Prioritizing Pediatric Eye Care in Saudi Arabia: A National Delphi Consensus Study
Abstract
1. Introduction
2. Materials and Methods
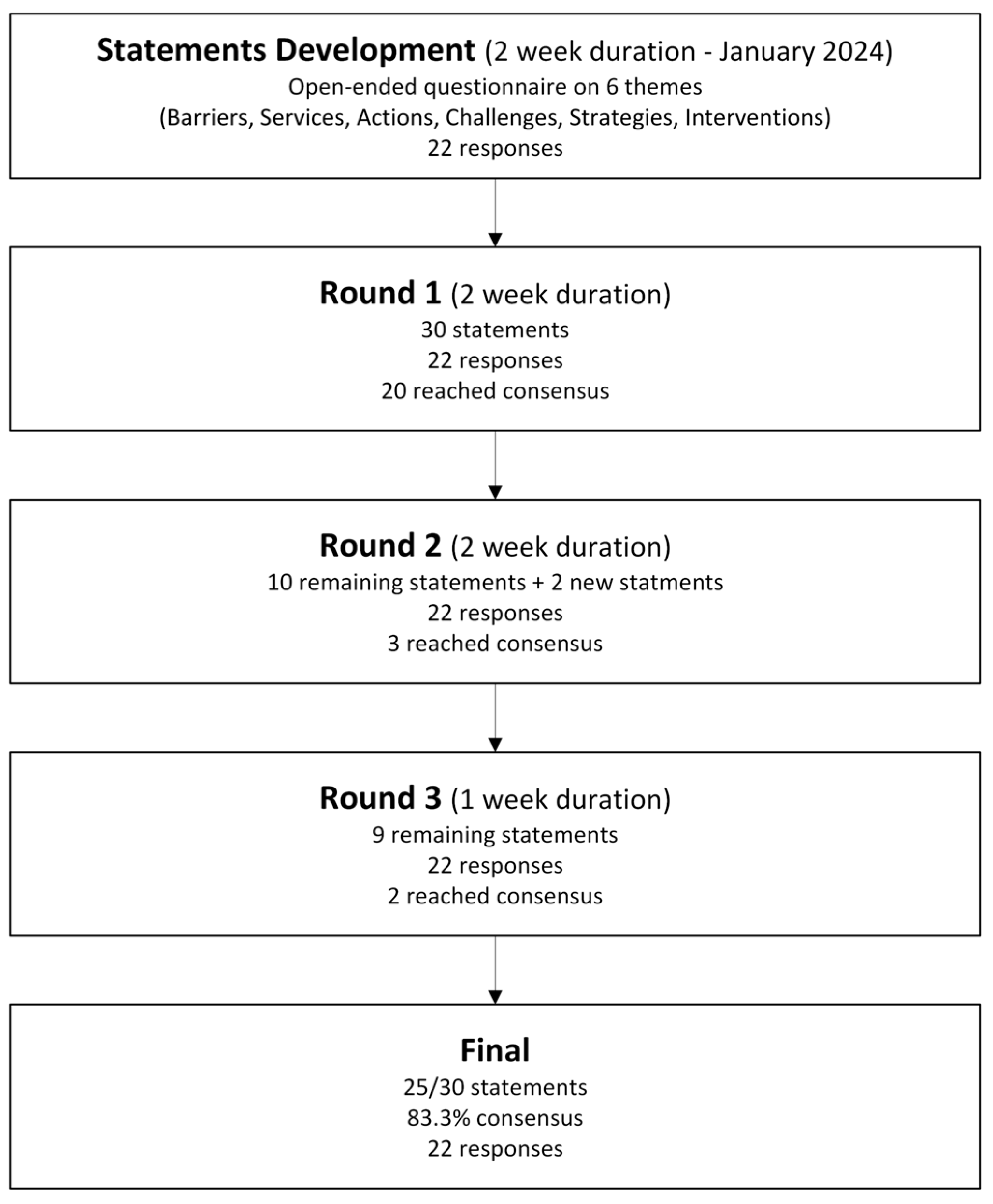
2.1. Study Design
2.2. Participant Selection
2.3. Inclusion Criteria
2.4. Ethical Approval
2.5. Panel Size
2.6. Delphi Process
2.7. Delphi Statement Development
- Barriers to accessing childhood eye care.
- Services and instruments for children with visual impairment.
- Actions needed to develop a national childhood eye care plan.
- Challenges faced by families of children with visual impairment.
- Strategies to improve childhood eye care services.
- Interventions to overcome access barriers.
2.7.1. Round One
2.7.2. Round Two
2.7.3. Round Three
2.8. Analysis
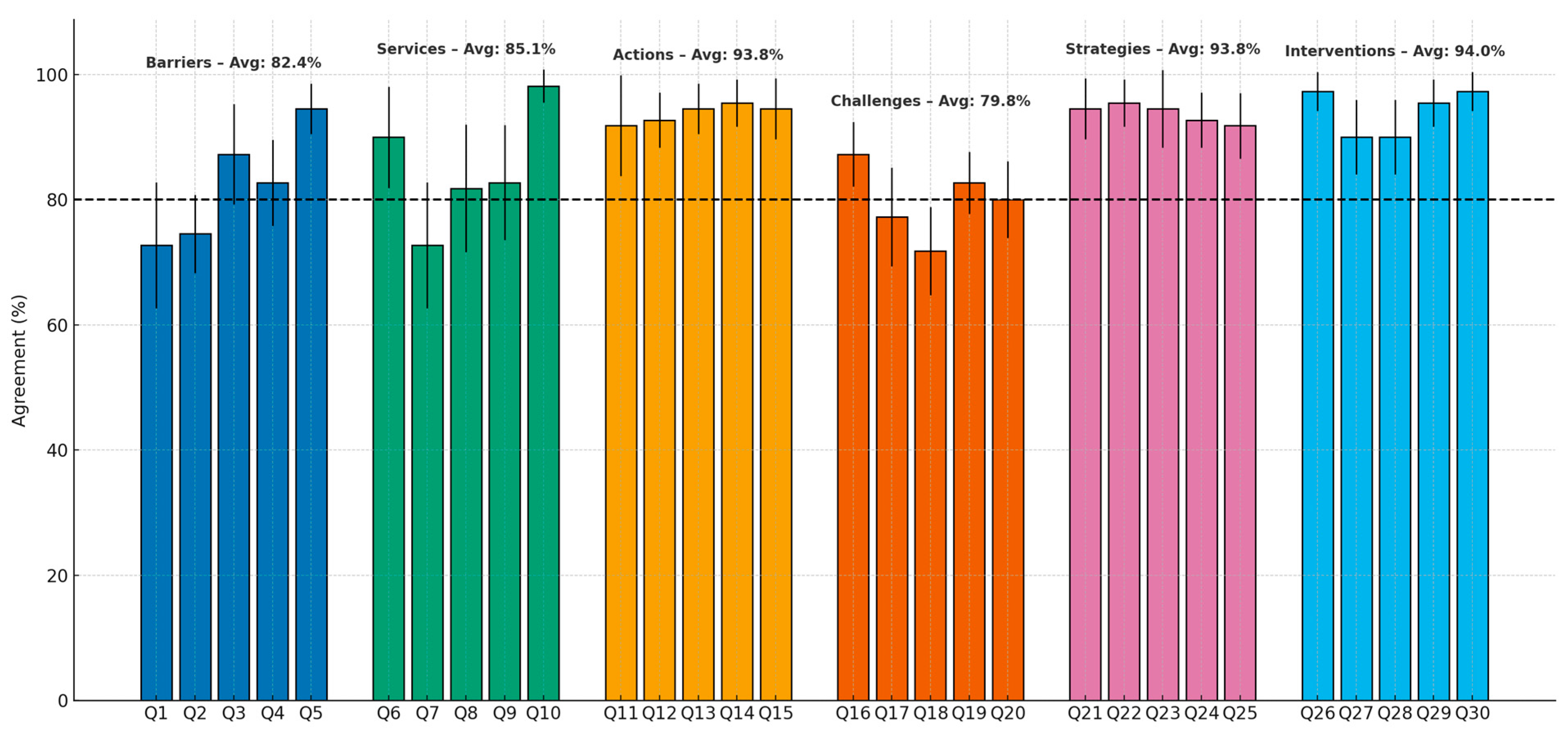
3. Results
4. Discussion
4.1. High Consensus Areas
- Integration of optometrists: Strong agreement was observed regarding the integration of optometrists into primary healthcare and the expansion of their roles.
- Mandatory school vision screening: There was unanimous support for implementing mandatory vision screening programs, particularly those aligned with vaccination schedules and school entry.
- Workforce development: High consensus emphasized the need to train and recruit additional pediatric eye care specialists.
- Public awareness: Participants supported launching nationwide campaigns to increase awareness of pediatric eye health.
- Infrastructure expansion: There was agreement on the need to establish specialized pediatric eye care clinics and introduce mobile eye clinics to improve accessibility.
4.2. Areas Requiring Further Attention (<80% Agreement)
- Shortage of pediatric eye care specialists (72.86%): Some participants may have perceived the current workforce as sufficient or had differing views regarding specialist distribution.
- Challenges with the government referral system (74.29%): Opinions varied concerning the complexity and usability of the referral system for parents.
- Need for specialized diagnostic tools (72.86%): Differences emerged regarding the necessity and prioritization of advanced tools such as photoscreeners and autorefractors.
- Access difficulties for families (77.14%): Participants reported varying experiences and perceptions with families’ ability to access specialized eye care.
- School accommodations for children with visual impairment (71.43%): Disparities in school resources across regions may have influenced participant responses.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| WHO | World Health Organization |
| IRB | Institutional review board |
| OD | Optometry doctor |
References
- Darraj, A.; Barakat, W.; Kenani, M.; Shajry, R.; Khawaji, A.; Bakri, S.; Makin, A.; Mohanna, A.; Yassin, A.O. Common Eye Diseases in Children in Saudi Arabia (Jazan). Ophthalmol. Eye Dis. 2016, 8, 33–39. [Google Scholar] [CrossRef]
- GBD 2019 Blindness and Vision Impairment Collaborators; Vision Loss Expert Group of the Global Burden of Disease Study. Trends in prevalence of blindness and distance and near vision impairment over 30 years: An analysis for the Global Burden of Disease Study. Lancet Glob. Health 2021, 9, e130–e143. [Google Scholar] [CrossRef]
- Gilbert, C.; Foster, A. Childhood blindness in the context of VISION 2020—The right to sight. Bull. World Health Organ. 2001, 79, 227–232. [Google Scholar]
- Burton, M.J.; Ramke, J.; Marques, A.P.; Bourne, R.R.; Congdon, N.; Jones, I.; Ah Tong, B.A.M.; Arunga, S.; Bachani, D.; Bascaran, C.; et al. The Lancet Global Health Commission on global eye health: Vision beyond 2020. Lancet Glob. Health 2021, 9, e489–e551. [Google Scholar] [CrossRef] [PubMed]
- Alrasheed, S. Systematic review and meta-analysis of childhood visual impairment in the Eastern Mediterranean Region. East. Mediterr. Health J. 2023, 29, 482–490. [Google Scholar] [CrossRef] [PubMed]
- Gonsalves, S.; Ganagi, S.; Vivedkanad, U. School screening in Coastal Karnataka. Rom. J. Ophthalmol. 2019, 63, 245–248. [Google Scholar] [CrossRef]
- IAPB. Vision and Hearing Screening for School-Age Children: Implementation Handbook. 2024. Available online: https://www.iapb.org/learn/resources/vision-and-hearing-screening-for-school-age-children-implementation-handbook/ (accessed on 16 September 2025).
- Al-Rowaily, M.A. Prevalence of refractive errors among pre-school children at King Abdulaziz Medical City, Riyadh, Saudi Arabia. Saudi J. Ophthalmol. 2010, 24, 45–48. [Google Scholar] [CrossRef] [PubMed]
- Moafa, M.A.; Alrasheed, S.H. Status of Childhood Eye Care Services in the Kingdom of Saudi Arabia: Eye Care Professionals’ Perspectives. Open Ophthalmol. J. 2022, 16, e187436412206200. [Google Scholar] [CrossRef]
- Donaldson, L.; Subramanian, A.; Conway, M.L. Eye care in young children: A parent survey exploring access and barriers. Clin. Exp. Optom. 2018, 101, 521–526. [Google Scholar] [CrossRef]
- Wang, P.; Bianchet, S.; Carter, M.; Hopman, W.; Law, C. Utilization and barriers to eye care following school-wide pediatric vision screening. Can. J. Ophthalmol. 2023, 58, 465–471. [Google Scholar] [CrossRef]
- Kemmanu, V.; Giliyar, S.K.; Shetty, B.K.; Singh, A.K.; Kumaramanickavel, G.; McCarty, C.A. Parental inability to detect eye diseases in children: Barriers to access of childhood eye-care services in south India. Eye 2018, 32, 467–468. [Google Scholar] [CrossRef]
- Carley, S.D.; Mackway-Jones, K.; Donnan, S. Delphi study into planning for care of children in major incidents. Arch. Dis. Child. 1999, 80, 406–409. [Google Scholar] [CrossRef]
- Prakash, W.D.; Marmamula, S.; Keeffe, J.; Khanna, R.C. Effective refractive error coverage and spectacle coverage among school children in Telangana, South India. Eye 2024, 38, 2143–2149. [Google Scholar] [CrossRef]
- Zhu, Z.; Chen, Y.; Tan, Z.; Xiong, R.; McGuinness, M.B.; Müller, A. Interventions recommended for myopia prevention and control among children and adolescents in China: A systematic review. Br. J. Ophthalmol. 2023, 107, 160–166. [Google Scholar] [CrossRef]
- Zhuo, D.; Chen, S.; Ren, X.; Wang, B.; Liu, L.; Xiao, L. The prevalence of lower eyelid epiblepharon and its association with refractive errors in Chinese preschool children: A cross-sectional study. BMC Ophthalmol. 2021, 21, 3. [Google Scholar] [CrossRef] [PubMed]
- Zuo, H.; Huang, B.; He, J.; Fang, L.; Huang, M. Machine Learning Approaches in High Myopia: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2025, 27, e57644. [Google Scholar] [CrossRef] [PubMed]
- Sherief, S.T.; Tesfaye, S.; Eshetu, Z.; Ali, A.; Dimaras, H. Child eye health in Ethiopia: A mixed methods analysis of policy and commitment to action. BMJ Open 2023, 13, e075622. [Google Scholar] [CrossRef] [PubMed]
- McKenna, H.; McDonough, S.; Keeney, S.; Hasson, F.; Lagan, K.; Ward, M.; Kelly, G.; Duffy, O. Research priorities for the therapy professions in Northern Ireland and the Republic of Ireland: A comparison of findings from a Delphi consultation. J. Allied Health 2014, 43, 98–109. [Google Scholar]
- Alrasheed, S.H.; Naidoo, K.S.; Clarke-Farr, P.C.; Binnawi, K.H. Building consensus for the development of child eye care services in South Darfur State of Sudan using the Delphi technique. Afr. J. Prim. Health Care Fam. Med. 2018, 10, e1–e9. [Google Scholar] [CrossRef]
- McCormick, I.; Mactaggart, I.; Resnikoff, S.; Muirhead, D.; Murthy, G.V.; Silva, J.C.; Bastawrous, A.; Stern, J.; Blanchet, K.; Wang, N.; et al. Eye health indicators for universal health coverage: Results of a global expert prioritisation process. Br. J. Ophthalmol. 2022, 106, 893–901. [Google Scholar] [CrossRef]
- Alrasheed, S.H. A systemic review of barriers to accessing paediatric eye care services in African countries. Afr. Health Sci. 2021, 21, 1887–1897. [Google Scholar] [CrossRef]
- World Health Organization. Vision and Eye Screening Implementation Handbook. Available online: https://www.who.int/publications/i/item/9789240082458 (accessed on 10 January 2024).
- Wilson, S.; Ctori, I.; Suttle, C.; Conway, M.; Shah, R. How accessible is primary eye care for children in England? Ophthalmic Physiol. Opt. 2021, 41, 1021–1033. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.E.; Sussberg, J.A.; Nelson, L.B.; Thuma, T.B.T. Review of the Disparities in Access to Pediatric Eye Care Among Low Socioeconomic Status and Underrepresented Racial Minority Groups Exacerbated by the Economic Downturn in Pediatric Ophthalmology. J. Pediatr. Ophthalmol. Strabismus 2024, 61, 172–178. [Google Scholar] [CrossRef] [PubMed]
- Adugna, M.B.; Nabbouh, F.; Shehata, S.; Ghahari, S. Barriers and facilitators to healthcare access for children with disabilities in low and middle income sub-Saharan African countries: A scoping review. BMC Health Serv. Res. 2020, 20, 15. [Google Scholar] [CrossRef]
- Malik, M.; Strang, N.; Hafeez, A.; Shabbir, M.; Iftikhar, F.; Jonuscheit, S. Barriers to accessing eye care in Pakistan: A mixed methods study. Prim. Health Care Res. Dev. 2025, 26, e58. [Google Scholar] [CrossRef] [PubMed]
- Hutchinson, A.K.; Morse, C.L.; Hercinovic, A.; Cruz, O.A.; Sprunger, D.T.; Repka, M.X.; Lambert, S.R.; Wallace, D.K. American Academy of Ophthalmology Preferred Practice Pattern Pediatric Ophthalmology/Strabismus Panel. Pediatric Eye Evaluations Preferred Practice Pattern. Ophthalmology 2023, 130, P222–P270. [Google Scholar] [CrossRef]
- Zhu, D.; Wang, Y.; Yang, X.; Yang, D.; Guo, K.; Guo, Y.; Jing, X.; Pan, C.W. Pre- and Postcycloplegic Refractions in Children and Adolescents. PLoS ONE 2016, 11, e0167628. [Google Scholar] [CrossRef]
- Rao, P.; Flower, K.B.; Jordan, K.A. Pediatric Vision Screening. Pediatr. Rev. 2024, 45, 726–728. [Google Scholar] [CrossRef]
- Yashadhana, A.; Lee, L.; Serova, N.; Nthete, E.; Burnett, A.M. Access to school-based eye health programs in Central Region, Malawi: A qualitative case study. Health Promot. Int. 2023, 38, daad002. [Google Scholar] [CrossRef]
- Olusanya, B.O.; Smythe, T.; Ogbo, F.A.; Nair, M.K.C.; Scher, M.; Davis, A.C. Global prevalence of developmental disabilities in children and adolescents: A systematic umbrella review. Front. Public Health 2023, 11, 1122009. [Google Scholar] [CrossRef]
- Silveira, J.C.P.; Souza, D.M.; Cardoso, C.S.; Oliveira, M.A.F. Barriers and facilitating strategies for healthcare access and reception for transgender children and adolescents. Rev. Bras. Enferm. 2025, 78 (Suppl. S2), e20240266. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chan, F.; Woodward, M.; Parappilly, M.; Fan, Y.; Tedla, S.; Tamornpark, R.; Anderson, J.; Chomchoei, C.; Kampun, M.; Yeemard, F.; et al. Knowledge acquisition and retention when implementing public health awareness training on common pediatric eye conditions in Thailand. Glob. Health J. 2025, 9, 27–36. [Google Scholar] [CrossRef]
- Aldebasi, Y.H. A descriptive study on compliance of spectacle-wear in children of primary schools at Qassim Province, Saudi Arabia. Int. J. Health Sci. 2013, 7, 291–299. [Google Scholar] [CrossRef]
- Li, T.T.; Fang, Z.S.; Xue, Y.X.; Chen, S.J.; Yang, Y.X.; Li, T.J.; Yang, Y.; Wu, Y. Parental awareness on myopia prevention and control among 350 children. Int. J. Ophthalmol. 2024, 17, 2109–2119. [Google Scholar] [CrossRef] [PubMed]
- Ang, M.; Flanagan, J.L.; Wong, C.W.; Müller, A.; Davis, A.; Keys, D.; Resnikoff, S.; Jong, M.; Wong, T.Y.; Sankaridurg, P. Review: Myopia control strategies recommendations from the 2018 WHO/IAPB/BHVI Meeting on Myopia. Br. J. Ophthalmol. 2020, 104, 1482–1487. [Google Scholar] [CrossRef] [PubMed]
| Profession | Qualification | Male | Female | Total |
|---|---|---|---|---|
| Optometrists | OD/BSc in Optometry | 5 | 3 | 8 |
| MSc in Optometry | 2 | 1 | 3 | |
| PhD in Optometry | 2 | 1 | 3 | |
| Ophthalmologists | Fellowship in Ophthalmology | 4 | 2 | 6 |
| PhD in Ophthalmology | 1 | 1 | 2 | |
| Total | 14 | 8 | 22 | |
| Themes and Related Delphi Statements | Consensus Level (%) | Mean ± SD | Median (IQR) |
|---|---|---|---|
| |||
| Lack of optometrists in primary healthcare centers | 94.29% | 4.73 ± 0.46 | 5 (4–5) |
| Lack of qualified school-based screening programs | 87.14% | 4.36 ± 0.90 | 4 (4–5) |
| Overburdened public healthcare systems | 82.86% | 4.14 ± 0.77 | 4 (4–5) |
| |||
| Availability of cycloplegic eye drops and diagnostic agents | 98.57% | 4.91 ± 0.29 | 5 (5–5) |
| Availability of basic optometry instruments | 90.00% | 4.50 ± 0.91 | 5 (4–5) |
| Availability of vision therapy tools | 82.86% | 4.14 ± 1.04 | 4 (4–5) |
| Availability of low vision aids | 81.43% | 4.09 ± 1.15 | 4 (4–5) |
| |||
| Employing optometrists in primary care settings | 95.71% | 4.77 ± 0.43 | 5 (5–5) |
| Establishing an efficient referral system | 94.29% | 4.73 ± 0.46 | 5 (4–5) |
| Implementing a centralized monitoring system | 94.29% | 4.73 ± 0.55 | 5 (5–5) |
| Mandating school vision screening | 92.86% | 4.64 ± 0.49 | 5 (4–5) |
| Conducting regular vision screenings for the community | 91.43% | 4.59 ± 0.91 | 5 (4–5) |
| |||
| High cost of visual aids | 87.14% | 4.36 ± 0.58 | 4 (4–5) |
| Stigma and social isolation | 82.86% | 4.14 ± 0.56 | 4 (4–4) |
| Uncertainty about where to seek care | 80.00% | 4.00 ± 0.69 | 4 (4–4) |
| |||
| Vision screening at key developmental milestones | 95.71% | 4.77 ± 0.43 | 5 (5–5) |
| Nationwide public awareness campaigns | 94.29% | 4.73 ± 0.55 | 5 (5–5) |
| Recognition of optometrists as primary care providers | 94.29% | 4.73 ± 0.70 | 5 (5–5) |
| Deployment of mobile eye clinics | 92.86% | 4.64 ± 0.49 | 5 (4–5) |
| Establishment of specialized pediatric eye care clinics | 91.43% | 4.59 ± 0.59 | 5 (4–5) |
| |||
| Expanding optometry services in primary health centers | 97.14% | 4.86 ± 0.35 | 5 (5–5) |
| Training more pediatric eye care specialists | 97.14% | 4.86 ± 0.35 | 5 (5–5) |
| Including vision screening in the child health passport | 95.71% | 4.77 ± 0.43 | 5 (5–5) |
| Increasing the number of pediatric eye care clinics | 90.00% | 4.50 ± 0.67 | 5 (4–5) |
| Providing specialized services in rural areas | 90.00% | 4.50 ± 0.67 | 5 (4–5) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alghamdi, M.A.; Almustanyir, A.; Alshuimi, A.A.; Alrasheed, S.H.; Alabdulkader, B.; Alanazi, M.; Altoaimi, B.H.; Bin Dulaym, M.; Alsamnan, L.Y.; Alghamdi, W. Prioritizing Pediatric Eye Care in Saudi Arabia: A National Delphi Consensus Study. Healthcare 2025, 13, 2467. https://doi.org/10.3390/healthcare13192467
Alghamdi MA, Almustanyir A, Alshuimi AA, Alrasheed SH, Alabdulkader B, Alanazi M, Altoaimi BH, Bin Dulaym M, Alsamnan LY, Alghamdi W. Prioritizing Pediatric Eye Care in Saudi Arabia: A National Delphi Consensus Study. Healthcare. 2025; 13(19):2467. https://doi.org/10.3390/healthcare13192467
Chicago/Turabian StyleAlghamdi, Mansour A., Ali Almustanyir, Abdulmalik A. Alshuimi, Saif Hassan Alrasheed, Balsam Alabdulkader, Muteb Alanazi, Basal H. Altoaimi, Mohammad Bin Dulaym, Lama Y. Alsamnan, and Waleed Alghamdi. 2025. "Prioritizing Pediatric Eye Care in Saudi Arabia: A National Delphi Consensus Study" Healthcare 13, no. 19: 2467. https://doi.org/10.3390/healthcare13192467
APA StyleAlghamdi, M. A., Almustanyir, A., Alshuimi, A. A., Alrasheed, S. H., Alabdulkader, B., Alanazi, M., Altoaimi, B. H., Bin Dulaym, M., Alsamnan, L. Y., & Alghamdi, W. (2025). Prioritizing Pediatric Eye Care in Saudi Arabia: A National Delphi Consensus Study. Healthcare, 13(19), 2467. https://doi.org/10.3390/healthcare13192467






