Implementation and Impact of a Patient Blood Management Program in an Urban Community Hospital: An Eight-Year Study
Abstract
1. Introduction
2. Methods
2.1. Hypothesis
2.2. Objective
2.3. Data Inclusion and Exclusion Criteria
- Emergency transfusions with uncrossmatched RBC for trauma or severe bleeding.
- Massive transfusion protocol events.
- Operation room (OR) transfusions.
- Outpatient transfusions.
- Transfusions involving plasma, platelets, or cryoprecipitate.
2.4. Study Outcomes
- 1.
- Mean and median pretransfusion Hgb levels triggering RBC orders.
- 2.
- Total annual RBC transfusion units.
- 3.
- Number of RBC units transfused at Hgb ≥ 7 g/dL (# Hb la7).
- 4.
- Percentage of RBC units transfused at Hgb ≥ 7 g/dL (% Hb la7).
- 5.
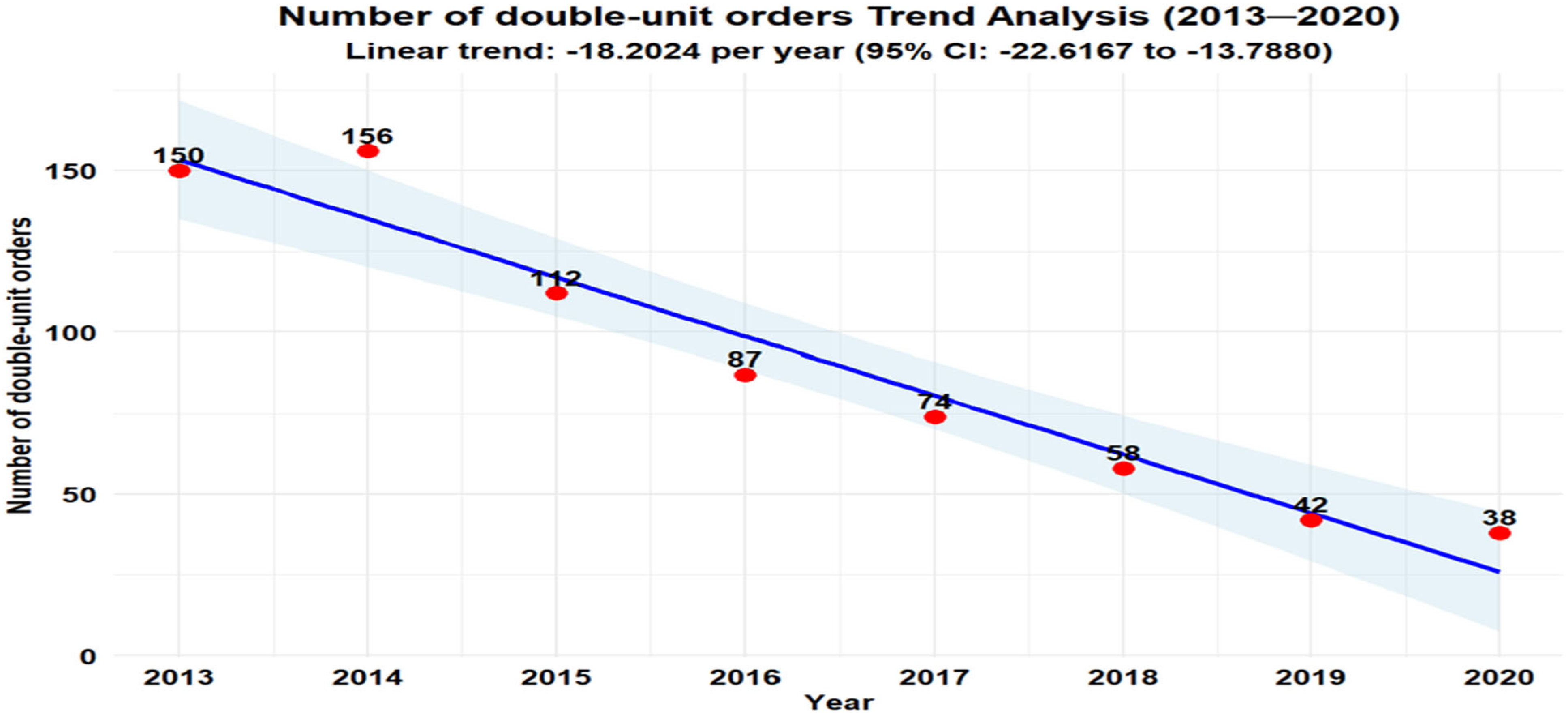
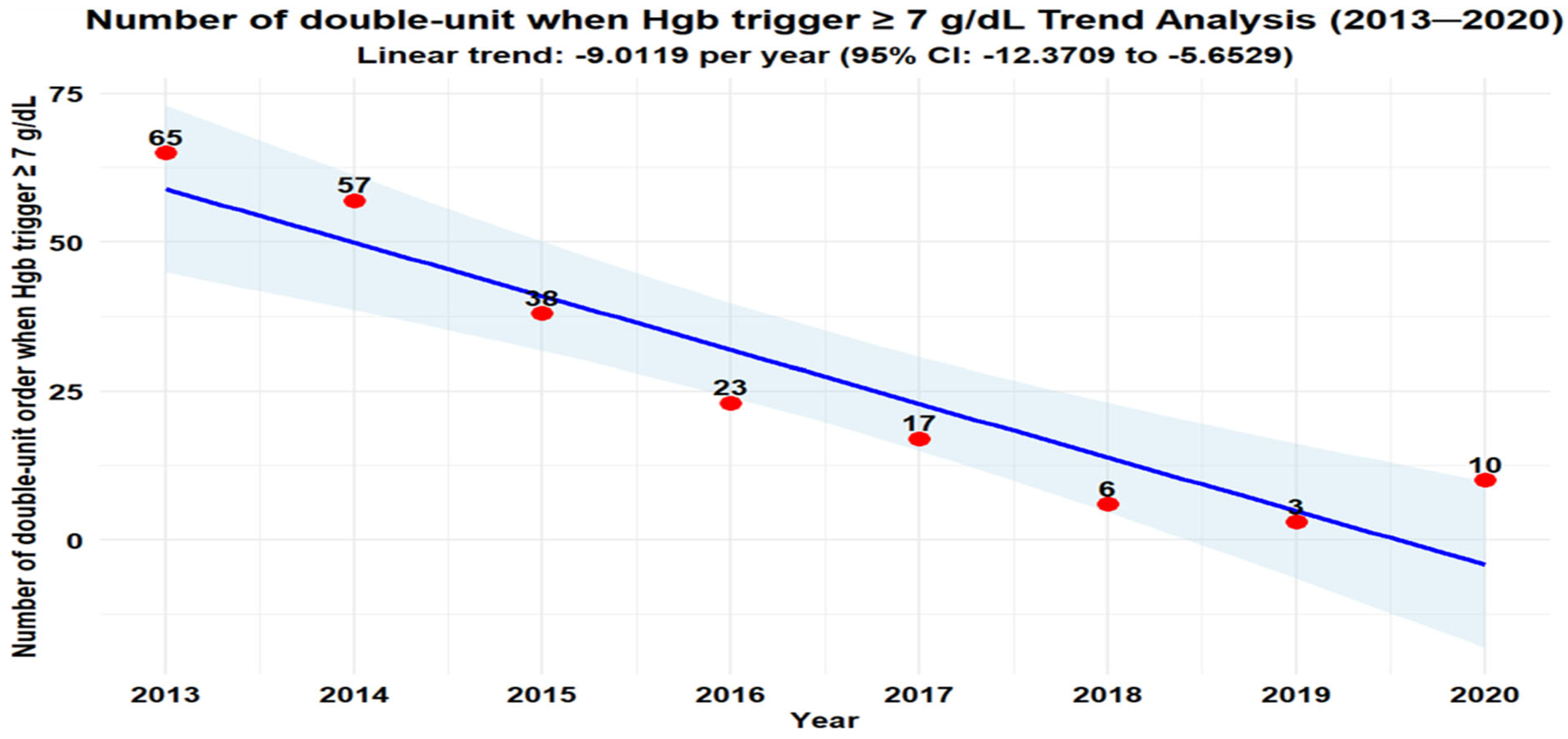
- Number of two-unit RBC orders.
- 6.
- Number and percentage of two-unit RBC orders at Hgb ≥ 7 g/dL.
- 7.
- Overall RBC transfusion rate (units per 1000 patient days, calculated as RBC transfusions ÷ (total discharges × average length of stay [LOS]).
- 8.
- Inpatient LOS (mean and median).
- 9.
- Cost savings from reduced unnecessary transfusions, estimated as
2.5. Statistical Analysis
2.6. Cost Sensitivity Analysis
3. Results
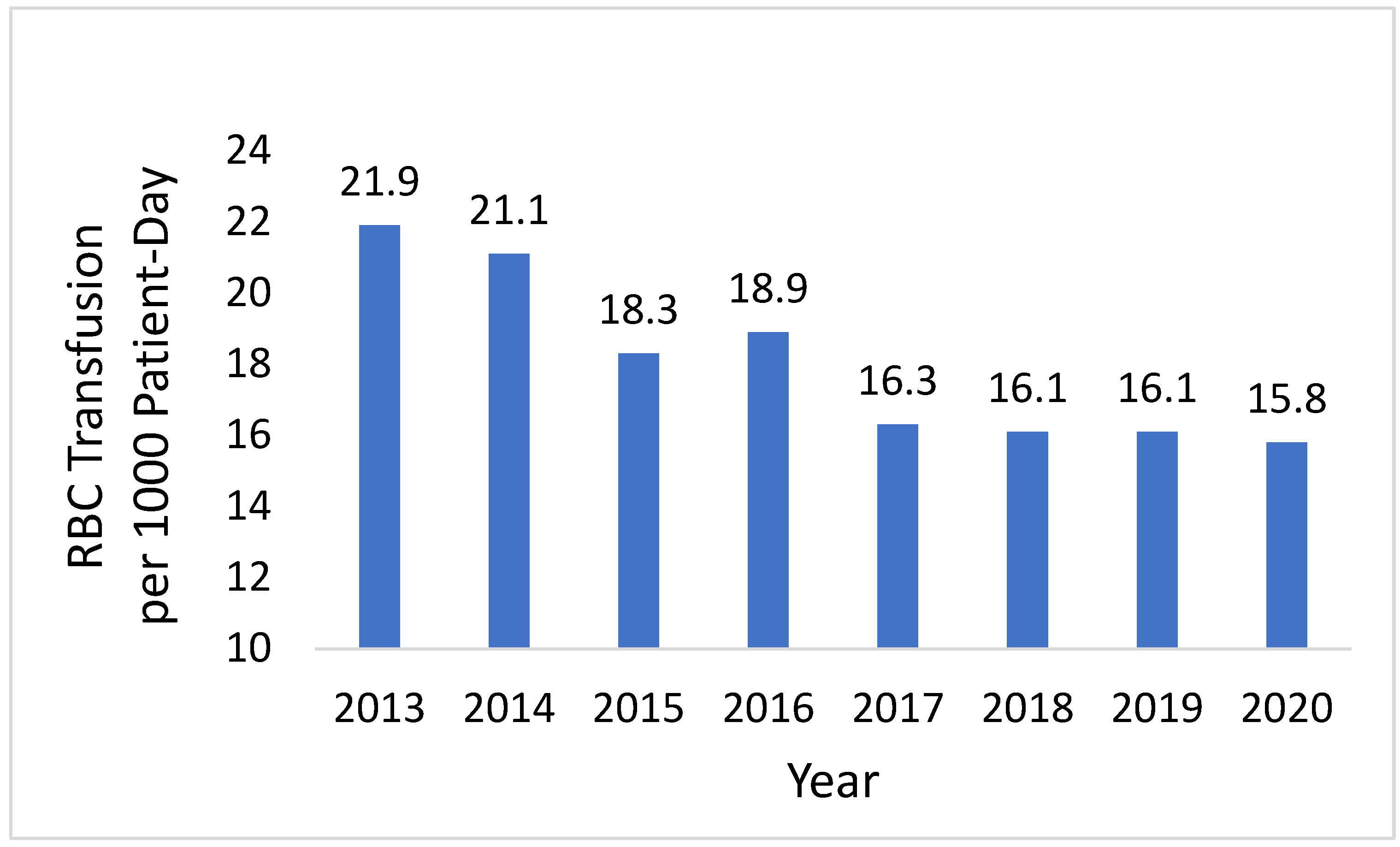
- Transfusion Rate: The annual inpatient overall RBC transfusion rate per 1000 patient days declined from 21.9 in 2013 to 15.8 in 2020 (Figure 4).
- ○
- All-item CPI adjustment → cumulative avoided transfusion cost over 2013–2020 ranges from USD 1.70 million (low bound) to USD 3.86 million (high bound).
- ○
- Medical-care CPI adjustment → cumulative avoided cost over 2013–2020 ranges from USD 1.86 million (low bound) to USD 4.21 million (high bound).
4. Discussion
4.1. Broader Implications and Future Directions
4.2. Challenges and Limitations
4.3. Cost Estimate
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Shander, A.; Lobel, G.P.; Javidroozi, M. Anesthesia for Patients with Anemia. Anesth. Clin. 2016, 34, 711–730. [Google Scholar] [CrossRef] [PubMed]
- Chau, M.; Cohil, D.; Schofield, N.; Abevsiri, S.; Klein, A.; Richards, T. Development and feasibility of a Patient Blood Management implementation programme in vascular surgery. Vasc. Med. 2020, 25, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Warner, M.A.; Schaefer, K.K.; Madde, N.; Burt, J.M.; Higgins, A.A.; Kor, D.J. Improvements in red blood cell transfusion utilization following implementation of a single-unit default for electronic ordering. Transfusion 2019, 59, 2218–2222. [Google Scholar] [CrossRef] [PubMed]
- Shander, A.; Hofmann, A.; Ozawa, S.; Theusinger, O.M.; Gombotz, H.; Spahn, D.R. Activity-based costs of blood transfusions in surgical patients at four hospitals. Transfusion 2010, 50, 753–765. [Google Scholar] [CrossRef] [PubMed]
- Abraham, I.; Sun, D. The cost of blood transfusion in Western Europe as estimated from six studies. Transfusion 2012, 52, 1983–1988. [Google Scholar] [CrossRef] [PubMed]
- CPI (All Items) Monthly Historical Table (Includes Jul 2010 → Jul 2020 Values)—U.S. BLS Historical CPI Table. Bureau of Labor Statistics. Available online: https://www.bls.gov/cpi/tables/supplemental-files/historical-cpi-u-202401.pdf (accessed on 22 August 2025).
- Medical-Care CPI (CPIMEDNS) Monthly Series—FRED (Data Table with Monthly Values). FRED. Available online: https://fred.stlouisfed.org/data/CPIMEDNS (accessed on 22 August 2025).
- Shander, A. Transfusion Overuse Exposing an International Problem and Patient Safety Issue. Available online: https://www.sabm.org/assets/pdfs/SABM-Transfusion-Overuse-2019.pdf (accessed on 24 August 2025).
- Jenkins, I.; Doucet, J.J.; Clay, B.; Kopko, P.; Fipps, D.; Hemmen, E.; Paulson, D. Transfusing Wisely: Clinical Decision Support Improves Blood Transfusion Practices. Jt. Comm. J. Qual. Patient Saf. 2017, 43, 389–395. [Google Scholar] [CrossRef] [PubMed]
- Warner, M.A.; Schulte, P.J.; Hanson, A.C.; Madde, N.R.; Burt, J.M.; Higgins, A.A.; Andrijasevic, N.M.; Kreuter, J.D.; Jacob, E.K.; Stubbs, J.R.; et al. Implementation of a Comprehensive Patient Blood Management Program for Hospitalized Patients at a Large United States Medical Center. Mayo Clin. Proc. 2021, 96, 2980–2990. [Google Scholar] [CrossRef] [PubMed]
- Wu, D.W.; Friedman, M.T.; Lombardi, D.P.; Hwang, R.; Sender, J.; Cobaj, V.; Niazi, M.; Li, Y.; Karpinos, R. Impact of Patient Blood Management on Red Blood Cell Utilization in an Urban Community Teaching Hospital: A Seven-Year Retrospective Study. Life 2024, 14, 232. [Google Scholar] [CrossRef] [PubMed]
- Podlasek, S.J.; Thakkar, R.N.; Rotello, L.C.; Fleury, T.A.; Demski, R.J.; Ness, P.M.; Frank, S.M.; Thakkar, R.D. Implementing a “Why give 2 when 1 will do?” Choosing Wisely campaign. Transfusion 2016, 56, 2164. [Google Scholar] [CrossRef] [PubMed]
- Fischer, D.P.; Zacharowski, K.D.; Müller, M.M.; Geisen, C.; Seifried, E.; Müller, H.; Meybohm, P. Patient blood management implementation strategies and their effect on physicians’ risk perception, clinical knowledge and perioperative practice—The frankfurt experience. Transfus. Med. Hemother. 2015, 42, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, A.; Spahn, D.R.; Holtorf, A.P. Making patient blood management the new norm(al) as experienced by implementors in diverse countries. BMC Health Serv. Res. 2021, 21, 634. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guidance on Implementing Patient Blood Management to Improve Global Blood Health Status. World Health Organization. 2025. Available online: https://iris.who.int/bitstream/handle/10665/380784/9789240104662-eng.pdf?sequence= (accessed on 19 August 2025).
- Leahy, M.F.; Hofmann, A.; Towler, S.; Trentino, K.M.; Burrows, S.A.; Swain, S.G.; Hamdorf, J.; Gallagher, T.; Koay, A.; Geelhoed, G.C.; et al. Improved outcomes and reduced costs associated with a health-system-wide patient blood management program: A retrospective observational study in four major adult tertiary-care hospitals. Transfusion 2017, 57, 1347–1358. [Google Scholar] [CrossRef] [PubMed]
- Froessler, B.; Palm, P.; Weber, I.; Hodyl, N.A.; Singh, R.; Murphy, E.M. The Important Role for Intravenous Iron in Perioperative Patient Blood Management in Major Abdominal Surgery: A Randomized Controlled Trial. Ann. Surg. 2016, 264, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Goodnough, L.T.; Hollenhorst, M.A. Clinical decision support and improved blood use in patient blood management. Hematol. Am. Soc. Hematol. Educ. Program 2019, 2019, 577–582. [Google Scholar] [CrossRef] [PubMed]

| Year | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | Total |
|---|---|---|---|---|---|---|---|---|---|
| (1) Number of transfused RBC units | 2061 | 1762 * | 1460 * | 1514 * | 1251 * | 1286 * | 1350 * | 1884 | N/A |
| (2) Number of RBC units transfused when Hgb trigger ≥ 7 g/dL | 1210 | 830 * | 572 * | 517 * | 371 * | 357 * | 310 * | 377 * | N/A |
| (3) % of RBC units transfused when Hgb trigger ≥ 7 g/dL = (2) ÷ (1) | 58.7 | 47.1 | 39.2 | 34.1 | 30.0 | 27.8 | 23.0 | 20.0 | N/A |
| (4) Potential reduction in RBC units = ((3) of year 2013 − (3) of this year) × (1) of the year) ** | N/A | 204 | 285 | 372 | 375 | 398 | 482 | 729 | 2844 |
| (5) Potential cost saving (USD) = (4) × USD 760 per unit | N/A | 155 K | 217 K | 283 K | 285 K | 302 K | 366 K | 554 K | USD 2.2 million |
| LOS (Days) | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 |
|---|---|---|---|---|---|---|---|---|
| Mean (Days) | 5.1 | 4.9 | 5.5 | 5.5 | 5.2 | 5.3 | 5.5 | 5.4 |
| Median (Days) | 3.0 | 3.0 | 3.0 | 3.0 | 3.0 | 3.0 | 3.0 | 3.0 |
| Author/Study | Focus/Topic | Methodology | Key Findings | Limitations |
|---|---|---|---|---|
| Fischer et al. (2015) [13] | PBM education and behavioral change | Observational study (within 2 years) | Shift toward physiological transfusion triggers | Physician perception-based; limited outcome data |
| Froessler et al. (2016) [17] | Preoperative IV iron therapy | Randomized controlled trial (over 3+ years) | Reduced transfusions (61%), improved recovery, shorter stays, cost saving | Specific to surgical patients; not generalizable to all PBM contexts |
| Jenkins et al. (2017) [9] | Clinical decision support for transfusions | Quality improvement study | Significant reduction in double-unit orders | Limited to one institution; no long-term follow-up |
| Leahy et al. (2017) [16] | System-wide PBM in Australia, involving over 600,000 patients | A 6-year retrospective study across 4 tertiary-care hospitals | Reduced transfusions (41%), mortality, infections, LOS, and product costs | Large-scale system; may not reflect smaller hospital settings |
| Goodnough & Hollenhorst (2019) [18] | Smart alerts in CPOE for PBM | An 11-year study for the impact of PBM CDS | 42% reduction in RBC use | Requires advanced EHR systems; scalability concerns |
| Warner et al. (2019) [10] | Single-unit default in electronic ordering | An 8-year observational study at a medical center | 33% reduction in RBC transfusions | Focused on academic center; may not generalize to smaller hospitals |
| Wu et al. (2024) [11] | PBM in a community hospital, without allocation of budgetary support | A 7-year retrospective study | 35.7% reduction in unnecessary RBC transfusions; cost savings; no harm to patients | Retrospective design; no patient-level COVID data; limited generalizability |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karpinos, R.; Friedman, M.; Lombardi, D.; Li, Y.; Cobaj, V.; Niazi, M.; Lai, P.; Wu, D.W. Implementation and Impact of a Patient Blood Management Program in an Urban Community Hospital: An Eight-Year Study. Healthcare 2025, 13, 2462. https://doi.org/10.3390/healthcare13192462
Karpinos R, Friedman M, Lombardi D, Li Y, Cobaj V, Niazi M, Lai P, Wu DW. Implementation and Impact of a Patient Blood Management Program in an Urban Community Hospital: An Eight-Year Study. Healthcare. 2025; 13(19):2462. https://doi.org/10.3390/healthcare13192462
Chicago/Turabian StyleKarpinos, Robert, Mark Friedman, Daniel Lombardi, Yahhua Li, Valdet Cobaj, Masooma Niazi, Phi Lai, and Ding Wen Wu. 2025. "Implementation and Impact of a Patient Blood Management Program in an Urban Community Hospital: An Eight-Year Study" Healthcare 13, no. 19: 2462. https://doi.org/10.3390/healthcare13192462
APA StyleKarpinos, R., Friedman, M., Lombardi, D., Li, Y., Cobaj, V., Niazi, M., Lai, P., & Wu, D. W. (2025). Implementation and Impact of a Patient Blood Management Program in an Urban Community Hospital: An Eight-Year Study. Healthcare, 13(19), 2462. https://doi.org/10.3390/healthcare13192462






