Penetrating Orbital Injury: A Narrative Review for Emergency Clinicians
Abstract
1. Introduction
2. Methods
3. Results and Discussion
3.1. Epidemiology, Morbidity, and Mortality
3.2. Mechanism of Injury
- Non-missile injuries: Objects with lower velocity (<100 m per second), such as chopsticks, branches, or pens, typically result in localized tissue laceration due to the pyramidal configuration of the orbit, which directs the object towards the orbital apex. In civilian settings, most POIs result from low-velocity injuries [2,9,15,16].
3.3. Complications
3.3.1. Ocular Complications
- Hyphema which may elevate intraocular pressure and lead to secondary glaucoma if not managed [10].
3.3.2. Infectious Complications
3.3.3. Cerebral Complications
3.3.4. Vascular Complications
3.4. Patterns of Injury
3.4.1. Superior Rim of the Orbit
3.4.2. Inferior Rim of the Orbit
3.4.3. Lateral Rim of the Orbit
3.4.4. Medial Rim of the Orbit
3.4.5. Extraorbital Entry
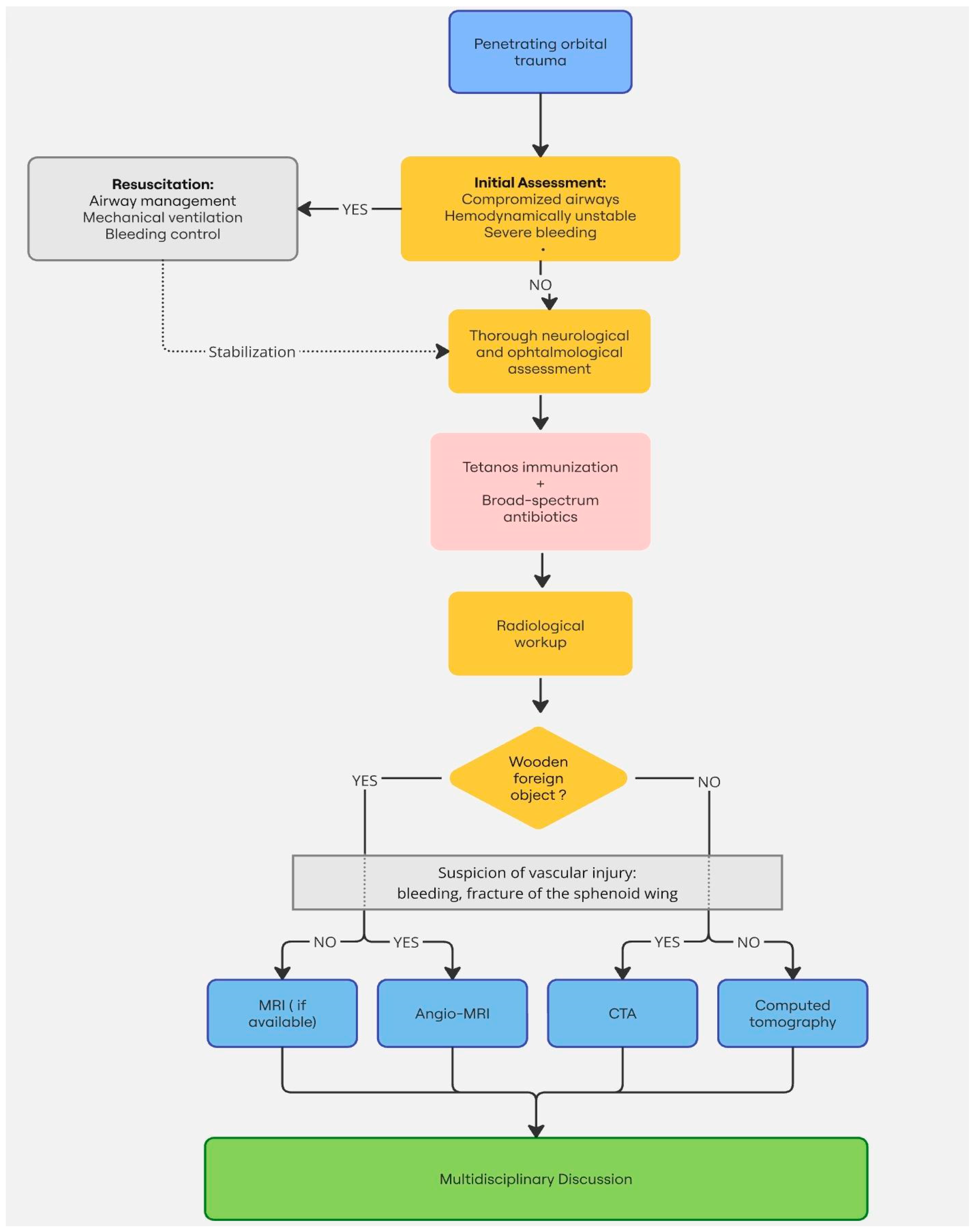
3.5. Radiological Work-Up
3.5.1. Computed Tomography (CT)
3.5.2. Magnetic Resonance Imaging (MRI)
3.5.3. Angiography
3.5.4. Ultrasonography
3.5.5. Conventional Radiography
3.6. Management and Treatment
3.6.1. Initial Evaluation and Resuscitation
3.6.2. Prophylactic Antibiotics
3.6.3. Surgical Management
3.6.4. Postoperative Follow-Up
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Barouj, M.D.; Tabrizi, R.; Behnia, P.; Tabrizi, M.A.A.; Kheirkhahi, M. Penetrating Orbital Injury; a Case Report and Treatment Algorithm. Arch. Acad. Emerg. Med. 2020, 8, e33. [Google Scholar] [CrossRef]
- Tabibkhooei, A.; Aslaninia, A.; Anousha, K. Childhood Transorbital Skull Base Penetrating Injury: Report of 2 Cases and Review of Literature. World Neurosurg. 2019, 131, 213–216. [Google Scholar] [CrossRef]
- Gonullu, M.E.; Filinte, G.T.; Cardak, N.G.A.; Kucuk, S.; Akoz, T. The Surgical Strategy for the Intraorbital Foreign Bodies. J. Craniofac. Surg. 2016, 27, 1785–1788. [Google Scholar] [CrossRef] [PubMed]
- Rzaev, D.A.; Danilin, V.E.; Letyagin, G.V.; Istomina, T.K.; Chishchina, N.V. Penetrating orbitocranial injury: A review of the literature and a case report of injury by a watercolor brush in a 3-year-old child. Zh Vopr Neirokhir Im NN Burdenko 2017, 81, 77–87. [Google Scholar] [CrossRef]
- Mzimbiri, J.M.; Li, J.; Bajawi, M.A.; Lan, S.; Chen, F.; Liu, J. Orbitocranial Low-Velocity Penetrating Injury: A Personal Experience, Case Series, Review of the literature, and Proposed Management Plan. World Neurosurg. 2016, 87, 26–34. [Google Scholar] [CrossRef]
- Agrawal, A.; Reddy, V.U.; Kumar, S.S.; Hegde, K.V.; Rao, G.M. Transorbital Orbitocranial Penetrating Injury with an Iron Rod. Craniomaxillofac. Trauma Reconstr. 2016, 9, 145–148. [Google Scholar] [CrossRef]
- Santander, X.A.; Revuelta, J.M.; Cotúa, C.; Rodriguez, B.A.; de Leyva Moreno, P.; Mazzei, A.S. Occult Transorbital Intracranial Injury by Windshield Wiper Handle: Case Report and Review of Literature. World Neurosurg. 2019, 126, 530–532. [Google Scholar] [CrossRef]
- Flament, J.; Moraine, A. Tree Branch through the Orbit into the Skull: A Case Report. Radiol. Case Rep. 2021, 16, 795–797. [Google Scholar] [CrossRef] [PubMed]
- Duinen, M.T.A. The Transorbital Intracranial Penetrating Injury; Springer Science+Business Media: Dordrecht, The Netherlands, 2000. [Google Scholar] [CrossRef]
- Négrel, A.D.; Thylefors, B. The global impact of eye injuries. Ophthalmic Epidemiol. 1998, 5, 143–169. [Google Scholar] [CrossRef]
- Webster, J.E.; Schneider, R.C.; Lofstrom, J.E. Observations upon the Management of Orbito-Cranial Wounds. J. Neurosurg. 1946, 3, 329–336. [Google Scholar] [CrossRef]
- Wikimedia Commons contributors. Eye Orbit Anatomy Superior. Available online: https://commons.wikimedia.org/wiki/File:Eye_orbit_anatomy_superior.jpg (accessed on 26 September 2024).
- Betts, J.G.; Young, K.A.; Wise, J.A.; Johnson, E.; Poe, B.; Kruse, D.H.; Korol, O.; Johnson, J.E.; Womble, M.; DeSaix, P. Anatomy and Physiology; OpenStax: Houston, TX, USA, 2013; Available online: https://openstax.org/books/anatomy-and-physiology/pages/7-2-the-skull (accessed on 26 September 2024).
- Awori, J.; Wilkinson, D.A.; Gemmete, J.J.; Thompson, B.G.; Chaudhary, N.; Pandey, A.S. Penetrating Head Injury by a Nail Gun: Case Report, Review of the Literature, and Management Considerations. J. Stroke Cerebrovasc. Dis. 2017, 26, e143–e149. [Google Scholar] [CrossRef] [PubMed]
- Mashriqi, F.; Iwanaga, J.; Loukas, M.; D’Antoni, A.V.; Tubbs, R.S. Penetrating Orbital Injuries: A Review. Cureus 2017, 9, e1725. [Google Scholar] [CrossRef] [PubMed]
- Dunya, I.M.; Rubin, P.A.; Shore, J.W. Penetrating orbital trauma. Int. Ophthalmol. Clin. 1995, 35, 25–36. [Google Scholar] [CrossRef] [PubMed]
- Turbin, R.E.; Maxwell, D.N.; Langer, P.D.; Frohman, L.P.; Hubbi, B.; Wolansky, L.; Mori, M. Patterns of transorbital intracranial injury: A review and comparison of occult and non-occult cases. Surv. Ophthalmol. 2006, 51, 449–460. [Google Scholar] [CrossRef] [PubMed]
- Schreckinger, M.; Orringer, D.; Thompson, B.G.; La Marca, F.; Sagher, O. Transorbital penetrating injury: Case series, review of the literature, and proposed management algorithm. J. Neurosurg. 2011, 114, 53–61. [Google Scholar] [CrossRef]
- Ghadersohi, S.; Ference, E.H.; Detwiller, K.; Kern, R.C. Presentation, workup, and management of penetrating transorbital and transnasal injuries: A case report and systematic review. Am. J. Rhinol Allergy 2017, 31, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Zhou, L.P.; Jin, J.; Yuan, H.F. Clinical diagnosis and treatment of intraorbital wooden foreign bodies. Chin. J. Traumatol. 2016, 19, 322–325. [Google Scholar] [CrossRef] [PubMed]
- Di Roio, C.; Jourdan, C.; Mottolese, C.; Convert, J.; Artru, F. Craniocerebral injury resulting from transorbital stick penetration in children. Childs Nerv. Syst. 2000, 16, 503–507. [Google Scholar] [CrossRef]
- Subburaman, N.; Sivabalan, K.; Ramachandran, M.; Chandrasekhar, D. Impacted knife injury of the orbit, maxilla and oropharynx. Indian J. Otolaryngol. Head Neck Surg. 2005, 57, 347–350. [Google Scholar] [CrossRef]
- Tenenholz, T.; Baxter, A.B.; McKhann, G.M. Orbital assault with a pencil: Evaluating vascular injury. AJR Am. J. Roentgenol. 1999, 173, 144. [Google Scholar] [CrossRef]
- Carothers, A. Orbitofacial wounds and cerebral artery injuries caused by umbrella tips. JAMA 1978, 239, 1151–1152. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.H.; Kim, H.; Yoon, E.S. Unrecognized intraorbital wooden foreign body. Arch. Craniofac. Surg. 2018, 19, 300–303. [Google Scholar] [CrossRef] [PubMed]
- Callison, C.; Nguyen, H. Tetanus Prophylaxis. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK559008/ (accessed on 26 September 2024).
- Ildan, F.; Bagdatoglu, H.; Boyar, B.; Doganay, M.; Çetinalp, E.; Karadayi, A. The nonsurgical management of a penetrating orbitocranial injury reaching the brain stem: Case report. J. Trauma Acute Care Surg. 1994, 36, 116–118. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.T.; Kung, W.H.; Chang, C.H.; Ku, W.N.; Tien, P.T.; Chiang, C.C.; Tsai, Y.Y. Endoscopy-assisted extraction of orbital and nasal foreign body. Taiwan J. Ophthalmol. 2020, 11, 421–424. [Google Scholar] [CrossRef]
- Sollini, G.; Giorli, A.; Zoli, M.; Farneti, P.; Arena, G.; Astarita, F.; Mazzatenta, D.; Pasquini, E. Endoscopic transnasal approach to remove an intraorbital bullet: Systematic review and case report. Acta. Otorhinolaryngol. Ital. 2024, 44, 207. [Google Scholar] [CrossRef] [PubMed]


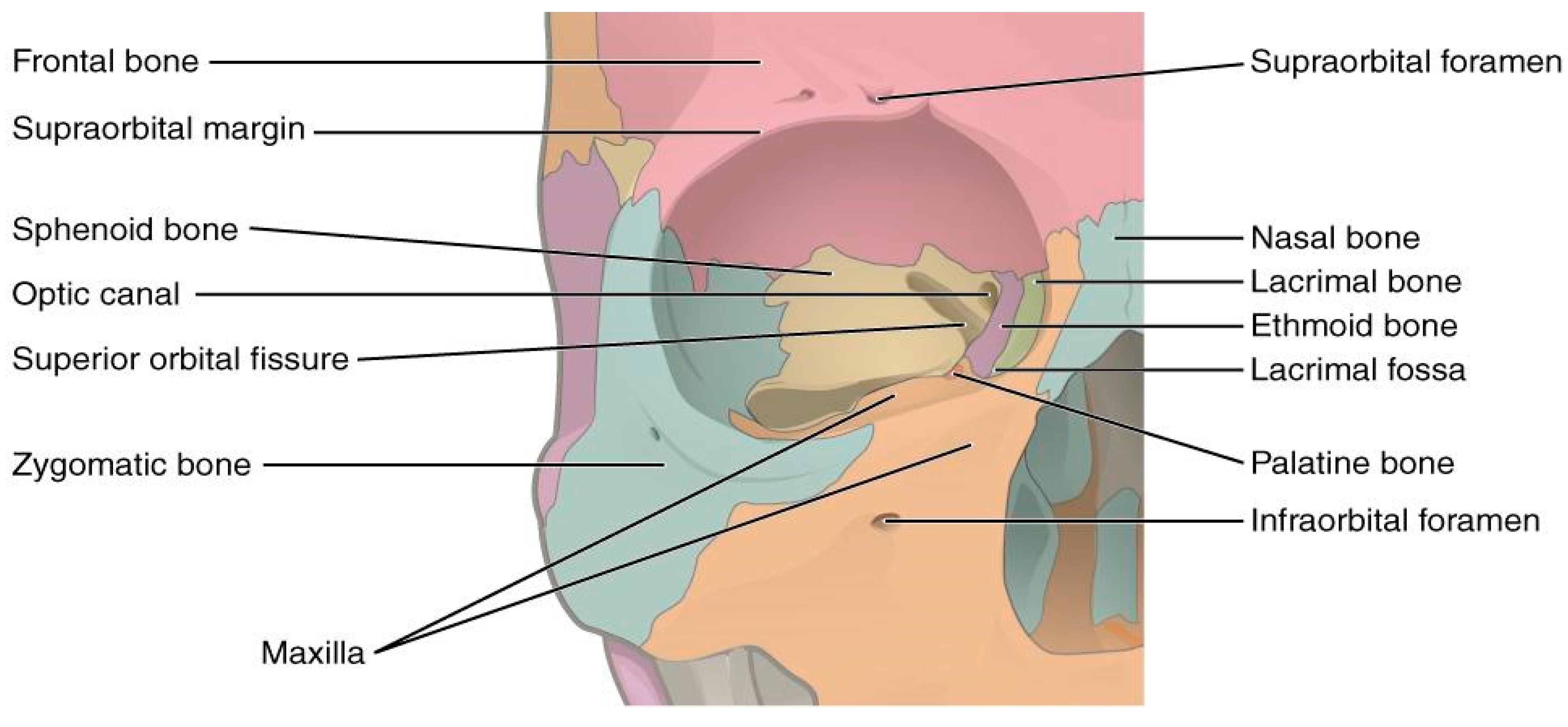
| Zone of Penetration | Involved Structures | Common Trajectories | Underlying Injuries | Clinical Findings | References |
|---|---|---|---|---|---|
| Superior Orbital Rim | Frontal bone, orbital roof, frontal lobe | Penetrates orbital roof into frontal lobe | Frontal lobe contusion, cerebrospinal fluid leaks | Lid laceration, clear fluid leakage, frontal lobe oedema | [5,15,17,18,19,22] |
| Inferior Orbital Rim | Infraorbital nerve, maxillary sinus, palate | Penetrates orbital floor into maxillary sinus and palate | Infraorbital nerve laceration, diplopia, maxillary sinus injury | Numbness, diplopia, infraorbital swelling, palatal perforation | |
| Lateral Orbital Rim | Zygomatic bone, lateral orbital wall | Penetretes lateral orbital wall without deep penetration | Zygomatic fracture, superficial trauma | Minimal penetration, lateral orbital swelling, often no deep neurovascular injury | |
| Medial Orbital Rim | Ethmoidal sinuses, optic nerve, brainstem (severe) | Penetrates medial orbital wall into sinuses or deeper | Optic nerve damage, ethmoidal sinus injury, brainstem contusion | Vision loss, optic neuropathy, sinus infection, potentially life-threatening brainstrem comlications | |
| Extraorbital Entry | Varies (e.g., maxillary sinus, nasal cavity) | Enters via facial structures but involves orbital tissues | Ophtalmoplegia, optic nerve damage, ethmoidal fracture | Blindless, cranial nerve palsies, globe rupture in some cases |
| Imaging Modality | Indication | Advantages | Limitations | References |
|---|---|---|---|---|
| Non-Contrast CT | Initial assessment, detection of fractures, metallic foreign bodies | Quick, widely available, good for fractures and metal | May miss organic materials like wood | [1,2,3,5,6,7,9,17,18,24,25] |
| MRI | Suspected organic foreign bodies, soft tissue assessment | Superior soft tissue contrast, identifies non-metal objects | Contraindicated with metallic foreign bodies | |
| CTA/MRA | Suspected vascular injury (carotid-cavernous fistula, pseudoaneurysm) | Visualizes blood vessels, identifies vascular complications | Limited in acute trauma with metal | |
| Orbital Ultrasonography | Assessment of soft tissue or fluid collection | Non-invasive, real-time imaging, useful for ocular conditions | Limited scope, requires specific expertise | |
| Orbital Ultrasonography | Initial screening in resource-limited settings | Readily available, low cost | Poor sensitivity for radiolucent objects like glass |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pirlet, F.; Flament, J. Penetrating Orbital Injury: A Narrative Review for Emergency Clinicians. Healthcare 2025, 13, 98. https://doi.org/10.3390/healthcare13020098
Pirlet F, Flament J. Penetrating Orbital Injury: A Narrative Review for Emergency Clinicians. Healthcare. 2025; 13(2):98. https://doi.org/10.3390/healthcare13020098
Chicago/Turabian StylePirlet, Florence, and Julien Flament. 2025. "Penetrating Orbital Injury: A Narrative Review for Emergency Clinicians" Healthcare 13, no. 2: 98. https://doi.org/10.3390/healthcare13020098
APA StylePirlet, F., & Flament, J. (2025). Penetrating Orbital Injury: A Narrative Review for Emergency Clinicians. Healthcare, 13(2), 98. https://doi.org/10.3390/healthcare13020098







