Comparative Analysis of Traumatic Cardiac Arrest: Role of Early Intervention and Care Pathway
Abstract
1. Introduction
2. Materials and Methods
2.1. Regional Characteristics
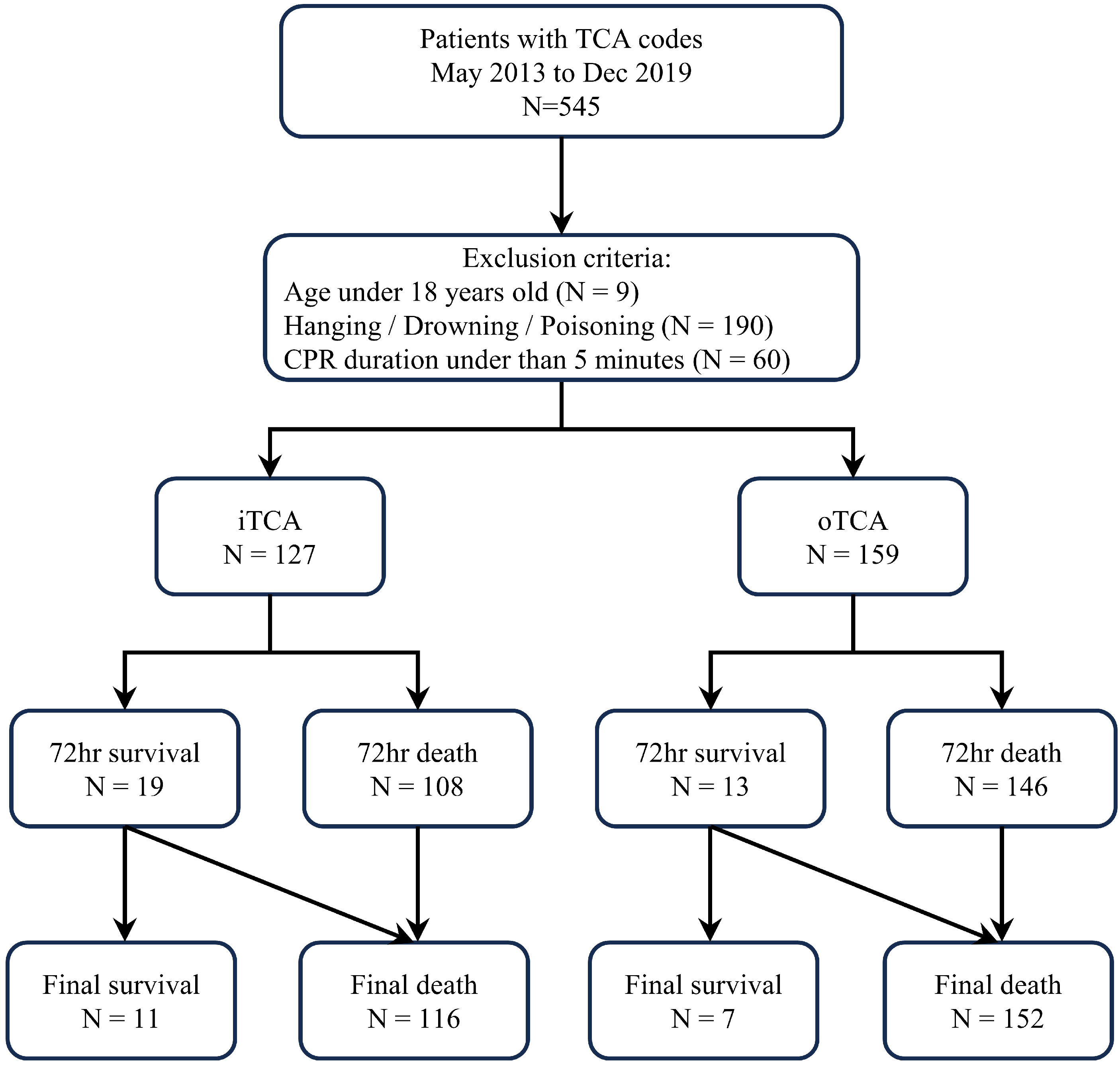
2.2. Study Design and Population
2.3. Data Collection
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
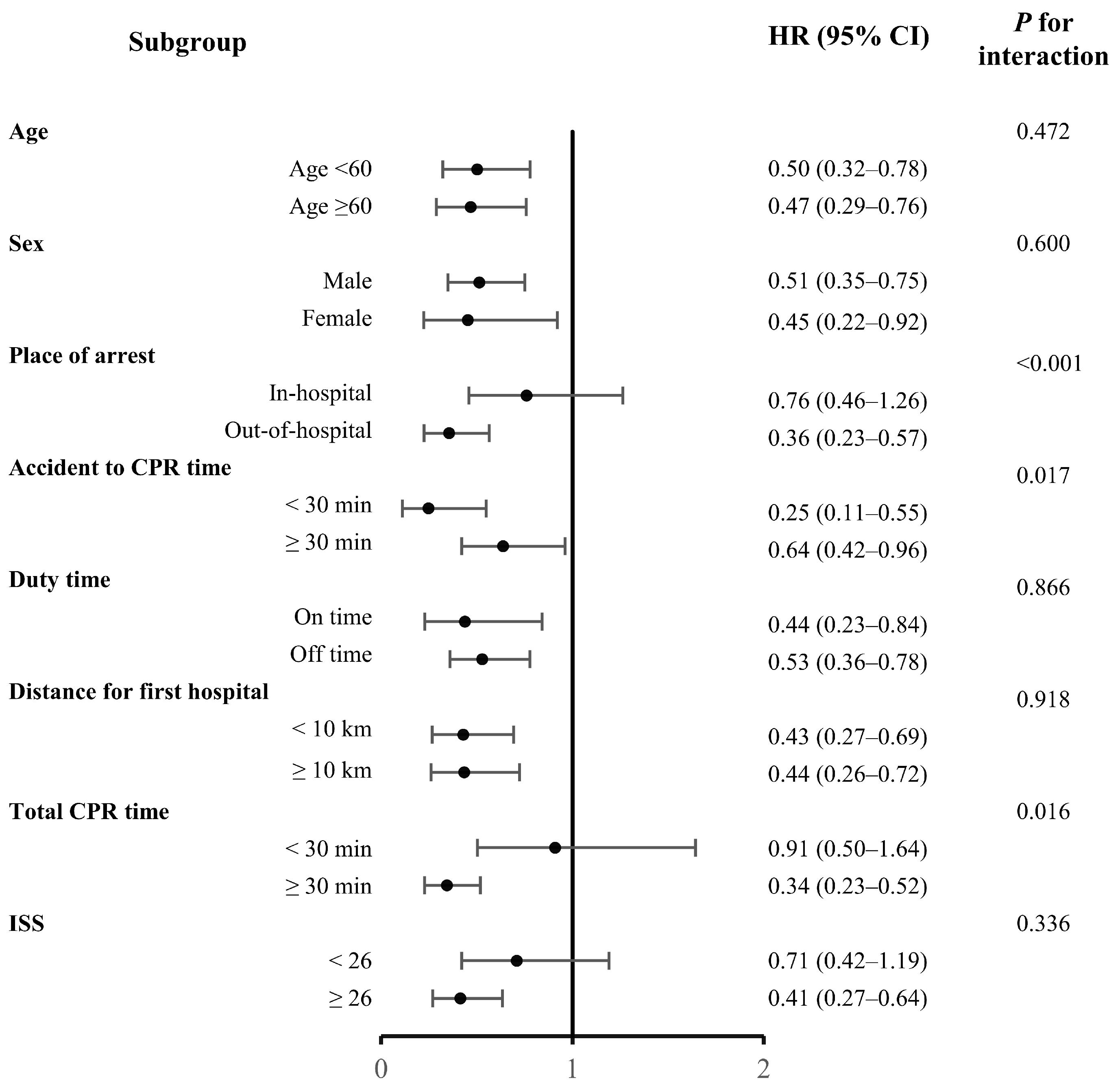
3.2. Cox Proportional Hazards Regression Analysis
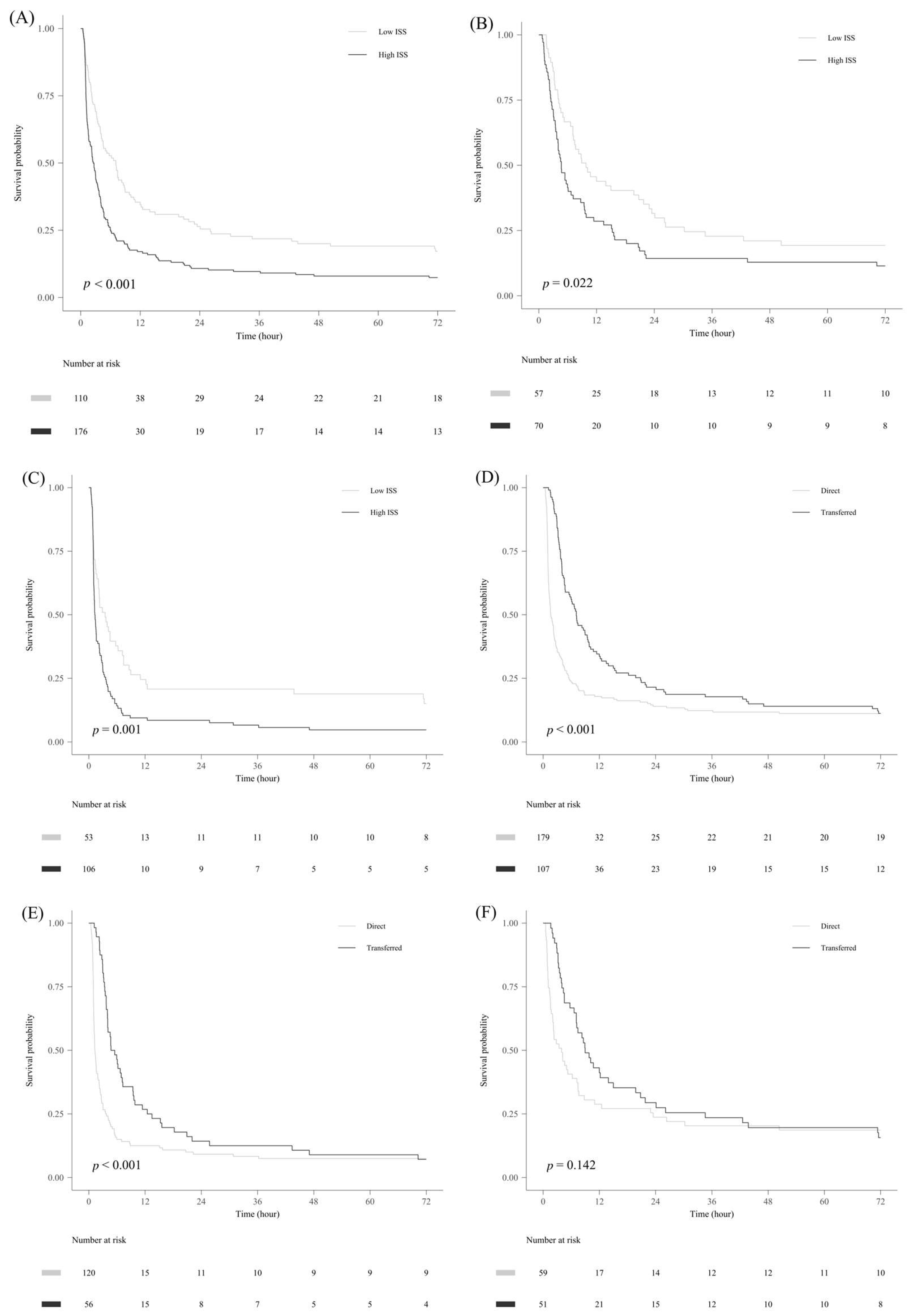
3.3. Kaplan–Meier Survival Analysis
3.4. Subgroup Analysis Based on Transfer Status
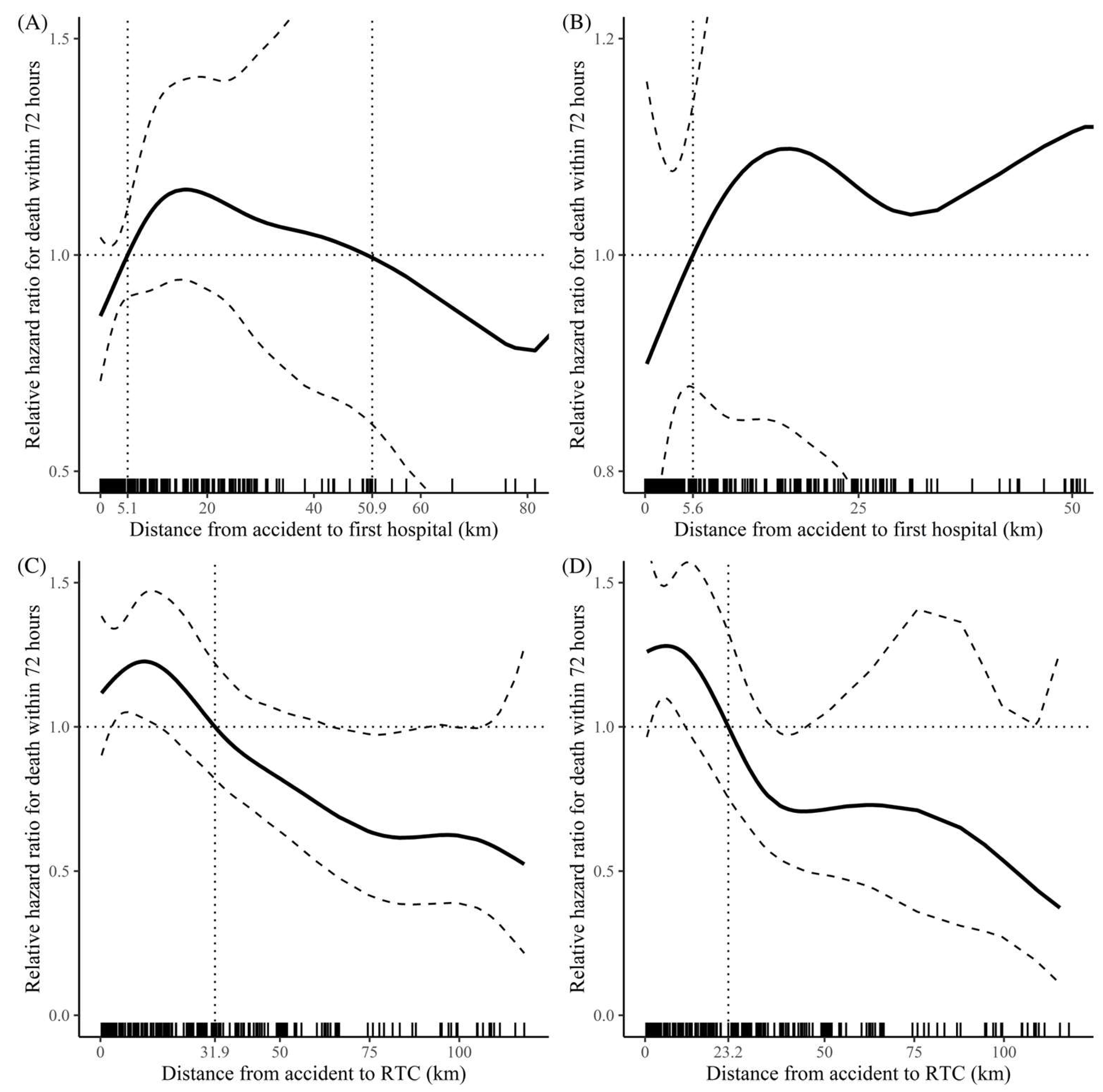
3.5. Restricted Cubic Spline Curve Analysis for Distance
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Kwon, J.; Lee, M.; Moon, J.; Huh, Y.; Song, S.; Kim, S.; Lee, S.J.; Lim, B.; Kim, H.J.; Kim, Y.; et al. National Follow-up Survey of Preventable Trauma Death Rate in Korea. J. Korean Med. Sci. 2022, 37, e349. [Google Scholar] [CrossRef]
- Lockey, D.; Crewdson, K.; Davies, G. Traumatic cardiac arrest: Who are the survivors? Ann. Emerg. Med. 2006, 48, 240–244. [Google Scholar] [CrossRef] [PubMed]
- Paffrath, T.; Lefering, R.; Flohe, S.; Trauma Register, D.G.U. How to define severely injured patients?—An Injury Severity Score (ISS) based approach alone is not sufficient. Injury 2014, 45 (Suppl. S3), S64–S69. [Google Scholar] [CrossRef] [PubMed]
- Im, C.W.L.T.; Ohk, T.G.; Kim, O.H.; Jung, S.K.; Kim, Y.; Ma, B.S.; Ahn, M.E.; Seo, J.Y.; Kim, D.W. Outcome of cardiopulmonary resuscitation for prehospital traumatic cardiac arrest: Focused on Gangwon province. J. Korean Soc. Emerg. Med. 2020, 31, 135–145. [Google Scholar]
- Deasy, C.; Bray, J.; Smith, K.; Harriss, L.; Morrison, C.; Bernard, S.; Cameron, P. Traumatic out-of-hospital cardiac arrests in Melbourne, Australia. Resuscitation 2012, 83, 465–470. [Google Scholar] [CrossRef]
- Huber-Wagner, S.; Lefering, R.; Qvick, M.; Kay, M.V.; Paffrath, T.; Mutschler, W.; Kanz, K.-G. Outcome in 757 severely injured patients with traumatic cardiorespiratory arrest. Resuscitation 2007, 75, 276–285. [Google Scholar] [CrossRef]
- Crewdson, K.; Lockey, D. Mortality in traumatic cardiac arrest. Resuscitation 2017, 113, e21. [Google Scholar] [CrossRef]
- Kim, S.M.; Hwang, S.O.; Lee, K.H.; Lee, J.W.; Hong, E.S.; Kim, H.; Lim, K.S. Outcome of Resuscitation Attempt in Patients with Cardiac Arrest from Trauma. J. Korean Soc. Traumatol. 1997, 10, 200–206. [Google Scholar]
- Harris, T.; Masud, S.; Lamond, A.; Abu-Habsa, M. Traumatic cardiac arrest: A unique approach. Eur. J. Emerg. Med. 2015, 22, 72–78. [Google Scholar] [CrossRef]
- Smith, J.E.; Rickard, A.; Wise, D. Traumatic cardiac arrest. J. R. Soc. Med. 2015, 108, 11–16. [Google Scholar] [CrossRef]
- Soar, J.; Perkins, G.D.; Abbas, G.; Alfonzo, A.; Barelli, A.; Bierens, J.J.; Brugger, H.; Deakin, C.D.; Dunning, J.; Georgiou, M.; et al. European Resuscitation Council Guidelines for Resuscitation 2010 Section 8. Cardiac arrest in special circumstances: Electrolyte abnormalities, poisoning, drowning, accidental hypothermia, hyperthermia, asthma, anaphylaxis, cardiac surgery, trauma, pregnancy, electrocution. Resuscitation 2010, 81, 1400–1433. [Google Scholar] [CrossRef]
- Hwang, K.; Jung, K.; Kwon, J.; Moon, J.; Heo, Y.; Lee, J.C.J.; Huh, Y. Distribution of Trauma Deaths in a Province of Korea: Is “Trimodal” Distribution Relevant Today? Yonsei Med. J. 2020, 61, 229–234. [Google Scholar] [CrossRef]
- Jung, K.; Kim, I.; Park, S.K.; Cho, H.; Park, C.Y.; Yun, J.H.; Kim, O.H.; Park, J.O.; Lee, K.-J.; Hong, K.J.; et al. Preventable Trauma Death Rate after Establishing a National Trauma System in Korea. J. Korean Med. Sci. 2019, 34, e65. [Google Scholar] [CrossRef] [PubMed]
- Yu, B.; Lee, G.; Lee, M.A.; Choi, K.; Hyun, S.; Jeon, Y.; Yoon, Y.-C.; Lee, J. Trauma Volume and Performance of a regional Trauma Center in Korea: Initial 5-year analysis. J. Trauma Inj. 2020, 33, 31–37. [Google Scholar] [CrossRef]
- Park, D.J.; Park, C.Y.; Cho, H.M.; Lee, K.H.; Han, H.-S. Current status and future prospects of trauma centers in Korea. J. Korean Med. Assoc. 2017, 60, 530–532. [Google Scholar] [CrossRef]
- Esposito, T.J.; Crandall, M.; Reed, R.L.; Gamelli, R.L.; Luchette, F.A. Socioeconomic factors, medicolegal issues, and trauma patient transfer trends: Is there a connection? J. Trauma 2006, 61, 1380–1386; discussion 1386–1388. [Google Scholar] [CrossRef]
- Sandroni, C.; D’Arrigo, S.; Nolan, J.P. Prognostication after cardiac arrest. Crit. Care 2018, 22, 150. [Google Scholar] [CrossRef]
- Lee, D.H.; Lee, B.K.; Cho, Y.S.; Jung, Y.H.; Lee, H.Y.; You, Y.H.; Lee, D.H.; Kim, Y.H.; Cha, K.-C.; Jeung, K.W. Slow Heart Rate Within 72 Hours After Cardiac Arrest Is Associated with Good Neurologic Outcome in Out-of-Hospital Cardiac Arrest Survivors Who Undergo Targeted Temperature Management with 33 °C. Ther. Hypothermia Temp. Manag. 2021, 11, 145–154. [Google Scholar] [CrossRef]
- Rajajee, V.; Muehlschlegel, S.; Wartenberg, K.E.; Alexander, S.A.; Busl, K.M.; Chou, S.H.Y.; Creutzfeldt, C.J.; Fontaine, G.V.; Fried, H.; Hocker, S.E. Guidelines for Neuroprognostication in Comatose Adult Survivors of Cardiac Arrest. Neurocrit Care 2023, 38, 533–563. [Google Scholar] [CrossRef]
- Pickens, J.J.; Copass, M.K.; Bulger, E.M. Trauma patients receiving CPR: Predictors of survival. J. Trauma 2005, 58, 951–958. [Google Scholar] [CrossRef]
- Fulton, R.L.; Voigt, W.J.; Hilakos, A.S. Confusion surrounding the treatment of traumatic cardiac arrest. J. Am. Coll. Surg. 1995, 181, 209–214. [Google Scholar]
- Stratton, S.J.; Brickett, K.; Crammer, T. Prehospital pulseless, unconscious penetrating trauma victims: Field assessments associated with survival. J. Trauma 1998, 45, 96–100. [Google Scholar] [CrossRef] [PubMed]
- Dane, F.C.; Russell-Lindgren, K.S.; Parish, D.C.; Durham, M.D.; Brown, T.D. In-hospital resuscitation: Association between ACLS training and survival to discharge. Resuscitation 2000, 47, 83–87. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.C.; Wu, K.H.; Hsiao, K.Y.; Hung, M.S.; Lai, Y.C.; Chen, Y.S.; Chang, C.-Y. Factors associated with outcomes in traumatic cardiac arrest patients without prehospital return of spontaneous circulation. Injury 2019, 50, 4–9. [Google Scholar] [CrossRef] [PubMed]
- Faucher, A.; Savary, D.; Jund, J.; Dorez, D.; Debaty, G.; Gaillard, A.; Atchabahian, A.; Tazarourte, K. Out-of-hospital traumatic cardiac arrest: An underrecognized source of organ donors. Transpl. Int. 2014, 27, 42–48. [Google Scholar] [CrossRef]
- Evans, C.C.; Petersen, A.; Meier, E.N.; Buick, J.E.; Schreiber, M.; Kannas, D.; Delores, R.N.; Michael, A.; MBBS the Resuscitation Outcomes Consortium Investigators. Prehospital traumatic cardiac arrest: Management and outcomes from the resuscitation outcomes consortium epistry-trauma and PROPHET registries. J. Trauma Acute Care Surg. 2016, 81, 285–293. [Google Scholar] [CrossRef]
- Beck, B.; Smith, K.; Mercier, E.; Bernard, S.; Jones, C.; Meadley, B.; Clair, T.S.; Jennings, P.A.; Nehme, Z.; Burke, M.; et al. Potentially preventable trauma deaths: A retrospective review. Injury 2019, 50, 1009–1016. [Google Scholar] [CrossRef]
- Chiara, O.; Cimbanassi, S.; Pitidis, A.; Vesconi, S. Preventable trauma deaths: From panel review to population based-studies. World J. Emerg. Surg. 2006, 1, 12. [Google Scholar] [CrossRef]

| All Patients (N = 286) | 72 h Survival (N = 32) | 72 h Death (N = 254) | p Value | |
|---|---|---|---|---|
| Sex | 0.970 | |||
| Male | 193 (67.5%) | 21 (65.6%) | 172 (67.7%) | |
| Female | 93 (32.5%) | 11 (34.4%) | 82 (32.3%) | |
| Age (years) | 59.0 [45.0; 71.0] | 59.0 [45.5; 65.0] | 59.0 [45.0; 73.0] | 0.408 |
| Ways of visit | 0.443 | |||
| EMS | 179 (62.6%) | 21 (65.6%) | 158 (62.2%) | |
| Hospital ambulance | 20 (7.0%) | 4 (12.5%) | 16 (6.3%) | |
| Private ambulance | 55 (19.2%) | 6 (18.8%) | 49 (19.3%) | |
| Air transportation | 30 (10.5%) | 1 (3.1%) | 29 (11.4%) | |
| Private vehicle | 2 (0.7%) | 0 (0.0%) | 2 (0.8%) | |
| Drunken state | 0.385 | |||
| Yes | 14 (4.9%) | 3 (9.4%) | 11 (4.3%) | |
| No | 164 (57.3%) | 19 (59.4%) | 145 (57.1%) | |
| Unknown | 108 (37.8%) | 10 (31.2%) | 98 (38.6%) | |
| Protection | 0.298 | |||
| Yes | 37 (12.9%) | 5 (15.6%) | 32 (12.6%) | |
| No | 182 (63.6%) | 23 (71.9%) | 159 (62.6%) | |
| Unknown | 67 (23.4%) | 4 (12.5%) | 63 (24.8%) | |
| ISS | 34.0 [22.0; 75.0] | 24.5 [17.0; 32.0] | 34.0 [24.0; 75.0] | <0.001 |
| AIS1 (head and neck) | 2.0 [0.0; 4.0] | 2.0 [0.0; 4.0] | 2.0 [0.0; 4.0] | 0.851 |
| AIS2 (face) | 0.0 [0.0; 0.0] | 0.0 [0.0; 2.0] | 0.0 [0.0; 0.0] | 0.006 |
| AIS3 (thorax) | 3.0 [0.0; 4.0] | 3.0 [0.0; 4.0] | 3.0 [0.0; 4.0] | 0.353 |
| AIS4 (abdomen and pelvis) | 0.0 [0.0; 2.0] | 0.0 [0.0; 2.0] | 0.0 [0.0; 2.0] | 0.379 |
| AIS5 (extremities) | 1.0 [0.0; 3.0] | 0.0 [0.0; 2.0] | 1.0 [0.0; 3.0] | 0.329 |
| AIS6 (external) | 0.0 [0.0; 0.0] | 0.0 [0.0; 0.0] | 0.0 [0.0; 0.0] | 0.022 |
| Place of cardiac arrest | 0.063 | |||
| Out of hospital | 159 (55.8%) | 13 (40.6%) | 146 (57.7%) | |
| First hospital | 4 (1.4%) | 1 (3.1%) | 3 (1.2%) | |
| ED of RTC | 81 (28.4%) | 15 (46.9%) | 66 (26.1%) | |
| Ward of RTC | 42 (14.7%) | 3 (9.4%) | 39 (15.4%) | |
| Pathway | 1.000 | |||
| Directly transported | 179 (62.6%) | 20 (62.5%) | 159 (62.6%) | |
| Transferred | 107 (37.4%) | 12 (37.5%) | 95 (37.4%) | |
| Duty time | 1.000 | |||
| Off-duty time | 206 (72.0%) | 23 (71.9%) | 183 (72.0%) | |
| On-duty time | 80 (28.0%) | 9 (28.1%) | 71 (28.0%) |
| All Patients (N = 286) | 72 h Survival (N = 32) | 72 h Death (N = 254) | p Value | |
|---|---|---|---|---|
| Total collapse time (min) | 37.5 [22.0; 55.0] | 12.0 [5.0; 25.5] | 40.0 [28.0; 57.0] | <0.001 |
| Total CPR time (min) | 35.0 [21.0; 49.0] | 10.0 [5.0; 21.0] | 36.0 [25.0; 51.0] | <0.001 |
| OHCA time (min) (N = 159) | 24.0 [14.0; 37.0] | 17.0 [12.0; 29.0] | 24.0 [15.0; 39.0] | 0.123 |
| OHCPR time (min) (N = 159) | 17.0 [10.0; 26.5] | 14.0 [7.0; 19.0] | 17.0 [10.0; 27.0] | 0.003 |
| IHCA time (min) | 24.0 [12.0; 32.0] | 6.0 [2.5; 10.5] | 27.0 [16.0; 34.0] | <0.001 |
| Time to CPR time (min) | 36.0 [14.0; 130.0] | 33.5 [13.5; 170.5] | 36.5 [14.0; 127.0] | 0.974 |
| Distance to RTC (km) | 18.1 [3.5; 42.7] | 9.6 [2.3; 45.0] | 19.5 [3.9; 42.7] | 0.368 |
| Distance to 1st hospital (km) | 4.5 [1.8; 18.0] | 2.6 [1.6; 7.7] | 5.5 [1.8; 19.0] | 0.145 |
| Distance from 1st hospital to RTC (km) (N = 107) | 41.1 [32.8; 61.3] | 41.1 [32.8; 88.4] | 41.1 [32.8; 49.4] | 0.361 |
| ROSC | 98 (34.3%) | 32 (100.0%) | 66 (26.0%) | <0.001 |
| Operation | 73 (25.5%) | 19 (59.4%) | 54 (21.3%) | <0.001 |
| Chest tube | 126 (44.1%) | 16 (50.0%) | 110 (43.3%) | 0.596 |
| Pelvic binder | 28 (9.8%) | 1 (3.1%) | 27 (10.6%) | 0.303 |
| ECMO | 5 (1.7%) | 2 (6.2%) | 3 (1.2%) | 0.178 |
| REBOA | 12 (4.2%) | 0 (0.0%) | 12 (4.7%) | 0.430 |
| Angiography | 10 (3.5%) | 2 (6.2%) | 8 (3.1%) | 0.697 |
| Transfusion (RBC) (mL) | 3200.0 [0.0; 8400.0] | 7720.0 [4020.0; 20,360.0] | 3120.0 [0.0; 7520.0] | <0.001 |
| Transfusion (FFP) (mL) | 1600.0 [0.0; 6400.0] | 4920.0 [2000.0; 19,800.0] | 0.0 [0.0; 6400.0] | <0.001 |
| Transfusion (PC) (mL) | 0.0 [0.0; 0.0] | 4320.0 [0.0; 7800.0] | 0.0 [0.0; 0.0] | <0.001 |
| Place of death | <0.001 | |||
| Emergency department | 168 (58.7%) | 0 (0.0%) | 168 (66.1%) | |
| Intensive care unit | 81 (28.3%) | 0 (0.0%) | 70 (27.5%) | |
| Operation room | 12 (4.2%) | 0 (0.0%) | 12 (4.7%) | |
| DAMA | 5 (1.7%) | 2 (6.2%) | 3 (1.2%) | |
| General ward | 1 (0.3%) | 0 (0.0%) | 1 (0.4%) | |
| Organ harvest | 1 (0.3%) | 1 (3.1%) | 0 (0.0%) |
| Variable | Unadjusted | Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|---|---|
| HR (95% CI) | p | HR (95% CI) | p | HR (95% CI) | p | HR (95% CI) | p | |
| Age | 1.00 (0.99–1.00) | 0.182 | 1.00 (0.99–1.01) | 0.826 | 1.00 (1.00–1.01) | 0.320 | 1.01 (1.00–1.01) | 0.105 |
| Sex | ||||||||
| Female | (Reference) | (Reference) | (Reference) | (Reference) | ||||
| Male | 1.07 (0.83–1.40) | 0.593 | 0.93 (0.71–1.22) | 0.606 | 0.93 (0.71–1.22) | 0.605 | 0.98 (0.75–1.28) | 0.881 |
| Pathway | ||||||||
| Direct | (Reference) | (Reference) | (Reference) | (Reference) | ||||
| Transferred | 0.78 (0.70–0.86) | <0.001 | 0.78 (0.71–0.86) | <0.001 | 0.86 (0.77–0.96) | 0.006 | 0.86 (0.76–0.97) | 0.014 |
| Place of arrest | ||||||||
| In | (Reference) | (Reference) | (Reference) | (Reference) | ||||
| Out | 1.16 (1.08–1.25) | <0.001 | 1.16 (1.08–1.25) | <0.001 | 1.12 (1.04–1.21) | 0.003 | 1.02 (0.91–1.14) | 0.716 |
| Accident to CPR time | 0.88 (0.84–0.94) | <0.001 | 0.93 (0.88–0.98) | 0.007 | 0.95 (0.90–0.99) | 0.050 | ||
| Duty time | ||||||||
| Off-duty time | (Reference) | (Reference) | (Reference) | |||||
| On-duty time | 0.85 (0.65–1.12) | 0.250 | 0.83 (0.62–1.09) | 0.182 | 0.73 (0.54–0.97) | 0.028 | ||
| Distance to 1st hospital | 1.00 (0.99–1.00) | 0.704 | 1.00 (0.99–1.00) | 0.518 | 1.00 (0.99–1.00) | 0.607 | ||
| Total CPR time | 1.00 (1.00–1.01) | 0.057 | 1.00 (1.00–1.01) | 0.018 | ||||
| ISS | 1.03 (1.02–1.04) | <0.001 | 1.03 (1.02–1.03) | <0.001 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jang, S.W.; Chung, J.S.; Jung, P.Y. Comparative Analysis of Traumatic Cardiac Arrest: Role of Early Intervention and Care Pathway. Healthcare 2025, 13, 2532. https://doi.org/10.3390/healthcare13192532
Jang SW, Chung JS, Jung PY. Comparative Analysis of Traumatic Cardiac Arrest: Role of Early Intervention and Care Pathway. Healthcare. 2025; 13(19):2532. https://doi.org/10.3390/healthcare13192532
Chicago/Turabian StyleJang, Sung Woo, Jae Sik Chung, and Pil Young Jung. 2025. "Comparative Analysis of Traumatic Cardiac Arrest: Role of Early Intervention and Care Pathway" Healthcare 13, no. 19: 2532. https://doi.org/10.3390/healthcare13192532
APA StyleJang, S. W., Chung, J. S., & Jung, P. Y. (2025). Comparative Analysis of Traumatic Cardiac Arrest: Role of Early Intervention and Care Pathway. Healthcare, 13(19), 2532. https://doi.org/10.3390/healthcare13192532






