An Exploratory Analysis of Public Perspectives and Attitudes Towards Radiation in Saudi Arabia
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Approval
2.2. Study Design and Settings
2.3. Population, Sample, and Sample Size
2.4. Validity and Reliability
2.5. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Insights into Radiation Sources and Risk Assessment
3.3. Participants’ Attitudes Towards Radiation Exposure
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
- Age:
- Sex:
- Level of Education:
- The current place of residence:
- Nationality
- Region:
- Community:
- Professional:
- Specialisation/field: Medical or Non-medical
- Are you interested in learning more about how to protect yourself from radiation?
- 11.
- Have you ever received any education or training on radiation protection, including online training courses?
- 12.
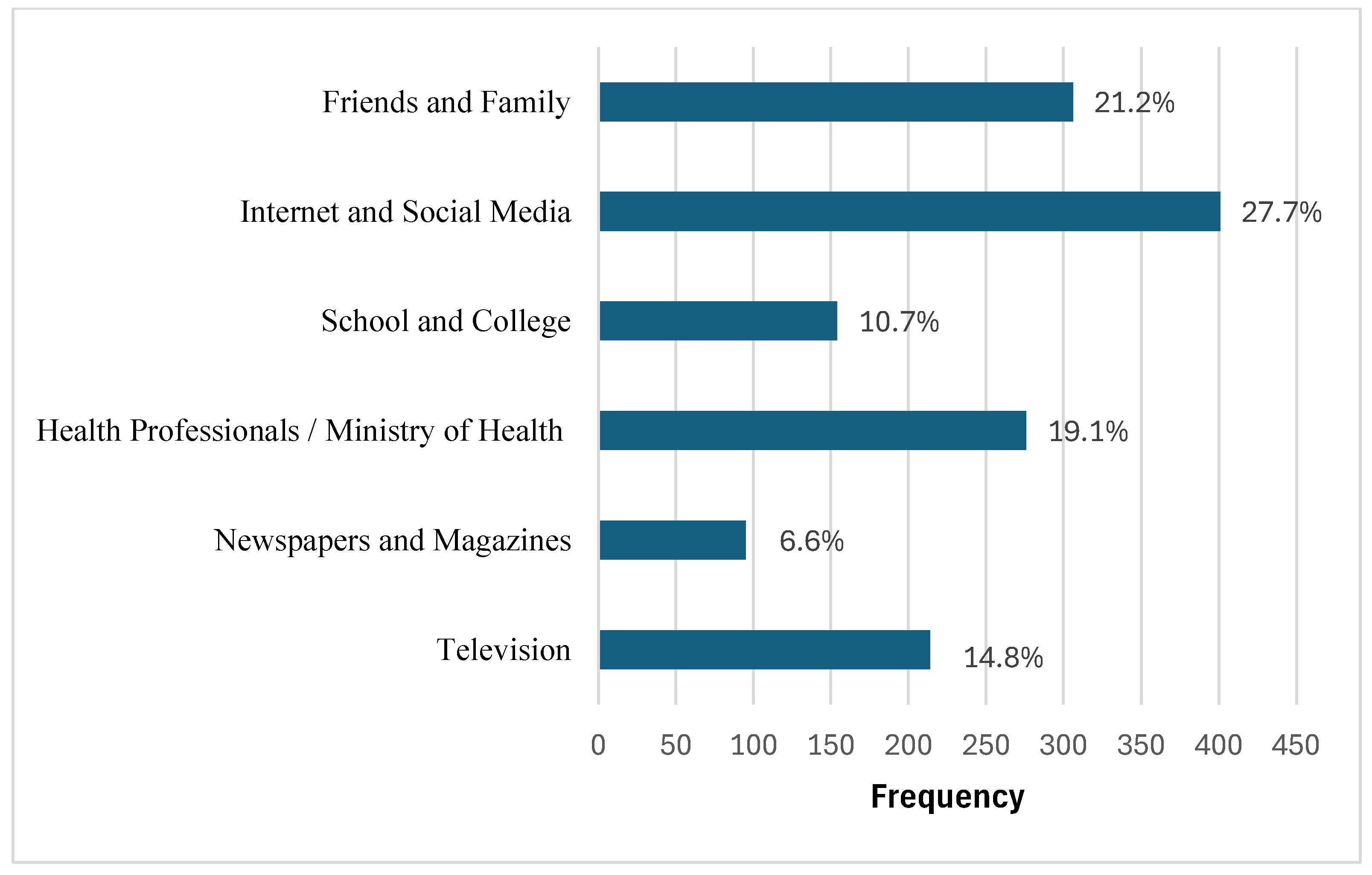
- Where do you get most of your information about radiation and its effects? (select all that applies):
- 13.
- How many times have you undergone diagnostic medical imaging (such as dental X-rays, CT scan, MRI, etc.) in the past two years?
- 14.
- How long will you spend in direct sunlight (in the peak time 10 am–4 pm) without using any protection (such as sunscreen, hats, sunglasses, … etc.)?
- 15.
- What radiation sources do you know? (Select all that apply):
- ◦
- Medical radiation (x-ray, MRI, CT)
- ◦
- The sun and stars (Cosmic radiation)
- ◦
- Household appliances (e.g., microwaves, TV)
- ◦
- Mobile devices
- ◦
- The rocks and soil (Terrestrial radiation)
- ◦
- Nuclear power reactors
- ◦
- Other
- I am familiar with the term “radiation”
- I am aware of the different sources of radiation in everyday life
- I am aware of the concept of radiation protection
- I am familiar with the safety measures related to radiation in medical fields.
- I am aware of the potential risks of radiation exposure in my daily life
- I am familiar with the use of radiation in various industries (e.g., hospitals, airports).
- I feel knowledgeable about the safety of consumer products that may emit radiation (e.g., Wi-Fi, cell phones).
- I understand the importance of public awareness regarding radiation sources and protection
- I regularly take precautions to minimise my exposure to unnecessary radiation.
- I can notice any changes or signs of skin damage due to radiation exposure from the sun
- I know the warning symbol for the presence of radiation in the hospital
- I know how to protect myself from medical imaging (such as using lead shielding or following instructions to avoid repetition)
- I believe I can distinguish between imaging modalities in the hospitals like ultrasound/MRI and X-ray/CT
- The media often exaggerates the risks of exposure to radiation.
- Sunscreen should be used daily, regardless of the weather.
- It is important for me to use sunglasses when going outdoors.
- I try hard to stay in the shadows when I am outside.
- I prefer to cover most of my body when I am outdoors during the day.
- It is important to limit direct sun exposure to reduce the risk of skin cancer. (I believe that there is a relationship between radiation and cancer).
- People should be more aware of the UV radiation risks associated with sun exposure.
- I feel comfortable when undergoing medical procedures that include X-ray imaging when necessary.
- I consult my doctor before repeating X-rays.
- Advancements in technology have made X-ray procedures much safer than in the past.
- Sufficient information about safety from radiation must be provided by professionals in the field of healthcare.
- The Healthcare Organisations must regulate the use of radiation in various industries more strictly.
- General education on radiation sources is necessary for the safety of society.
- I avoid putting the mobile phone near my head for long periods.
- I am extinguishing the unused electronic devices to reduce radiological emissions.
- I support spreading awareness about the risks of radiation and how to prevent it.
- I avoid accompanying patients inside the radiology room if not necessary
- I regularly inspect devices that emit radiation (such as mobile phones and microwaves) to ensure their safety.
- I am concerned about the possible health risks associated with radiation exposure.
- I read the instructions or warnings related to radiation before using electronic devices.
- I prefer using lower-radiation alternatives to electronic devices when available.
References
- Podgorsak, E.B. BASIC RADIATION PHYSICS. In Review of Radiation Oncology Physics: A Handbook for Teachers and Students; International Atomic Energy Agency Publication: Vienna, Austria, 2005. [Google Scholar]
- Ananthaswamy, H.N. Sunlight and skin cancer. J. Biomed. Biotechnol. 2001, 1, 49. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, B.K. How Sun Exposure Causes Skin Cancer: An Epidemiological Perspective. Springer: Dordrecht, The Netherlands, 2004. [Google Scholar]
- Armstrong, B.K.; Kricker, A. Skin Cancer. Dermatol. Clin. 1995, 13, 583–594. [Google Scholar] [CrossRef] [PubMed]
- ICRP. The 2007 Recommendations of the International Commission on Radiological Protection. Ann. ICRP 2007, 103, 2–4. [Google Scholar]
- International Atomic Energy Agency. Radiation Protection. 2021. Available online: https://www.iaea.org/topics/radiation-protection (accessed on 9 May 2025).
- World Health Organization. Radiation. 2022. Available online: https://www.who.int/health-topics/radiation#tab=tab_3 (accessed on 9 May 2025).
- Alburayh, A.A.; Alosaimi, M.; Alshumiesy, H.; Alzahrani, A.T.; Alkhars, A.S.; Doaib, D.M.; Alsaleh, M.H.; Albakri, A.; Alrajhi, N.A.; Almansour, B.; et al. Assessment of Public Knowledge and Perceptions Toward Radiation Exposure Risks in Saudi Arabia: A Survey Study. Cureus 2025, 17, e80351. [Google Scholar] [CrossRef] [PubMed]
- Norwegian Radiation and Nuclear Safety Authority (DSA). What Can I Do?—DSA. 2024. Available online: https://www.dsa.no/en/preparedness/what-can-i-do (accessed on 16 May 2025).
- Radiation and Nuclear Safety Authority (STUK). Instructions for Members of the Public. 2024. Available online: https://stuk.fi/en/instructions-for-members-of-the-public (accessed on 16 May 2025).
- Overview. Available online: https://www.vision2030.gov.sa/en/overview (accessed on 22 February 2025).
- Alkharusi, H. A descriptive analysis and interpretation of data from Likert scales in educational and psychological research. Indian J. Psychol. Educ. 2022, 12, 13–16. [Google Scholar]
- Daniel, W.; Cross, C. Biostatistics: A Foundation for Analysis in the Health Sciences; Wiley: Hoboken, NJ, USA, 2013. [Google Scholar]
- Tavakol, M.; Dennick, R. Making sense of Cronbach’s alpha. Int. J. Med. Educ. 2011, 2, 53–55. [Google Scholar] [CrossRef] [PubMed]
- Al-Mefty, O.; Kersh, J.E.; Routh, A.; Smith, R.R. The long-term side effects of radiation therapy for benign brain tumors in adults. J. Neurosurg. 1990, 73, 502–512. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, P.K.; Wu, J.C. Radiation exposure from imaging tests: Is there an increased cancer risk? Expert Rev. Cardiovasc. Ther. 2011, 9, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Evans, K.M.; Bodmer, J.; Edwards, B.; Levins, J.; O’mEara, A.; Ruhotina, M.; Smith, R.; Delaney, T.; Hoffman-Contois, R.; Boccuzzo, L.; et al. An Exploratory Analysis of Public Awareness and Perception of Ionizing Radiation and Guide to Public Health Practice in Vermont. J. Environ. Public Health 2015, 2015, 476495. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.I.; Haims, A.H.; Monico, E.P.; Brink, J.A.; Forman, H.P. Diagnostic CT Scans: Assessment of Patient, Physician, and Radiologist Awareness of Radiation Dose and Possible Risks1. Radiology 2004, 231, 393–398. [Google Scholar] [CrossRef] [PubMed]
- Slovic, P. Perception of Risk. Science 1987, 236, 280–285. [Google Scholar] [CrossRef] [PubMed]
- Gavrilas, L.; Kotsis, K.T. Electromagnetic radiation: A comprehensive review of misconceptions. Eurasian J. Sci. Environ. Educ. 2024, 4, 19–38. [Google Scholar] [CrossRef] [PubMed]
- Bahakeem, B.; Binafeef, R.; Alammar, R.; Aljadaibi, A.; Alshammari, A.; Alshammari, F.; Orfi, M.; Babour, R.; Alyousif, S.; Radif, W.; et al. Knowledge, Attitude, and Perception Regarding Radiation Hazards and Protection among Saudi Arabia’s General Population. Arch. Pharm. Pract. 2024, 15, A06241538. [Google Scholar]
- Khamtuikrua, C.; Suksompong, S. Awareness about radiation hazards and knowledge about radiation protection among healthcare personnel: A quaternary care academic center–based study. SAGE Open Med. 2020, 8, 2050312120901733. [Google Scholar] [CrossRef] [PubMed]
- Salih, S.; Nordin, M.N.; Alkatheeri, A.; Nasser, A.; Saif, M.; Abdallah, Z.; Alderei, A.; Faisal, L.A.; Alhasan, M.; Hasaneen, M. Assessment of Nursing Students’ Awareness toward Ionizing Radiation: Cross-Sectional Study. Nurs. Rep. 2023, 13, 855–864. [Google Scholar] [CrossRef] [PubMed]
- Alkhayal, A.M.; Alothman, A.S.; Alathel, A.H.; Almaslamani, A.; Alfehaid, O.N.; Alhassan, I.A.; Alrabeeah, K.A.; Ghazwani, Y.G. Knowledge and attitude of radiation safety and the use of protective measures among healthcare workers in a tertiary center. Eur. Rev. Med. Pharmacol. Sci. 2023, 27, 2047–2051. [Google Scholar] [PubMed]
- Hunt, S.; Frewer, L.J.; Shepherd, R. Public trust in sources of information about radiation risks in the UK. J. Risk Res. 1999, 2, 167–180. [Google Scholar] [CrossRef]
- Flynn, J.; Slovic, P.; Mertz, C.K. Gender, race, and perception of environmental health risks. Risk Anal. 1994, 14, 1101–1108. [Google Scholar] [CrossRef] [PubMed]
- Sung, H.; Kim, J.U.; Lee, D.; Jin, Y.W.; Jo, H.; Jun, J.K.; Park, S.; Seo, S. Radiation risk perception and its associated factors among residents living near nuclear power plants: A nationwide survey in Korea. Nucl. Eng. Technol. 2022, 54, 1295–1300. [Google Scholar] [CrossRef]

| Characteristics | n | % |
|---|---|---|
| Age (years) | ||
| 18–24 | 257 | 28.9 |
| 25–34 | 142 | 16.0 |
| 35–44 | 157 | 17.7 |
| 45–54 | 178 | 20.0 |
| 55–60 | 81 | 9.1 |
| >60 | 57 | 6.4 |
| Sex | ||
| Male | 221 | 24.9 |
| Female | 667 | 75.1 |
| Education level | ||
| Primary/elementary education | 17 | 1.9 |
| High school | 169 | 19.0 |
| Diploma | 95 | 10.7 |
| Bachelor’s (BSc) degree | 520 | 58.6 |
| Postgraduate (MSc, PhD) degree | 87 | 9.8 |
| Nationality | ||
| Saudi | 840 | 94.6 |
| Non-Saudi | 48 | 5.4 |
| Geographic area | ||
| Central region | 152 | 17.1 |
| Western region | 640 | 72.1 |
| Eastern region | 18 | 2.0 |
| Southern region | 31 | 3.5 |
| Northern region | 47 | 5.3 |
| Place of residence | ||
| Rural | 29 | 3.3 |
| Urban | 859 | 96.7 |
| Professional background | ||
| Medical | 117 | 13.2 |
| Nonmedical | 771 | 86.8 |
| Employment Status | ||
| Student | 231 | 26.0 |
| Unemployed | 111 | 12.5 |
| Employed | 382 | 43.0 |
| Free work | 33 | 3.7 |
| Retired | 131 | 14.8 |
| Received any education or training on radiation protection | ||
| No | 706 | 79.5 |
| Yes | 109 | 12.3 |
| Unsure | 73 | 8.2 |
| Interested in learning about radiation protection | ||
| No | 25 | 2.8 |
| Yes | 786 | 88.5 |
| Unsure | 77 | 8.7 |
| Time spent in direct sunlight (10 AM to 4 PM) without protection | ||
| <30 min | 333 | 37.5 |
| 30–60 min | 120 | 13.5 |
| >1 h | 96 | 10.8 |
| Avoid direct sunlight | 212 | 23.9 |
| Unsure | 127 | 14.3 |
| Times you have had medical imaging (e.g., X-rays, CT, and MRI) in the past 2 years | ||
| None | 175 | 19.7 |
| Once | 151 | 17.0 |
| Twice | 168 | 18.9 |
| 3–5 times | 211 | 23.8 |
| >5 times | 140 | 15.8 |
| Unsure | 43 | 4.8 |
| Characteristics | Awareness Score | Attitude Score | ||
|---|---|---|---|---|
| Mean ± SD | p-Value | Mean ± SD | p-Value | |
| Age | ||||
| 18–24 | 3.40 ± 0.92 | 0.13 | 3.44 ± 0.78 | 0.01 * |
| 25–34 | 3.38 ± 0.89 | 3.49 ± 0.77 | ||
| 35–44 | 3.33 ± 0.96 | 3.67 ± 0.78 | ||
| 45–54 | 3.26 ± 0.79 | 3.64 ± 0.74 | ||
| 55–60 | 3.17 ± 0.92 | 3.44 ± 0.85 | ||
| >60 | 3.82 ± 0.81 | 3.74 ± 0.70 | ||
| Sex | ||||
| Male | 3.43 ± 1.00 | 0.03 * | 3.45 ± 0.89 | 0.02 * |
| Female | 3.31 ± 0.85 | 3.60 ± 0.75 | ||
| Education level | ||||
| Primary/Elementary | 3.54 ± 0.98 | 0.96 | 3.70 ± 0.63 | 0.20 |
| High School | 3.35 ± 1.00 | 3.48 ± 0.90 | ||
| Diploma | 3.38 ± 0.94 | 3.64 ± 0.79 | ||
| Bachelor’s (BSc) | 3.31 ± 0.85 | 3.57 ± 0.76 | ||
| Postgraduate (MSc, PhD) | 3.30 ± 0.89 | 3.46 ± 0.75 | ||
| Nationality | ||||
| Saudi | 3.34 ± 0.89 | 0.83 | 3.65 ± 0.79 | 0.39 |
| Non-Saudi | 3.33 ± 0.85 | 3.52 ± 0.63 | ||
| Geographical area | ||||
| Central region | 3.23 ± 0.85 | 0.02 * | 3.50 ± 0.73 | 0.08 |
| Eastern region | 3.33 ± 0.89 | 3.57 ± 0.79 | ||
| Western region | 3.75 ± 0.50 | 3.65 ± 0.71 | ||
| Southern region | 3.60 ± 1.12 | 3.77 ± 0.95 | ||
| Northern region | 3.29 ± 1.01 | 3.34 ± 0.83 | ||
| Place of residence | ||||
| Rural | 3.40 ± 1.23 | 0.36 | 3.78 ± 0.72 | 0.07 |
| Urban | 3.33 ± 0.88 | 3.55 ± 0.79 | ||
| Professional background | ||||
| Medical | 3.62 ± 0.99 | <0.01 * | 3.59 ± 0.87 | 0.45 |
| Non-medical | 3.29 ± 1.00 | 3.56 ± 0.77 | ||
| Employment status | ||||
| Student | 3.43 ± 0.92 | <0.01 * | 3.44 ± 0.80 | <0.01 * |
| Unemployed | 3.05 ± 0.93 | 3.39 ± 0.83 | ||
| Employed | 3.39 ± 0.86 | 3.64 ± 0.75 | ||
| Free work | 3.07 ± 0.92 | 3.41 ± 0.85 | ||
| Retired | 3.27 ± 0.86 | 3.63 ± 0.79 | ||
| Received any education or training on radiation protection | ||||
| No | 3.23 ± 0.86 | <0.01 * | 3.53 ± 0.75 | 0.55 |
| Yes | 3.85 ± 1.00 | 3.64 ± 1.02 | ||
| Unsure | 3.48 ± 0.76 | 3.57 ± 0.75 | ||
| Interested in learning about radiation protection | ||||
| No | 3.27 ± 0.90 | <0.01 * | 3.24 ± 0.74 | <0.01 * |
| Yes | 3.36 ± 0.89 | 3.60 ± 0.78 | ||
| Unsure | 2.96 ± 0.80 | 3.16 ± 0.80 | ||
| Time spent in direct sunlight (10 AM to 4 PM) without protection | ||||
| <30 min | 3.34 ± 0.86 | 0.02 * | 3.53 ± 0.74 | 0.38 |
| 30–60 min | 3.42 ± 0.98 | 3.56 ± 0.84 | ||
| >1 h | 3.52 ± 1.01 | 3.55 ± 0.93 | ||
| Avoid direct sunlight | 3.22 ± 0.90 | 3.59 ± 0.79 | ||
| Unsure | 3.26 ± 0.76 | 3.54 ± 0.72 | ||
| Times you have had medical imaging (e.g., X-rays, CT, and MRI) in the past 2 years | ||||
| None | 3.36 ± 0.93 | 0.13 | 3.54 ± 0.80 | 0.10 |
| Once | 3.21 ± 0.88 | 3.50 ± 0.82 | ||
| Twice | 3.37 ± 0.97 | 3.56 ± 0.83 | ||
| 3–5 times | 3.25 ± 0.86 | 3.55 ± 0.73 | ||
| >5 times | 3.49 ± 0.81 | 3.67 ± 0.76 | ||
| Unsure | 3.33 ± 0.85 | 3.32 ± 0.80 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alzahrani, H.M.; Alzahrani, F.; Aljohani, H.; Albalawi, S.; Aljurbua, S.; Elzaki, M.; Alsharif, W.; Alhummiany, B.; Gareeballah, A.; Altay, E.A.; et al. An Exploratory Analysis of Public Perspectives and Attitudes Towards Radiation in Saudi Arabia. Healthcare 2025, 13, 2538. https://doi.org/10.3390/healthcare13192538
Alzahrani HM, Alzahrani F, Aljohani H, Albalawi S, Aljurbua S, Elzaki M, Alsharif W, Alhummiany B, Gareeballah A, Altay EA, et al. An Exploratory Analysis of Public Perspectives and Attitudes Towards Radiation in Saudi Arabia. Healthcare. 2025; 13(19):2538. https://doi.org/10.3390/healthcare13192538
Chicago/Turabian StyleAlzahrani, Hanan M., Fahad Alzahrani, Hala Aljohani, Shouq Albalawi, Shatha Aljurbua, Maisa Elzaki, Walaa Alsharif, Bashair Alhummiany, Awadia Gareeballah, Eman Abdurhman Altay, and et al. 2025. "An Exploratory Analysis of Public Perspectives and Attitudes Towards Radiation in Saudi Arabia" Healthcare 13, no. 19: 2538. https://doi.org/10.3390/healthcare13192538
APA StyleAlzahrani, H. M., Alzahrani, F., Aljohani, H., Albalawi, S., Aljurbua, S., Elzaki, M., Alsharif, W., Alhummiany, B., Gareeballah, A., Altay, E. A., Elmahdi, T. S. A., Alsaedi, A., Abdallah, M. J., Jamjoom, L. G., & Almutairi, B. S. (2025). An Exploratory Analysis of Public Perspectives and Attitudes Towards Radiation in Saudi Arabia. Healthcare, 13(19), 2538. https://doi.org/10.3390/healthcare13192538






