Effects of Physical Activity on Executive Function and Emotional Regulation in Children and Adolescents with Neurodevelopmental Disorders: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Information Sources
2.2. Search Strategy
2.3. Inclusion Criteria
2.4. Exclusion Criteria
2.5. Study Selection Process
2.6. Data Extraction
2.7. Assessment of Methodological Quality
2.8. Analytical Decisions for Meta-Analysis
3. Results
3.1. Study Selection Process
3.2. Methodological Quality
3.3. Characteristics of the Studies
3.4. Study Results
3.5. Meta-Analysis
3.5.1. Subgroup Analysis
Executive Function
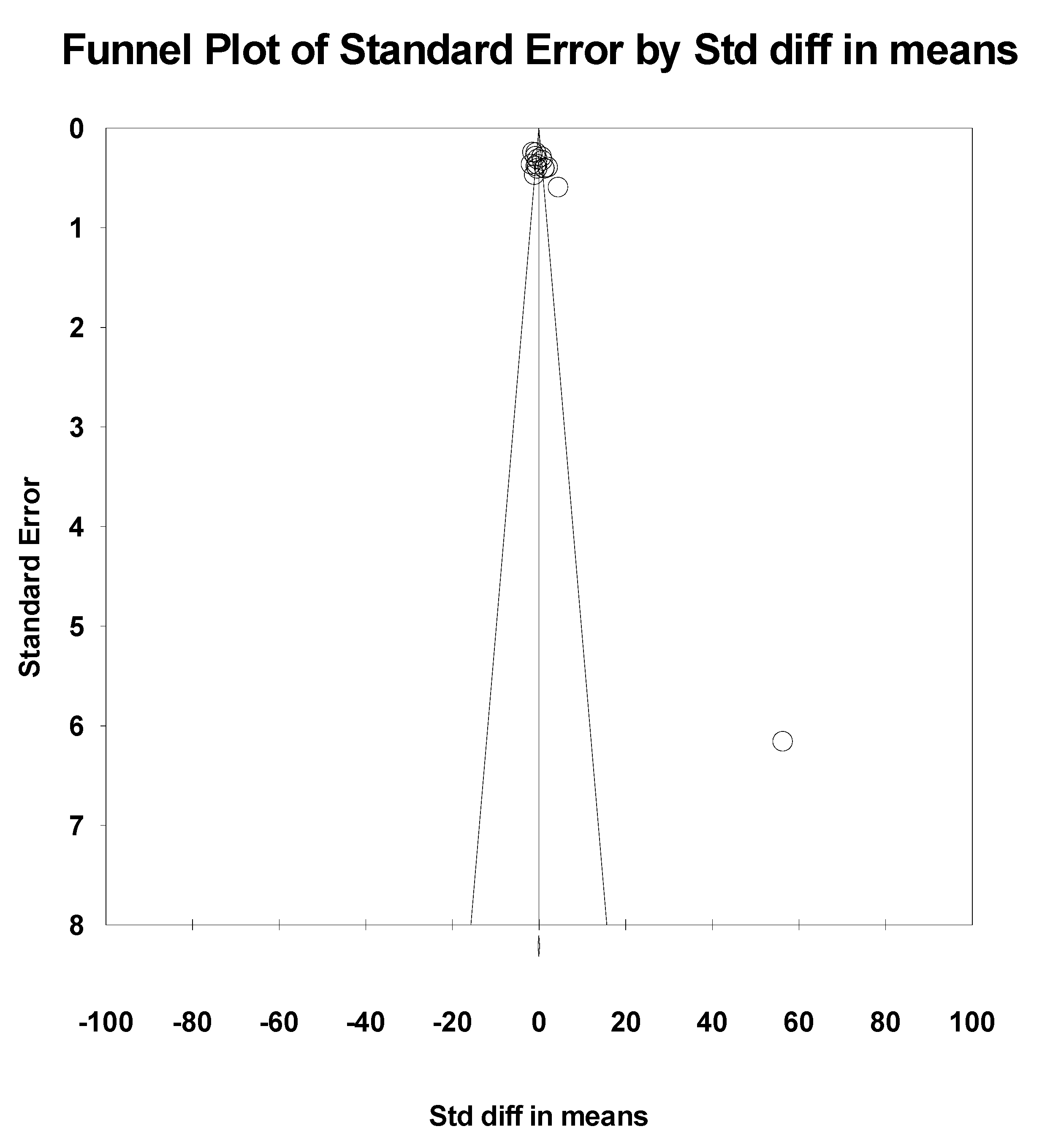
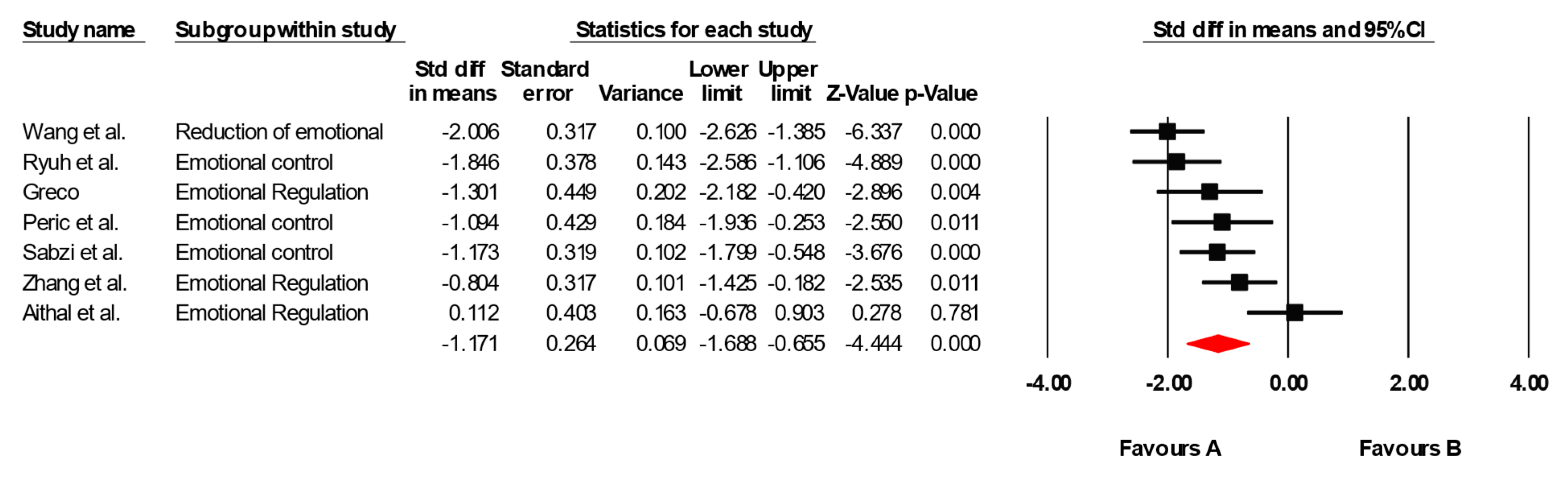
Emotional Regulation
Groups of Age
Total Training Duration
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| NDD | Neurodevelopmental disorder |
| ADHD | Attention-deficit/hyperactivity disorder |
| ASD | Autism spectrum disorder |
| ID | Intellectual disability |
| DCD | Developmental coordination disorder |
| PA | Physical Activity |
| RCTs | Randomized clinical trials |
| WOS | Web of Science |
| HPA | Hypothalamic–pituitary–adrenal |
References
- Centers for Disease Control and Prevention. Data and Statistics on Children’s Mental Health. 2023. Available online: https://www.cdc.gov/childrensmentalhealth/data.html (accessed on 3 November 2024).
- Boyle, C.A.; Boulet, S.; Schieve, L.A.; Cohen, R.A.; Blumberg, S.J.; Yeargin-Allsopp, M.; Visser, S.; Kogan, M.D. Trends in the prevalence of developmental disabilities in US children, 1997–2008. Pediatrics 2011, 127, 1034–1042. [Google Scholar] [CrossRef]
- Baio, J.; Wiggins, L.; Christensen, D.L.; Maenner, M.J.; Daniels, J.; Warren, Z.; Kurzius-Spencer, M.; Zahorodny, W.; Rosenberg, C.R.; White, T.; et al. Prevalence of Autism Spectrum Disorder Among Children Aged 8 Years-Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2016. Morb. Mortal. Wkly. Rep. (MMWR) 2020, 39, 1–12, Erratum in Morb. Mortal. Wkly. Rep. (MMWR) 2020, 69, 503. [Google Scholar] [CrossRef]
- Diamond, A.; Ling, D.S. Conclusions about Interventions, Programs, and Approaches for Improving Executive Functions That Appear Justified and Those That, Despite Much Hype, Do Not. Dev. Cogn. Neurosci. 2016, 18, 34–48. [Google Scholar] [CrossRef] [PubMed]
- Defayette, A.B.; Whitmyre, E.D.; Lopez, R.; Brown, B.; Wolff, J.C.; Spirito, A.; Esposito-Smythers, C. Adolescent depressed mood and difficulties with emotion regulation: Concurrent trajectories of change. J. Adolesc. 2021, 91, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Sciberras, E.; Mulraney, M.; Silva, D.; Coghill, D. Prenatal Risk Factors and the Etiology of ADHD—Review of Existing Evidence. Curr. Psychiatry Rep. 2017, 19, 1. [Google Scholar] [CrossRef] [PubMed]
- Shaw, P.; Stringaris, A.; Nigg, J.; Leibenluft, E. Emotion Dysregulation in Attention Deficit Hyperactivity Disorder. Am. J. Psychiatry 2014, 171, 276–293. [Google Scholar] [CrossRef]
- Starosta, J.; Izydorczyk, B.; Sitnik-Warchulska, K.; Lizińczyk, S. Impulsivity and Difficulties in Emotional Regulation as Predictors of Binge-Watching Behaviours. Front. Psychiatry 2021, 12, 743870. [Google Scholar] [CrossRef]
- Lord, C.; Elsabbagh, M.; Baird, G.; Veenstra-Vanderweele, J. Autism Spectrum Disorder. Lancet 2018, 392, 508–520. [Google Scholar] [CrossRef]
- Drechsler, R.; Brem, S.; Brandeis, D.; Grünblatt, E.; Berger, G.; Walitza, S. ADHD: Current Concepts and Treatments in Children and Adolescents. Neuropediatrics 2020, 51, 315–335. [Google Scholar] [CrossRef]
- Yang, G.; Liu, Q.; Wang, W.; Liu, W.; Li, J. Effect of Aerobic Exercise on the Improvement of Executive Function in Children with Attention Deficit Hyperactivity Disorder: A Systematic Review and Meta-Analysis. Front. Psychol. 2024, 15, 1376354. [Google Scholar] [CrossRef]
- Ziereis, S.; Jansen, P. Effects of Physical Activity on Executive Function and Motor Performance in Children with ADHD. Res. Dev. Disabil. 2015, 38, 181–191. [Google Scholar] [CrossRef]
- Best, J.R. Effects of Physical Activity on Children’s Executive Function: Contributions of Experimental Research on Aerobic Exercise. Dev. Rev. 2010, 30, 331–551. [Google Scholar] [CrossRef]
- de Bruijn, A.G.M.; Hartman, E.; Kostons, D.; Visscher, C.; Bosker, R.J. Exploring the Relations among Physical Fitness, Executive Functioning, and Low Academic Achievement. J. Exp. Child Psychol. 2018, 167, 204–221. [Google Scholar] [CrossRef]
- Egger, F.; Benzing, V.; Conzelmann, A.; Schmidt, M. Boost your brain, while having fun: A randomized controlled trial on the cognitive and academic benefits of combined physical and cognitive training in children. Front. Psychol. 2019, 10, 2020. [Google Scholar] [CrossRef]
- Martín-Rodríguez, A.; Gostian-Ropotin, L.A.; Beltrán-Velasco, A.I.; Belando-Pedreño, N.; Simón, J.A.; López-Mora, C.; Navarro-Jiménez, E.; Tornero-Aguilera, J.F.; Clemente-Suárez, V.J. Sporting Mind: The Interplay of Physical Activity and Psychological Health. Sports 2024, 12, 37. [Google Scholar] [CrossRef]
- Li, J.; Zhou, X.; Huang, Z.; Shao, T. Effect of exercise intervention on depression in children and adolescents: A systematic review and network meta-analysis. BMC Public Health 2023, 23, 1918. [Google Scholar] [CrossRef]
- Voss, M.W.; Vivar, C.; Kramer, A.F.; van Praag, H. Bridging Animal and Human Models of Exercise-Induced Brain Plasticity. Trends Cogn. Sci. 2013, 17, 525–544. [Google Scholar] [CrossRef] [PubMed]
- Miranda, M.; Morici, J.F.; Zanoni, M.B.; Bekinschtein, P. Brain-Derived Neurotrophic Factor: A Key Molecule for Memory in the Healthy and the Pathological Brain. Front. Cell. Neurosci. 2019, 13, 363. [Google Scholar] [CrossRef]
- Toader, C.; Serban, M.; Munteanu, O.; Covache-Busuioc, R.-A.; Enyedi, M.; Ciurea, A.V.; Tataru, C.P. From Synaptic Plasticity to Neurodegeneration: BDNF as a Transformative Target in Medicine. Int. J. Mol. Sci. 2025, 26, 4271. [Google Scholar] [CrossRef] [PubMed]
- Lerma-Castaño, P.R.; Roldán-González, E.; Robledo-Castro, C.; Hederich, C.; Garzón-Cadena, H.P.; Vargas, P.A.S.; Montenegro, L.C.G. Effects of Physical Exercise on Gross Motor Skills in Children with Autism Spectrum Disorder. J. Autism Dev. Disord. 2023, 54, 2816–2825. [Google Scholar] [CrossRef] [PubMed]
- Benzing, V.; Schmidt, M. The Effect of Exergaming on Executive Functions in Children with ADHD: A Randomized Clinical Trial. Scand. J. Med. Sci. Sports 2019, 29, 1243–1253. [Google Scholar] [CrossRef] [PubMed]
- Bosgraaf, L.; Spreen, M.; Pattiselanno, K.; van Hooren, S. Art Therapy for Psychosocial Problems in Children and Adolescents: A Systematic Narrative Review on Art Therapeutic Means and Forms of Expression, Therapist Behavior, and Supposed Mechanisms of Change. Front. Psychol. 2020, 11, 584685. [Google Scholar] [CrossRef]
- Cashin, A.G.; McAuley, J.H. Clinimetrics: Physiotherapy Evidence Database (PEDro) Scale. J. Physiother. 2020, 66, 59. [Google Scholar] [CrossRef] [PubMed]
- de Morton, N.A. The PEDro Scale Is a Valid Measure of the Methodological Quality of Clinical Trials: A Demographic Study. Aust. J. Physiother. 2009, 55, 129–133. [Google Scholar] [CrossRef]
- Chang, S.H.; Shie, J.J.; Yu, N.Y. Enhancing Executive Functions and Handwriting with a Concentrative Coordination Exercise in Children with ADHD: A Randomized Clinical Trial. Percept. Mot. Skills 2022, 129, 1014–1035. [Google Scholar] [CrossRef]
- Da Silva, L.A.D.; Doyenart, R.; Salvan, P.H.; Rodrigues, W.; Lopes, J.F.; Gomes, K.; Thirupathi, A.; De Pinho, R.A.; Silveira, P.C. Swimming Training Improves Mental Health Parameters, Cognition and Motor Coordination in Children with Attention Deficit Hyperactivity Disorder. Int. J. Environ. Health Res. 2020, 30, 584–592. [Google Scholar] [CrossRef]
- Liang, X.; Qiu, H.; Wang, P.; Sit, C.H.P. The Impacts of a Combined Exercise on Executive Function in Children with ADHD: A Randomized Controlled Trial. Scand. J. Med. Sci. Sports 2022, 32, 1297–1312. [Google Scholar] [CrossRef]
- Ludyga, S.; Muecke, M.; Leuenberger, R.; Bruggisser, F.; Pühse, U.; Gerber, M.; Capone-Mori, A.; Keutler, C.; Brotzmann, M.; Weber, P. Behavioral and Neurocognitive Effects of Judo Training on Working Memory Capacity in Children with ADHD: A Randomized Controlled Trial. Neuroimage Clin. 2022, 36, 103156. [Google Scholar] [CrossRef]
- Ji, C.; Yang, J.; Lin, L.; Chen, S. Executive Function Improvement for Children with Autism Spectrum Disorder: A Comparative Study Between Virtual Training and Physical Exercise Methods. Children 2022, 9, 507. [Google Scholar] [CrossRef]
- Mero Piedra, A.L.; Pesthy, O.; Marton, K. Effects of a Physical Education Intervention on Attention and Inhibitory Control in Ecuadorian Children with Intellectual Disabilities. J. Intellect. Disabil. 2024, 28, 261–274. [Google Scholar] [CrossRef] [PubMed]
- Damanpak, S.; Sabzi, A.H. The Effect of Selected Motor Games on Executive Functions of Children with Developmental Coordination Disorders. Int. J. Pediatr. 2022, 10, 15449–15459. [Google Scholar] [CrossRef]
- Wang, S. Yoga for Emotional Control in Children with ADHD. Rev. Bras. Med. Esporte 2023, 29, 1–4. [Google Scholar] [CrossRef]
- Ryuh, Y.; Choi, P.; Oh, J.; Chen, C.C.; Lee, Y. Impact of Inclusive Soccer Program on Psychosocial Development of Children with and without Intellectual Disabilities. J. Dev. Phys. Disabil. 2019, 31, 691–705. [Google Scholar] [CrossRef]
- Greco, G. Multilateral Training Using Physical Activity and Social Games Improves Motor Skills and Executive Function in Children with Autism Spectrum Disorder. Eur. J. Spec. Educ. Res. 2020, 5, 4. [Google Scholar] [CrossRef]
- Greco, G.; de Ronzi, R. Effect of Karate Training on Social, Emotional, and Executive Functioning in Children with Autism Spectrum Disorder. J. Phys. Educ. Sport 2020, 20, 1637–1645. [Google Scholar] [CrossRef]
- Hashemi, A.; Khodaverdi, Z.; Zamani, M.H. Effect of Wii Fit Training on Visual Perception and Executive Function in Boys with Developmental Coordination Disorders: A Randomized Controlled Trial. Res. Dev. Disabil. 2022, 124, 104196. [Google Scholar] [CrossRef]
- Ji, H.Q.; Wu, S.S.; Won, J.; Weng, S.; Lee, S.; Seo, S.; Park, J.-J. The Effects of Exergaming on Attention in Children with Attention Deficit/Hyperactivity Disorder: Randomized Controlled Trial. JMIR Serious Games 2023, 11, e40438. [Google Scholar] [CrossRef]
- Kadri, A.; Slimani, M.; Bragazzi, N.L.; Tod, D.; Azaiez, F. Effect of Taekwondo Practice on Cognitive Function in Adolescents with Attention Deficit Hyperactivity Disorder. Int. J. Environ. Res. Public Health 2019, 16, 204. [Google Scholar] [CrossRef]
- Rafiei Milajerdi, H.; Sheikh, M.; Najafabadi, G.G.; Saghaei, B.; Naghdi, N.; Dewey, D. The Effects of Physical Activity and Exergaming on Motor Skills and Executive Functions in Children with Autism Spectrum Disorder. Games Health J. 2021, 10, 33–42. [Google Scholar] [CrossRef] [PubMed]
- Sani, N.G.; Akbarfahimi, M.; Akbari, S.; Zarei, M.A.; Taghizadeh, G. Neurofeedback training versus perceptual-motor exercises interventions in visual attention for children with attention-deficit/hyperactivity disorder: A randomized controlled trial. Basic Clin. Neurosci. 2022, 13, 215–224. [Google Scholar] [CrossRef]
- Perić, D.B.; Milićević-Marinković, B.; Djurović, D. The Effect of the Adapted Soccer Programme on Motor Learning and Psychosocial Behaviour in Adolescents with Down Syndrome. J. Intellect. Disabil. Res. 2021, 65, 925–935. [Google Scholar] [CrossRef] [PubMed]
- Sabzi, A.H.; Dana, A.; Salehian, M.H.; Shaygan Yekta, H. The Effect of Water Treadmill Exercise on Children with Attention Deficit Hyperactivity Disorder. Int. J. Pediatr. 2021, 9, 13671–13681. [Google Scholar] [CrossRef]
- Zhang, Z.; Li, R.; Zhou, Z.; Wang, P.; Yang, B.; Wang, X. The Effect of Physical Activity on Quality of Life and Parenting Stress in Children with Attention-Deficit/Hyperactivity Disorder: A Randomized Controlled Trial. Disabil. Health J. 2023, 16, 101377. [Google Scholar] [CrossRef]
- Aithal, S.; Karkou, V.; Makris, S.; Karaminis, T.; Powell, J. A Dance Movement Psychotherapy Intervention for the Wellbeing of Children with an Autism Spectrum Disorder: A Pilot Intervention Study. Front. Psychol. 2021, 12, 588418. [Google Scholar] [CrossRef]
- Atak, E.; Hajebrahimi, F.; Algun, Z.C. The Effect of Dual-Task Balance Exercises on Cognitive Functions Among Children with Mild and Borderline Mental Retardation: A Randomized Controlled Trial. Eur. J. Physiother. 2022, 25, 324–332. [Google Scholar] [CrossRef]
- Huang, C.J.; Tu, H.Y.; Hsueh, M.C.; Chiu, Y.H.; Huang, M.Y.; Chou, C.C. Effects of Acute Aerobic Exercise on Executive Function in Children with and without Learning Disability: A Randomized Controlled Trial. Adapt. Phys. Activ. Q. 2020, 37, 404–422. [Google Scholar] [CrossRef]
- Álvarez-Bueno, C.; Pesce, C.; Cavero-Redondo, I.; Sánchez-López, M.; Garrido-Miguel, M.; Martínez-Vizcaíno, V. Academic Achievement and Physical Activity: A Meta-Analysis. Pediatrics 2017, 140, e20171498. [Google Scholar] [CrossRef]
- Walker, R.; House, D.; Kent-Saisch, S.; Porter, A.; Salway, R.; Emm-Collison, L.; Beets, M.; Lubans, D.R.; de Vocht, F.; Jago, R. Designing Context-Specific Physical Activity Interventions for English Primary Schools: Insights from a Four-Month Rapid Ethnography. BMC Public Health 2025, 25, 2497. [Google Scholar] [CrossRef]
- Wang, H.; Sun, X.; Chattopadhyay, K. Development of a School-Based Intervention to Increase Physical Activity Levels among Chinese Children: A Systematic Iterative Process Based on the Behavior Change Wheel and Theoretical Domains Framework. Front. Public Health 2021, 9, 610245. [Google Scholar] [CrossRef] [PubMed]
- Jiang, C.; Razak, N.A.; Rasyid, N.M.; Cheng, H. Investigating the Youth Physical Activity Promotion (YPAP) Model among Chinese Middle School Students. BMC Public Health 2025, 25, 1843. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Li, L.; He, X.; Wang, H. Mediating Roles of School Climate and Perceived Barriers in Physical Activity among Chinese Students. Risk Manag. Healthc. Policy 2024, 17, 3125–3136. [Google Scholar] [CrossRef]
- Hoy, S.; Jakobsson, B.T.; Lunde, C.; Larsson, H. Negotiating Adolescents’ Physically Active Life during the School Day: Opportunities and Barriers in Differing School Contexts. Front. Sports Act. Living 2025, 7, 1505189. [Google Scholar] [CrossRef]
- Rethinking Children’s Physical Activity Interventions at School: A New Context-Specific Approach. Res. Gate 2025. Available online: https://www.researchgate.net/publication/370426670 (accessed on 29 August 2025).
- Girotti, M.; Adler, S.M.; Bulin, S.E.; Fucich, E.A.; Paredes, D.; Morilak, D.A. Prefrontal Cortex Executive Processes Affected by Stress in Health and Disease. Prog. Neuropsychopharmacol. Biol. Psychiatry 2018, 85, 161–179. [Google Scholar] [CrossRef]
- Löytömäki, J.; Laakso, M.L.; Huttunen, K. Social-Emotional and Behavioural Difficulties in Children with Neurodevelopmental Disorders: Emotion Perception in Daily Life and in a Formal Assessment Context. J. Autism Dev. Disord. 2023, 53, 4744–4758. [Google Scholar] [CrossRef] [PubMed]
- Diamond, A.; Ling, D.S. Review: Can Physical Activity Improve Executive Function and Academic Achievement in Children? Trends Neurosci. Educ. 2019, 17, 100117. [Google Scholar] [CrossRef]
- de Almeida, A.A.; Noll, M. Physical Activity and Lifestyle Behaviors in Children and Adolescents. Children 2024, 11, 1403. [Google Scholar] [CrossRef]
- Hasan, A.M.R.; Rashid, H.; Smith, G.; Selim, M.A.; Rasheed, S.; Houghton, C. The Role of Aerobic Fitness in Cortical Thickness and Mathematics Achievement in Preadolescent Children. PLoS ONE 2020, 15, e0230321. [Google Scholar] [CrossRef]
- Ludyga, S.; Gerber, M.; Brand, S.; Holsboer-Trachsler, E.; Pühse, U. Acute Effects of Moderate Aerobic Exercise on Specific Aspects of Executive Function in Different Age and Fitness Groups: A Meta-Analysis. Psychophysiology 2020, 57, e13529. [Google Scholar] [CrossRef]
- Han, H.; Zhang, J.; Zhang, F.; Li, F.; Wu, Z. Optimal exercise interventions for enhancing cognitive function in older adults: A network meta-analysis. Front. Aging Neurosci. 2025, 17, 1510773. [Google Scholar] [CrossRef]
- Xue, Y.; Yang, Y.; Huang, T. Effects of chronic exercise interventions on executive function among children and ad-olescents: A systematic review with meta-analysis. Br. J. Sports Med. 2019, 53, 1397–1404. [Google Scholar] [CrossRef]
- Yang, S.; Jinj, L.; He, Q.; Wang, H. Fostering emotional well-being in adolescents: The role of physical activity, emotional intelligence, and interpersonal forgiveness. Fron. Psychol. 2024, 15, 140822. [Google Scholar] [CrossRef] [PubMed]
- Eisenberg, N.; Spinrad, T.L.; Eggum, N.D. Emotion-Related Self-Regulation and Its Relation to Children’s Maladjustment. Annu. Rev. Clin. Psychol. 2010, 6, 495–525. [Google Scholar] [CrossRef] [PubMed]
- Lubans, D.; Richards, J.; Hillman, C.; Faulkner, G.; Beauchamp, M.; Nilsson, M.; Kelly, P.; Smith, J.; Raine, L.; Biddle, S. Physical Activity for Cognitive and Mental Health in Youth: A Systematic Review of Mechanisms. Pediatrics 2016, 138, e20161642. [Google Scholar] [CrossRef] [PubMed]
- Mandolesi, L.; Polverino, A.; Montuori, S.; Foti, F.; Ferraioli, G.; Sorrentino, P.; Sorrentino, G. Effects of Physical Exercise on Cognitive Functioning and Wellbeing: Biological and Psychological Benefits. Front. Psychol. 2018, 9, 509. [Google Scholar] [CrossRef]
- Schuch, F.B.; Vancampfort, D.; Richards, J.; Rosenbaum, S.; Ward, P.B.; Stubbs, B. Exercise as a Treatment for Depression: A Meta-Analysis Adjusting for Publication Bias. J. Psychiatr. Res. 2016, 77, 42–51. [Google Scholar] [CrossRef]
- Pascoe, M.C.; Bailey, A.P.; Craike, M.; Carter, T.; Patten, R.; Stepto, N.; Parker, A. Physical Activity and Exercise in Youth Mental Health Promotion: A Scoping Review. BMJ Open Sport Exerc. Med. 2020, 6, e000677. [Google Scholar] [CrossRef]
- Biddle, S.J.H.; Ciaccioni, S.; Thomas, G.; Vergeer, I. Physical Activity and Mental Health in Children and Adolescents: An Updated Review of Reviews and an Analysis of Causality. Psychol. Sport Exerc. 2019, 42, 146–155. [Google Scholar] [CrossRef]




| Study | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chang et al. [26] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5/10 |
| Da Silva et al. [27] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4/10 |
| Liang et al. [28] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5/10 |
| Ludyga et al. [29] | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 7/10 |
| Ji et al. [30] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4/10 |
| Mero Piedra et al. [31] | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 4/10 |
| Damanpak & Sabzi [32] | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 5/10 |
| Wang et al. [33] | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 5/10 |
| Ryuh et al. [34] | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 5/10 |
| Greco [35] | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 5/10 |
| Greco & De Ronzi [36] | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 5/10 |
| Hashemi et al. [37] | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 5/10 |
| Ji et al. [38] | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 6/10 |
| Kadri et al. [39] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4/10 |
| Milajerdi et al. [40] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6/10 |
| Sani et al. [41] | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 5/10 |
| Perić et al. [42] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5/10 |
| Sabzi et al. [43] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 6/10 |
| Zhang et al. [44] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6/10 |
| Aithal et al. [45] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5/10 |
| Atak et al. [46] | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 6/10 |
| Huang et al. [47] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5/10 |
| Authors | Study Design/ Setting | Type of NDD; Diagnosed Methods | Age | Sample size (Exercise/ Control) | Type of Physical Activity | Session Duration, Frequency | Total Sessions, Total Duration | Outcomes and Measures | Results |
|---|---|---|---|---|---|---|---|---|---|
| Chang et al. [26] | RCT/School | ADHD; DSM-5 | 8.3 ± 1.3 | 40 (20/20) | Table tennis (CEE) | 60 min, 3x/week | 36 sessions, 2160 min | WCST, Stroop Word and Color Test | Cognitive flexibility and inhibitory control improved (p = 0.002 and p = 0.017) |
| Da Silva et al. [27] | RCT/University | ADHD; DSM-IV | 12.1 ± 1.6 | 20 (10/10) | Swimming | 45 min, 2x/week | 16 sessions, 720 min | Test of trails | Cognitive flexibility (p = 0.042) |
| Liang et al. [28] | RCT/Not reported | ADHD; DSM-5 | 8.5 ± 1.5 | 80 (40/40) | Combined exercise | 60 min, 3x/week | 36 sessions, 2160 min | Flanker, Tower of London, Trail Making Test | Improvements in working memory and cognitive flexibility (p < 0.01) |
| Ludyga et al. [29] | RCT/Not reported | ADHD; DSM-5 | 10.4 ± 13 | 41 (23/18) | Judo (CEE) | 60 min, 2x/week | 24 sessions, 1440 min | Change Detection paradigm | Working memory improved (K-score p = 0.030) |
| Ji et al. [30] | RCT/Not reported | ASD; ICD-10 | 12.8 ± 2.7 | 66 (33/33) | Physical exercise | 60 min, 3x/week | 27 sessions, 1620 min | Digit span, Flanker test, Stroop test | Improvements in memory and inhibition (p < 0.001) |
| Mero Piedra et al. [31] | RCT/Not reported | Intellectual disability; Clinically diagnosed | 12.7 ± 1.35 | 30 (15/15) | Physical education | 60 min, 2x/week | 12 sessions, 720 min | Executive function, Inhibition, Interference | No significant differences (p = 0.94, p = 0.13) |
| Damanpak & Sabzi [32] | RCT/Not reported | DCD; DCDQ | 10.7 ± 0.5 | 30 (15/15) | Motor games | 60 min, 3x/week | 24 sessions, 1440 min | Coolidge Executive Functioning Scale | Improvements in planning, organization, and inhibition (p = 0.001) |
| Wang et al. [33] | RCT/Not reported | ASD; DSM-5 | 7 ± 0.8 | 60 (30/30) | Sensory integration | 40 min, 2x/week | 16 sessions, 640 min | CBCL, PSQ, SSRS | Reduction in emotional and behavioral problems (p < 0.001) |
| Ryuh et al. [34] | RCT/Clinic | ADHD; DSM-5 | 10.8 ± 0.7 | 40 (20/20) | Educational games | 60 min, 2x/week | 16 sessions, 960 min | Stroop test, Emotional control scale | Improvements in emotional control and inhibitory control |
| Greco [35] | RCT/Clinical | ASD; ADOS-2 | 9.3 ± 0.92 | 24 (12/12) | Not reported | 70 min, 2x/week | 24 sessions, 1680 min | Behavior Rating Inventory of Executive Function | Improvements in emotional, cognitive, and behavioral regulation (p < 0.05) |
| Greco & De Ronzi [36] | RCT/Clinical | ASD; ADOS-2 | 9.1 ± 1.0 | 28 (14/14) | Karate training | 45 min, 2x/week | 24 sessions, 1080 min | EF: BRIEF | Significant improvements in executive functions |
| Hashemi et al. [37] | RCT/School | DCD; DSM-V | 9.6 ± 2.24 | 50 (25/25) | Usual care | 30 min, 3x/week | 24 sessions, 720 min | EF: CAS-planning, Attention: CAS-attention, Memory: TVPS-R | Improvements in attention, memory, and planning |
| Ji et al. [38] | RCT/Clinical | ADHD; Clinical diagnosis | 9.0 ± 1.5 | 42 (21/21) | Stationary bike exercise | 50 min, 3x/week | 12 sessions, 600 min | EF: GNG; Attention: FAIR | Improvements in sustained attention and inhibitory functions |
| Kadri et al. [39] | RCT/School | ADHD; Psychologist | 14.4 ± 3.22 | 40 (20/20) | Taekwondo Practice | 50 min, 2x/week | Approx. 144 sessions | EF: Stroop Task; Attention: Ruff 2 and 7 | Improvements in selective attention and inhibitory control |
| Milajerdi et al. [40] | RCT/School | ASD; ADOS-2 | 8.2 ± 1.5 | 40 (20/20) | Exergaming | 35 min, 3x/week | 24 sessions, 840 min | EF: WCST | Improvements in cognitive flexibility |
| Sani et al. [41] | RCT/Clinical | ADHD; DSM-V | 7.5 ± 1.3 | 25/25 | Neurofeedback | ≈42 min, 3x/week | 20 sessions, ~840 min | Attention: CPT | Significant improvements in sustained care |
| Perić et al. [42] | RCT | ID; WISC | 15.7 ± 0.5 | 25 (12/13) | No PA | 60 min, 2x/week | 32 sessions, 1920 min | Psychosocial variables assessment | Significant reduction in aggression, anxiety, and depression (p < 0.05) |
| Sabzi et al. [43] | RCT/ NR | ADHD; CPRS-R | 9.5 ± 0.5 | 46(23/23) | Water treadmill | 30 min/session, 3 times/week | 24 sessions, 720 min | Conduct problems, Anxiety: Conner’s Parent Rating Scale—Revised | Externalizing problems Conduct problems (p = 0.003) Internalizing problems Anxiety (p = 0.017) |
| Zhang et al. [44] | RCT/ Clinical | ADHD; DSM-5 | 8.8 ± 1.42 | 43(22/21) | Motor skills training | 60 min/session, 3 times/week | 36 sessions, 2160 min | Quality of life: Pediatric Quality of Life Inventory | Psychological well-being Quality of life (p = 0.046) |
| Aithal et al. [45] | RCT/ NR | ASD; DSM-5 | 10.7 ± 1.25 | 26(10/16) | Dance movement | 40 min/session, twice/week | 10 sessions, 400 min | Emotional and social well-being: Strengths and Difficulties Questionnaire | Psychological well-being Emotional and social well-being (p = 0.02) |
| Atak et al. [46] | RCT/ NR | ID; WISC-R | 8.7 ± 1.6 | 30(15/15) | Balance training | 30 min/session, twice/week | 24 sessions, 720 min | Attention, impulsivity: MOXO attention scale | Cognitive function Attention (p = 0.001) Externalizing problems Impulsivity (p = 0.003) |
| Huang et al. [47] | RCT/ School | LD; DSM-4 | 12 ± 0.81 | 51(25/26) | Acute aerobic exercise | 30 min/session | 1 session, 30 min | Sustained attention: sustained attention test | Cognitive function Sustained attention (p < 0.05) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carcelén-Fraile, M.d.C.; Hita-Contreras, F.; Mesas-Aróstegui, M.A.; Aibar-Almazán, A. Effects of Physical Activity on Executive Function and Emotional Regulation in Children and Adolescents with Neurodevelopmental Disorders: A Systematic Review and Meta-Analysis. Healthcare 2025, 13, 2415. https://doi.org/10.3390/healthcare13192415
Carcelén-Fraile MdC, Hita-Contreras F, Mesas-Aróstegui MA, Aibar-Almazán A. Effects of Physical Activity on Executive Function and Emotional Regulation in Children and Adolescents with Neurodevelopmental Disorders: A Systematic Review and Meta-Analysis. Healthcare. 2025; 13(19):2415. https://doi.org/10.3390/healthcare13192415
Chicago/Turabian StyleCarcelén-Fraile, María del Carmen, Fidel Hita-Contreras, María Aurora Mesas-Aróstegui, and Agustín Aibar-Almazán. 2025. "Effects of Physical Activity on Executive Function and Emotional Regulation in Children and Adolescents with Neurodevelopmental Disorders: A Systematic Review and Meta-Analysis" Healthcare 13, no. 19: 2415. https://doi.org/10.3390/healthcare13192415
APA StyleCarcelén-Fraile, M. d. C., Hita-Contreras, F., Mesas-Aróstegui, M. A., & Aibar-Almazán, A. (2025). Effects of Physical Activity on Executive Function and Emotional Regulation in Children and Adolescents with Neurodevelopmental Disorders: A Systematic Review and Meta-Analysis. Healthcare, 13(19), 2415. https://doi.org/10.3390/healthcare13192415


_MD__MPH_PhD.png)





