A Survey on Digital Solutions for Health Services Management: Features and Use Cases from Brazilian National Literature
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Database and Search Strategy
2.3. Study Selection
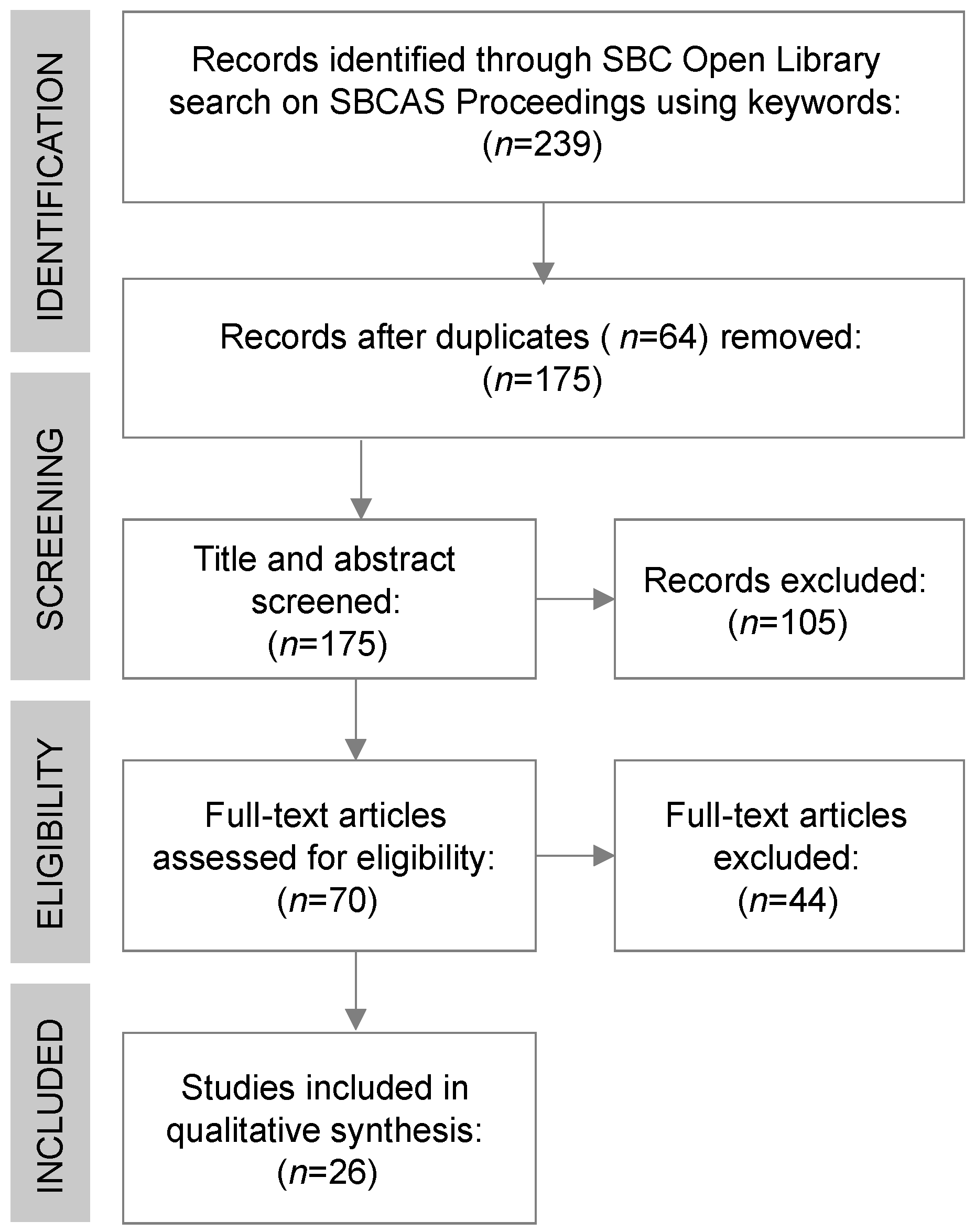
- Identification and Duplicate Removal: The search string was executed on the SOL database; duplicate studies were identified and removed.
- Title and Abstract Screening: Titles and abstracts identified through the search strategy were reviewed with a preliminary examination to determine whether they were related to the aim of this review.
- Full-Text Assessment: Potentially relevant studies determined to be eligible based on the title or abstract were retrieved and evaluated with a full-text reading to settle their adequacy to the eligibility criteria.
2.4. Eligibility Criteria
- Target Audience: Includes features that primarily benefit health managers or policymakers as the intended users of the described technology.
- Technological Focus: Centers around technology-based decision-support tools, software systems, analytical methods, or algorithms applied to healthcare management.
- Application Context: Provides insights into real-world applications, specific use cases, implementation contexts, or deployments within health services.
- Scope of Analysis: Offers information on the features, implementation challenges, or implications of the technologies within health systems management.
- Patient or Clinical Focus: Primarily targets individual patients or clinical practitioners, rather than adopting a managerial, population, panel, or collective focus.
- Lack of Real-World Application: Consists solely of theoretical proposals or descriptions without links to practical application or case studies.
- Non-Technological Tools: Focuses exclusively on organizational policies, process redesign, or intervention programs that do not involve a specific technological tool or system as a core component.
2.5. Data Extraction and Synthesis
- Article Metadata: The publication year, primary authors, and study location/context.
- Technological Characteristics: The specific type and name of the software, platform, algorithm, model, or method used or developed.
- Application Domain: The specific area within the health system (e.g., primary care, hospital administration, epidemiological surveillance, and outbreak prediction).
- Key Factors Considered: The main variables, indicators, criteria, or features central to the analysis, prediction, evaluation, or decision support.
- Implications for Practice: Reported or suggested impacts, recommendations, or potential benefits for health management practice, service delivery, or health policy.
3. Results
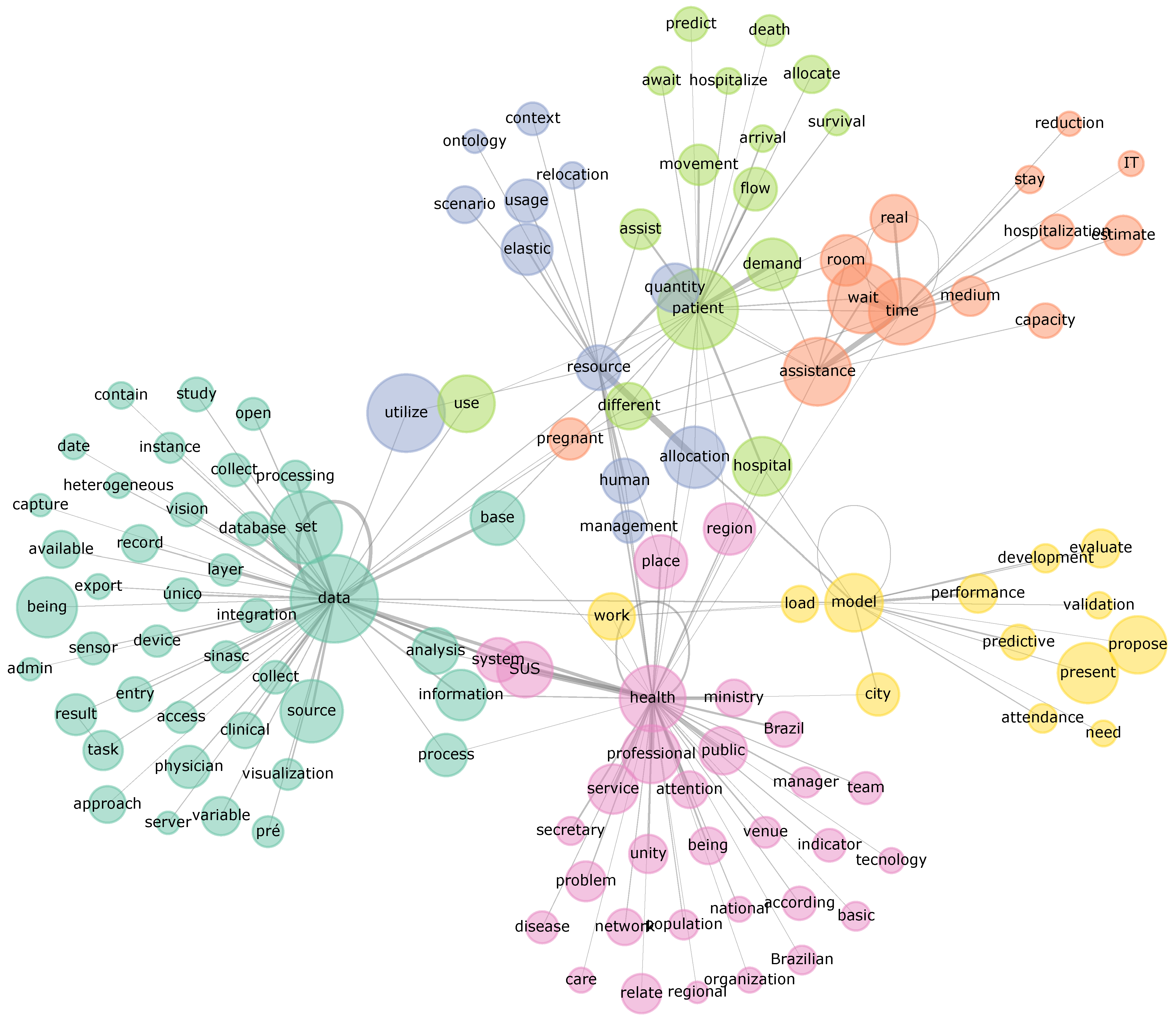
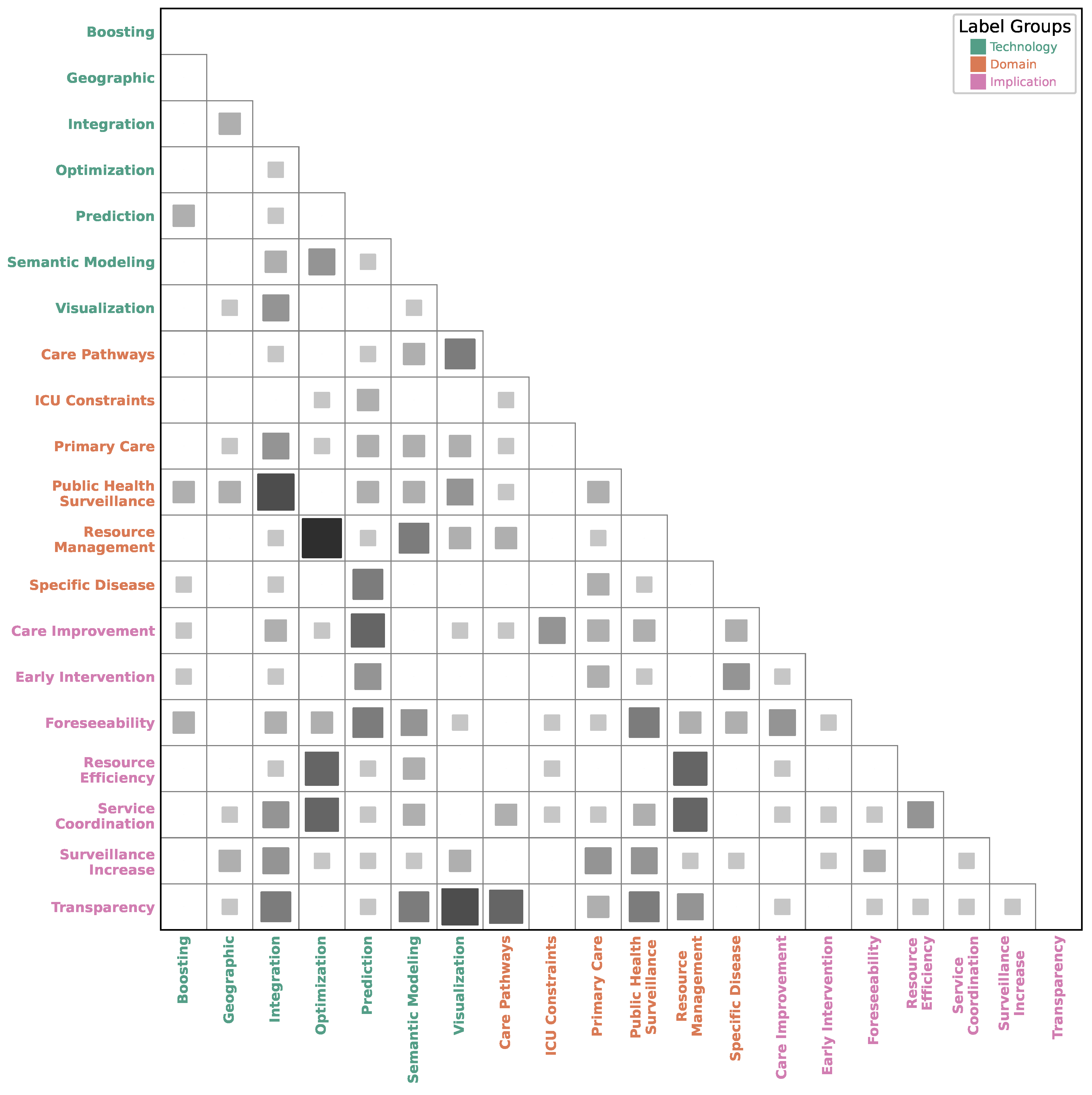
3.1. Application Domains
3.2. Technological Approaches
3.3. Maturity and Implications
4. Discussion
4.1. AI and Machine Learning Applications
4.2. Optimizing Hospital Operations
4.3. Public Health Surveillance and Primary Care
4.4. Strategic Planning and Resource Allocation
4.5. Data Integration and Semantic Technologies
4.6. Maturity, Readiness, and Barriers to Real-World Implementation
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AI | Artificial Intelligence |
| BPMN | Business Process Model and Notation |
| DHIS2 | District Health Information System 2 |
| CNN | Convolutional neural network |
| FHS | Family Health Strategy (primary care program) |
| HL7-FHIR | HL7 Fast Healthcare Interoperability Resources |
| ICU | Intensive Care Unit |
| OSF | Open Science Framework |
| SBC | Brazilian Computer Society |
| SBCAS | Brazilian Symposium on Computing Applied to Health |
| SUS | Unified Health System (of Brazil) |
| TRL | Technology Readiness Level |
| WHO | World Health Organization |
References
- Greenhalgh, T.; Papoutsi, C. Studying complexity in health services research: Desperately seeking an overdue paradigm shift. BMC Med. 2018, 16, 95. [Google Scholar] [CrossRef]
- Wehrmeister, F.C.; Wendt, A.T.; Sardinha, L.M. Inequalities and Chronic Non-Communicable Diseases in Brazil. Epidemiologia Serviços Saúde 2022, 31. [Google Scholar] [CrossRef]
- Rocha, T.A.H.; da Silva, N.C.; Amaral, P.V.; Barbosa, A.C.Q.; Rocha, J.V.M.; Alvares, V.; de Almeida, D.G.; Thumé, E.; Thomaz, E.B.A.F.; de Sousa Queiroz, R.C.; et al. Addressing geographic access barriers to emergency care services: A national ecologic study of hospitals in Brazil. Int. J. Equity Health 2017, 16, 149. [Google Scholar] [CrossRef] [PubMed]
- Vărzaru, A.A. Assessing the Relationships of Expenditure and Health Outcomes in Healthcare Systems: A System Design Approach. Healthcare 2025, 13, 352. [Google Scholar] [CrossRef] [PubMed]
- Flokou, A.; Aletras, V.H.; Miltiadis, C.; Karaferis, D.C.; Niakas, D.A. Efficiency of Primary Health Services in the Greek Public Sector: Evidence from Bootstrapped DEA/FDH Estimators. Healthcare 2024, 12, 2230. [Google Scholar] [CrossRef]
- Ford, G.; Compton, M.; Millett, G.; Tzortzis, A. The Role of Digital Disruption in Healthcare Service Innovation. In Service Business Model Innovation in Healthcare and Hospital Management; Springer International Publishing: Berlin/Heidelberg, Germany, 2016; pp. 57–70. [Google Scholar] [CrossRef]
- Coates, A.; Chung, A.Q.; Lessard, L.; Grudniewicz, A.; Espadero, C.; Gheidar, Y.; Bemgal, S.; Da Silva, E.; Sauré, A.; King, J.; et al. The use and role of digital technology in learning health systems: A scoping review. Int. J. Med. Inform. 2023, 178, 105196. [Google Scholar] [CrossRef]
- Bellei, E.A.; De Marchi, A.C.B. Championing health systems management with digital innovation and applications in the age of artificial intelligence: Protocol for a research program. F1000Research 2024, 13, 741. [Google Scholar] [CrossRef]
- Bradley, E.H.; Taylor, L.A.; Cuellar, C.J. Management Matters: A Leverage Point for Health Systems Strengthening in Global Health. Int. J. Health Policy Manag. 2015, 4, 411–415. [Google Scholar] [CrossRef]
- Stoumpos, A.I.; Talias, M.A.; Ntais, C.; Kitsios, F.; Jakovljevic, M. Knowledge Management and Digital Innovation in Healthcare: A Bibliometric Analysis. Healthcare 2024, 12, 2525. [Google Scholar] [CrossRef]
- Veras, R.d.M.S. Simpósio Brasileiro de Computação Aplicada à Saúde—SBCAS. J. Health Inform. 2022, 14. [Google Scholar]
- Veras, R.d.M.S. Brazilian Symposium on Computing Applied to Healthcare (SBCAS). Comput. Methods Biomech. Biomed. Eng. Imaging Vis. 2023, 11, 287. [Google Scholar] [CrossRef]
- Simon, H.A. Reason in Human Affairs; Stanford University Press: Redwood City, CA, USA, 1990. [Google Scholar]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Bellei, E.A.; Fernandes, R.V.; De Marchi, A.C.B. Technologies and decision-support tools for health systems management: A scoping review of features and use cases. Expert Rev. Pharmacoeconomics Outcomes Res. 2024, 25, 297–305. [Google Scholar] [CrossRef]
- Carvalho, P.; Da Conceição, F.; Barreto, J. Malha Digital dos Territórios da Estratégia Saúde da Família do Município de Castanhal—PA. In Proceedings of the Anais do XV Workshop de Informática Médica; Brazilian Computer Society: Porto Alegre, Brazil, 2015; pp. 229–232. [Google Scholar] [CrossRef]
- Inácio, A.; Savaris, A.; Alves, J.; von Wangenheim, A. Sistema Integrado de Análise e Visualização Epidemiológica Georreferenciada Online para Telemedicina. In Proceedings of the Anais do XVI Workshop de Informática Médica; Brazilian Computer Society: Porto Alegre, Brazil, 2016; pp. 2547–2556. [Google Scholar] [CrossRef][Green Version]
- Redeker, G.A.; Webber, T.; Czekster, R.M.; Quickert, S.; Bowles, J.K.F. Estimating capacity and resource allocation in healthcare settings using business process modelling and simulation. In Proceedings of the Anais do XVII Workshop de Informática Médica; Brazilian Computer Society: Porto Alegre, Brazil, 2017; pp. 1979–1982. [Google Scholar] [CrossRef]
- Jasmim, L.d.O.; Ziviani, A.; Ito, M.; Paiva, P.B. Caracterização de Atendimentos em uma Rede de Atenção à Saúde. In Proceedings of the Anais do XVII Workshop de Informática Médica; Brazilian Computer Society: Porto Alegre, Brazil, 2017; pp. 2044–2047. [Google Scholar] [CrossRef]
- Oliveira, L.B.; Lima, R.; Santos, D.F.S.; Barbosa, P.E.S.; Matos, F. Uma Abordagem SDN para Priorização de Tráfego em Ambientes Hospitalares Inteligentes. In Proceedings of the Anais do XVIII Simpósio Brasileiro de Computação Aplicada à Saúde; Brazilian Computer Society: Porto Alegre, Brazil, 2018. [Google Scholar] [CrossRef]
- Vargas, R.; Webber, T.; Czekster, R.; Berardi, R.G. Análise do processo de faturamento de contas de internação hospitalar combinando BPMN e Simulação. In Proceedings of the Anais do XVIII Simpósio Brasileiro de Computação Aplicada à Saúde; Brazilian Computer Society: Porto Alegre, Brazil, 2018. [Google Scholar] [CrossRef]
- Schmidt, D.; Da Silva, D.B.; Da Costa, C.A.; Righi, R.d.R. Um Modelo de Predição de Mortalidade em Unidades de Terapia Intensiva Baseado em Deep Learning. In Proceedings of the Anais do XVIII Simpósio Brasileiro de Computação Aplicada à Saúde; Brazilian Computer Society: Porto Alegre, Brazil, 2018. [Google Scholar] [CrossRef]
- Veras, N.D.L.; Viana, W.; Da Silva, M.L.; Júnior, E.B.S. Balanceamento Automático de Metas para Estabilização de Indicadores de Saúde na Atenção Básica. In Proceedings of the Anais do XIX Simpósio Brasileiro de Computação Aplicada à Saúde; Brazilian Computer Society: Porto Alegre, Brazil, 2019; pp. 175–186. [Google Scholar] [CrossRef]
- Ferré, F.; De Oliveira, G.; De Queiroz, M.; Gonçalves, F. Sala de Situação aberta com dados administrativos para gestão de Protocolos Clínicos e Diretrizes Terapêuticas de tecnologias providas pelo SUS. In Proceedings of the Anais do XX Simpósio Brasileiro de Computação Aplicada à Saúde; Brazilian Computer Society: Porto Alegre, Brazil, 2020; pp. 392–403. [Google Scholar] [CrossRef]
- Rolim, T.; Avila, C.; Arruda, N.; Silva, J.; Maia, J.; Oliveira, M.; Andrade, L.; Vidal, V. Um Enfoque Incremental para Construção do Grafo de Conhecimento do SUS. In Proceedings of the Anais do XX Simpósio Brasileiro de Computação Aplicada à Saúde; Brazilian Computer Society: Porto Alegre, Brazil, 2020; pp. 72–83. [Google Scholar] [CrossRef]
- Fischer, G.; Costa, C.; Righi, R. Usando IoT e Conceitos de Elasticidade em Cloud para Análise de Recursos Humanos em Hospitais Inteligentes. In Proceedings of the Anais do XX Simpósio Brasileiro de Computação Aplicada à Saúde; Brazilian Computer Society: Porto Alegre, Brazil, 2020; pp. 226–237. [Google Scholar] [CrossRef]
- Silva, M.; Santos, N.; Rosa, C.; Santos, M.; Ito, M.; Vieira, A.; Ziviani, A.; Oliveira, R. Análise dos Atendimentos de Gestantes na Rede de Atenção Básica de Saúde no Município de São Paulo. In Proceedings of the Anais do XX Simpósio Brasileiro de Computação Aplicada à Saúde; Brazilian Computer Society: Porto Alegre, Brazil, 2020; pp. 250–261. [Google Scholar] [CrossRef]
- Moreira, J.R.H.; Bernardino, H.S.; Barbosa, H.J.C.; Vieira, A.B. Modelos de Aprendizado de Máquina na Predição de Diabetes Tipo 1 na Gestação usando Dados do Sistema Único de Saúde. In Proceedings of the Anais do XXI Simpósio Brasileiro de Computação Aplicada à Saúde; Brazilian Computer Society: Porto Alegre, Brazil, 2021; pp. 392–403. [Google Scholar] [CrossRef]
- Gomes, N.B.P.; Franco, S.d.C.; Salvador, L.d.N. ONTOVID—Uma Abordagem para Construção de Grafos de Conhecimento Semântico com Enfoque em Notificações e Óbitos Relacionados ao Novo Coronavírus (COVID-19). In Proceedings of the Anais do XXII Simpósio Brasileiro de Computação Aplicada à Saúde; Brazilian Computer Society: Porto Alegre, Brazil, 2022; pp. 425–436. [Google Scholar] [CrossRef]
- Rodrigues, G.; Kreutz, D. Modelo preditivo para classificação de risco de óbito de pacientes com COVID-19 utilizando dados abertos. In Proceedings of the Anais do XXII Simpósio Brasileiro de Computação Aplicada à Saúde; Brazilian Computer Society: Porto Alegre, Brazil, 2022; pp. 144–155. [Google Scholar] [CrossRef]
- Moreira, J.R.H.; Bernardino, H.S.; Vieira, A.B. Predição de Óbito Neonatal usando Dados dos Sistemas de Informação do SUS e de Censo Demográfico. In Proceedings of the Anais do XXII Simpósio Brasileiro de Computação Aplicada à Saúde; Brazilian Computer Society: Porto Alegre, Brazil, 2022; pp. 234–245. [Google Scholar] [CrossRef]
- Pereira, G.R.; Costa, L.d.F.; Kon, F. Análise e visualização do processo de regionalização do Sistema Único de Saúde (SUS): Uma perspectiva em sistemas complexos. In Proceedings of the Anais Estendidos do XXIII Simpósio Brasileiro de Computação Aplicada à Saúde; Brazilian Computer Society: Porto Alegre, Brazil, 2023; pp. 84–89. [Google Scholar] [CrossRef]
- Aleixo, R.; Kon, F.; Camargo, R.Y.d. Predição de Surtos de Dengue e Diagnóstico de Sífilis Congênita Utilizando Aprendizado de Máquina. In Proceedings of the Anais Estendidos do XXIII Simpósio Brasileiro de Computação Aplicada à Saúde; Brazilian Computer Society: Porto Alegre, Brazil, 2023; pp. 96–101. [Google Scholar] [CrossRef]
- Cid, L.M.; San Felice, M.C.; Hokama, P.H.D.B. Uma Abordagem Multiobjetivo para o Problema do Escalonamento de Médicos. In Proceedings of the Anais do XXIII Simpósio Brasileiro de Computação Aplicada à Saúde; Brazilian Computer Society: Porto Alegre, Brazil, 2023; pp. 372–383. [Google Scholar] [CrossRef]
- Gregório, I.O.; Garcés, L.; Almeida, A. Proposta de uma aplicação para apoiar a gestão dos programas de controle endêmico na cidade de Itajubá. In Proceedings of the Anais Estendidos do XXIII Simpósio Brasileiro de Computação Aplicada à Saúde; Brazilian Computer Society: Porto Alegre, Brazil, 2023; pp. 205–210. [Google Scholar] [CrossRef]
- Fischer, G.S.; Costa, C.A.d.; Righi, R.d.R. Usando Dados de Sinais Vitais dos Cidadãos e a Técnica de Elasticidade para gerência de Hospitais no Contexto de Cidades Inteligentes. In Proceedings of the Anais do XXIII Simpósio Brasileiro de Computação Aplicada à Saúde; Brazilian Computer Society: Porto Alegre, Brazil, 2023; pp. 268–279. [Google Scholar] [CrossRef]
- Teixeira, I.V.; Endo, P.T. Predição de casos de sífilis congênita: Uma avaliação de desempenho de diferentes modelos de aprendizado de máquina. In Proceedings of the Anais Estendidos do XXIII Simpósio Brasileiro de Computação Aplicada à Saúde; Brazilian Computer Society: Porto Alegre, Brazil, 2023; pp. 120–125. [Google Scholar] [CrossRef]
- Alencar, M.A.d.S.; Correa, N.C.C.; Souza, S.E. Telemonitoramento de Agravos como Estratégia na Atenção Primária à Saúde. In Proceedings of the Anais do XXIV Simpósio Brasileiro de Computação Aplicada à Saúde; Brazilian Computer Society: Porto Alegre, Brazil, 2024; pp. 639–644. [Google Scholar] [CrossRef]
- Fischer, G.S.; Righi, R.d.R.; Costa, C.A.d.; Roehrs, A. Combinando Elasticidade Proativa e Reativa para Gestão Multi-Hospitalar de Recursos Humanos no Contexto das Cidades Inteligentes. In Proceedings of the Anais do XXIV Simpósio Brasileiro de Computação Aplicada à Saúde; Brazilian Computer Society: Porto Alegre, Brazil, 2024; pp. 249–260. [Google Scholar] [CrossRef]
- Gomes, C.E.V.; Clímaco, G.; Carvalho, J.A.F.N.d.; Quintanilha, D.B.P. Modelagem Matemática para a Alocação de Leitos de UTI com Diferentes Tipos de Leitos e Taxa de Ocupação. In Proceedings of the Anais do XXIV Simpósio Brasileiro de Computação Aplicada à Saúde; Brazilian Computer Society: Porto Alegre, Brazil, 2024; pp. 226–237. [Google Scholar] [CrossRef]
- Consoli, B.; Viera, R.; Bordini, R.H.; Manssour, I.H. Predicting Inpatient Admissions in Brazilian Hospitals. In Proceedings of the Anais do XXIV Simpósio Brasileiro de Computação Aplicada à Saúde; Brazilian Computer Society: Porto Alegre, Brazil, 2024; pp. 284–295. [Google Scholar] [CrossRef]
- Babayoff, O.; Shehory, O.; Geller, S.; Shitrit-Niselbaum, C.; Weiss-Meilik, A.; Sprecher, E. Improving Hospital Outpatient Clinics Appointment Schedules by Prediction Models. J. Med. Syst. 2022, 47, 5. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Liu, X.; Xie, X.; Li, L. Robust Elective Hospital Admissions With Contextual Information. IEEE Trans. Autom. Sci. Eng. 2024, 21, 5402–5420. [Google Scholar] [CrossRef]
- Santamato, V.; Tricase, C.; Faccilongo, N.; Iacoviello, M.; Marengo, A. Exploring the Impact of Artificial Intelligence on Healthcare Management: A Combined Systematic Review and Machine-Learning Approach. Appl. Sci. 2024, 14, 10144. [Google Scholar] [CrossRef]
- Bellei, E.A.; Domenighi, P.R.; Freitas, C.M.D.S.; De Marchi, A.C.B. Digital Solutions for Health Services and Systems Management: Narrative Review of Certified Software Features in the Brazilian Market. JMIR Med. Inform. 2024, 12, e65281. [Google Scholar] [CrossRef]
- World Health Organization. Global Strategy on Digital Health 2020–2025; World Health Organization: Genève, Switzerland, 2021. [Google Scholar]
- Lopes, J.; Guimarães, T.; Duarte, J.; Santos, M. Enhancing Surgery Scheduling in Health Care Settings With Metaheuristic Optimization Models: Algorithm Validation Study. JMIR Med. Inform. 2025, 13, e57231. [Google Scholar] [CrossRef]
- Bin Abdul Baten, R. How are US hospitals adopting artificial intelligence? Early evidence from 2022. Health Aff. Sch. 2024, 2, qxae123. [Google Scholar] [CrossRef]
- Kostkova, P.; Saigí-Rubió, F.; Eguia, H.; Borbolla, D.; Verschuuren, M.; Hamilton, C.; Azzopardi-Muscat, N.; Novillo-Ortiz, D. Data and Digital Solutions to Support Surveillance Strategies in the Context of the COVID-19 Pandemic. Front. Digit. Health 2021, 3, 707902. [Google Scholar] [CrossRef]
- Shaw, N.; McGuire, S. Understanding the use of geographical information systems (GISs) in health informatics research: A review. BMJ Health Care Inform. 2017, 24, 228–233. [Google Scholar] [CrossRef]
- Olawade, D.B.; Wada, O.J.; David-Olawade, A.C.; Kunonga, E.; Abaire, O.; Ling, J. Using artificial intelligence to improve public health: A narrative review. Front. Public Health 2023, 11, 1196397. [Google Scholar] [CrossRef] [PubMed]
- Silva, I.d.S.; Silva, C.R.D.V.; Martiniano, C.S.; Araújo, A.J.d.; Figueiredo, R.C.d.; Lapão, L.V.; Moioli, R.C.; Brito, E.W.G.; Uchoa, S.A.d.C. Digital health and quality of care in Primary Health Care: An evaluation model. Front. Public Health 2024, 12, 1443862. [Google Scholar] [CrossRef] [PubMed]
- Dolcini, M.; Borghi, S.; Rossitti, M.; Brambilla, A.; Mangili, S.; Torrieri, F.; Capolongo, S. Facility Management Costs for Hospital Infrastructures: Insights from the Italian Healthcare System. Healthcare 2025, 13, 924. [Google Scholar] [CrossRef]
- Dehnavieh, R.; Haghdoost, A.; Khosravi, A.; Hoseinabadi, F.; Rahimi, H.; Poursheikhali, A.; Khajehpour, N.; Khajeh, Z.; Mirshekari, N.; Hasani, M.; et al. The District Health Information System (DHIS2): A literature review and meta-synthesis of its strengths and operational challenges based on the experiences of 11 countries. Health Inf. Manag. J. 2018, 48, 62–75. [Google Scholar] [CrossRef]
- Zhang, H.; Lyu, T.; Yin, P.; Bost, S.; He, X.; Guo, Y.; Prosperi, M.; Hogan, W.R.; Bian, J. A scoping review of semantic integration of health data and information. Int. J. Med. Inform. 2022, 165, 104834. [Google Scholar] [CrossRef]
- Gøeg, K.R.; Rasmussen, R.K.; Jensen, L.; Wollesen, C.M.; Larsen, S.; Pape-Haugaard, L.B. A future-proof architecture for telemedicine using loose-coupled modules and HL7 FHIR. Comput. Methods Programs Biomed. 2018, 160, 95–101. [Google Scholar] [CrossRef]
- Amar, F.; April, A.; Abran, A. Electronic Health Record and Semantic Issues Using Fast Healthcare Interoperability Resources: Systematic Mapping Review. J. Med. Internet Res. 2024, 26, e45209. [Google Scholar] [CrossRef]
- Fernandez, M.; Pinto, H.A.; Fernandes, L.M.M.; Oliveira, J.A.S.d.; Lima, A.M.F.d.S.; Santana, J.S.S.; Chioro, A. Interoperability in universal healthcare systems: Insights from Brazil’s experience integrating primary and hospital health care data. Front. Digit. Health 2025, 7, 1622302. [Google Scholar] [CrossRef]
- Costa, M.V.d.S.; Camargos, M.C.S.; Viana, S.M.N.; Mendes, U.V.d.S. Advances and challenges of interoperability in the Unified Health System. J. Health Inform. 2025, 17, 1112. [Google Scholar] [CrossRef]
- Walker, D.M.; Tarver, W.L.; Jonnalagadda, P.; Ranbom, L.; Ford, E.W.; Rahurkar, S. Perspectives on Challenges and Opportunities for Interoperability: Findings From Key Informant Interviews With Stakeholders in Ohio. JMIR Med. Inform. 2023, 11, e43848. [Google Scholar] [CrossRef]
- Guo, C.; Ashrafian, H.; Ghafur, S.; Fontana, G.; Gardner, C.; Prime, M. Challenges for the evaluation of digital health solutions—A call for innovative evidence generation approaches. Npj Digit. Med. 2020, 3, 110. [Google Scholar] [CrossRef]
- Marwaha, J.S.; Landman, A.B.; Brat, G.A.; Dunn, T.; Gordon, W.J. Deploying digital health tools within large, complex health systems: Key considerations for adoption and implementation. Npj Digit. Med. 2022, 5, 13. [Google Scholar] [CrossRef] [PubMed]
- Frisinger, A.; Papachristou, P. The voice of healthcare: Introducing digital decision support systems into clinical practice—A qualitative study. BMC Prim. Care 2023, 24, 67. [Google Scholar] [CrossRef] [PubMed]
- Yfanti, S.; Sakkas, N. Technology Readiness Levels (TRLs) in the Era of Co-Creation. Appl. Syst. Innov. 2024, 7, 32. [Google Scholar] [CrossRef]
- Zakiyah, N.; Marulin, D.; Alfaqeeh, M.; Puspitasari, I.M.; Lestari, K.; Lim, K.K.; Fox-Rushby, J. Economic Evaluations of Digital Health Interventions for Patients With Heart Failure: Systematic Review. J. Med. Internet Res. 2024, 26, e53500. [Google Scholar] [CrossRef]
- Yang, Y.; Subhani, G.; Sakina.; Zhou, Y. Natural resource and energy efficiency in BRICS countries: Can green innovation capabilities really change the game? Gondwana Res. 2025, 145, 228–239. [Google Scholar] [CrossRef]
- Camacho, J.; Zanoletti-Mannello, M.; Landis-Lewis, Z.; Kane-Gill, S.L.; Boyce, R.D. A Conceptual Framework to Study the Implementation of Clinical Decision Support Systems (BEAR): Literature Review and Concept Mapping. J. Med. Internet Res. 2020, 22, e18388. [Google Scholar] [CrossRef]
| Author | Year | Tool, Technology, or Technique | Application Domain & Scope | Key Factors or Variables Used | Foundation or Validation Technique | Implications for Practice |
|---|---|---|---|---|---|---|
| Carvalho et al. [16] | 2015 | Territorial digital map of family health strategy; geographic information systems | Primary health care, leprosy control; Castanhal, PA, Brazil | FHS territories, health data, risk factors | GIS-based visualization and analysis | Enhanced information management for health programs, leprosy control. |
| Inácio et al. [17] | 2016 | GISTelemed (georeferenced epidemiological analysis tool) | Telemedicine, epidemiological view; Santa Catarina state | Structured and semi-structured data, morbidity, mortality | Case study or feedback from experts | Improved epidemiological surveillance and resource allocation. |
| Redeker et al. [18] | 2017 | Business process modeling and simulation; BPMN, discrete-event simulation | Healthcare capacity and resource allocation | Surgical center capacity, performance indices | Simulation of ”what if” scenarios | Optimized resource use and improved healthcare process management. |
| Jasmim et al. [19] | 2017 | Analysis of healthcare network; complex network analysis | Healthcare network characterization | Patient flow, service types, professionals, patients | Exploratory study of patient flows | Better understanding of healthcare network behavior and resource allocation. |
| Oliveira et al. [20] | 2018 | Software-defined networking (SDN) | Hospital network management, prioritization of traffic | Medical device traffic, network quality parameters | SDN-based traffic prioritization | Improved network quality of service for critical devices. |
| Vargas et al. [21] | 2018 | BPMN, discrete-event simulation | Analysis of billing process, hospital accounting | Process activities, time, resource usage | Proof simulations | Identification of bottlenecks and improvement in billing process. |
| Schmidt et al. [22] | 2018 | Deep learning model (CNN) | Mortality prediction in intensive care units; MIMIC III database | Patient data, risk of death | Comparison with APACHE II model | Improved prediction of mortality risk in ICUs. |
| Veras et al. [23] | 2019 | Tool for automatic goal balancing; Simulation of contingent scenarios | Health indices in primary care | Health indicators, planned values, deviations | Statistical significance tests | Improved planning and monitoring of indicators in dynamic scenarios. |
| Ferré et al. [24] | 2020 | Platform for knowledge management and visualization; data extraction, wiki documentation | Health technology assessment, SUS data; Brazil | Outpatient records, clinical protocols, dispensing records, user data | Automated extraction and visualization, documented in wiki | Transparent knowledge management and reproducible statistical analysis for decision-making. |
| Rolim et al. [25] | 2020 | Enterprise knowledge graph; incremental construction, ontologies, semantic integration | SUS data integration; Brazil | Data from SIM and SINASC, health data sources | SPARQL queries for validation | Flexible and extensible approach for integrating various SUS data sources. |
| Fischer et al. [26] | 2020 | Helastic model; IoT and elasticity in cloud computing | Human resource analysis in intelligent hospitals | Patient room usage, healthcare professional availability | Predictive approach for resource movement | Reduced waiting times and optimized resource allocation. |
| Silva et al. [27] | 2020 | Analysis of pregnant women’s care trajectories; data analysis | Healthcare network analysis for pregnant women; São Paulo | Patient trajectories, attendance records, health units | Analysis of patient trajectories | Better visibility of the healthcare system. |
| Moreira et al. [28] | 2021 | Machine learning models for type 1 diabetes prediction; classification model | Diabetes prediction in pregnancy | Outpatient production data, patient characteristics | Sensitivity, and precision of the classifier | Early prediction and better care to pregnant women at risk. |
| Gomes et al. [29] | 2022 | ONTOVID (semantic knowledge graphs); NeOn methodology, ontology-based data integration | COVID-19 data analysis, mortality information | Mortality data, COVID-19 notifications, vaccinations, hospitalizations | Validation by health department managers | Improved data integration and accurate extraction of indicators. |
| Rodrigues and Kreutz [30] | 2022 | Predictor for mortality risk in COVID-19; random forests | COVID-19 mortality risk classification; Brazil | Patient data, risk of death | AUC-ROC score for model evaluation | Assist in decision-making in the hospital environment. |
| Moreira et al. [31] | 2022 | Prediction of neonatal death; classifier using SUS and census data | Neonatal death prediction | SUS information systems data, demographic census data | Accuracy and sensitivity of prediction | Early warning system for neonatal risks and improved maternal/newborn monitoring. |
| Pereira et al. [32] | 2023 | Web platform for visualization and analysis; complex system techniques | Health regionalization; Brazil | Patient flow records from SIHSUS, health regions | Visualization and interactive web platform | Support evidence-based public policymaking in health regionalization. |
| Aleixo et al. [33] | 2023 | Machine learning models (LightGBM, XGBoost, Catboost); statistical analysis | Dengue outbreak prediction, congenital syphilis diagnosis | Sociodemographic, climatic, historical case data, mosquito index | AUC metric for syphilis, outbreak identification accuracy for dengue | Improved prediction of disease outbreaks and diagnosis of congenital syphilis. |
| Cid et al. [34] | 2023 | Constraint programming the in physician rostering problem | Physician scheduling in hospitals | Service demand, physician availability, scheduling preferences | Test and proof | Improved efficiency and fairness in physician scheduling. |
| Gregório et al. [35] | 2023 | Information system for endemic control; app for health agents | Aedes aegypti control; Itajubá, MG, Brazil | Epidemiological data, weekly reports, field data | Data collection and reporting system | Enhanced monitoring of endemic control actions. |
| Fischer et al. [36] | 2023 | CityHealth model; elasticity concept in cloud computing | Hospital management in smart cities | Vital signs data, hospital resource usage, patient demand | Emulation of smart city with hospitals | Reduced waiting times and improved resource management. |
| Teixeira and Endo [37] | 2023 | Machine learning models (SVM, AdaBoost); Statistical analysis | Prediction of congenital syphilis; Pernambuco, Brazil | Clinical and sociodemographic data of pregnant women | Performance evaluation of different models | Assist in resource allocation and optimize healthcare actions in low-resource settings. |
| Alencar et al. [38] | 2024 | Telemonitoring system; data extraction from RNDS, PEC, SINAN | Telemonitoring of health programs; Manaus, AM, Brazil | Patient data, reports, graphs, municipal indicators | Real-time reporting and graphing | Remote monitoring of patients and support for decision making by health managers. |
| Fischer et al. [39] | 2024 | ElCareCity model; Reactive and proactive elasticity | Multi-hospital resource management in smart cities | Patient usage of health environments, personnel allocation | Emulation of smart city with hospital environments | Efficient allocation of health professionals and reduced waiting times. |
| Gomes et al. [40] | 2024 | Mathematical modeling for ICU bed allocation optimization | ICU bed allocation | Bed types, occupancy rate, patient survival rates | Computational simulation with real data | Improved ICU bed allocation and patient survival rates. |
| Consoli et al. [41] | 2024 | Prediction of inpatient admissions; AI solution | Inpatient flow prediction | Patient data, length of stay | Accuracy of prediction | Accelerated administrative processes and improved care. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bellei, E.A.; Moretto, C.F.; Freitas, C.M.D.S.; De Marchi, A.C.B. A Survey on Digital Solutions for Health Services Management: Features and Use Cases from Brazilian National Literature. Healthcare 2025, 13, 2348. https://doi.org/10.3390/healthcare13182348
Bellei EA, Moretto CF, Freitas CMDS, De Marchi ACB. A Survey on Digital Solutions for Health Services Management: Features and Use Cases from Brazilian National Literature. Healthcare. 2025; 13(18):2348. https://doi.org/10.3390/healthcare13182348
Chicago/Turabian StyleBellei, Ericles Andrei, Cleide Fátima Moretto, Carla Maria Dal Sasso Freitas, and Ana Carolina Bertoletti De Marchi. 2025. "A Survey on Digital Solutions for Health Services Management: Features and Use Cases from Brazilian National Literature" Healthcare 13, no. 18: 2348. https://doi.org/10.3390/healthcare13182348
APA StyleBellei, E. A., Moretto, C. F., Freitas, C. M. D. S., & De Marchi, A. C. B. (2025). A Survey on Digital Solutions for Health Services Management: Features and Use Cases from Brazilian National Literature. Healthcare, 13(18), 2348. https://doi.org/10.3390/healthcare13182348








