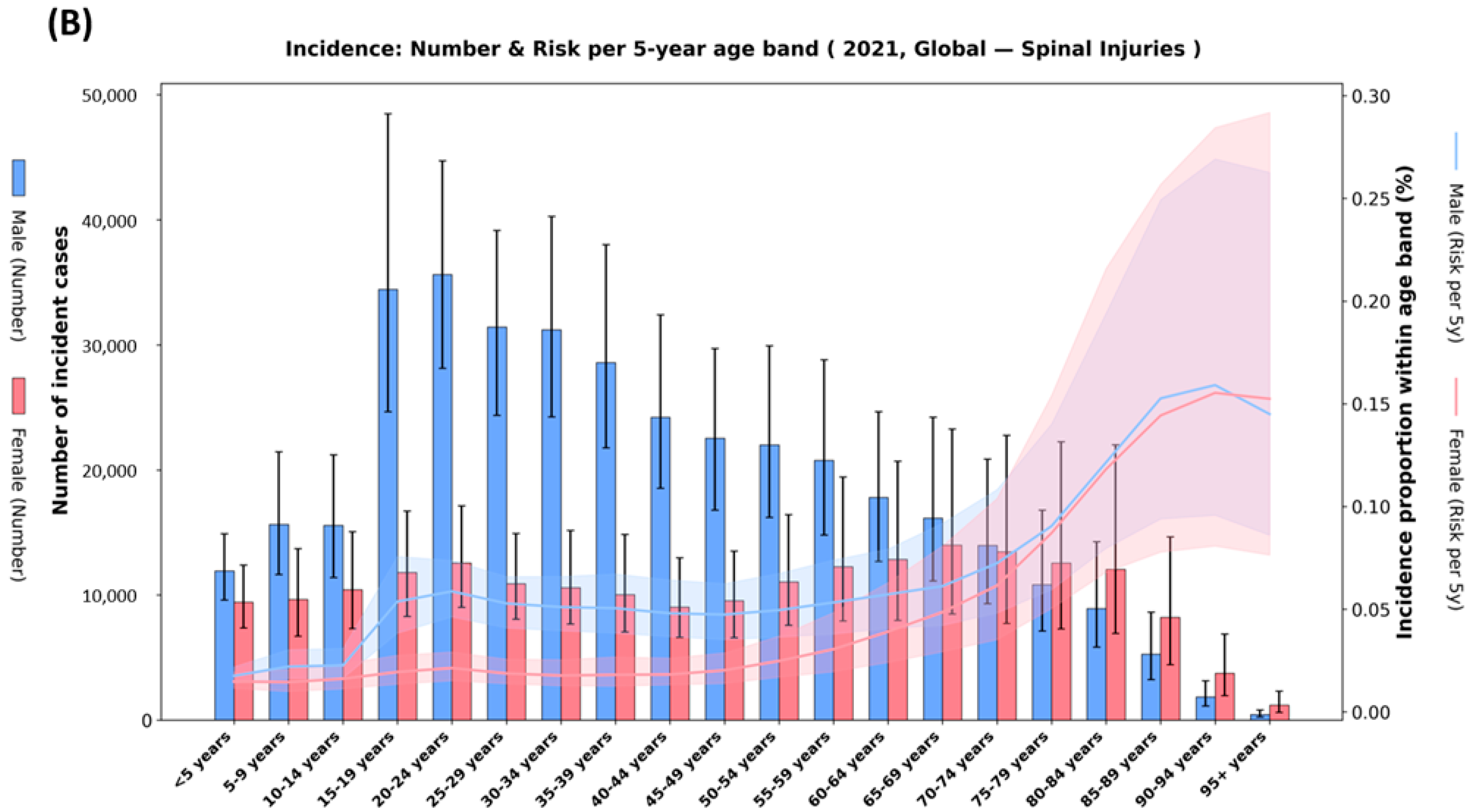
3.2.4. Age- and Sex-Specific Prevalence in 2021
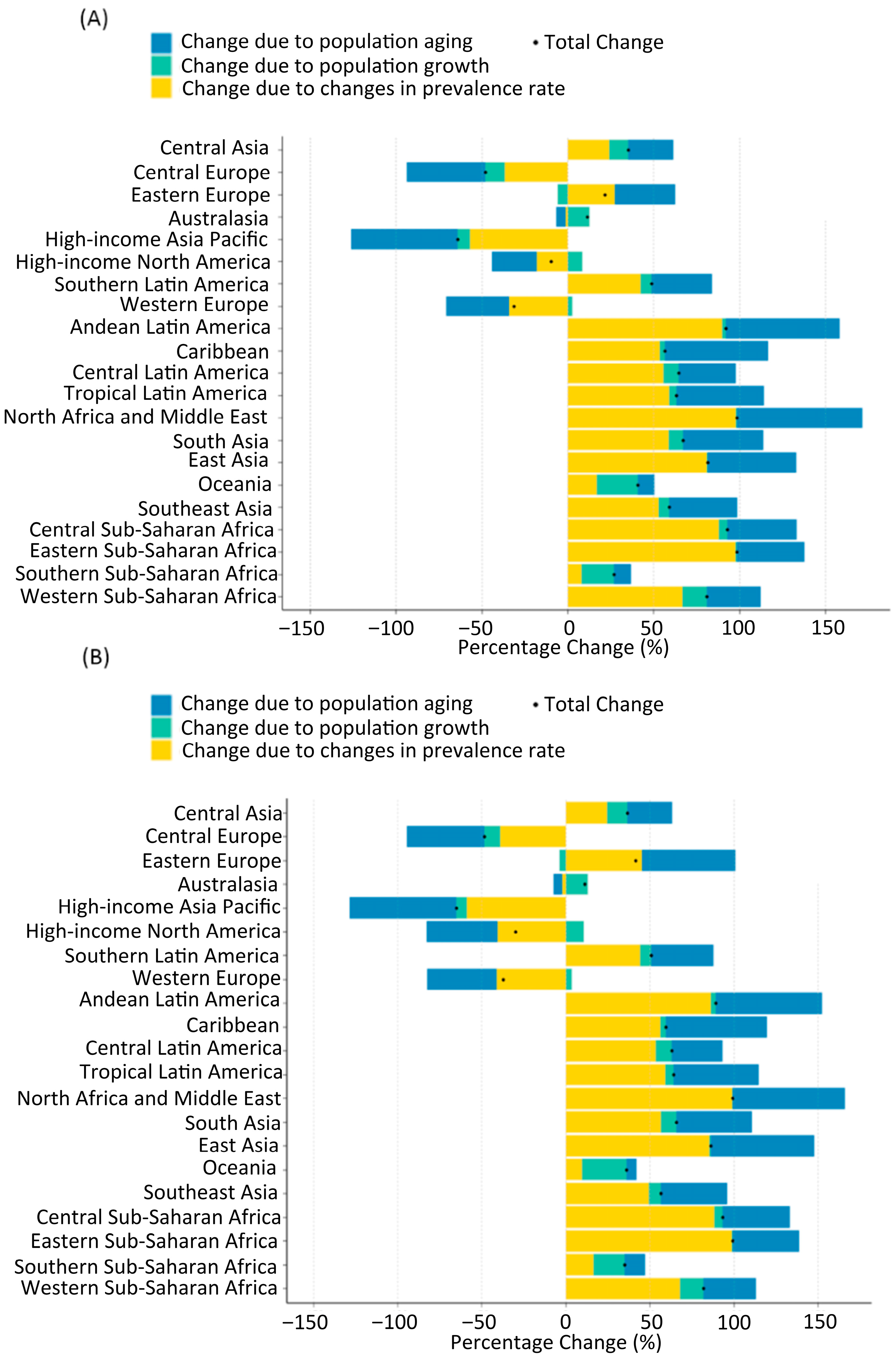
3.2.5. Projections of SCI by 2050
3.2.6. Decomposition of Drivers (Das Gupta)
3.2.7. Model Validation
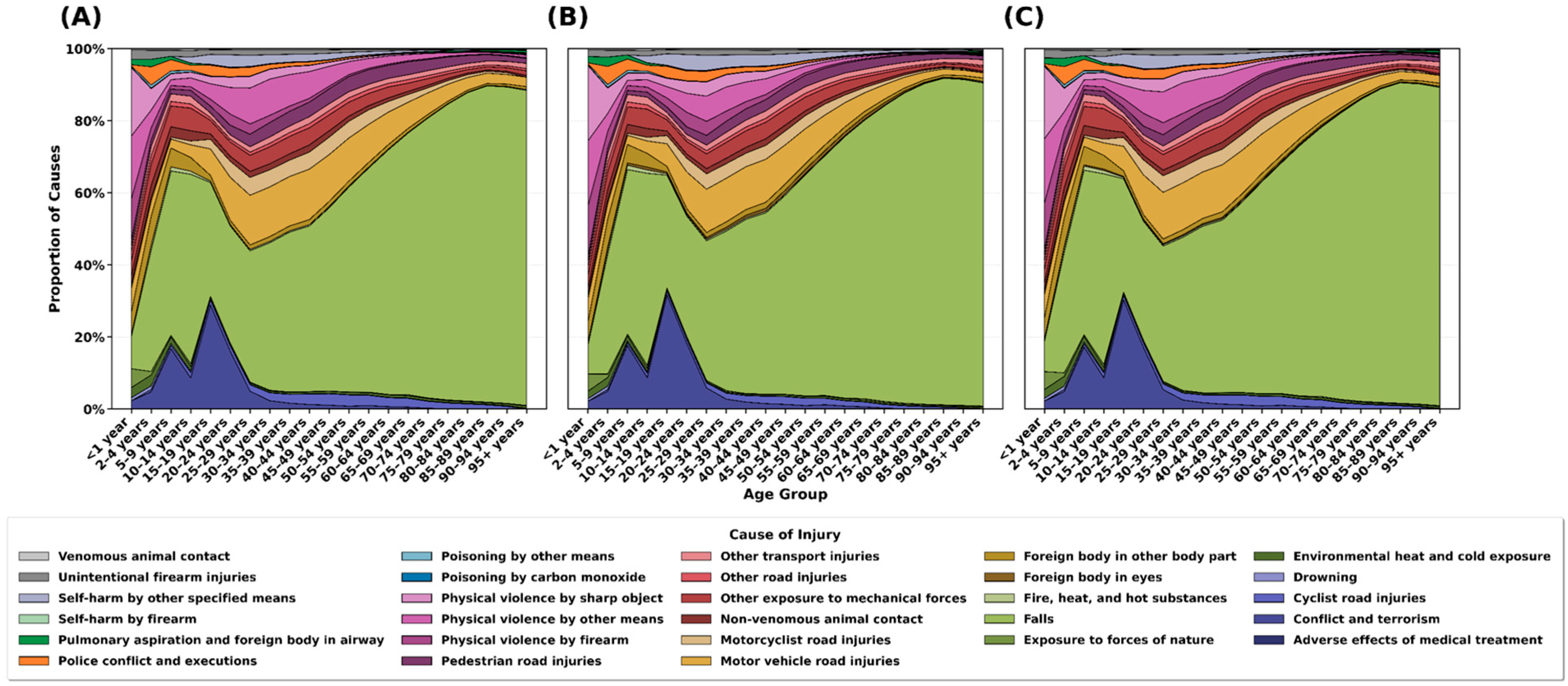
3.2.8. Age-Specific Causes of SCI
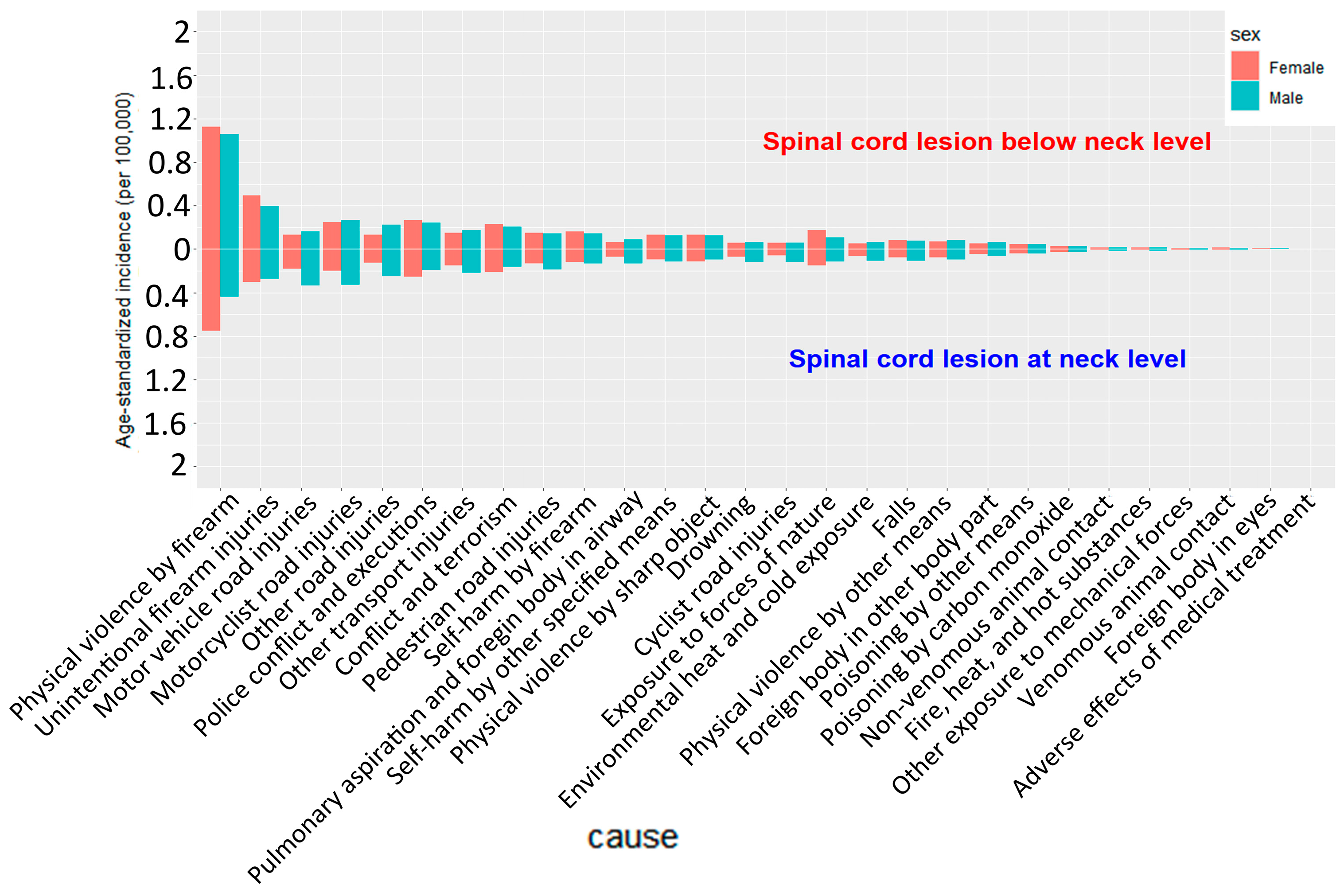
3.2.9. Sex-Specific Causes of SCI
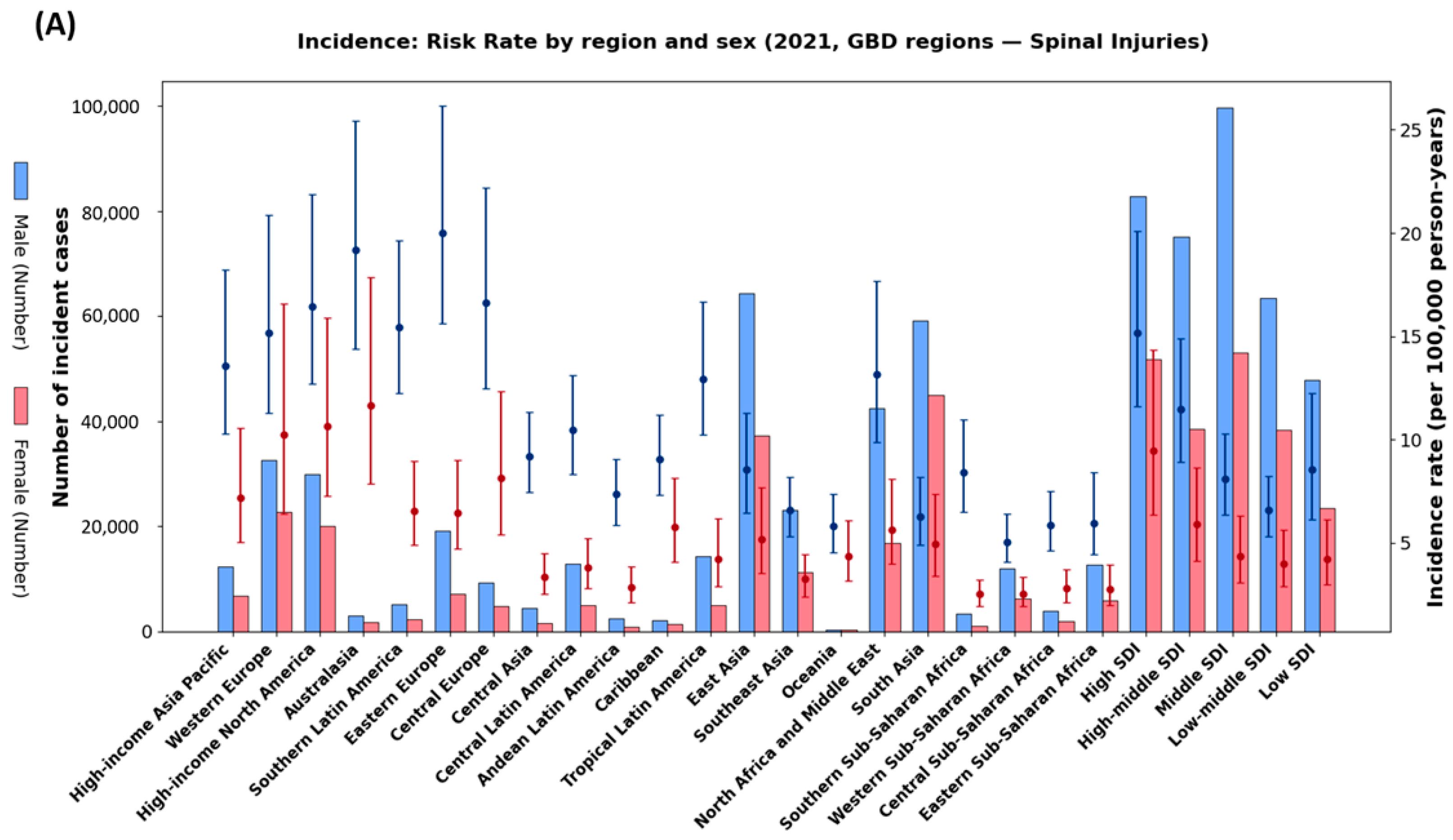
3.2.10. Region-Specific Causes of SCI
3.2.11. High-Income Regions (High-Income Asia Pacific, Western Europe, High-Income North America, Australasia)
3.2.12. Middle-Income Regions (Eastern Europe, Central Europe, Latin America)
3.2.13. Low-Income Regions (Sub-Saharan Africa, South Asia)
3.2.14. Comparison by Lesion Level
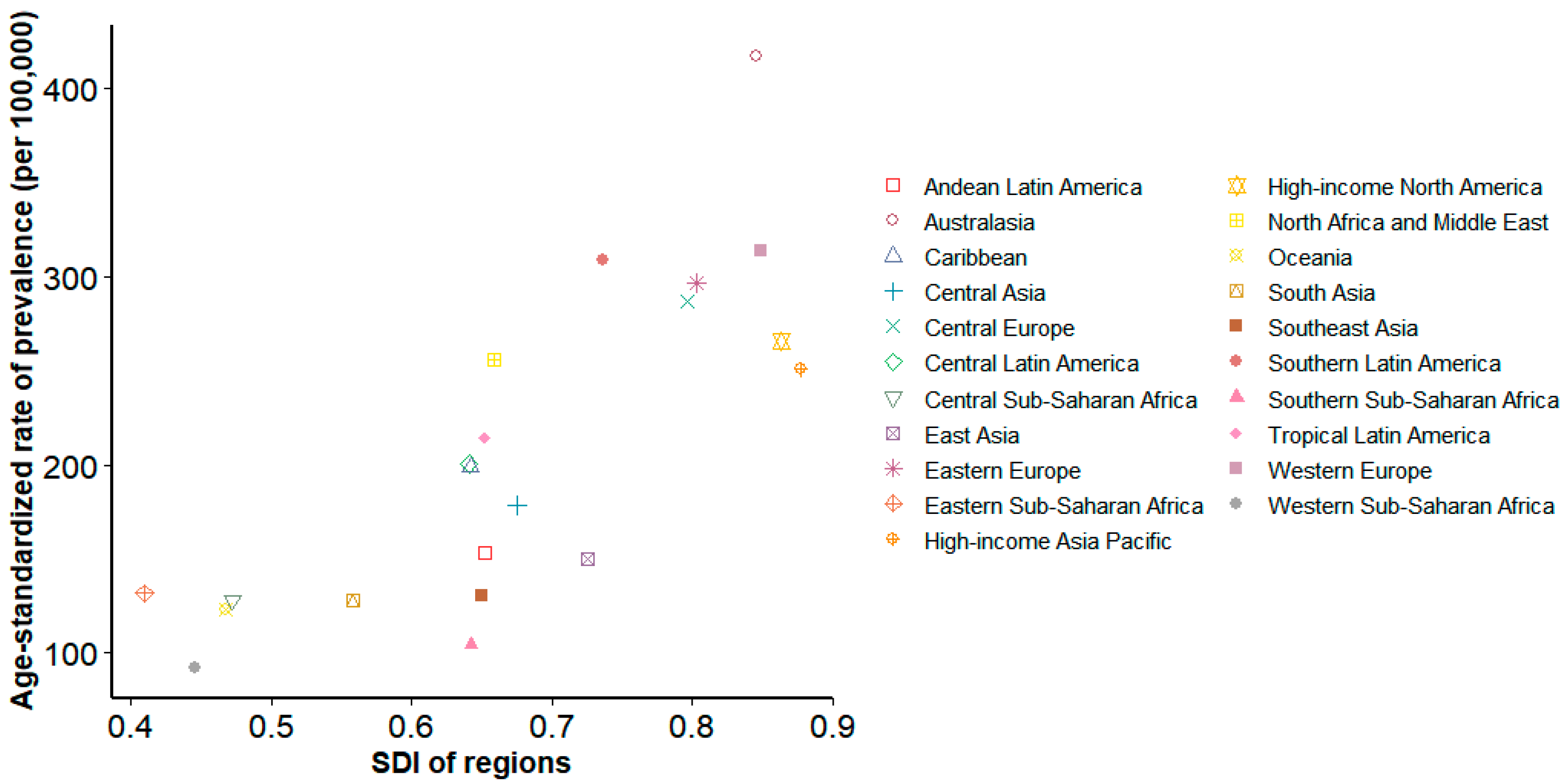
3.2.15. Sociodemographic Factors and SCI Prevalence
4. Discussion
4.1. Global Prevalence and Burden
4.2. Social and Economic Impact of SCI
4.3. Projections of SCI by 2050
4.4. Disparities in the Burden of SCI Between HICs and LMICs
4.5. Age-Specific Burden of SCI
4.6. Sex Differences in the Burden of SCI
4.7. Regional Etiologic Patterns of SCI
4.8. Strengths
- -
- This study provides systematic global, regional, and national estimates of SCI prevalence and YLDs using GBD 2021 data, with projections through 2050.
- -
- Application of Bayesian meta-regression (DisMod-MR 2.1) enabled generation of age-, sex-, and location-specific estimates with high reliability.
4.9. Limitations
- -
- Data and measurement: In many low-income settings, SCI data remain sparse or underreported, potentially reducing estimate accuracy. Cross-national coding differences may also introduce over- or underestimation.
- -
- Diagnostic capacity bias: We could not quantify the correlation between prevalence and diagnostic capacity (e.g., MRI availability, access to care); thus, higher prevalence in HICs may reflect true burden and/or better ascertainment, and should be interpreted cautiously.
- -
- Modeling assumptions: Projections are trend-based and assume stable exposures and policies; we did not model counterfactual scenarios (e.g., improved road safety, fall-prevention scale-up, rehabilitation expansion).
- -
- Sensitivity analyses: Scenario-based sensitivity analyses (e.g., road-safety improvements, aging-policy changes) were not performed.
- -
- Regional extrapolation risk: For regions with volatile recent trends, extrapolation can be implausible. For example, the below-neck-level projection for East Asia over-extrapolated a post-2007 surge and implausibly exceeded the global total by 2050; such outputs require cautious interpretation and potential model constraints.
- -
- Disability weight simplification: Applying a single disability weight to both neck- and below-neck-level injuries may underestimate the higher functional/QoL impact of cervical injuries.
- -
- Validation limits: Systematic per-country validation remains limited due to scarce national registries, although spot checks using extreme-burden countries (Table S4) showed consistency.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| SCI | Spinal cord injury |
| MS | Multiple sclerosis |
| GBD | Global burden of disease |
| YLDs | Years lived with disability |
| SDI | Sociodemographic Index |
| HICs | High-income countries |
| LMICs | Low- and middle-income countries |
References
- Rupp, R.; Biering-Sørensen, F.; Burns, S.P.; Graves, D.E.; Guest, J.; Jones, L.; Read, M.S.; Rodriguez, G.M.; Schuld, C.; Tansey-Md, K.E. International Standards for Neurological Classification of Spinal Cord Injury: Revised 2019. Top. Spinal Cord Inj. Rehabil. 2021, 27, 1–22. [Google Scholar] [CrossRef]
- Ahuja, C.S.; Wilson, J.R.; Nori, S.; Kotter, M.; Druschel, C.; Curt, A.; Fehlings, M.G. Traumatic spinal cord injury. Nat. Rev. Dis. Primers 2017, 3, 17018. [Google Scholar] [CrossRef]
- World Health Organization; International Spinal Cord Society. International Perspectives on Spinal Cord Injury; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Borg, S.J.; Geraghty, T.; Arora, M.; Foster, M.; Marshall, R.; Nunn, A.; Middleton, J.W. Employment outcomes following spinal cord injury: A population-based cross-sectional study in Australia. Spinal Cord 2021, 59, 1120–1131. [Google Scholar] [CrossRef]
- Merritt, C.H.; Taylor, M.A.; Yelton, C.J.; Ray, S.K. Economic impact of traumatic spinal cord injuries in the United States. Neuroimmunol. Neuroinflamm. 2019, 6, 9. [Google Scholar] [CrossRef]
- Feigin, V.L.; Nichols, E.; Alam, T.; Bannick, M.S.; Beghi, E.; Blake, N.; Culpepper, W.J.; Dorsey, E.R.; Elbaz, A.; Ellenbogen, R.G. Global, regional, and national burden of neurological disorders, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 459–480. [Google Scholar] [CrossRef]
- Singh, A.; Tetreault, L.; Kalsi-Ryan, S.; Nouri, A.; Fehlings, M.G. Global prevalence and incidence of traumatic spinal cord injury. Clin. Epidemiol. 2014, 2014, 309–331. [Google Scholar]
- Liu, Y.; Yang, X.; He, Z.; Li, J.; Li, Y.; Wu, Y.; Manyande, A.; Feng, M.; Xiang, H. Spinal cord injury: Global burden from 1990 to 2019 and projections up to 2030 using Bayesian age-period-cohort analysis. Front. Neurol. 2023, 14, 1304153. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Shang, Z.; Zhang, W.; Hu, X.; Shen, R.; Zhang, K.; Zhang, Y.; Zhang, L.; Liu, B.; Pang, M. Global, regional, and national burden of spinal cord injury from 1990 to 2021 and projections for 2050: A systematic analysis for the Global Burden of Disease 2021 study. Ageing Res. Rev. 2025, 103, 102598. [Google Scholar] [CrossRef] [PubMed]
- Stevens, G.A.; Alkema, L.; Black, R.E.; Boerma, J.T.; Collins, G.S.; Ezzati, M.; Grove, J.T.; Hogan, D.R.; Hogan, M.C.; Horton, R. Guidelines for accurate and transparent health estimates reporting: The GATHER statement. Lancet 2016, 388, e19–e23. [Google Scholar] [CrossRef]
- Ding, W.; Hu, S.; Wang, P.; Kang, H.; Peng, R.; Dong, Y.; Li, F. Spinal cord injury: The global incidence, prevalence, and disability from the global burden of disease study 2019. Spine 2022, 47, 1532–1540. [Google Scholar] [CrossRef] [PubMed]
- Bürkner, P.-C. brms: An R package for Bayesian multilevel models using Stan. J. Stat. Softw. 2017, 80, 1–28. [Google Scholar] [CrossRef]
- Cunha, N.S.; Malvea, A.; Sadat, S.; Ibrahim, G.M.; Fehlings, M.G. Pediatric spinal cord injury: A review. Children 2023, 10, 1456. [Google Scholar] [CrossRef]
- Chevan, A.; Sutherland, M. Revisiting Das Gupta: Refinement and extension of standardization and decomposition. Demography 2009, 46, 429–449. [Google Scholar] [CrossRef]
- DeVivo, M.J. Epidemiology of traumatic spinal cord injury: Trends and future implications. Spinal Cord 2012, 50, 365–372. [Google Scholar] [CrossRef]
- Center, S.L. Facts and Figures at a Glance; Birmingham, A.L., Ed.; University of Alabama at Birmingham: Birmingham, AL, USA, 2016; Volume 10. [Google Scholar]
- Hossain, M.S.; Harvey, L.A.; Islam, M.S.; Rahman, M.A.; Liu, H.; Herbert, R.D.; CIVIC Trial Collaboration. Loss of work-related income impoverishes people with SCI and their families in Bangladesh. Spinal Cord 2020, 58, 423–429. [Google Scholar] [CrossRef]
- Tan, X.; Liu, X.; Shao, H. Healthy China 2030: A vision for health care. Value Health Reg. Issues 2017, 12, 112–114. [Google Scholar] [CrossRef] [PubMed]
- Shiferaw, W.S.; Akalu, T.Y.; Mulugeta, H.; Aynalem, Y.A. The global burden of pressure ulcers among patients with spinal cord injury: A systematic review and meta-analysis. BMC Musculoskelet. Disord. 2020, 21, 334. [Google Scholar] [CrossRef] [PubMed]
- Ogbole, G.I.; Adeyomoye, A.O.; Badu-Peprah, A.; Mensah, Y.; Nzeh, D.A. Survey of magnetic resonance imaging availability in West Africa. Pan. Afr. Med. J. 2018, 30, 240. [Google Scholar] [CrossRef] [PubMed]
- Rubiano, A.M.; Carney, N.; Chesnut, R.; Puyana, J.C. Global neurotrauma research challenges and opportunities. Nature 2015, 527, S193–S197. [Google Scholar] [CrossRef]
- Oderud, T. Surviving spinal cord injury in low income countries. Afr. J. Disabil. 2014, 3, a80. [Google Scholar] [CrossRef]
- Kobusingye, O.C.; Hyder, A.A.; Bishai, D.; Hicks, E.R.; Mock, C.; Joshipura, M. Emergency medical systems in low-and middle-income countries: Recommendations for action. Bull. World Health Organ. 2005, 83, 626–631. [Google Scholar]
- World Health Organization. Global Status Report on Road Safety 2018; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Cummings, S.R.; Melton, L.J. Epidemiology and outcomes of osteoporotic fractures. Lancet 2002, 359, 1761–1767. [Google Scholar] [CrossRef]
- Nouri, A.; Da Broi, M.; May, A.; Janssen, I.; Molliqaj, G.; Davies, B.; Pandita, N.; Schaller, K.; Tessitore, E.; Kotter, M. Odontoid fractures: A review of the current state of the art. J. Clin. Med. 2024, 13, 6270. [Google Scholar] [CrossRef]
- Okuwaki, S.; Funayama, T.; Koda, M.; Eto, F.; Yamaji, A.; Yokogawa, N.; Sasagawa, T.; Ando, K.; Nakashima, H.; Kato, S.; et al. Characteristics of the cervical spine and cervical cord injuries in older adults with cervical ossification of the posterior longitudinal ligament. Sci. Rep. 2023, 13, 2689. [Google Scholar] [CrossRef]
- Loder, R.T.; Mishra, A.; Atoa, B.; Young, A. Spinal injury associated with firearm use. Cureus 2021, 13, e13918. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.; Cripps, R.A.; Fitzharris, M.; Wing, P. The global map for traumatic spinal cord injury epidemiology: Update 2011, global incidence rate. Spinal Cord 2014, 52, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Ackery, A.; Tator, C.; Krassioukov, A. A global perspective on spinal cord injury epidemiology. J. Neurotrauma 2004, 21, 1355–1370. [Google Scholar] [CrossRef] [PubMed]
- Burns, A.S.; O’Connell, C. The challenge of spinal cord injury care in the developing world. J. Spinal Cord Med. 2012, 35, 3–8. [Google Scholar] [CrossRef]
- Furlan, J.C.; Gulasingam, S.; Craven, B.C. Epidemiology of war-related spinal cord injury among combatants: A systematic review. Glob. Spine J. 2019, 9, 545–558. [Google Scholar] [CrossRef]
- Hoque, M.F.; Grangeon, C.; Reed, K. Spinal cord lesions in Bangladesh: An epidemiological study 1994–1995. Spinal Cord 1999, 37, 858–861. [Google Scholar] [CrossRef]

| (A) Neck-Level Spinal Cord Injuries | ||||||
| Number of Prevalent Cases | Age-Standardized Prevalence Rate per 100,000 | Percentage Change in Age-Standardized Prevalence Rate from 1990 to 2021 | Number of YLDs | Age-Standardized Rate of YLDs per 100,000 | Percentage Change in Age-Standardized Rate of YLDs per 100,000 from 1990 to 2021 | |
| Global | 7,423,601 (6,744,305 to 8,352,639) | 88 (80 to 100) | −0.17% (−0.18 to −0.15) | 2,905,920 (2,070,218 to 3,764,134) | 35 (25 to 45) | −0.21% (−0.21 to −0.19) |
| Central Europe, Eastern Europe, and Central Asia | 623,910 (571,153 to 679,453) | 125 (114 to 137) | −0.2% (−0.21 to −0.19) | 237,632 (169,121 to 303,721) | 48 (34 to 62) | −0.24% (−0.26 to −0.23) |
| Central Asia | 80,405 (72,475 to 91,342) | 82 (74 to 93) | −0.18% (−0.19 to −0.15) | 33,062 (23,144 to 43,389) | 34 (23 to 44) | −0.21% (−0.24 to −0.18) |
| Central Europe | 195,626 (178,384 to 215,033) | 134 (122 to 148) | −0.12% (−0.13 to −0.12) | 72,954 (51,704 to 94,120) | 51 (36 to 66) | −0.18% (−0.21 to −0.17) |
| Eastern Europe | 347,878 (317,244 to 379,590) | 136 (125 to 150) | −0.2% (−0.21 to −0.2) | 131,615 (94,674 to 168,599) | 52 (37 to 67) | −0.24% (−0.26 to −0.23) |
| High-income | 2,189,184 (2,004,303 to 2,412,320) | 154 (142 to 169) | −0.23% (−0.23 to −0.22) | 804,438 (581,439 to 1,035,355) | 58 (41 to 75) | −0.25% (−0.25 to −0.24) |
| Australasia | 83,449 (74,836 to 93,591) | 225 (199 to 253) | −0.15% (−0.17 to −0.13) | 30,802 (21,864 to 40,108) | 84 (59 to 111) | −0.16% (−0.16 to −0.15) |
| High-income Asia Pacific | 352,220 (323,624 to 386,775) | 135 (124 to 149) | −0.31% (−0.31 to −0.3) | 130,234 (93,364 to 168,343) | 51 (36 to 66) | −0.33% (−0.34 to −0.32) |
| High-income North America | 674,634 (613,670 to 739,189) | 139 (128 to 151) | −0.25% (−0.24 to −0.26) | 243,021 (174,278 to 309,329) | 51 (36 to 65) | −0.27% (−0.26 to −0.28) |
| Southern Latin America | 121,955 (112,339 to 132,701) | 162 (149 to 177) | 0.05% (0.03 to 0.05) | 47,491 (34,450 to 60,752) | 63 (46 to 81) | −0.02% (−0.01 to 0) |
| Western Europe | 956,925 (868,113 to 1,066,230) | 169 (152 to 190) | −0.21% (−0.22 to −0.2) | 352,889 (249,483 to 459,795) | 64 (44 to 84) | −0.22% (−0.24 to −0.21) |
| Latin America and Caribbean | 595,836 (545,422 to 656,732) | 94 (86 to 104) | −0.14% (−0.13 to −0.16) | 240,204 (169,301 to 312,936) | 38 (27 to 49) | −0.19% (−0.2 to −0.17) |
| Andean Latin America | 47,241 (42,378 to 54,760) | 72 (64 to 83) | −0.02% (0.01 to −0.06) | 19,051 (13,590 to 24,756) | 29 (20 to 38) | −0.11% (−0.11 to −0.14) |
| Caribbean | 45,799 (36,150 to 64,892) | 92 (72 to 133) | 0.49% (0.24 to 1) | 19,068 (12,561 to 30,171) | 39 (25 to 62) | 0.48% (0.36 to 0.89) |
| Central Latin America | 248,604 (225,442 to 281,664) | 94 (85 to 106) | −0.27% (−0.26 to −0.3) | 100,208 (70,683 to 128,309) | 38 (27 to 48) | −0.32% (−0.34 to −0.32) |
| Tropical Latin America | 254,191 (229,709 to 281,264) | 101 (91 to 112) | −0.07% (−0.08 to −0.06) | 101,877 (73,864 to 132,130) | 40 (29 to 53) | −0.13% (−0.14 to −0.1) |
| North Africa and Middle East | 733,916 (557,226 to 1,051,272) | 118 (90 to 168) | 0.03% (0.03 to 0.03) | 295,290 (188,889 to 467,159) | 47 (30 to 74) | −0.04% (−0.07 to 0.02) |
| South Asia | 1,043,559 (941,263 to 1,178,872) | 58 (53 to 65) | 0.09% (0.08 to 0.12) | 435,161 (316,813 to 560,991) | 24 (18 to 31) | 0.02% (0.03 to 0.06) |
| Southeast Asia, east Asia, and Oceania | 1,794,921 (1,656,802 to 1,958,579) | 68 (63 to 75) | 0.01% (0 to 0.01) | 698,114 (497,592 to 896,538) | 27 (19 to 35) | −0.09% (−0.1 to −0.05) |
| East Asia | 1,345,847 (1,244,874 to 1,458,414) | 71 (66 to 77) | 0.04% (0.03 to 0.04) | 511,349 (366,019 to 662,719) | 27 (19 to 35) | −0.08% (−0.1 to −0.05) |
| Oceania | 6850 (6131 to 7947) | 56 (51 to 65) | 0.37% (0.33 to 0.45) | 3007 (2107 to 3887) | 24 (17 to 31) | 0.34% (0.34 to 0.36) |
| Southeast Asia | 442,224 (384,239 to 537,680) | 60 (52 to 72) | −0.07% (−0.06 to −0.15) | 183,757 (130,575 to 251,455) | 25 (18 to 34) | −0.13% (−0.11 to −0.15) |
| Sub-Saharan Africa | 442,275 (353,948 to 595,288) | 49 (40 to 66) | −0.04% (−0.06 to −0.04) | 195,082 (134,468 to 286,237) | 21 (15 to 32) | −0.08% (−0.08 to −0.03) |
| Central Sub-Saharan Africa | 60,143 (44,116 to 89,445) | 56 (41 to 83) | 0.21% (0.13 to 0.31) | 26,763 (16,756 to 43,290) | 24 (16 to 40) | 0.16% (0.11 to 0.24) |
| Eastern Sub-Saharan Africa | 186,103 (133,709 to 291,562) | 57 (40 to 89) | −0.03% (0.03 to −0.07) | 82,551 (53,111 to 131,717) | 25 (16 to 40) | −0.08% (−0.05 to −0.11) |
| Southern Sub-Saharan Africa | 37,233 (34,301 to 40,654) | 46 (43 to 51) | −0.43% (−0.42 to −0.44) | 15,649 (11,349 to 19,449) | 19 (14 to 24) | −0.45% (−0.45 to −0.45) |
| Western Sub-Saharan Africa | 158,796 (138,926 to 191,824) | 42 (37 to 49) | 0.14% (0.09 to 0.23) | 70,119 (50,247 to 92,436) | 18 (13 to 24) | 0.1% (0.09 to 0.16) |
| (B) Below-Neck Spinal Cord Injuries | ||||||
| Number of Prevalent Cases | Age-Standardized Prevalence Rate per 100,000 | Percentage Change in Age-Standardized Prevalence Rate from 1990 to 2021 | Number of YLDs | Age-Standardized Rate of YLDs per 100,000 | Percentage Change in Age-Standardized Rate of YLDs per 100,000 from 1990 to 2021 | |
| Global | 7,977,081 (7,150,375 to 9,155,049) | 95 (85 to 109) | −0.18% (−0.2 to −0.14) | 1,660,317 (1,148,393 to 2,345,733) | 20 (14 to 28) | −0.29% (−0.3 to −0.27) |
| Central Europe, Eastern Europe, and Central Asia | 742,302 (677,934 to 820,823) | 146 (133 to 162) | −0.21% (−0.21 to −0.2) | 135,615 (94,895 to 184,783) | 27 (19 to 37) | −0.36% (−0.36 to −0.33) |
| Central Asia | 94,450 (84,900 to 106,458) | 97 (87 to 109) | −0.18% (−0.2 to −0.17) | 21,884 (15,117 to 30,300) | 22 (15 to 31) | −0.28% (−0.3 to −0.26) |
| Central Europe | 227,830 (206,852 to 253,503) | 153 (138 to 170) | −0.16% (−0.17 to −0.14) | 38,451 (26,486 to 53,726) | 26 (18 to 36) | −0.37% (−0.38 to −0.34) |
| Eastern Europe | 420,022 (385,322 to 461,941) | 160 (147 to 178) | −0.2% (−0.2 to −0.19) | 75,280 (52,094 to 103,014) | 29 (20 to 40) | −0.35% (−0.36 to −0.33) |
| High-income | 1,921,663 (1,777,023 to 2,084,318) | 135 (124 to 147) | −0.25% (−0.25 to −0.25) | 315,500 (219,411 to 431,929) | 23 (15 to 31) | −0.3% (−0.32 to −0.3) |
| Australasia | 72,033 (64,899 to 80,741) | 193 (172 to 216) | −0.19% (−0.2 to −0.18) | 11,789 (8044 to 16,299) | 32 (22 to 44) | −0.2% (−0.21 to −0.19) |
| High-income Asia Pacific | 301,367 (279,124 to 331,301) | 116 (106 to 128) | −0.33% (−0.34 to −0.32) | 49,302 (33,909 to 67,461) | 19 (13 to 27) | −0.41% (−0.43 to −0.4) |
| High-income North America | 612,529 (564,982 to 664,508) | 126 (117 to 137) | −0.27% (−0.27 to −0.28) | 98,250 (67,873 to 131,470) | 21 (14 to 28) | −0.3% (−0.3 to −0.31) |
| Southern Latin America | 111,011 (102,952 to 120,875) | 147 (136 to 160) | 0.01% (−0.01 to 0.01) | 21,726 (15,258 to 29,465) | 29 (20 to 39) | −0.21% (−0.21 to −0.18) |
| Western Europe | 824,722 (753,071 to 911,533) | 145 (131 to 162) | −0.24% (−0.24 to −0.22) | 134,433 (92,612 to 184,891) | 24 (16 to 33) | −0.28% (−0.3 to −0.27) |
| Latin America and Caribbean | 673,948 (612,096 to 745,341) | 107 (97 to 118) | −0.17% (−0.16 to −0.18) | 152,452 (105,859 to 203,532) | 24 (17 to 32) | −0.33% (−0.34 to −0.32) |
| Andean Latin America | 53,578 (47,491 to 62,396) | 82 (72 to 95) | −0.06% (−0.04 to −0.11) | 11,873 (8221 to 16,577) | 18 (12 to 25) | −0.3% (−0.32 to −0.33) |
| Caribbean | 53,007 (40,972 to 77,927) | 107 (81 to 159) | 0.49% (0.21 to 1.07) | 13,568 (8381 to 21,628) | 28 (17 to 44) | 0.48% (0.29 to 0.84) |
| Central Latin America | 281,254 (250,868 to 322,430) | 106 (95 to 122) | −0.28% (−0.27 to −0.31) | 62,900 (43,911 to 87,260) | 24 (17 to 33) | −0.43% (−0.43 to −0.43) |
| Tropical Latin America | 286,109 (259,071 to 319,707) | 113 (102 to 127) | −0.14% (−0.13 to −0.12) | 64,110 (44,576 to 84,822) | 25 (18 to 34) | −0.3% (−0.32 to −0.29) |
| North Africa and Middle East | 845,673 (617,408 to 1,306,946) | 138 (101 to 212) | 0.03% (−0.01 to 0.03) | 187,822 (114,166 to 337,074) | 30 (19 to 54) | −0.2% (−0.24 to −0.14) |
| South Asia | 1,238,974 (1,101,859 to 1,392,457) | 70 (62 to 78) | 0.03% (0 to 0.05) | 320,436 (226,727 to 437,659) | 18 (13 to 24) | −0.16% (−0.16 to −0.12) |
| Southeast Asia, east Asia, and Oceania | 2,009,736 (1,826,885 to 2,218,767) | 77 (69 to 85) | −0.04% (−0.06 to −0.04) | 387,724 (270,461 to 533,675) | 15 (10 to 21) | −0.33% (−0.34 to −0.3) |
| East Asia | 1,482,829 (1,367,846 to 1,625,239) | 79 (72 to 86) | −0.03% (−0.03 to −0.01) | 258,674 (180,186 to 353,506) | 14 (10 to 19) | −0.37% (−0.37 to −0.34) |
| Oceania | 7934 (7043 to 9342) | 67 (60 to 77) | 0.33% (0.29 to 0.41) | 2334 (1642 to 3040) | 19 (14 to 25) | 0.27% (0.28 to 0.25) |
| Southeast Asia | 518,973 (433,170 to 652,801) | 70 (59 to 87) | −0.07% (−0.09 to −0.14) | 126,715 (85,919 to 186,473) | 17 (12 to 25) | −0.24% (−0.23 to −0.26) |
| Sub-Saharan Africa | 544,784 (419,861 to 788,338) | 63 (48 to 91) | −0.01% (−0.06 to 0.06) | 160,768 (102,917 to 260,953) | 18 (12 to 30) | −0.11% (−0.15 to −0.02) |
| Central Sub-Saharan Africa | 75,010 (52,619 to 119,583) | 72 (50 to 115) | 0.24% (0.08 to 0.43) | 22,722 (13,781 to 40,341) | 21 (13 to 38) | 0.1% (0.01 to 0.24) |
| Eastern Sub-Saharan Africa | 237,422 (161,438 to 408,142) | 75 (50 to 132) | 0.03% (0.01 to 0.06) | 71,663 (423,69 to 131,261) | 22 (13 to 42) | −0.09% (−0.12 to −0.07) |
| Southern Sub-Saharan Africa | 45,354 (41,668 to 49,898) | 58 (53 to 63) | −0.38% (−0.38 to −0.39) | 11,782 (8392 to 15,513) | 15 (11 to 20) | −0.44% (−0.43 to −0.44) |
| Western Sub-Saharan Africa | 186,997 (161,440 to 229,724) | 50 (44 to 61) | 0.11% (0.05 to 0.24) | 54,601 (37,545 to 79,349) | 14 (10 to 21) | 0% (−0.01 to 0.1) |
| (A) Neck-Level Spinal Cord Injuries. | ||||||
| Age-Standardized Prevalence | Cases (Millions) | |||||
| 2030 | 2040 | 2050 | 2030 | 2040 | 2050 | |
| Global | 0.09% (0.08–0.11) | 0.08% (0.07–0.1) | 0.08% (0.07–0.1) | 7.44 (6.83–9.13) | 7.46 (6.87–9.52) | 7.3 (6.74–9.71) |
| Andean Latin America | 0.19% (0.17–0.21) | 0.26% (0.23–0.28) | 0.38% (0.33–0.39) | 0.14 (0.12–0.15) | 0.22 (0.19–0.24) | 0.34 (0.3–0.35) |
| Australasia | 0.22% (0.19–0.24) | 0.2% (0.17–0.21) | 0.18% (0.16–0.19) | 0.07 (0.06–0.08) | 0.07 (0.06–0.08) | 0.07 (0.06–0.07) |
| Caribbean | 0.14% (0.09–0.24) | 0.18% (0.1–0.36) | 0.24% (0.12–0.54) | 0.07 (0.04–0.12) | 0.09 (0.05–0.18) | 0.12 (0.06–0.27) |
| Central Asia | 0.09% (0.07–0.12) | 0.08% (0.07–0.12) | 0.08% (0.06–0.13) | 0.09 (0.07–0.12) | 0.09 (0.08–0.14) | 0.1 (0.08–0.16) |
| Central Europe | 0.07% (0.07–0.07) | 0.05% (0.05–0.05) | 0.04% (0.04–0.04) | 0.08 (0.07–0.08) | 0.05 (0.05–0.05) | 0.03 (0.04–0.03) |
| Central Latin America | 0.2% (0.18–0.21) | 0.26% (0.23–0.25) | 0.33% (0.29–0.3) | 0.6 (0.54–0.62) | 0.82 (0.73–0.79) | 1.08 (0.96–0.98) |
| Central Sub-Saharan Africa | 0.18% (0.07–0.47) | 0.28% (0.08–0.91) | 0.44% (0.1–1.77) | 0.3 (0.11–0.79) | 0.58 (0.17–1.91) | 1.08 (0.24–4.36) |
| East Asia | 0.21% (0.18–0.23) | 0.32% (0.27–0.37) | 0.51% (0.42–0.6) | 3.09 (2.69–3.51) | 4.63 (3.94–5.36) | 6.78 (5.58–7.98) |
| Eastern Europe | 0.22% (0.2–0.24) | 0.25% (0.23–0.28) | 0.29% (0.26–0.31) | 0.45 (0.41–0.49) | 0.48 (0.44–0.53) | 0.52 (0.47–0.58) |
| Eastern Sub-Saharan Africa | 0.17% (0.06–0.49) | 0.25% (0.07–0.89) | 0.37% (0.08–1.63) | 0.93 (0.34–2.72) | 1.7 (0.49–6.12) | 2.95 (0.67–13.11) |
| High-income Asia Pacific | 0.07% (0.07–0.08) | 0.05% (0.05–0.05) | 0.03% (0.03–0.04) | 0.13 (0.13–0.14) | 0.09 (0.08–0.09) | 0.05 (0.05–0.06) |
| High-income North America | 0.07% (0.07–0.07) | 0.05% (0.05–0.05) | 0.03% (0.03–0.03) | 0.27 (0.26–0.29) | 0.2 (0.19–0.2) | 0.14 (0.13–0.14) |
| North Africa and Middle East | 0.16% (0.09–0.34) | 0.19% (0.09–0.46) | 0.22% (0.1–0.63) | 1.2 (0.69–2.5) | 1.55 (0.78–3.81) | 1.95 (0.86–5.62) |
| Oceania | 0.05% (0.05–0.05) | 0.04% (0.05–0.04) | 0.04% (0.05–0.04) | 0.01 (0.01–0.01) | 0.01 (0.01–0.01) | 0.01 (0.01–0.01) |
| South Asia | 0.11% (0.09–0.12) | 0.14% (0.12–0.16) | 0.18% (0.15–0.21) | 2.14 (1.88–2.49) | 2.86 (2.48–3.39) | 3.71 (3.18–4.47) |
| Southeast Asia | 0.08% (0.06–0.1) | 0.09% (0.06–0.1) | 0.09% (0.07–0.11) | 0.58 (0.45–0.72) | 0.66 (0.5–0.81) | 0.73 (0.53–0.89) |
| Southern Latin America | 0.28% (0.25–0.31) | 0.34% (0.3–0.37) | 0.42% (0.35–0.46) | 0.2 (0.18–0.22) | 0.26 (0.22–0.28) | 0.32 (0.27–0.35) |
| Southern Sub-Saharan Africa | 0.07% (0.06–0.07) | 0.07% (0.07–0.07) | 0.08% (0.07–0.08) | 0.06 (0.06–0.07) | 0.07 (0.07–0.08) | 0.08 (0.08–0.09) |
| Tropical Latin America | 0.21% (0.17–0.27) | 0.28% (0.22–0.37) | 0.36% (0.27–0.51) | 0.51 (0.41–0.64) | 0.68 (0.53–0.91) | 0.88 (0.66–1.25) |
| Western Europe | 0.11% (0.1–0.12) | 0.09% (0.08–0.1) | 0.07% (0.06–0.07) | 0.51 (0.46–0.55) | 0.4 (0.36–0.43) | 0.31 (0.28–0.32) |
| Western Sub-Saharan Africa | 0.05% (0.04–0.08) | 0.05% (0.04–0.09) | 0.06% (0.04–0.12) | 0.31 (0.24–0.47) | 0.44 (0.32–0.75) | 0.6 (0.4–1.13) |
| (B) Below-Neck Spinal Cord Injuries. | ||||||
| Age-Standardized Prevalence | Cases (Millions) | |||||
| 2030 | 2040 | 2050 | 2030 | 2040 | 2050 | |
| Global | 0.09% (0.07–0.1) | 0.08% (0.06–0.09) | 0.08% (0.05–0.08) | 7.64 (5.95–8.48) | 7.52 (5.5–8.3) | 7.22 (4.98–7.92) |
| Andean Latin America | 0.2% (0.17–0.26) | 0.28% (0.23–0.37) | 0.39% (0.31–0.52) | 0.15 (0.12–0.19) | 0.23 (0.19–0.3) | 0.35 (0.27–0.46) |
| Australasia | 0.19% (0.17–0.21) | 0.18% (0.16–0.19) | 0.16% (0.15–0.17) | 0.06 (0.06–0.07) | 0.06 (0.06–0.07) | 0.06 (0.06–0.06) |
| Caribbean | 0.17% (0.1–0.29) | 0.23% (0.11–0.44) | 0.3% (0.12–0.66) | 0.08 (0.05–0.14) | 0.11 (0.06–0.22) | 0.15 (0.06–0.33) |
| Central Asia | 0.11% (0.09–0.14) | 0.11% (0.08–0.14) | 0.11% (0.08–0.15) | 0.12 (0.09–0.14) | 0.13 (0.09–0.16) | 0.14 (0.09–0.18) |
| Central Europe | 0.08% (0.08–0.08) | 0.06% (0.06–0.06) | 0.04% (0.04–0.04) | 0.09 (0.08–0.09) | 0.06 (0.06–0.06) | 0.04 (0.04–0.04) |
| Central Latin America | 0.23% (0.2–0.26) | 0.28% (0.25–0.32) | 0.35% (0.31–0.39) | 0.67 (0.59–0.76) | 0.9 (0.79–1.01) | 1.17 (1.03–1.3) |
| Central Sub-Saharan Africa | 0.22% (0.08–0.64) | 0.33% (0.1–1.28) | 0.52% (0.11–2.53) | 0.37 (0.14–1.1) | 0.7 (0.2–2.69) | 1.28 (0.28–6.25) |
| East Asia | 0.29% (0.25–0.31) | 0.48% (0.42–0.52) | 0.82% (0.7–0.88) | 4.26 (3.78–4.57) | 6.96 (6.06–7.42) | 11.05 (9.42–11.73) |
| Eastern Europe | 0.33% (0.3–0.37) | 0.4% (0.37–0.46) | 0.5% (0.45–0.57) | 0.66 (0.6–0.74) | 0.78 (0.7–0.88) | 0.91 (0.82–1.03) |
| Eastern Sub-Saharan Africa | 0.25% (0.08–0.85) | 0.39% (0.1–1.68) | 0.61% (0.12–3.32) | 1.4 (0.45–4.7) | 2.69 (0.66–11.52) | 4.95 (0.93–26.71) |
| High-income Asia Pacific | 0.06% (0.06–0.07) | 0.04% (0.04–0.05) | 0.03% (0.03–0.03) | 0.11 (0.1–0.12) | 0.07 (0.07–0.08) | 0.05 (0.04–0.05) |
| High-income North America | 0.06% (0.06–0.07) | 0.04% (0.04–0.05) | 0.03% (0.03–0.03) | 0.24 (0.22–0.26) | 0.17 (0.16–0.18) | 0.12 (0.11–0.13) |
| North Africa and Middle East | 0.17% (0.1–0.36) | 0.19% (0.1–0.46) | 0.21% (0.1–0.58) | 1.27 (0.74–2.67) | 1.57 (0.81–3.79) | 1.89 (0.87–5.23) |
| Oceania | 0.05% (0.06–0.05) | 0.05% (0.06–0.05) | 0.05% (0.06–0.04) | 0.01 (0.01–0.01) | 0.01 (0.01–0.01) | 0.01 (0.01–0.01) |
| South Asia | 0.13% (0.11–0.14) | 0.16% (0.14–0.18) | 0.2% (0.17–0.22) | 2.5 (2.2–2.8) | 3.28 (2.86–3.67) | 4.16 (3.6–4.67) |
| Southeast Asia | 0.09% (0.07–0.12) | 0.09% (0.07–0.13) | 0.1% (0.07–0.14) | 0.65 (0.49–0.87) | 0.73 (0.52–0.98) | 0.79 (0.54–1.07) |
| Southern Latin America | 0.27% (0.24–0.28) | 0.33% (0.28–0.35) | 0.4% (0.34–0.42) | 0.19 (0.17–0.21) | 0.25 (0.22–0.26) | 0.31 (0.27–0.33) |
| Southern Sub-Saharan Africa | 0.09% (0.09–0.1) | 0.1% (0.1–0.11) | 0.11% (0.12–0.12) | 0.09 (0.08–0.09) | 0.11 (0.11–0.11) | 0.13 (0.13–0.14) |
| Tropical Latin America | 0.25% (0.21–0.32) | 0.32% (0.26–0.44) | 0.41% (0.33–0.6) | 0.58 (0.49–0.76) | 0.77 (0.63–1.07) | 1 (0.79–1.47) |
| Western Europe | 0.1% (0.09–0.11) | 0.07% (0.07–0.08) | 0.06% (0.05–0.06) | 0.42 (0.4–0.47) | 0.33 (0.31–0.36) | 0.25 (0.24–0.28) |
| Western Sub-Saharan Africa | 0.07% (0.05–0.11) | 0.08% (0.06–0.14) | 0.09% (0.06–0.19) | 0.42 (0.33–0.69) | 0.62 (0.46–1.16) | 0.87 (0.61–1.86) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, M.; Jeong, W.; Jang, S.; Park, J.H.; Bae, Y.; Lee, S.W. Spinal Cord Injury Epidemiology and Causes: A Worldwide Analysis with 2050 Projections. Healthcare 2025, 13, 2552. https://doi.org/10.3390/healthcare13202552
Kim M, Jeong W, Jang S, Park JH, Bae Y, Lee SW. Spinal Cord Injury Epidemiology and Causes: A Worldwide Analysis with 2050 Projections. Healthcare. 2025; 13(20):2552. https://doi.org/10.3390/healthcare13202552
Chicago/Turabian StyleKim, Minyoung, Woonyoung Jeong, Suho Jang, Jin Hoon Park, Youngoh Bae, and Seung Won Lee. 2025. "Spinal Cord Injury Epidemiology and Causes: A Worldwide Analysis with 2050 Projections" Healthcare 13, no. 20: 2552. https://doi.org/10.3390/healthcare13202552
APA StyleKim, M., Jeong, W., Jang, S., Park, J. H., Bae, Y., & Lee, S. W. (2025). Spinal Cord Injury Epidemiology and Causes: A Worldwide Analysis with 2050 Projections. Healthcare, 13(20), 2552. https://doi.org/10.3390/healthcare13202552








