Mindfulness Improves Awareness and Cortisol Levels During COVID-19 Lockdown: A Randomised Controlled Trial in Healthcare Workers
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Procedure
2.2. Description of the MBSR Intervention
2.3. Physiological Evaluation
2.4. Psychological Evaluation
2.5. Qualitative Observations
2.6. Statistical Data Analysis
3. Results
3.1. Sample Characteristics
3.2. Baseline Homogeneity Between the Two Groups
3.3. Repeated-Measures ANOVA
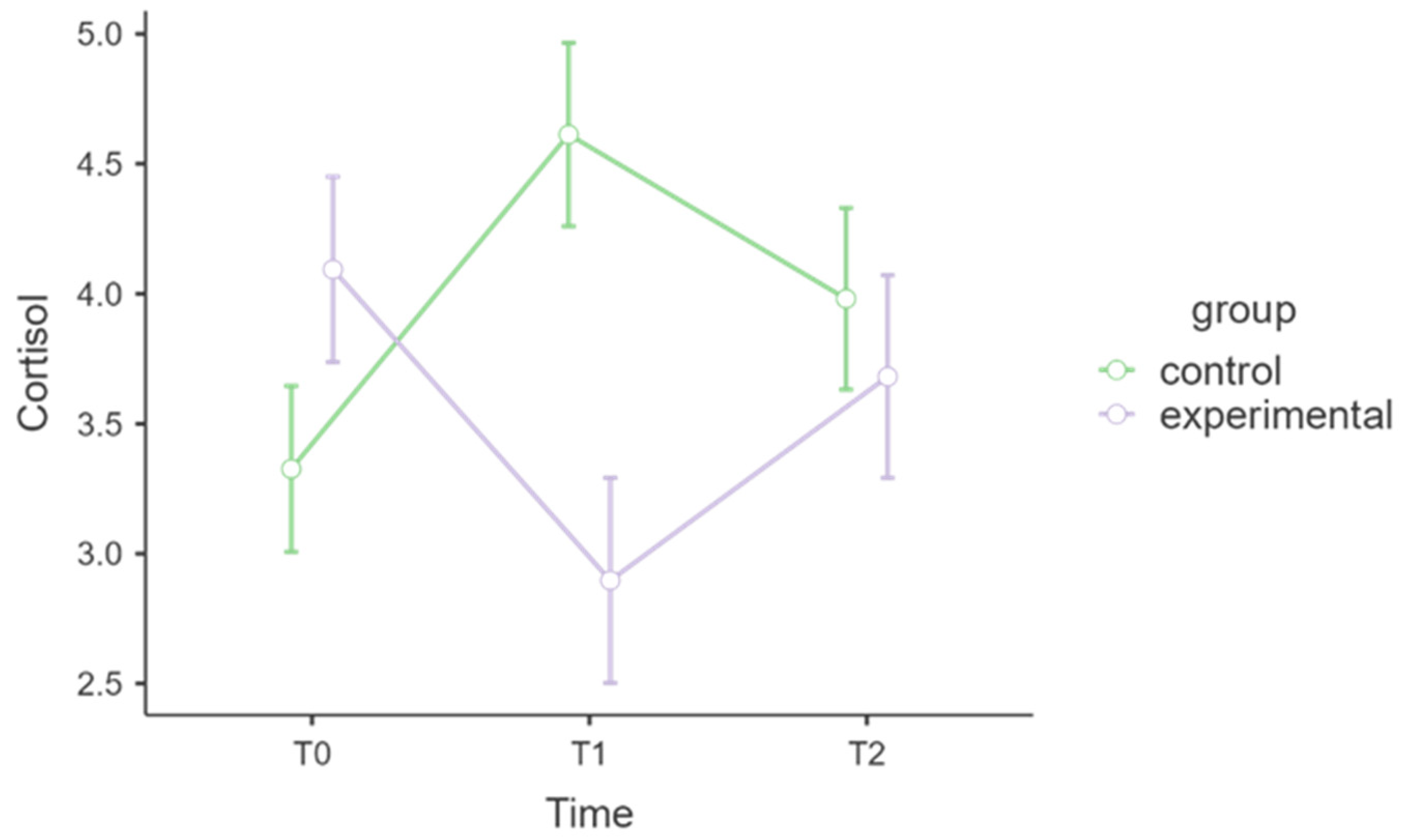
3.3.1. Cortisol Outcome
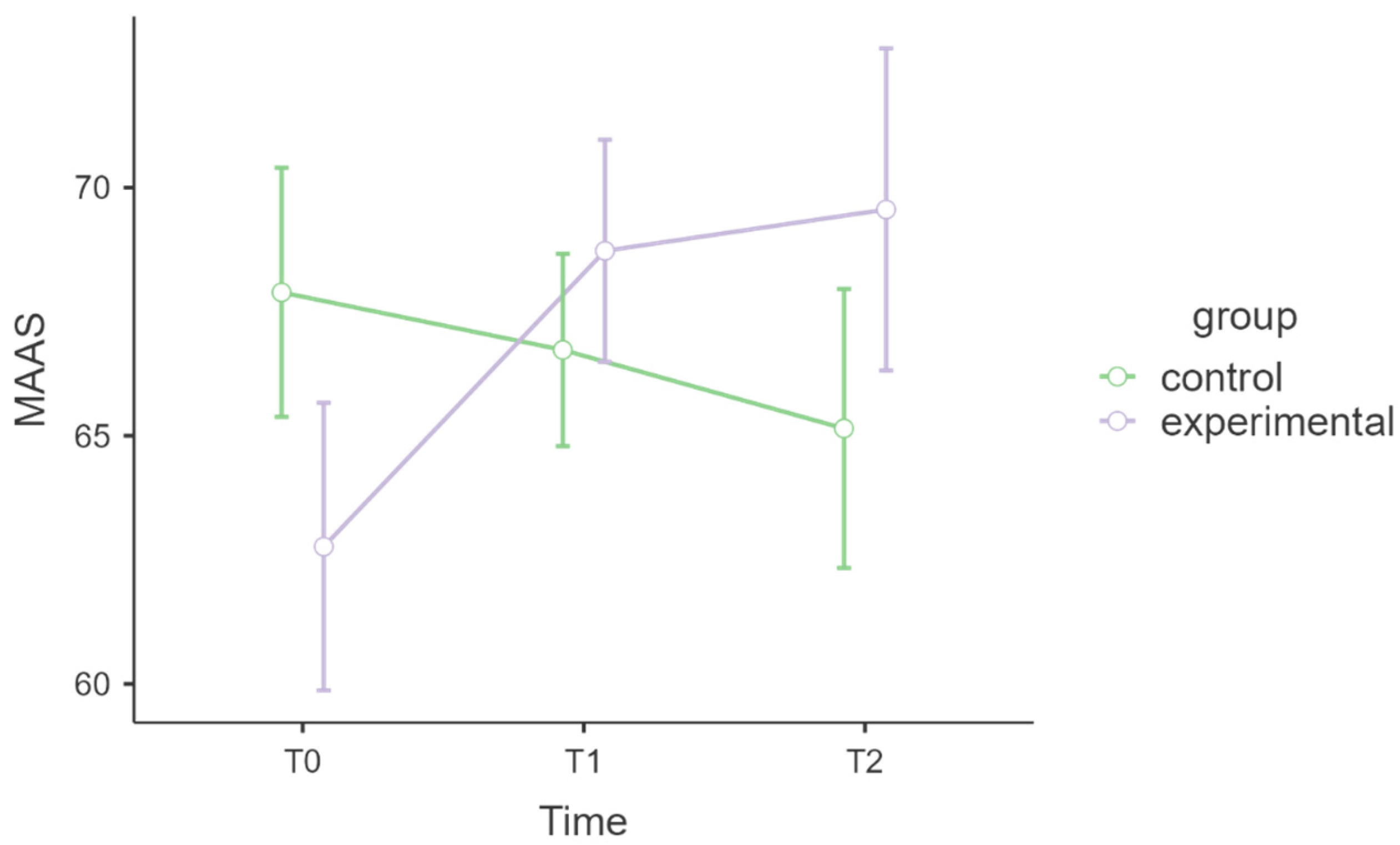
3.3.2. MAAS, Attention, and Awareness
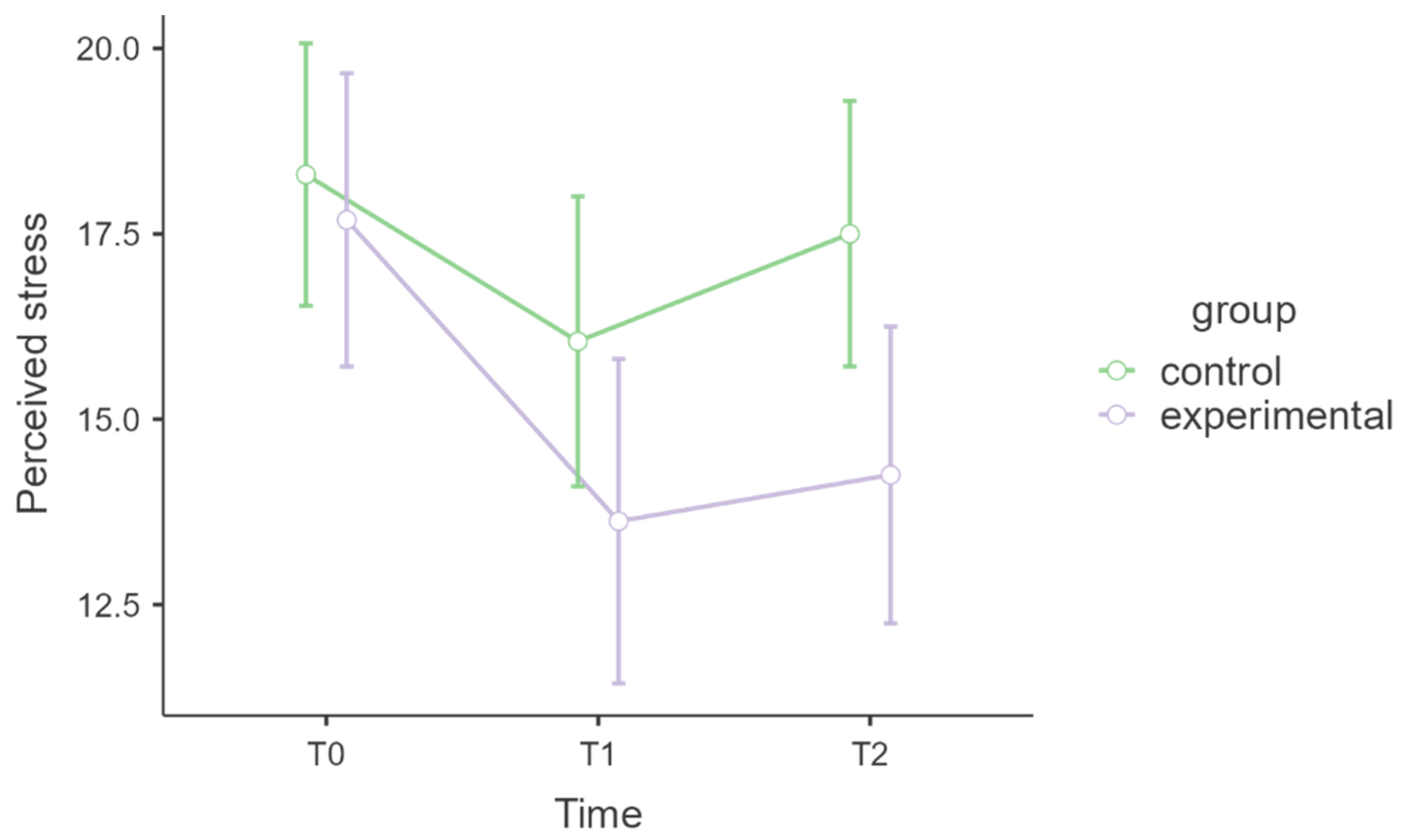
3.3.3. Perceived Stress Levels
3.3.4. IANUS, Job Strain
3.3.5. IANUS Emotional Fatigue
3.4. Qualitative Observations Results
4. Discussions
4.1. Limitations and Future Research
4.2. Strengths of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Btatement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Du, M.; Hu, K. Frontline Health Care Workers’ Mental Workload During the COVID-19 Pandemic: A Cross-Sectional Study. Asia Pac. J. Public Health 2021, 33, 303–305. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Aguilar, C.; Casado-Aranda, L.-A.; Farrés Fernández, M.; Minué Lorenzo, S. Has COVID-19 Changed the Workload for Primary Care Physicians? The Case of Spain. Fam. Pract. 2021, 38, cmab028. [Google Scholar] [CrossRef]
- Hoogendoorn, M.E.; Brinkman, S.; Bosman, R.J.; Haringman, J.; De Keizer, N.F.; Spijkstra, J.J. The Impact of COVID-19 on Nursing Workload and Planning of Nursing Staff on the Intensive Care: A Prospective Descriptive Multicenter Study. Int. J. Nurs. Stud. 2021, 121, 104005. [Google Scholar] [CrossRef]
- Barello, S.; Palamenghi, L.; Graffigna, G. Burnout and Somatic Symptoms among Frontline Healthcare Professionals at the Peak of the Italian COVID-19 Pandemic. Psychiatry Res. 2020, 290, 113129. [Google Scholar] [CrossRef]
- Nadeem, F.; Sadiq, A.; Raziq, A.; Iqbal, Q.; Haider, S.; Saleem, F.; Bashaar, M. Depression, Anxiety, and Stress Among Nurses During the COVID-19 Wave III: Results of a Cross-Sectional Assessment. J. Multidiscip. Healthc. 2021, 14, 3093–3101. [Google Scholar] [CrossRef] [PubMed]
- Wahlster, S.; Sharma, M.; Lewis, A.K.; Patel, P.V.; Hartog, C.S.; Jannotta, G.; Blissitt, P.; Kross, E.K.; Kassebaum, N.J.; Greer, D.M.; et al. The Coronavirus Disease 2019 Pandemic’s Effect on Critical Care Resources and Health-Care Providers. Chest 2021, 159, 619–633. [Google Scholar] [CrossRef]
- Morgantini, L.A.; Naha, U.; Wang, H.; Francavilla, S.; Acar, Ö.; Flores, J.M.; Crivellaro, S.; Moreira, D.; Abern, M.; Eklund, M.; et al. Factors Contributing to Healthcare Professional Burnout during the COVID-19 Pandemic: A Rapid Turnaround Global Survey. PLoS ONE 2020, 15, e0238217. [Google Scholar] [CrossRef]
- Conti, C.; Fontanesi, L.; Lanzara, R.; Rosa, I.; Doyle, R.L.; Porcelli, P. Burnout Status of Italian Healthcare Workers during the First COVID-19 Pandemic Peak Period. Healthcare 2021, 9, 510. [Google Scholar] [CrossRef] [PubMed]
- Rossi, A.A.; Panzeri, A.; Fernandez, I.; Invernizzi, R.; Taccini, F.; Mannarini, S. The Impact of Trauma Core Dimensions on Anxiety and Depression: A Latent Regression Model through the Post-Traumatic Symptom Questionnaire (PTSQ). Sci. Rep. 2024, 14, 23036. [Google Scholar] [CrossRef]
- Contreras, A.; Butter, S.; Granziol, U.; Panzeri, A.; Peinado, V.; Trucharte, A.; Zavlis, O.; Valiente, C.; Vázquez, C.; Murphy, J.; et al. The Network Structure of Psychopathological and Resilient Responses to the Pandemic: A Multicountry General Population Study of Depression and Anxiety. J. Trauma. Stress 2024, 37, 126–140. [Google Scholar] [CrossRef]
- Finstad, G.L.; Giorgi, G.; Lulli, L.G.; Pandolfi, C.; Foti, G.; León-Perez, J.M.; Cantero-Sánchez, F.J.; Mucci, N. Resilience, Coping Strategies and Posttraumatic Growth in the Workplace Following COVID-19: A Narrative Review on the Positive Aspects of Trauma. Int. J. Environ. Res. Public Health 2021, 18, 9453. [Google Scholar] [CrossRef]
- Dragioti, E.; Tsartsalis, D.; Mentis, M.; Mantzoukas, S.; Gouva, M. Impact of the COVID-19 Pandemic on the Mental Health of Hospital Staff: An Umbrella Review of 44 Meta-Analyses. Int. J. Nurs. Stud. 2022, 131, 104272. [Google Scholar] [CrossRef]
- Vacca, A.; Minò, M.V.; Longo, R.; Lucisani, G.; Solomita, B.; Franza, F. The Emotional Impact on Mental Health Workers in the Care of Patients with Mental Disorders in the Pandemic and Post COVID-19 Pandemic: A Measure of “Burnout” and “Compassion Fatigue”. Psychiatr. Danub. 2023, 35, 292–295. [Google Scholar] [PubMed]
- Minò, M.; Vacca, A.; Longo, R.; Lucisani, G.; Solomita, B.; Franza, F. Stress Work and Hopelessness in Mental Health Workers/Caregivers: An Observational Study in Pandemic and Post COVID-19 Pandemic. Psychiatr. Danub. 2023, 35, 266–270. [Google Scholar] [PubMed]
- Bennett, K.M.; Panzeri, A.; Derrer-Merk, E.; Butter, S.; Hartman, T.K.; Mason, L.; McBride, O.; Murphy, J.; Shevlin, M.; Gibson-Miller, J.; et al. Predicting Resilience during the COVID-19 Pandemic in the United Kingdom: Cross-Sectional and Longitudinal Results. PLoS ONE 2023, 18, e0283254. [Google Scholar] [CrossRef] [PubMed]
- Gourret Baumgart, J.; Kane, H.; El-Hage, W.; Deloyer, J.; Maes, C.; Lebas, M.-C.; Marazziti, D.; Thome, J.; Fond-Harmant, L.; Denis, F. The Early Impacts of the COVID-19 Pandemic on Mental Health Facilities and Psychiatric Professionals. Int. J. Environ. Res. Public. Health 2021, 18, 8034. [Google Scholar] [CrossRef]
- Rossi, A.A.; Panzeri, A.; Taccini, F.; Parola, A.; Mannarini, S. The Rising of the Shield Hero. Development of the Post-Traumatic Symptom Questionnaire (PTSQ) and Assessment of the Protective Effect of Self-Esteem from Trauma-Related Anxiety and Depression. J. Child Adolesc. Trauma 2024, 17, 83–101. [Google Scholar] [CrossRef]
- Minò, M.; Vacca, A.; Colizzi, I.; Solomita, B.; Franza, F.; Tavormina, G. The Effect of the Pandemic on the Care of Patients with Mental Disorders: Measure of “Compassion Fatigue” and “Burn-Out” in the Operator. Psychiatr. Danub. 2021, 33, 114–118. [Google Scholar]
- Viswanathan, R.; Myers, M.F.; Fanous, A.H. Support Groups and Individual Mental Health Care via Video Conferencing for Frontline Clinicians During the COVID-19 Pandemic. Psychosomatics 2020, 61, 538–543. [Google Scholar] [CrossRef]
- Panzeri, A.; Rossi Ferrario, S.; Cerutti, P. Psychological Differences Among Healthcare Workers of a Rehabilitation Institute During the COVID-19 Pandemic: A Two-Step Study. Front. Psychol. 2021, 12, 636129. [Google Scholar] [CrossRef]
- Matiz, A.; Fabbro, F.; Paschetto, A.; Cantone, D.; Paolone, A.R.; Crescentini, C. Positive Impact of Mindfulness Meditation on Mental Health of Female Teachers during the COVID-19 Outbreak in Italy. Int. J. Environ. Res. Public Health 2020, 17, 6450. [Google Scholar] [CrossRef] [PubMed]
- Marotta, M.; Gorini, F.; Parlanti, A.; Berti, S.; Vassalle, C. Effect of Mindfulness-Based Stress Reduction on the Well-Being, Burnout and Stress of Italian Healthcare Professionals during the COVID-19 Pandemic. J. Clin. Med. 2022, 11, 3136. [Google Scholar] [CrossRef] [PubMed]
- Wexler, T.M.; Schellinger, J. Mindfulness-Based Stress Reduction for Nurses: An Integrative Review. J. Holist. Nurs. 2023, 41, 40–59. [Google Scholar] [CrossRef] [PubMed]
- Kabat-Zinn, J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness; Delta Trade Paperback/Bantam Dell: New York, NY, USA, 2005; p. 504. ISBN 978-0-385-30312-5. [Google Scholar]
- Grossman, P.; Niemann, L.; Schmidt, S.; Walach, H. Mindfulness-Based Stress Reduction and Health Benefits. J. Psychosom. Res. 2004, 57, 35–43. [Google Scholar] [CrossRef]
- Rossi, A.A.; Pizzoli, S.F.M.; Fernandez, I.; Invernizzi, R.; Panzeri, A.; Taccini, F.; Mannarini, S. The Shield of Self-Esteem: Buffering against the Impact of Traumatic Experiences, Fear, Anxiety, and Depression. Behav. Sci. 2024, 14, 901. [Google Scholar] [CrossRef]
- Liu, X.; Xu, Y.; Xu, H.; Jiang, L.; Wang, T.; Chen, C.; Lee, A.; Zhu, P. Anxiety and Sleep Quality among Front-Line Nurses Treating First Wave COVID-19 in China: The Mediating Role of Mindfulness. Arch. Psychiatr. Nurs. 2022, 41, 341–347. [Google Scholar] [CrossRef]
- Bossi, F.; Zaninotto, F.; D’Arcangelo, S.; Lattanzi, N.; Malizia, A.P.; Ricciardi, E. Mindfulness-Based Online Intervention Increases Well-Being and Decreases Stress after Covid-19 Lockdown. Sci. Rep. 2022, 12, 6483. [Google Scholar] [CrossRef]
- Fazia, T.; Bubbico, F.; Nova, A.; Riggi, E.; Caimi, G.; Calgan, B.; Salvato, G.; Bruno, S.; Bottini, G.; Bernardinelli, L. Online Short-Term Mindfulness-Based Intervention During COVID-19 Quarantine in Italy: Effects on Wellbeing, Stress, and Anxiety. Front. Psychol. 2022, 13, 914183. [Google Scholar] [CrossRef]
- Perez, S.G.; Nuccio, A.G.; Stripling, A.M. A Rapid Review of the Detrimental Impact of Loneliness and Social Isolation in Caregivers of Older Adults. Am. J. Geriatr. Psychiatry 2021, 29, S122–S123. [Google Scholar] [CrossRef]
- Gardi, C.; Fazia, T.; Stringa, B.; Giommi, F. A Short Mindfulness Retreat Can Improve Biological Markers of Stress and Inflammation. Psychoneuroendocrinology 2022, 135, 105579. [Google Scholar] [CrossRef]
- Lengacher, C.A.; Reich, R.R.; Paterson, C.L.; Shelton, M.; Shivers, S.; Ramesar, S.; Pleasant, M.L.; Budhrani-Shani, P.; Groer, M.; Post-White, J.; et al. A Large Randomized Trial: Effects of Mindfulness-Based Stress Reduction (MBSR) for Breast Cancer (BC) Survivors on Salivary Cortisol and IL-6. Biol. Res. Nurs. 2019, 21, 39–49. [Google Scholar] [CrossRef]
- Jones, C.; Gwenin, C. Cortisol Level Dysregulation and Its Prevalence—Is It Nature’s Alarm Clock? Physiol. Rep. 2021, 8, e14644. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, D.B.; Thayer, J.F.; Vedhara, K. Stress and Health: A Review of Psychobiological Processes. Annu. Rev. Psychol. 2021, 72, 663–688. [Google Scholar] [CrossRef]
- Raggi, P.; Quyyumi, A.A.; Henein, M.Y.; Vaccarino, V. Psychosocial Stress and Cardiovascular Disease. Am. J. Prev. Cardiol. 2025, 22, 100968. [Google Scholar] [CrossRef] [PubMed]
- Villalba, D.K.; Lindsay, E.K.; Marsland, A.L.; Greco, C.M.; Young, S.; Brown, K.W.; Smyth, J.M.; Walsh, C.P.; Gray, K.; Chin, B.; et al. Mindfulness Training and Systemic Low-Grade Inflammation in Stressed Community Adults: Evidence from Two Randomized Controlled Trials. PLoS ONE 2019, 14, e0219120. [Google Scholar] [CrossRef]
- Panzeri, A.; Bottesi, G.; Ghisi, M.; Scalavicci, C.; Spoto, A.; Vidotto, G. Emotional Regulation, Coping, and Resilience in Informal Caregivers: A Network Analysis Approach. Behav. Sci. 2024, 14, 709. [Google Scholar] [CrossRef] [PubMed]
- Lau, J.; Koh, W.-L.; Ng, J.S.; Khoo, A.M.-G.; Tan, K.-K. Understanding the Mental Health Impact of COVID-19 in the Elderly General Population: A Scoping Review of Global Literature from the First Year of the Pandemic. Psychiatry Res. 2023, 329, 115516. [Google Scholar] [CrossRef]
- Santarnecchi, E.; D’Arista, S.; Egiziano, E.; Gardi, C.; Petrosino, R.; Vatti, G.; Reda, M.; Rossi, A. Interaction between Neuroanatomical and Psychological Changes after Mindfulness-Based Training. PLoS ONE 2014, 9, e108359. [Google Scholar] [CrossRef]
- Sezer, I.; Pizzagalli, D.A.; Sacchet, M.D. Resting-State fMRI Functional Connectivity and Mindfulness in Clinical and Non-Clinical Contexts: A Review and Synthesis. Neurosci. Biobehav. Rev. 2022, 135, 104583. [Google Scholar] [CrossRef]
- Random Number Generator. Available online: https://stattrek.com/statistics/random-number-generator (accessed on 18 September 2025).
- Cohen, S.; Kamarck, T.; Mermelstein, R. A Global Measure of Perceived Stress. J. Health Soc. Behav. 1983, 24, 385. [Google Scholar] [CrossRef]
- Majani, G.; Di Tano, G.; Giardini, A.; De Maria, R.; Russo, G.; Maestri, R.; Marini, M.; Milli, M.; Aspromonte, N. Prevalence of Job-Related Distress and Satisfaction in a Nationwide Cardiology Setting: The IANUS—itAliaN Cardiologists’ Undetected Distress Study. J. Cardiovasc. Med. 2016, 17, 587–594. [Google Scholar] [CrossRef]
- Brown, K.W.; Ryan, R.M. The Benefits of Being Present: Mindfulness and Its Role in Psychological Well-Being. J. Pers. Soc. Psychol. 2003, 84, 822–848. [Google Scholar] [CrossRef] [PubMed]
- Kriakous, S.A.; Elliott, K.A.; Lamers, C.; Owen, R. The Effectiveness of Mindfulness-Based Stress Reduction on the Psychological Functioning of Healthcare Professionals: A Systematic Review. Mindfulness 2021, 12, 1–28. [Google Scholar] [CrossRef]
- Pan, D.; Jentsch, V.L.; Langer, K.; Hagedorn, B.; Höffken, O.; Wolf, O.T.; Merz, C.J. What a Difference Timing Makes: Cortisol Effects on Neural Underpinnings of Emotion Regulation. Neurobiol. Stress 2023, 25, 100544. [Google Scholar] [CrossRef] [PubMed]
- Calderone, A.; Latella, D.; Impellizzeri, F.; De Pasquale, P.; Famà, F.; Quartarone, A.; Calabrò, R.S. Neurobiological Changes Induced by Mindfulness and Meditation: A Systematic Review. Biomedicines 2024, 12, 2613. [Google Scholar] [CrossRef]
- Gotink, R.A.; Meijboom, R.; Vernooij, M.W.; Smits, M.; Hunink, M.G.M. 8-Week Mindfulness Based Stress Reduction Induces Brain Changes Similar to Traditional Long-Term Meditation Practice—A Systematic Review. Brain Cogn. 2016, 108, 32–41. [Google Scholar] [CrossRef] [PubMed]
- Koncz, A.; Demetrovics, Z.; Takacs, Z.K. Meditation Interventions Efficiently Reduce Cortisol Levels of At-Risk Samples: A Meta-Analysis. Health Psychol. Rev. 2021, 15, 56–84. [Google Scholar] [CrossRef]
- Bränström, R.; Kvillemo, P.; Åkerstedt, T. Effects of Mindfulness Training on Levels of Cortisol in Cancer Patients. Psychosomatics 2013, 54, 158–164. [Google Scholar] [CrossRef] [PubMed]
- Yavuz Sercekman, M. Exploring the Sustained Impact of the Mindfulness-Based Stress Reduction Program: A Thematic Analysis. Front. Psychol. 2024, 15, 1347336. [Google Scholar] [CrossRef]
- Finistrella, M.; Luchina, E. The effect of a Mindfulness-based stress reduction program on the mental health of a sample of Italian healthcare professionals: A quasi-experimental study design. Ital. J. Psychol. Occup. Health 2024, 4, 27–40. [Google Scholar] [CrossRef]
- Aghamohammadi, F.; Saed, O.; Ahmadi, R.; Kharaghani, R. The Effectiveness of Adapted Group Mindfulness-Based Stress Management Program on Perceived Stress and Emotion Regulation in Midwives: A Randomized Clinical Trial. BMC Psychol. 2022, 10, 123. [Google Scholar] [CrossRef] [PubMed]
- Janssen, M.; Heerkens, Y.; Kuijer, W.; Van Der Heijden, B.; Engels, J. Effects of Mindfulness-Based Stress Reduction on Employees’ Mental Health: A Systematic Review. PLoS ONE 2018, 13, e0191332. [Google Scholar] [CrossRef]
- Sampei, M.; Okubo, R.; Sado, M.; Piedvache, A.; Mizoue, T.; Yamaguchi, K.; Morisaki, N. Emotional Exhaustion of Burnout Among Medical Staff and Its Association With Mindfulness and Social Support: A Single Center Study During the COVID-19 Pandemic in Japan. Front. Psychiatry 2022, 13, 774919. [Google Scholar] [CrossRef]
- Conversano, C.; Di Giuseppe, M.; Miccoli, M.; Ciacchini, R.; Gemignani, A.; Orrù, G. Mindfulness, Age and Gender as Protective Factors Against Psychological Distress During COVID-19 Pandemic. Front. Psychol. 2020, 11, 1900. [Google Scholar] [CrossRef] [PubMed]
- Consoli, S.; Rossi, A.; Thompson, L.Y.; Volpi, C.; Mannarini, S.; Castelnuovo, G.; Molinari, E. Assessing Psychometric Properties of the Italian Version of the Heartland Forgiveness Scale. Front. Psychol. 2020, 11, 596501. [Google Scholar] [CrossRef]
- Baskin, T.W.; Enright, R.D. Intervention Studies on Forgiveness: A Meta-Analysis; Wiley Blackwell: Hoboken, NJ, USA, 2004; Volume 82, pp. 79–90. [Google Scholar]
- Niveau, N.; New, B.; Beaudoin, M. Self-Esteem Interventions in Adults—A Systematic Review and Meta-Analysis. J. Res. Personal. 2021, 94, 104131. [Google Scholar] [CrossRef]
- Panzeri, A.; Bettinardi, O.; Bottesi, G.; Bertolotti, G.; Brambatti, L.; Monfredo, M.; Mignemi, G.; Bruno, G.; Vidotto, G.; Spoto, A.; et al. Assessment of Perceived Support in the Context of Emergency: Development and Validation of the Psycho-Social Support Scale. Curr. Psychol. 2023, 42, 22514–22525. [Google Scholar] [CrossRef]
- De Kock, J.H.; Latham, H.A.; Leslie, S.J.; Grindle, M.; Munoz, S.A.; Ellis, L.; Polson, R.; O’Malley, C.M. A Rapid Review of the Impact of COVID-19 on the Mental Health of Healthcare Workers: Implications for Supporting Psychological Well-Being. BMC Public Health 2021, 21, 104. [Google Scholar] [CrossRef]
- Mignemi, G.; Panzeri, A.; Granziol, U.; Bruno, G.; Bertamini, M.; Giulio, V.; Spoto, A. The Mediating Role of Scientifical-Medical Satisfaction between COVID-19 Conspiracy Beliefs and Vaccine Confidence: A Two-Waves Structural Equation Model. J. Behav. Med. 2023, 46, 201–211. [Google Scholar] [CrossRef]
- Faraci, P.; Bottaro, R.; Valenti, G.D.; Craparo, G. Psychological Well-Being During the Second Wave of COVID-19 Pandemic: The Mediation Role of Generalized Anxiety. Psychol. Res. Behav. Manag. 2022, 15, 695–709. [Google Scholar] [CrossRef] [PubMed]
- Rossi, A.A.; Marconi, M.; Taccini, F.; Verusio, C.; Mannarini, S. Screening for Distress in Oncological Patients: The Revised Version of the Psychological Distress Inventory (PDI-R). Front. Psychol. 2022, 13, 859478. [Google Scholar] [CrossRef] [PubMed]
- Panzeri, A.; DeVita, M.; Di Rosa, E.; Bottesi, G.; Brundisini, V.; Guarrera, C.; Ravelli, A.; Ponza, I.; Cattelan, A.; Volpe, B.; et al. Trauma Shaping the Psychopathological Correlates of Patients with Long-COVID: A 6-Months Longitudinal Study with Repeated Measures Mixed Models. Psychiatry Res. 2023, 330, 115609. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, S.G.; Gómez, A.F. Mindfulness-Based Interventions for Anxiety and Depression. Psychiatr. Clin. N. Am. 2017, 40, 739–749. [Google Scholar] [CrossRef] [PubMed]



| Variables | Control Group (n = 20) | MBSR Group (n = 17) | Statistics and p Value |
| Age (Mean ± SD) | 41.75 ± 10.93 | 42.82 ± 11.54 | t = |0.29|, df = 35, p = 0.773, Cohen’s d = −0.10 |
| Sex Male Female | 3 17 | 3 14 | X2 = 0.05, df = 1, p = 0.828 |
| Work position nurses, educators, and social health workers | 16 | 14 | X2 = 0.07, df = 1, p = 0.791 |
| physicians, psychologists | 4 | 3 |
| Control Group (n = 20) | Experimental MBSR Group (n = 17) | |
|---|---|---|
| Cortisol t0 | 3.33 (1.27) | 4.09 (1.60) |
| Cortisol t1 | 4.61 (1.85) | 2.90 (1.14) |
| Cortisol t2 | 3.98 (1.70) | 3.68 (1.36) |
| Perceived stress scale t0 | 18.30 (8.46) | 17.76 (6.95) |
| Perceived stress scale t1 | 16.05 (9.11) | 13.62 (8.28) |
| Perceived stress scale t2 | 17.50 (7.94) | 14.24 (7.83) |
| Attention and awareness t0 | 67.89 (10.24) | 62.72 (12.02) |
| Attention and awareness t1 | 66.73 (9.45) | 68.87 (7.26) |
| Attention and awareness t2 | 65.15 (12.41) | 68.74 (12.18) |
| IANUS Job strain t0 | 49.25 (9.50) | 51.47 (14.87) |
| IANUS Job strain t1 | 50.00 (11.58) | 48.44 (18.32) |
| IANUS Job strain t2 | 50.50 (16.54) | 45.88 (15.43) |
| IANUS Positive meaning t0 | 79.95 (14.91) | 77.57 (14.83) |
| IANUS Positive meaning t1 | 82.19 (12.55) | 77.73 (14.61) |
| IANUS Positive meaning t2 | 77.50 (14.96) | 77.21 (14.14) |
| IANUS Emotional fatigue t0 | 40.83 (14.02) | 49.51 (26.10) |
| IANUS Emotional fatigue t1 | 41.67 (11.79) | 43.23 (26.57) |
| IANUS Emotional fatigue t2 | 35.00 (9.21) | 42.16 (22.72) |
| IANUS Relational difficulties t0 | 43.33 (7.45) | 47.55 (13.10) |
| IANUS Relational difficulties t1 | 42.92 (13.32) | 46.35 (18.25) |
| IANUS Relational difficulties t2 | 44.58 (13.86) | 44.12 (11.32) |
| First part | ||||||||||||||||||
| Cortisol—Within-Subjects Effects | df | F | p | η2p | ||||||||||||||
| Time | 2 | 0.1 | 0.907 | 0 | ||||||||||||||
| Time ✻ group | 2 | 10.08 | < 0.001 | 0.23 | ||||||||||||||
| Residual | 68 | |||||||||||||||||
| Between-Subjects Effects | df | F | p | η2p | ||||||||||||||
| Group | 1 | 1.09 | 0.303 | 0.03 | ||||||||||||||
| Residual | 34 | |||||||||||||||||
| Cortisol Estimated Marginal Means—Time ✻ group | 95% CI | |||||||||||||||||
| Group | Time | Mean | SE | Lower | Upper | |||||||||||||
| Control | T0 | 3.33 | 0.32 | 2.68 | 3.97 | |||||||||||||
| T1 | 4.61 | 0.35 | 3.9 | 5.33 | ||||||||||||||
| T2 | 3.98 | 0.35 | 3.27 | 4.69 | ||||||||||||||
| Experimental | T0 | 4.09 | 0.36 | 3.37 | 4.82 | |||||||||||||
| T1 | 2.9 | 0.39 | 2.1 | 3.7 | ||||||||||||||
| T2 | 3.68 | 0.39 | 2.89 | 4.47 | ||||||||||||||
| Second part: Post hoc-tests | ||||||||||||||||||
| Time | Group 1 | time | Group 2 | Mean Difference | SE | t | p | pholm | ||||||||||
| T0 | Control | – | T0 | Exp. | −0.77 | 0.48 | −1.6 | 0.118 | 0.886 | |||||||||
| T0 | Control | – | T1 | control | −1.29 | 0.34 | −3.75 | <.001 | 0.010 * | |||||||||
| T0 | Control | – | T1 | Exp. | 0.43 | 0.51 | 0.85 | 0.404 | 1 | |||||||||
| T0 | Control | – | T2 | control | −0.65 | 0.39 | −1.7 | 0.098 | 0.886 | |||||||||
| T0 | Control | – | T2 | Exp. | −0.36 | 0.5 | −0.7 | 0.486 | 1 | |||||||||
| T0 | Exp. | – | T1 | control | −0.52 | 0.5 | −1.03 | 0.308 | 1 | |||||||||
| T0 | Exp. | – | T1 | Exp. | 1.2 | 0.38 | 3.12 | 0.004 | 0.048 * | |||||||||
| T0 | Exp. | – | T2 | control | 0.11 | 0.5 | 0.23 | 0.823 | 1 | |||||||||
| T0 | Exp. | – | T2 | Exp. | 0.41 | 0.43 | 0.96 | 0.345 | 1 | |||||||||
| T1 | Control | – | T1 | Exp. | 1.72 | 0.53 | 3.24 | 0.003 | 0.037 * | |||||||||
| T1 | Control | – | T2 | control | 0.63 | 0.38 | 1.67 | 0.105 | 0.886 | |||||||||
| T1 | Control | – | T2 | Exp. | 0.93 | 0.53 | 1.77 | 0.085 | 0.855 | |||||||||
| T1 | Exp. | – | T2 | control | −1.08 | 0.53 | −2.06 | 0.047 | 0.567 | |||||||||
| T1 | Exp. | – | T2 | Exp. | −0.78 | 0.42 | −1.85 | 0.073 | 0.806 | |||||||||
| T2 | Control | – | T2 | Exp. | 0.3 | 0.52 | 0.57 | 0.571 | 1 | |||||||||
| Part 1 | |||||||||||||||
| Within-Subjects Effects | df | F | p | η2p | |||||||||||
| Time | 2 | 1.22 | 0.301 | 0.04 | |||||||||||
| Time ✻ group | 2 | 4.51 | 0.015 | 0.12 | |||||||||||
| Residual | 66 | ||||||||||||||
| Between-Subjects Effects | df | F | p | η2p | |||||||||||
| Group | 1 | 0.02 | 0.895 | 0.00 | |||||||||||
| Residual | 33 | ||||||||||||||
| MAAS, Estimated Marginal Means—Time ✻ group | 95% Confidence Interval | ||||||||||||||
| group | Time | Mean | SE | Lower | Upper | ||||||||||
| Control | T1 | 67.89 | 2.51 | 62.78 | 73.00 | ||||||||||
| T2 | 66.73 | 1.94 | 62.79 | 70.67 | |||||||||||
| T3 | 65.15 | 2.81 | 59.43 | 70.86 | |||||||||||
| experimental | T1 | 62.77 | 2.90 | 56.87 | 68.66 | ||||||||||
| T2 | 68.73 | 2.24 | 64.17 | 73.28 | |||||||||||
| T3 | 69.56 | 3.24 | 62.96 | 76.16 | |||||||||||
| Part 2: post hoc tests | |||||||||||||||
| Time | group | Time | group | Mean Difference | SE | df | t | p | pholm | ||||||
| T0 | control | T0 | Exp. | 5.12 | 3.83 | 33.00 | 1.34 | 0.191 | 1 | ||||||
| T1 | control | 1.16 | 1.99 | 33.00 | 0.58 | 0.564 | 1 | ||||||||
| T1 | Exp. | −0.84 | 3.36 | 33.00 | −0.25 | 0.805 | 1 | ||||||||
| T2 | control | 2.74 | 2.51 | 33.00 | 1.09 | 0.282 | 1 | ||||||||
| T2 | Exp. | −1.67 | 4.10 | 33.00 | −0.41 | 0.687 | 1 | ||||||||
| Exp. | T1 | control | −3.96 | 3.49 | 33.00 | −1.14 | 0.264 | 1 | |||||||
| T1 | Exp. | −5.96 | 2.30 | 33.00 | −2.60 | 0.014 | 0.210 | ||||||||
| T2 | control | −2.38 | 4.04 | 33.00 | −0.59 | 0.559 | 1 | ||||||||
| T2 | Exp. | −6.79 | 2.89 | 33.00 | −2.35 | 0.025 | 0.351 | ||||||||
| T1 | control | T1 | Exp. | −2.00 | 2.96 | 33.00 | −0.67 | 0.505 | 1 | ||||||
| T2 | control | 1.58 | 1.94 | 33.00 | 0.81 | 0.421 | 1 | ||||||||
| T2 | Exp. | −2.83 | 3.78 | 33.00 | −0.75 | 0.459 | 1 | ||||||||
| Exp. | T2 | control | 3.58 | 3.59 | 33.00 | 1.00 | 0.326 | 1 | |||||||
| T2 | Exp. | −0.83 | 2.24 | 33.00 | −0.37 | 0.713 | 1 | ||||||||
| T2 | control | T2 | Exp. | −4.41 | 4.29 | 33.00 | −1.03 | 0.311 | 1 | ||||||
| Within-Subjects Effects | df | F | p | η2p | |||
| Time | 2 | 4.33 | 0.017 | 0.11 | |||
| time ✻ group | 2 | 0.76 | 0.471 | 0.02 | |||
| Residual | 68 | ||||||
| Between-Subjects Effects | df | F | p | η2p | |||
| group | 1 | 0.73 | 0.400 | 0.02 | |||
| Residual | 34 | ||||||
| Estimated Marginal Means—Time ✻ group | 95% CI | ||||||
| Group | Time | Mean | SE | Lower | Upper | ||
| Control | T0 | 18.30 | 1.77 | 14.70 | 21.90 | ||
| T1 | 16.05 | 1.96 | 12.07 | 20.03 | |||
| T2 | 17.50 | 1.79 | 13.86 | 21.14 | |||
| Experimental | T0 | 17.69 | 1.98 | 13.66 | 21.71 | ||
| T1 | 13.62 | 2.19 | 9.18 | 18.07 | |||
| T2 | 14.25 | 2.00 | 10.18 | 18.32 | |||
| Within-Subjects Effects | Df | F | p | η2p | |
| Time | 2 | 0.71 | 0.493 | 0.02 | |
| time ✻ group | 2 | 1.74 | 0.183 | 0.05 | |
| Residual | 68 | ||||
| Between-Subjects Effects | Df | F | p | η2p | |
| group | 1 | 0.04 | 0.846 | 0.00 | |
| Residual | 34 | ||||
| Estimated Marginal Means—Time ✻ group | 95% CI | ||||
| Group | Time | Mean | SE | Lower | Upper |
| Control | T0 | 49.25 | 2.74 | 43.68 | 54.82 |
| T1 | 50.00 | 3.34 | 43.21 | 56.79 | |
| T2 | 50.50 | 3.61 | 43.16 | 57.84 | |
| Experimental | T0 | 52.19 | 3.07 | 45.96 | 58.42 |
| T1 | 48.44 | 3.73 | 40.85 | 56.03 | |
| T2 | 46.56 | 4.04 | 38.35 | 54.77 | |
| First part | ||||||||||||
| Within-Subjects Effects | ||||||||||||
| Effect | df | F | p | η2ₚ | ||||||||
| Time | 2 | 6.71 | 0.002 | 0.16 | ||||||||
| Time ✻ Group | 2 | 2.96 | 0.059 | 0.08 | ||||||||
| Residual | 68 | |||||||||||
| Between-Subjects Effects | ||||||||||||
| Effect | df | F | p | η2ₚ | ||||||||
| Group | 1 | 1.24 | 0.274 | 0.04 | ||||||||
| Residual | 34 | |||||||||||
| IANUS emotional fatigue, estimates marginal means—Time ✻ group | ||||||||||||
| Group | Time | mean | SE | 95% CI Lower | 95% CI Upper | |||||||
| Control | T0 | 40.83 | 4.54 | 31.61 | 50.05 | |||||||
| T1 | 41.67 | 4.41 | 32.70 | 50.63 | ||||||||
| T2 | 35.00 | 3.75 | 27.38 | 42.62 | ||||||||
| Experimental | T0 | 51.04 | 5.07 | 40.73 | 61.35 | |||||||
| T1 | 43.23 | 4.93 | 33.21 | 53.25 | ||||||||
| T2 | 43.23 | 4.19 | 34.71 | 51.75 | ||||||||
| Second part: post hoc tests | ||||||||||||
| Time | Group | Time | Group | Mean Difference | SE | df | t | p | pholm | |||
| T0 | Control | T0 | Exp. | −10.21 | 6.81 | 34.0 | −1.50 | 0.143 | 1 | |||
| T1 | Control | −0.83 | 2.23 | 34.0 | −0.37 | 0.711 | 1 | |||||
| T1 | Exp. | −2.40 | 6.70 | 34.0 | −0.36 | 0.723 | 1 | |||||
| T2 | Control | 5.83 | 2.70 | 34.0 | 2.16 | 0.038 | 0.413 | |||||
| T2 | Exp. | −2.40 | 6.18 | 34.0 | −0.39 | 0.700 | 1 | |||||
| Exp. | T1 | Control | 9.37 | 6.72 | 34.0 | 1.39 | 0.172 | 1 | ||||
| T1 | Exp. | 7.81 | 2.49 | 34.0 | 3.13 | 0.004 | 0.053 | |||||
| T2 | Control | 16.04 | 6.31 | 34.0 | 2.54 | 0.016 | 0.188 | |||||
| T2 | Exp. | 7.81 | 3.01 | 34.0 | 2.59 | 0.014 | 0.181 | |||||
| T1 | Control | T1 | Exp. | −1.56 | 6.62 | 34.0 | −0.24 | 0.815 | 1 | |||
| T2 | Control | 6.67 | 2.50 | 34.0 | 2.67 | 0.012 | 0.163 | |||||
| T2 | Exp. | −1.56 | 6.08 | 34.0 | −0.26 | 0.799 | 1 | |||||
| Exp. | T2 | Control | 8.23 | 6.19 | 34.0 | 1.33 | 0.193 | 1 | ||||
| T2 | Exp. | 0.00 | 2.80 | 34.0 | 0.00 | 1.000 | 1 | |||||
| T2 | Control | T2 | Exp. | −8.23 | 5.62 | 34.0 | −1.46 | 0.153 | 1 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Panzeri, A.; Bettinardi, O.; Giommi, F.; Grassi, M.; Rossetti, M.; Barile, P.; Del Bello, B.; Gardi, C. Mindfulness Improves Awareness and Cortisol Levels During COVID-19 Lockdown: A Randomised Controlled Trial in Healthcare Workers. Healthcare 2025, 13, 2455. https://doi.org/10.3390/healthcare13192455
Panzeri A, Bettinardi O, Giommi F, Grassi M, Rossetti M, Barile P, Del Bello B, Gardi C. Mindfulness Improves Awareness and Cortisol Levels During COVID-19 Lockdown: A Randomised Controlled Trial in Healthcare Workers. Healthcare. 2025; 13(19):2455. https://doi.org/10.3390/healthcare13192455
Chicago/Turabian StylePanzeri, Anna, Ornella Bettinardi, Fabio Giommi, Maddalena Grassi, Massimo Rossetti, Pasqua Barile, Barbara Del Bello, and Concetta Gardi. 2025. "Mindfulness Improves Awareness and Cortisol Levels During COVID-19 Lockdown: A Randomised Controlled Trial in Healthcare Workers" Healthcare 13, no. 19: 2455. https://doi.org/10.3390/healthcare13192455
APA StylePanzeri, A., Bettinardi, O., Giommi, F., Grassi, M., Rossetti, M., Barile, P., Del Bello, B., & Gardi, C. (2025). Mindfulness Improves Awareness and Cortisol Levels During COVID-19 Lockdown: A Randomised Controlled Trial in Healthcare Workers. Healthcare, 13(19), 2455. https://doi.org/10.3390/healthcare13192455







