Adolescent Idiopathic Scoliosis in the Adult Patient: New Classification with a Treatment-Oriented Guideline
Abstract
1. Introduction
2. Materials and Methods
3. Results
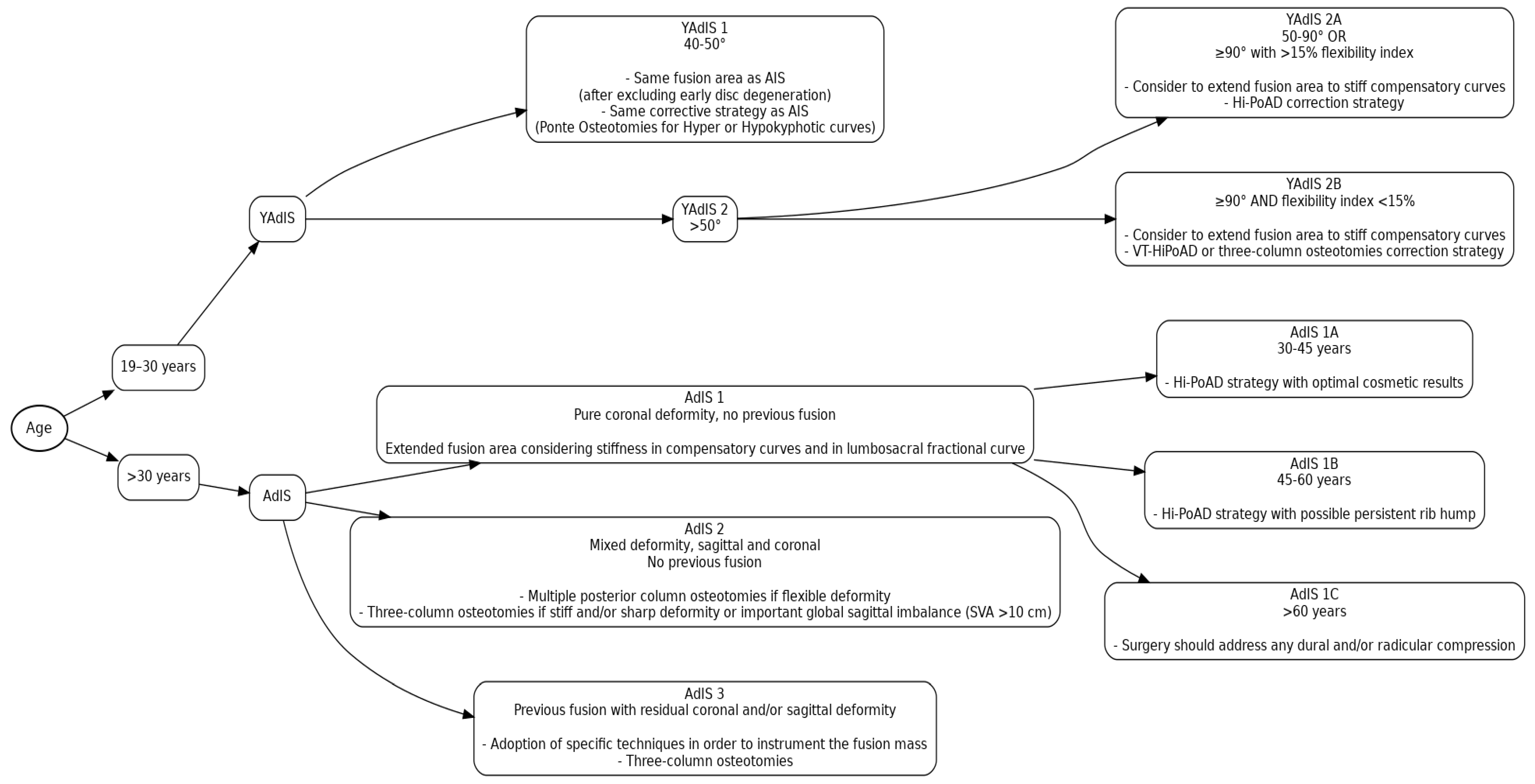
3.1. Young Adult Idiopathic Scoliosis (YAdIS—19–30 Years Old)
3.1.1. YAdIS 1
3.1.2. YAdIS 2
- -
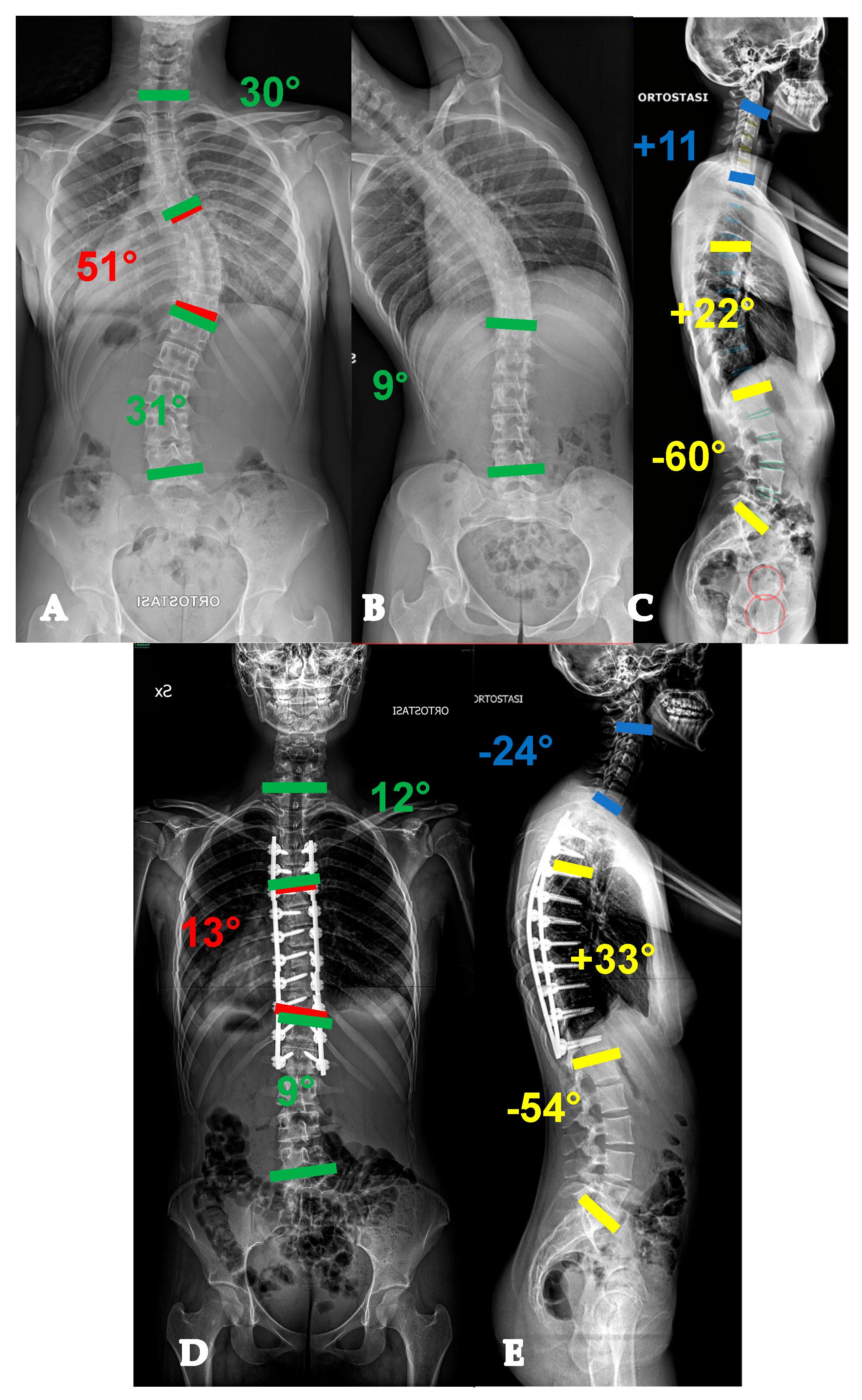
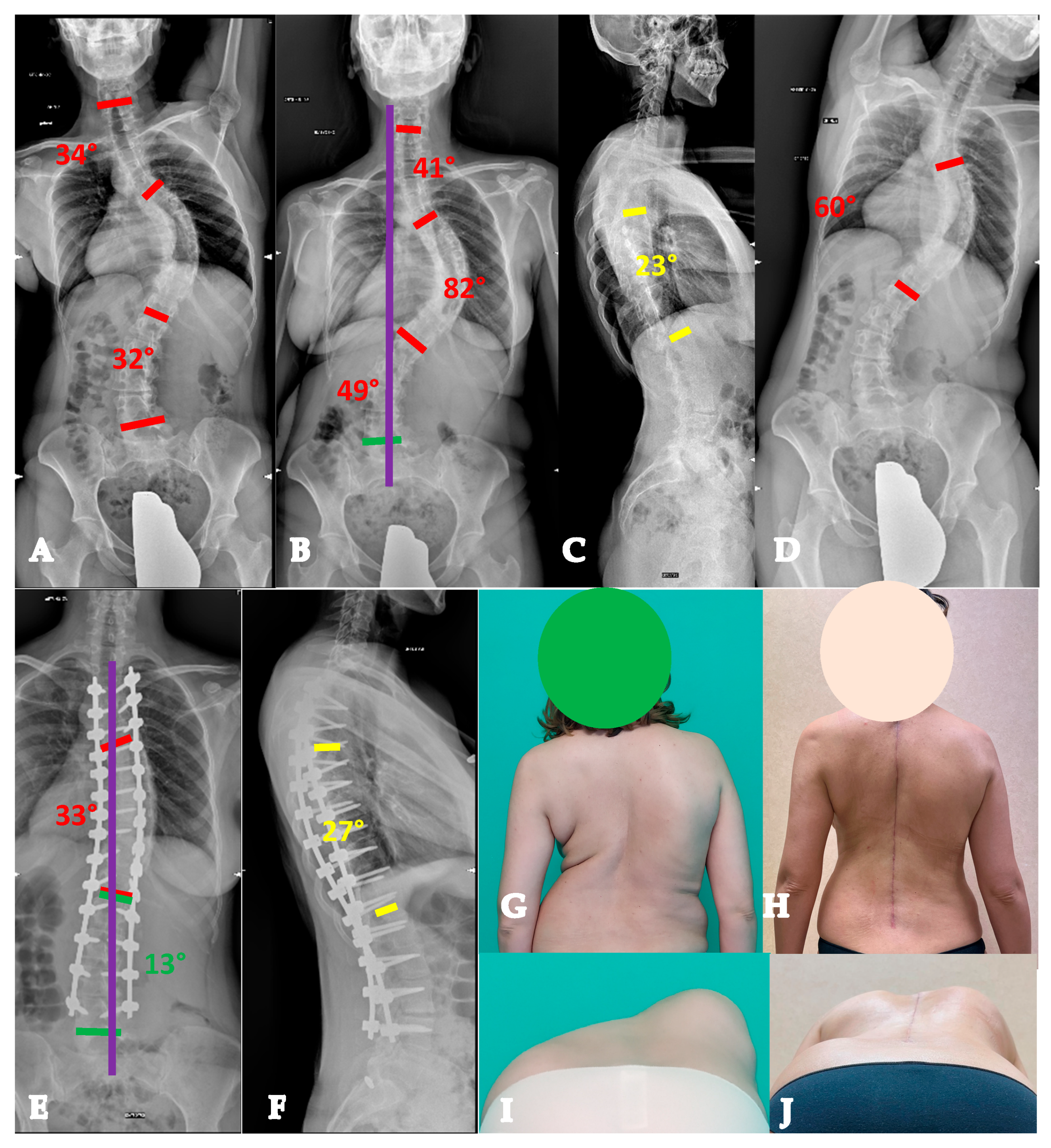
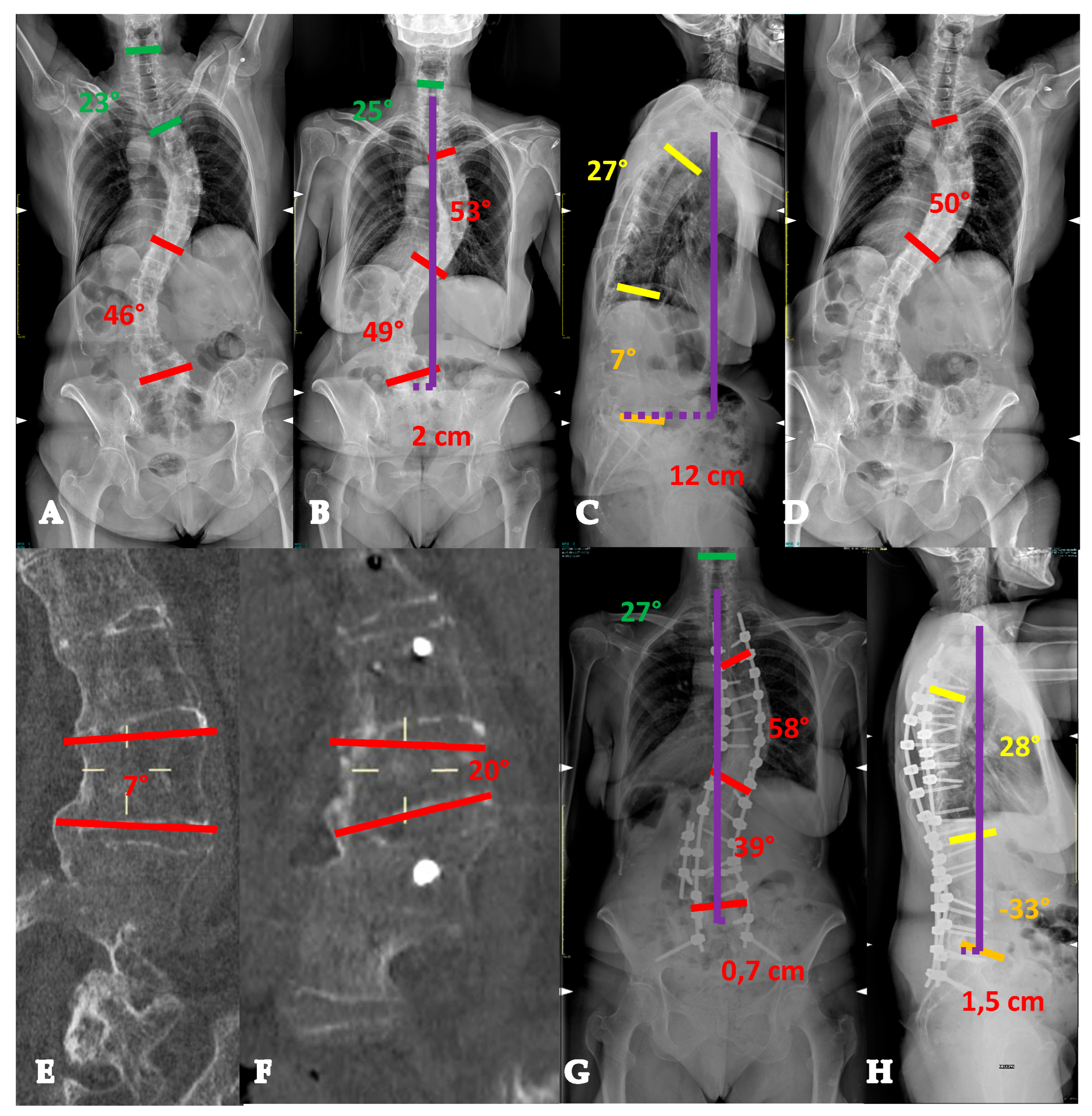
- For curves < 90° OR ≥90° and with a flexibility index > 15% (YADIS 2A), a combination of strategies with an all-posterior approach, already published by the authors under the acronym HiPoAD (High-Density Pedicle Screws, Ponte Osteotomies, Asymmetric Rods Contouring, Direct Vertebral Rotation) [10], may be sufficient to address the deformity. In particular, high-density constructs are preferrable in order to dissipate the corrective forces on every level and decrease the pull-out risks. Then, an aggressive posterior release based on multiple asymmetric Ponte osteotomies is of paramount importance, in order to allow an optimal deroto-translation over two asymmetrically contoured rods (Figure 3) [10,11].
- -
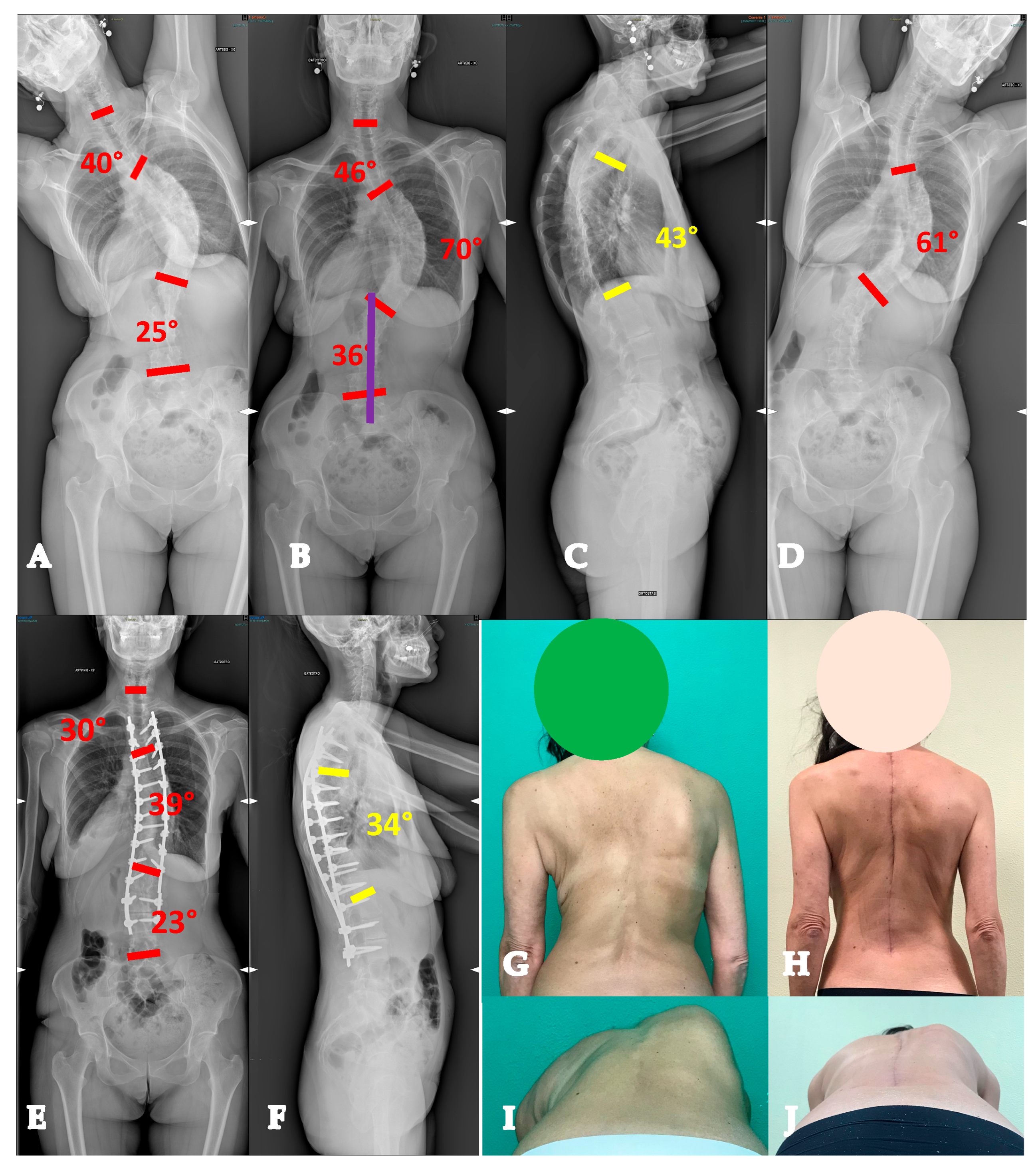
- For curves ≥ 90° AND with a flexibility index < 15% (YADIS 2B), the HiPoAD technique, even though it proved to be effective for this kind of curve when addressed during adolescent years [12], may not be powerful enough for YAdIS 2 patients. These cases should be addressed with a three-columnar approach. One strategy could be to adopt three-column osteotomies like VCR. A possible alternative, in order to avoid the risks of a three-column osteotomy, is to perform a three-columnar release through a combined approach: an anterior thoracoscopic release (wide resection of anterior longitudinal ligament and multiple periapical discectomies), followed by a posterior column release based on multiple Ponte Osteotomies and a posterior correction (VT-HiPoAD, Videothoracoscopic release—HiPoAD) (Figure 4).
3.2. Adult Idiopathic Scoliosis (AdIS—>30 Years Old)
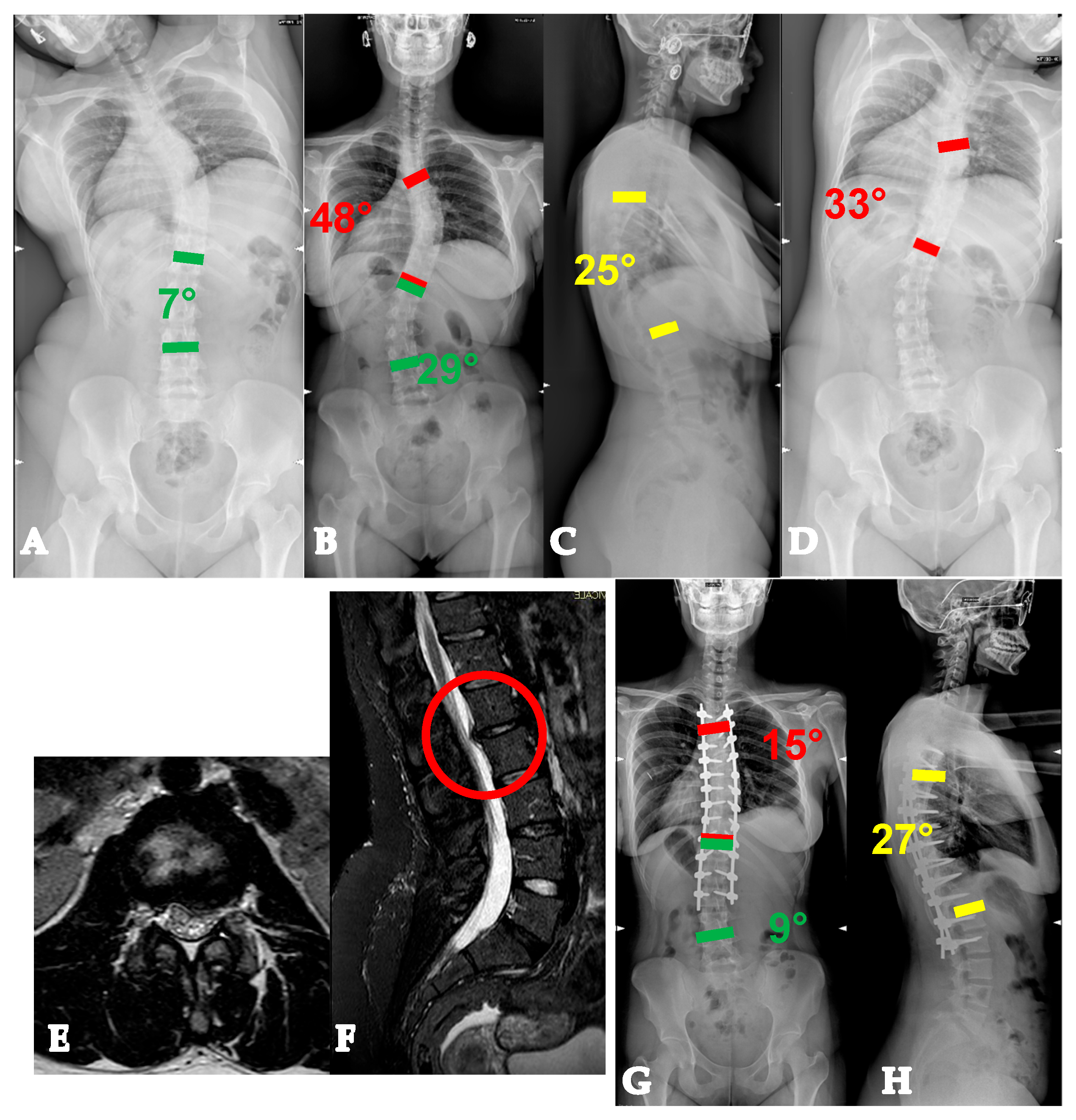
3.2.1. AdIS 1
- -
- -
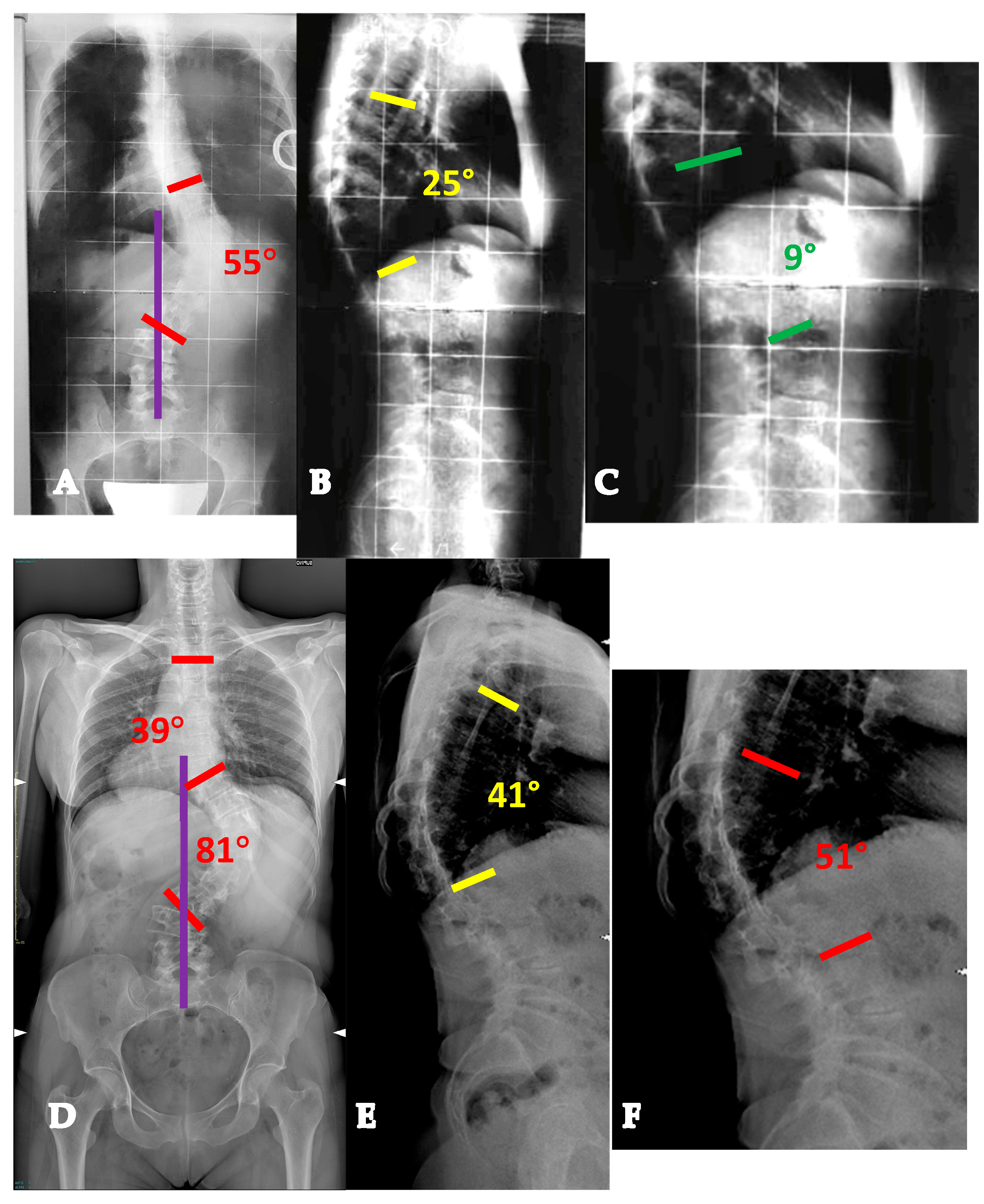
- AdIS 1B: 45–60 years old. These patients usually have a stiffer main curve, with the not infrequent presence of anterior column osteophytes, especially at the concave side. In this setting, combined corrective strategies based on posterior releases (Hi-PoAD [10]) can still achieve an optimal translation, but often, derotation potential is limited, with a possible residual of a partial rib hump (Figure 6).
- -
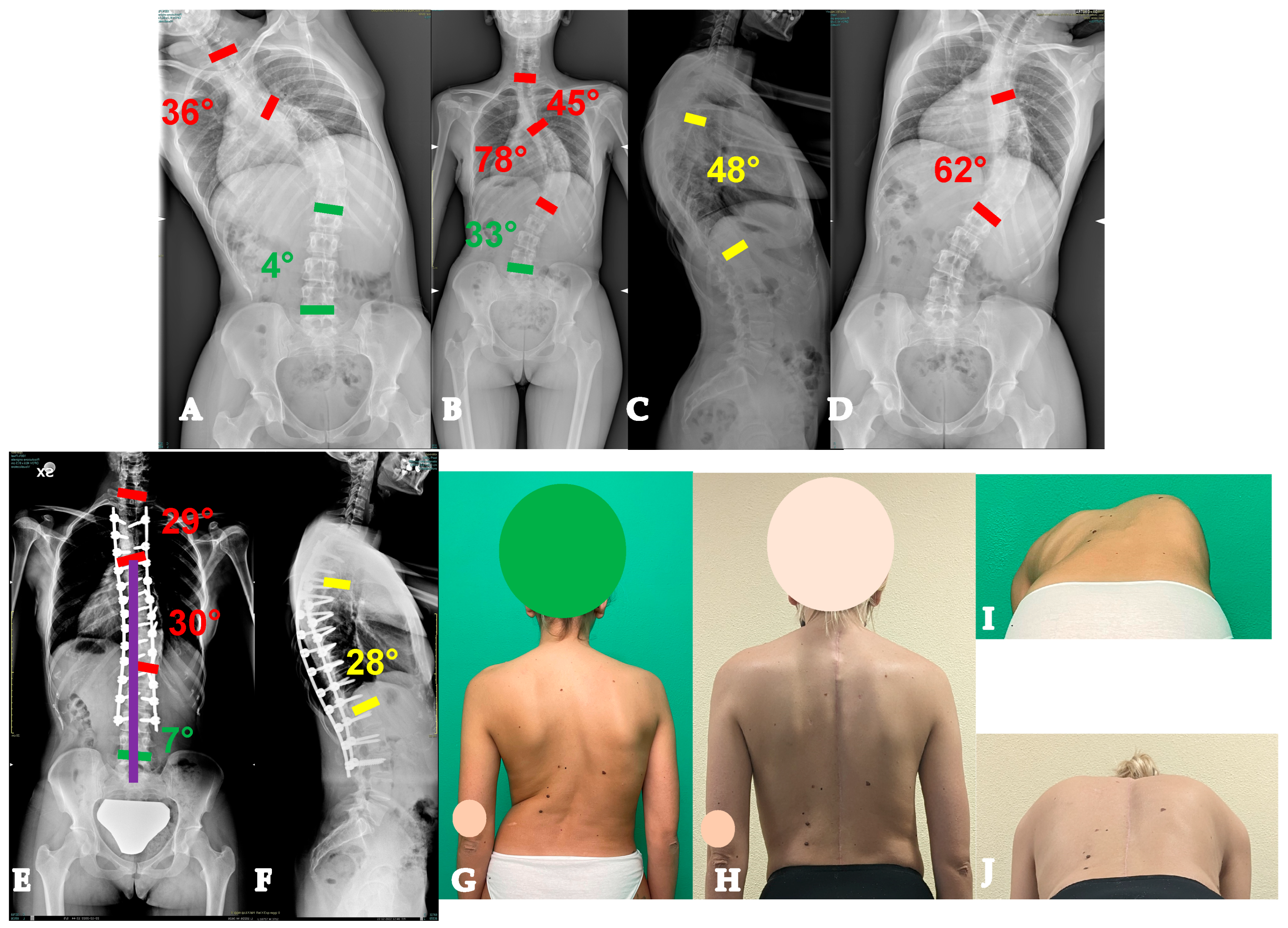
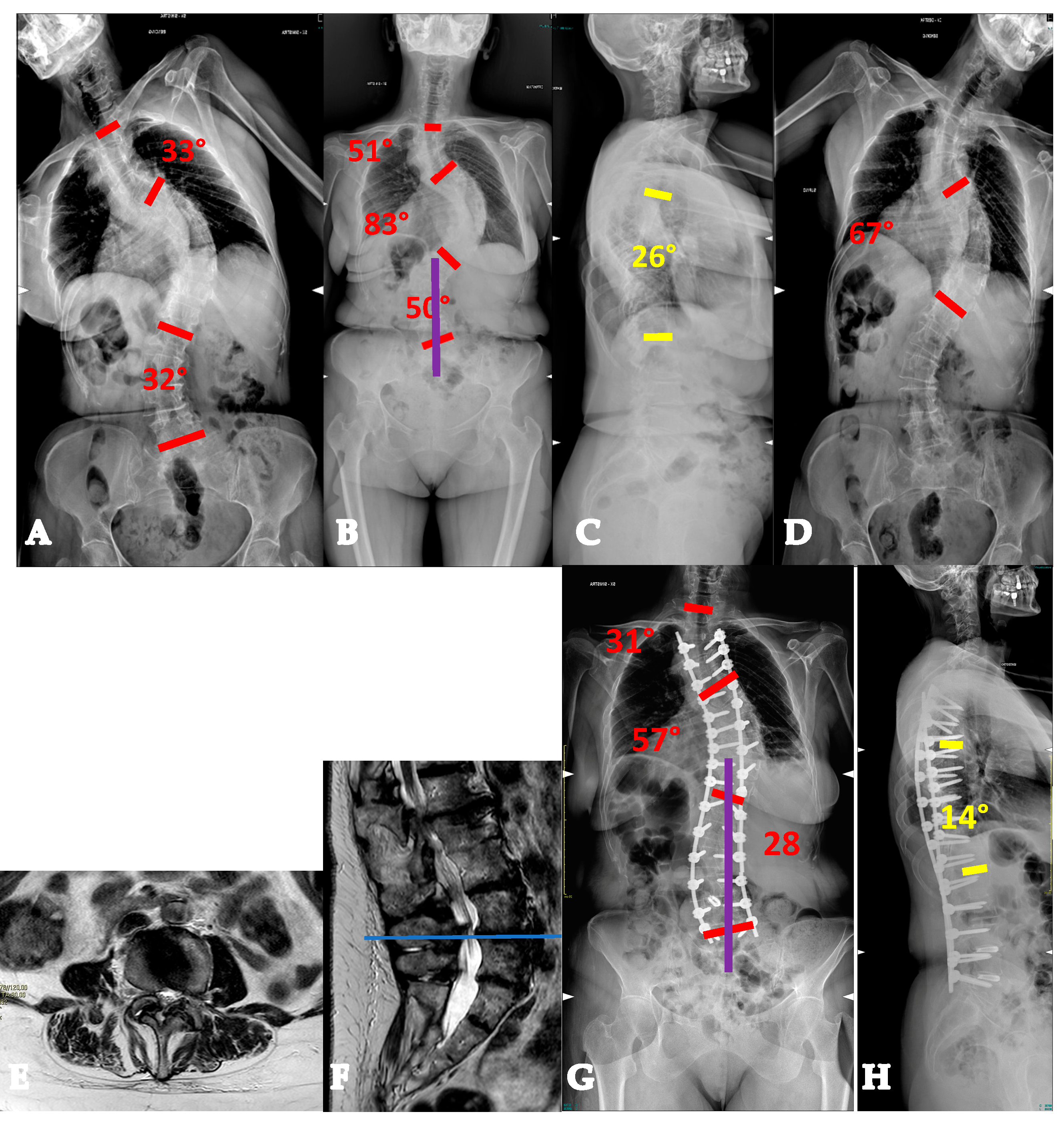
- AdIS 1C: >60 years old. This is infrequent, since patients in this age group more commonly tend to lie in the AdIS 2 group. This group is burdened by an increased stiffness due to an even more frequent anterior column spontaneous fusion, resulting in a less powerful correction both in terms of translation and derotation, with a consequent smaller correction rate and more prominent residual rib hump. However, it must be considered that these patients more commonly present to surgeons because of pain rather than cosmetic concerns. In this view, pain generators should be carefully identified and adequately treated, performing foraminal and/or central decompressions and discectomies where appropriate (Figure 7).
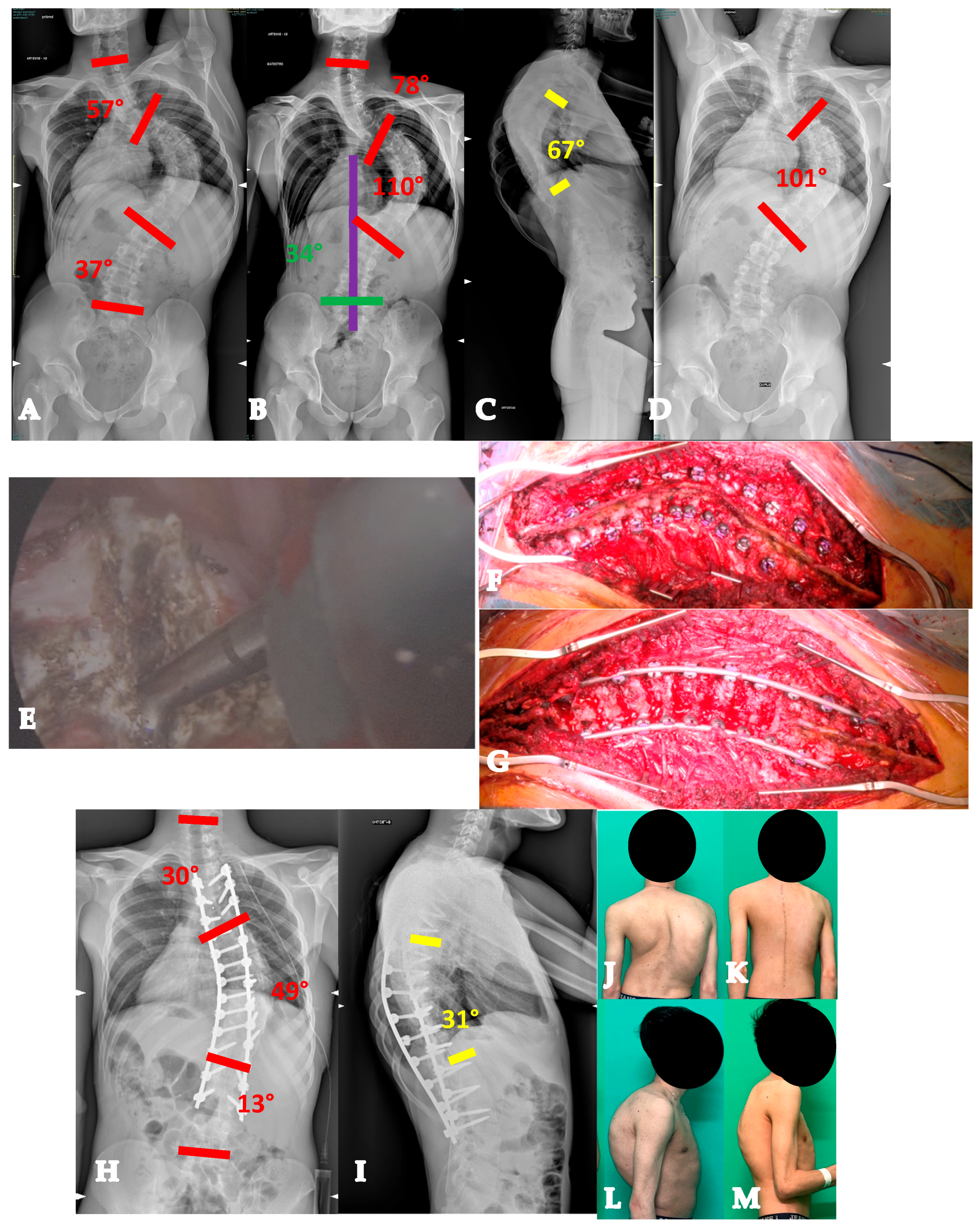
3.2.2. AdIS 2
3.2.3. AdIS 3
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Aebi, M. The adult scoliosis. Eur. Spine J. 2005, 14, 925–948. [Google Scholar] [CrossRef]
- Lin, J.D.; Osorio, J.A.; Baum, G.R.; Menger, R.P.; Reid, P.C.; Dyrszka, M.D.; Amorosa, L.F.; Sardar, Z.M.; Mandigo, C.E.; Angevine, P.D.; et al. A new modular radiographic classification of adult idiopathic scoliosis as an extension of the Lenke classification of adolescent idiopathic scoliosis. Spine Deform. 2021, 9, 175–183. [Google Scholar] [CrossRef]
- Lavelle, W.; Kurra, S.; Hu, X.; Lieberman, I. Clinical Outcomes of Idiopathic Scoliosis Surgery: Is There a Difference Between Young Adult Patients and Adolescent Patients? Cureus 2020, 12, e8118. [Google Scholar] [CrossRef]
- Gomez-Rice, A.; Capdevila-Bayo, M.; Núñez-Pereira, S.; Haddad, S.; Vila-Casademunt, A.; Pérez-Grueso, F.; Kleinstück, F.; Obeid, I.; Alanay, A.; Pellise, F.; et al. A 5-year follow-up of the effect of corrective surgery in young adults with idiopathic scoliosis. Spine Deform. 2023, 11, 605–615. [Google Scholar] [CrossRef] [PubMed]
- Zhu, F.; Bao, H.; Yan, P.; Liu, S.; Zhu, Z.; Liu, Z.; Bao, M.; Qiu, Y. Comparison of Surgical Outcome of Adolescent Idiopathic Scoliosis and Young Adult Idiopathic Scoliosis: A Match-pair Analysis of 160 Patients. Spine 2017, 42, E1133–E1139. [Google Scholar] [CrossRef] [PubMed]
- Kurra, S.; DeMercurio, P.; Lavelle, W.F. Comparison of operative implications between adolescent and young adult idiopathic scoliosis patients from scoliosis research society mortality and morbidity database. Spine Deform. 2022, 10, 1133–1138. [Google Scholar] [CrossRef] [PubMed]
- Scoliosis Research Society Bracing Manual. Scoliosis Research Society Brace Manual; Scoliosis Research Society: Milwaukee, WI, USA, 2003. [Google Scholar]
- Bess, S.; Boachie-Adjei, O.; Burton, D.; Cunningham, M.; Shaffrey, C.; Shelokov, A.; Hostin, R.; Schwab, F.; Wood, K.; Akbarnia, B. Pain and disability determine treatment modality for older patients with adult scoliosis, while deformity guides treatment for younger patients. Spine 2009, 34, 2186–2190. [Google Scholar] [CrossRef]
- Lenke, L.G.; Betz, R.R.; Harms, J.; Bridwell, K.H.; Clements, D.H.; Lowe, T.G.; Blanke, K. Adolescent idiopathic scoliosis. A new classification to determine extent of spinal arthrodesis. J. Bone Jt. Surg. Ser. A 2001, 83, 1169–1181. [Google Scholar] [CrossRef]
- Faldini, C.; Barile, F.; Perna, F.; Pasini, S.; Fiore, M.; Viroli, G.; Di Martino, A.; Ruffilli, A. Hi-PoAD technique for Adolescent Idiopathic Scoliosis in Adult: Personal case series. Eur. Spine J. 2021, 30, 3509–3516. [Google Scholar] [CrossRef]
- Zhang, Y.; Hai, Y.; Tao, L.; Yang, J.; Zhou, L.; Yin, P.; Pan, A.; Zhang, Y.; Liu, C. Posterior Multiple-Level Asymmetrical Ponte Osteotomies for Rigid Adult Idiopathic Scoliosis. World Neurosurg. 2019, 127, e467–e473. [Google Scholar] [CrossRef]
- Faldini, C.; Viroli, G.; Barile, F.; Manzetti, M.; Ialuna, M.; Traversari, M.; Vita, F.; Ruffilli, A. One stage correction via the Hi-PoAD technique for the management of severe, stiff, adolescent idiopathic scoliosis curves > 90°. Spine Deform. 2023, 11, 957–967. [Google Scholar] [CrossRef]
- Dewan, M.C.; Mummareddy, N.; Bonfield, C. The influence of pregnancy on women with adolescent idiopathic scoliosis. Eur. Spine J. 2018, 27, 253–263. [Google Scholar] [CrossRef]
- Okanishi, N.; Kito, N.; Akiyama, M.; Yamamoto, M. Spinal curvature and characteristics of postural change in pregnant women. Acta Obstet. Gynecol. Scand. 2012, 91, 856–861. [Google Scholar] [CrossRef]
- Moore, K.; Dumas, G.A.; Reid, J.G. Postural changes associated with pregnancy and their relationship with low-back pain. Clin. Biomech. 1990, 5, 169–174. [Google Scholar] [CrossRef]
- Satin, A.M.; Kisinde, S.; Lieberman, I.H. Robotic-Assisted Revision Spine Surgery. Int. J. Spine Surg. 2022, 16, S14–S21. [Google Scholar] [CrossRef] [PubMed]
- Lim, M.R.; Girardi, F.P.; Yoon, S.C.; Huang, R.C.; Cammisa, F.P.J. Accuracy of computerized frameless stereotactic image-guided pedicle screw placement into previously fused lumbar spines. Spine 2005, 30, 1793–1798. [Google Scholar] [CrossRef] [PubMed]
- Faldini, C.; Barile, F.; Cerasoli, T.; Ialuna, M.; Viroli, G.; Manzetti, M.; Traversari, M.; Mazzotti, A.; Ruffilli, A. Accuracy of Patient-Specific 3D-Printed Guides for Pedicle Screw Insertion in Spine Revision Surgery: Results of a Retrospective Study. Surg. Technol. Int. 2022, 41, 395–401. [Google Scholar] [CrossRef]
- Lewis, S.J.; Arun, R.; Bodrogi, A.; Lebel, D.E.; Magana, S.P.; Dear, T.E.; Witiw, C. The use of fusion mass screws in revision spinal deformity surgery. Eur. Spine J. 2014, 23, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Mittal, A.; Rosinski, A.; Odeh, K.; Balcescu, C.; Ungurean, V.; Ungurean, V.; Kondrashov, D.G. Fusion Mass Screws in Revision Spinal Deformity Surgery: A Simple and Safe Alternative Fixation. Int. J. Spine Surg. 2023, 17, 17–24. [Google Scholar] [CrossRef]
- Chan, C.Y.W.; Gani, S.M.A.; Chung, W.H.; Chiu, C.K.; Hasan, M.S.; Kwan, M.K. A Comparison Between the Perioperative Outcomes of Female Adolescent Idiopathic Scoliosis (AIS) Versus Adult Idiopathic Scoliosis (AdIS) Following Posterior Spinal Fusion: A Propensity Score Matching Analysis Involving 425 Patients. Glob. Spine J. 2023, 13, 81–88. [Google Scholar] [CrossRef]
- Lonner, B.S.; Ren, Y.; Bess, S.; Kelly, M.; Kim, H.J.; Yaszay, B.; Lafage, V.; Marks, M.; Miyanji, F.; Shaffrey, C.I.; et al. Surgery for the Adolescent Idiopathic Scoliosis Patients After Skeletal Maturity: Early Versus Late Surgery. Spine Deform. 2019, 7, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.-Q.; Zhao, Y.-F.; Bai, Y.-S.; Liu, K.P.G.; He, S.-S.; Wang, C.-F.; Zhang, J.-T.; Li, M. Factors affecting curve flexibility in skeletally immature and mature idiopathic scoliosis. J. Orthop. Sci. 2011, 16, 133–138. [Google Scholar] [CrossRef]
- Deviren, V.; Berven, S.; Kleinstueck, F.; Antinnes, J.; Smith, J.A.; Hu, S.S. Predictors of flexibility and pain patterns in thoracolumbar and lumbar idiopathic scoliosis. Spine 2002, 27, 2346–2349. [Google Scholar] [CrossRef]
- Bridwell, K.H.; Berven, S.; Glassman, S.; Hamill, C.; Horton, W.C., 3rd; Lenke, L.G.; Schwab, F.; Baldus, C.; Shainline, M. Is the SRS-22 instrument responsive to change in adult scoliosis patients having primary spinal deformity surgery? Spine 2007, 32, 2220–2225. [Google Scholar] [CrossRef]
- Silman, A.J.; O’Neill, T.W.; Cooper, C.; Kanis, J.; Felsenberg, D. Influence of physical activity on vertebral deformity in men and women: Results from the European Vertebral Osteoporosis Study. J. Bone Miner. Res. 1997, 12, 813–819. [Google Scholar] [CrossRef] [PubMed]
- Özyemişci Taşkıran, Ö. Rehabilitation in adult spinal deformity. Turk. J. Phys. Med. Rehabil. 2020, 66, 231–243. [Google Scholar] [CrossRef]
- Louie, P.K.; Iyer, S.; Khanna, K.; Harada, G.K.; Khalid, A.; Gupta, M.; Burton, D.; Shaffrey, C.; Lafage, R.; Lafage, V.; et al. Revision Strategies for Harrington Rod Instrumentation: Radiographic Outcomes and Complications. Glob. Spine J. 2022, 12, 654–662. [Google Scholar] [CrossRef]
- Jackson, T.J.; Hassan, F.M.; Weintraub, M.; Taha, O.; Elfilali, M.; Kulubya, E.; Lewerenz, E.; Reyes, J.L.; Sevensky, R.; Coury, J.R.; et al. Older adult idiopathic scoliosis patients have greater improvement in self-image compared to younger adult and adolescent idiopathic scoliosis patients following posterior spinal fusion. Spine Deform. 2025. [Google Scholar] [CrossRef] [PubMed]
- Kamata, Y.; Suzuki, S.; Takeda, K.; Iga, T.; Takahashi, Y.; Tsuji, O.; Nagoshi, N.; Matsumoto, M.; Nakamura, M.; Watanabe, K. Increased Surgical Invasiveness but Favorable Scoliosis Research Society-22 Scores in Adult Idiopathic Scoliosis with Major Thoracic Curves: A Comparative Study with Adolescent Idiopathic Scoliosis. Spine Surg. Relat. Res. 2025, 9, 453–459. [Google Scholar] [CrossRef]
- LaBarge, M.E.; Chanbour, H.; Waddell, W.H.; Vickery, J.; Jonzzon, S.; Roth, S.G.; Croft, A.J.; Abtahi, A.M.; Louer, C.R.; Martus, J.E.; et al. Clinical and radiographic outcomes following correction of idiopathic scoliosis in adolescence vs young adulthood. Spine Deform. 2023, 11, 1443–1451. [Google Scholar] [CrossRef] [PubMed]
- Ohashi, M.; Watanabe, K.; Hirano, T.; Hasegawa, K.; Tashi, H.; Minato, K.; Shibuya, Y.; Sato, M.; Kubota, M.; Sekimoto, H.; et al. Natural course of moderate adolescent idiopathic scoliosis: A mean 25-year follow-up study. Eur. Spine J. 2025. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Viroli, G.; Ruffilli, A.; Traversari, M.; Mazzotti, A.; Manzetti, M.; Zielli, S.O.; Arceri, A.; Faldini, C. Adolescent Idiopathic Scoliosis in the Adult Patient: New Classification with a Treatment-Oriented Guideline. Healthcare 2025, 13, 2418. https://doi.org/10.3390/healthcare13192418
Viroli G, Ruffilli A, Traversari M, Mazzotti A, Manzetti M, Zielli SO, Arceri A, Faldini C. Adolescent Idiopathic Scoliosis in the Adult Patient: New Classification with a Treatment-Oriented Guideline. Healthcare. 2025; 13(19):2418. https://doi.org/10.3390/healthcare13192418
Chicago/Turabian StyleViroli, Giovanni, Alberto Ruffilli, Matteo Traversari, Antonio Mazzotti, Marco Manzetti, Simone Ottavio Zielli, Alberto Arceri, and Cesare Faldini. 2025. "Adolescent Idiopathic Scoliosis in the Adult Patient: New Classification with a Treatment-Oriented Guideline" Healthcare 13, no. 19: 2418. https://doi.org/10.3390/healthcare13192418
APA StyleViroli, G., Ruffilli, A., Traversari, M., Mazzotti, A., Manzetti, M., Zielli, S. O., Arceri, A., & Faldini, C. (2025). Adolescent Idiopathic Scoliosis in the Adult Patient: New Classification with a Treatment-Oriented Guideline. Healthcare, 13(19), 2418. https://doi.org/10.3390/healthcare13192418








