Exploring Therapists’ Experiences of an Educational Website to Support Telehealth Delivery of Constraint-Induced Movement Therapy
Abstract
1. Introduction
- What is the level of user engagement with the TeleCIMT learning modules and resources?
- What are users’ experiences and opinions regarding the ease of use and design of the TeleCIMT website?
- What are the clinician-reported barriers and enablers to the implementation of TeleCIMT in practice?
2. Methods
2.1. Eligibility
2.2. Recruitment and Consent
2.3. Data Collection
2.4. Data Analysis
3. Results
3.1. Demographics
3.2. Experience in Delivering CIMT
“…improved functional use of their affected upper limb...convenience of being able to do therapy in their own home”.(Respondent 190)
“All achieved overall functional improvements and goals…”.(Respondent 209)
3.3. Website Engagement
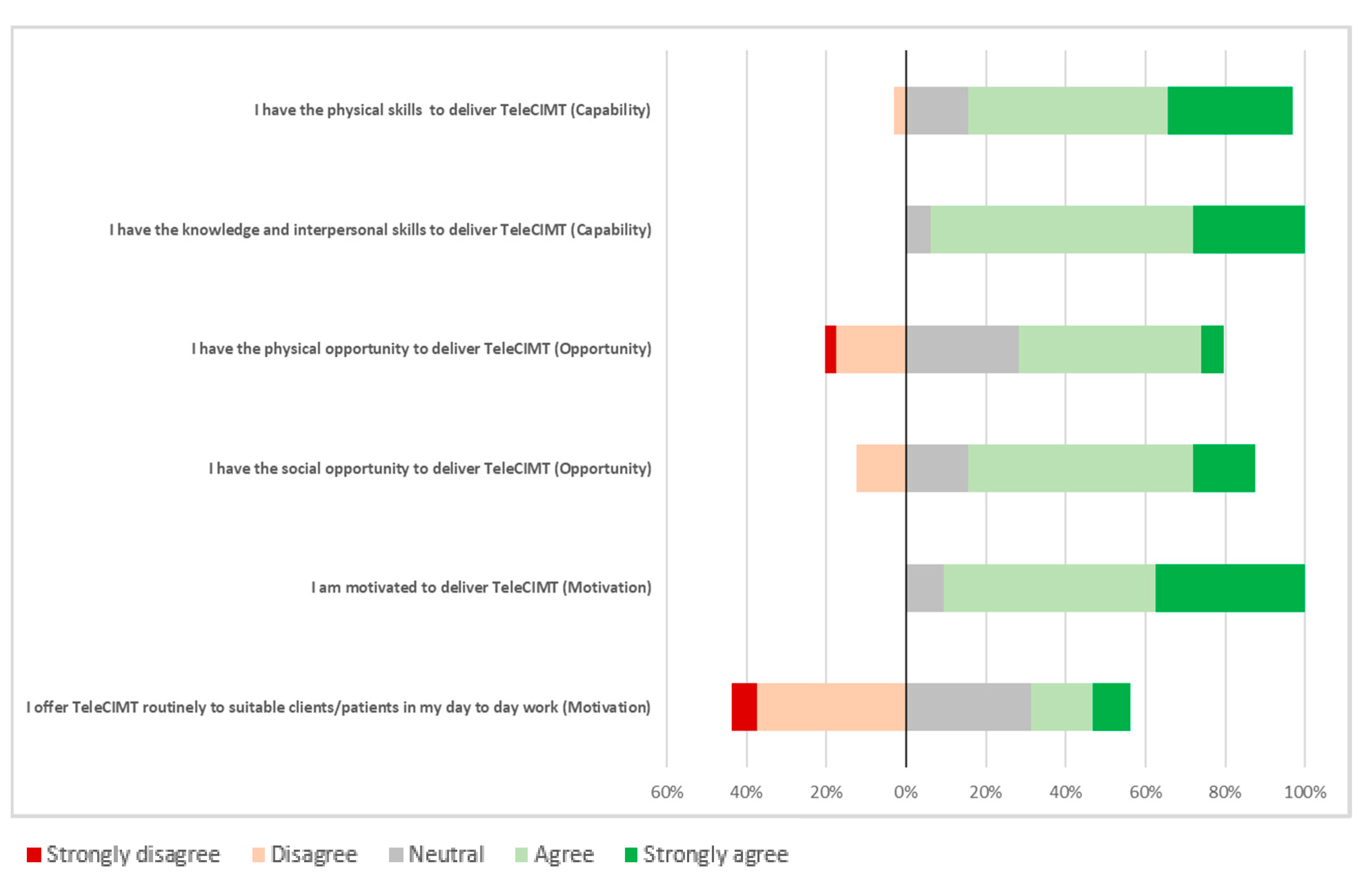
3.4. Clinician-Perceived Barriers and Enablers to Implementing TeleCIMT in Practice
“I think a barrier to using CIMT in everyday practice can be the time needed to set up the programme and deliver it, especially in the public sector. This website really assists in reducing the amount of time needed for prep, and hopefully that can drive change in our workplace”.(Respondent 504)
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kwakkel, G.; Veerbeek, J.M.; van Wegen, E.E.; Wolf, S.L. Constraint-induced movement therapy after stroke. Lancet Neurol. 2015, 14, 224–234. [Google Scholar] [CrossRef] [PubMed]
- Corbetta, D.; Sirtori, V.; Castellini, G.; Moja, L.; Gatti, R. Constraint-induced movement therapy for upper extremities in people with stroke. Cochrane Libr. Cochrane Rev. 2015, 2015, CD004433. [Google Scholar] [CrossRef] [PubMed]
- Stroke Foundation. Clinical Guidelines for Stroke Management. Available online: https://informme.org.au/guidelines/living-clinical-guidelines-for-stroke-management (accessed on 20 March 2024).
- Intercollegiate Stroke Working Party. National Clinical Guideline for Stroke for the UK and Ireland; Intercollegiate Stroke Working Party: London, UK, 2023; Available online: http://www.strokeguideline.org (accessed on 20 March 2024).
- McCluskey, A.; Massie, L.; Gibson, G.; Pinkerton, L.; Vandenberg, A. Increasing the delivery of upper limb constraint-induced movement therapy post-stroke: A feasibility implementation study. Aust. Occup. Ther. J. 2020, 67, 237–249. [Google Scholar] [CrossRef] [PubMed]
- Pedlow, K.; Lennon, S.; Wilson, C. Application of constraint-induced movement therapy in clinical practice: An online survey. Arch. Phys. Med. Rehabil. 2014, 95, 276–282. [Google Scholar] [CrossRef]
- Uswatte, G.; Taub, E.; Lum, P.; Brennan, D.; Barman, J.; Bowman, M.H.; Taylor, A.; McKay, S.; Sloman, S.B.; Morris, D.M.; et al. Tele-rehabilitation of upper-extremity hemiparesis after stroke: Proof-of-concept randomized controlled trial of in-home Constraint-Induced Movement therapy. Restor. Neurol. Neurosci. 2021, 39, 303–318. [Google Scholar] [CrossRef]
- Lum, P.S.; Taub, E.; Schwandt, D.; Postman, M.; Hardin, P.; Uswatte, G. Automated Constraint-Induced Therapy Extension (AutoCITE) for movement deficits after stroke. J. Rehabil. Res. Dev. 2004, 41, 249–258. [Google Scholar] [CrossRef]
- Lum, P.S.; Uswatte, G.; Taub, E.; Hardin, P.; Mark, V.W. A telerehabilitation approach to delivery of constraint-induced movement therapy. J. Rehabil. Res. Dev. 2006, 43, 391–400. [Google Scholar] [CrossRef]
- Christie, L.J.; Fearn, N.; McCluskey, A.; Lannin, N.A.; Shiner, C.T.; Kilkenny, A.; Boydell, J.; Meharg, A.; Howes, E.; Churilov, L.; et al. Remote constraint induced therapy of the upper extremity (ReCITE): A feasibility study protocol. Front. Neurol. 2022, 13, 1010449. [Google Scholar] [CrossRef]
- Glinsky, J.V.; Ilha, J.; Xiong, Y.; Gomez, G.; Rostagnor, S.; Martín-Manjarrés, S.; Tranter, K.; Muldoon, S.; Weerts, E.; Harvey, L.A. The 2022 Massive Open Online Course (MOOC) to train physiotherapists in the management of people with spinal cord injuries: A qualitative and quantitative analysis of learners’ experiences and its impact. Spinal Cord 2023, 61, 615–623. [Google Scholar] [CrossRef]
- Scrivener, K.; Akkermans, J.; Svanetti, S.; Szilas, C.; Robson, M.; Love, S. Examining user perspective of an online learning resource for physiotherapists: A mixed methods study of the TRAIN program. Physiother. Res. Int. 2021, 26, e1917. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef] [PubMed]
- Vanderbilt University. REDCap (Research Electronic Data Capture); Vanderbilt University: Nashville, TN, USA, 2023. [Google Scholar]
- Michie, S.; van Stralen, M.M.; West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. 2011, 6, 42. [Google Scholar] [CrossRef]
- IBM. SPSS Statistics 28; IBM: Armonk, NY, USA, 2022. [Google Scholar]
- Fleet, A.; Page, S.J.; MacKay-Lyons, M.; Boe, S.G. Modified constraint-induced movement therapy for upper extremity recovery post stroke: What is the evidence? Top. Stroke Rehabil. 2014, 21, 319–331. [Google Scholar] [CrossRef]
- Christie, L.J.; Rendell, R.; McCluskey, A.; Fearn, N.; Hunter, A.; Lovarini, M. Development of a behaviour change intervention to increase the delivery of upper limb constraint-induced movement therapy programs to people with stroke and traumatic brain injury. Disabil. Rehabil. 2023, 46, 4931–4942. [Google Scholar] [CrossRef]
- Weerakkody, A.; Emmanuel, R.; White, J.; Godecke, E.; Singer, B. Unlocking the restraint—Development of a behaviour change intervention to increase the provision of modified constraint-induced movement therapy in stroke rehabilitation. Aust. Occup. Ther. J. 2023, 70, 661–677. [Google Scholar] [CrossRef]
- Lawdis, K.; Baist, H.; Pittman, C.O. Use of online training modules for professional development with school-based therapists: Outcome project. J. Occup. Ther. Sch. Early Interv. 2017, 10, 300–314. [Google Scholar] [CrossRef]
- Jolliffe, L.; Hoffmann, T.; Churilov, L.; Lannin, N.A. What is the feasibility and observed effect of two implementation packages for stroke rehabilitation therapists implementing upper limb guidelines? A cluster controlled feasibility study. BMJ Open Qual. 2020, 9, e000954. [Google Scholar] [CrossRef]
- Christie, L.J.; Rendell, R.; Fearn, N.; Descallar, J.; McCluskey, A.; Pearce, A.; Wong, L.; Lovarini, M. Increasing the delivery of upper limb constraint-induced movement therapy programs for stroke and brain injury survivors: Evaluation of the ACTIveARM project. Disabil. Rehabil. 2023, 46, 4943–4955. [Google Scholar] [CrossRef]
- Stephenson, A.; Howes, S.; Murphy, P.J.; Deutsch, J.E.; Stokes, M.; Pedlow, K.; McDonough, S.M. Factors influencing the delivery of telerehabilitation for stroke: A systematic review. PLoS ONE 2022, 17, e0265828. [Google Scholar] [CrossRef]
- Cacciamani, S.; Perrucci, V.; Khanlari, A.; Balboni, G. Sense of community and peer feedback in a blended University Course. Educ. Inf. Technol. 2023, 29, 5211–5223. [Google Scholar] [CrossRef]
- Walsh, S.; Pollard, N. ‘Seeing the bigger picture’: A post-graduate online learning community facilitates political competence for occupational therapists. J. Furth. High. Educ. 2019, 44, 971–983. [Google Scholar] [CrossRef]
- Farber, R.S. Distance education and teaching online: My journey from mystery to mastery. Occup. Ther. Health Care 2013, 27, 272–279. [Google Scholar] [PubMed]
- Openshaw, K.P.; Schultz, J.C.; Millington, M.J. Implications of Communities of Practice in Distance Rehabilitation Education. Rehabil. Res. Policy Educ. 2008, 22, 163–170. [Google Scholar] [CrossRef]
- Mandiberg, J.M.; Gates, L.B. A community of practice for peer mental workers: Lessons learned. Am. J. Psychiatr. Rehabil. 2017, 20, 156–174. [Google Scholar] [CrossRef]
- Regmi, K.; Jones, L. A systematic review of the factors—Enablers and barriers—Affecting e-learning in health sciences education. BMC Med. Educ. 2020, 20, 91. [Google Scholar] [CrossRef]
- Lee, K.; Fanguy, M.; Bligh, B.; Lu, X.S. Adoption of online teaching during the COVID-19 Pandemic: A systematic analysis of changes in university teaching activity. Educ. Rev. 2022, 74, 460–483. [Google Scholar] [CrossRef]
- Chandan, K.; Kealey, C.; Timpson, P.; Murphy, B. Blended learning model incorporating online learning for a competency-focused, work-based learning (WBL) programme—Allied healthcare case-study. High. Educ. Ski. Work.-Based Learn. 2022, 12, 791–806. [Google Scholar] [CrossRef]
- Nolan, A. Engaging the Adult Learner: An Action Research Study on Delivering Effective Online Learning Experiences. Instructional Design Capstones Collection. 2023, 84. Available online: https://scholarworks.umb.edu/instruction_capstone/84 (accessed on 20 March 2024).
| Characteristic | Description | n (%) |
|---|---|---|
| Gender | Female Male | 38 (95) 2 (5) |
| Role | Qualified clinician | 40 (100) |
| Allied health student | 0 (0) | |
| Discipline | Occupational Therapy | 29 (72.5) |
| Physiotherapy | 11 (27.5) | |
| Years of experience in | 0–5 years | 16 (40) |
| neurological rehabilitation | 6–15 years | 8 (20) |
| More than 15 years | 16 (40) | |
| Area/s of practice * | Acute care | 5 (12.5) |
| Inpatient rehabilitation | 13 (32.5) | |
| Outpatient rehabilitation | 19 (47.5) | |
| Community | 17 (42.5) | |
| Other | 1 (2.8) | |
| Type of service | Public | 35 (87.5) |
| Private | 4 (10) | |
| Not-for-profit organisation | 1 (2.5) | |
| Country of practice | Australia | 26 (65) |
| New Zealand | 4 (10) | |
| United Kingdom | 9 (22.5) | |
| United States of America | 1 (2.5) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Makroglou, K.; Fearn, N.; Portelli, B.; Badge, H.; Boydell, J.; Kilkenny, A.; Meharg, A.; Christie, L.J. Exploring Therapists’ Experiences of an Educational Website to Support Telehealth Delivery of Constraint-Induced Movement Therapy. Healthcare 2025, 13, 159. https://doi.org/10.3390/healthcare13020159
Makroglou K, Fearn N, Portelli B, Badge H, Boydell J, Kilkenny A, Meharg A, Christie LJ. Exploring Therapists’ Experiences of an Educational Website to Support Telehealth Delivery of Constraint-Induced Movement Therapy. Healthcare. 2025; 13(2):159. https://doi.org/10.3390/healthcare13020159
Chicago/Turabian StyleMakroglou, Kate, Nicola Fearn, Bianca Portelli, Helen Badge, Jessamy Boydell, Anna Kilkenny, Annie Meharg, and Lauren J. Christie. 2025. "Exploring Therapists’ Experiences of an Educational Website to Support Telehealth Delivery of Constraint-Induced Movement Therapy" Healthcare 13, no. 2: 159. https://doi.org/10.3390/healthcare13020159
APA StyleMakroglou, K., Fearn, N., Portelli, B., Badge, H., Boydell, J., Kilkenny, A., Meharg, A., & Christie, L. J. (2025). Exploring Therapists’ Experiences of an Educational Website to Support Telehealth Delivery of Constraint-Induced Movement Therapy. Healthcare, 13(2), 159. https://doi.org/10.3390/healthcare13020159








