Implementing a Mixed Health Service Model as an Informed Modality to Enhance Prevention and Promote Workplace Health in the Greek Regional Public Sector: A Pilot Study in Crete
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Ethical Approval and Informed Consent
2.3. Setting and Participants
2.4. Data Collection Procedures
2.5. Intervention and Follow-Up Procedures
2.6. Service Satisfaction Assessment
2.7. Statistical Analysis
3. Results
3.1. Participation and Demographics
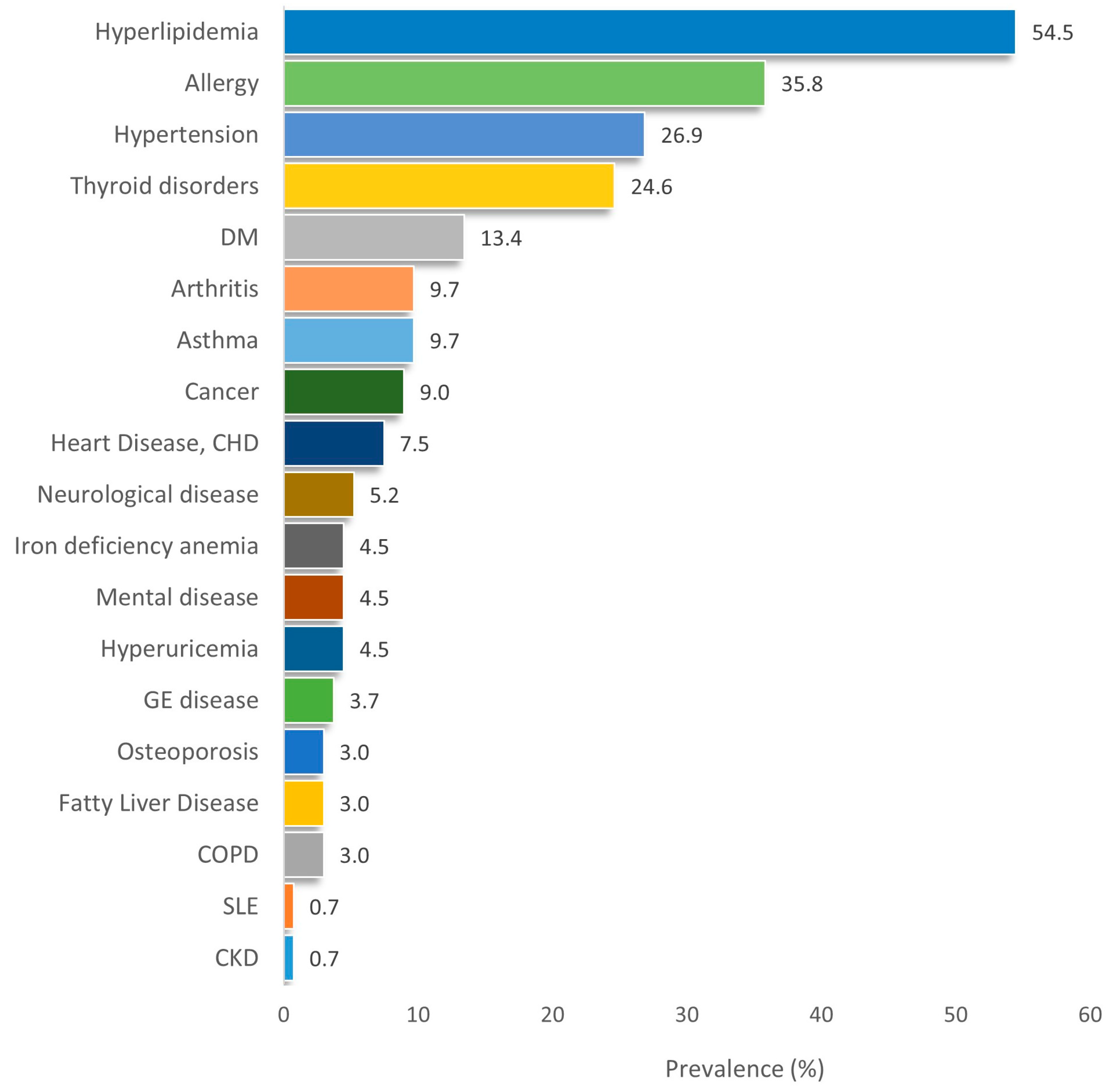
3.2. Prevalence of Chronic Conditions and Metabolic Syndrome
3.3. Vaccination Status
3.4. Mental Health and Perceived Stress
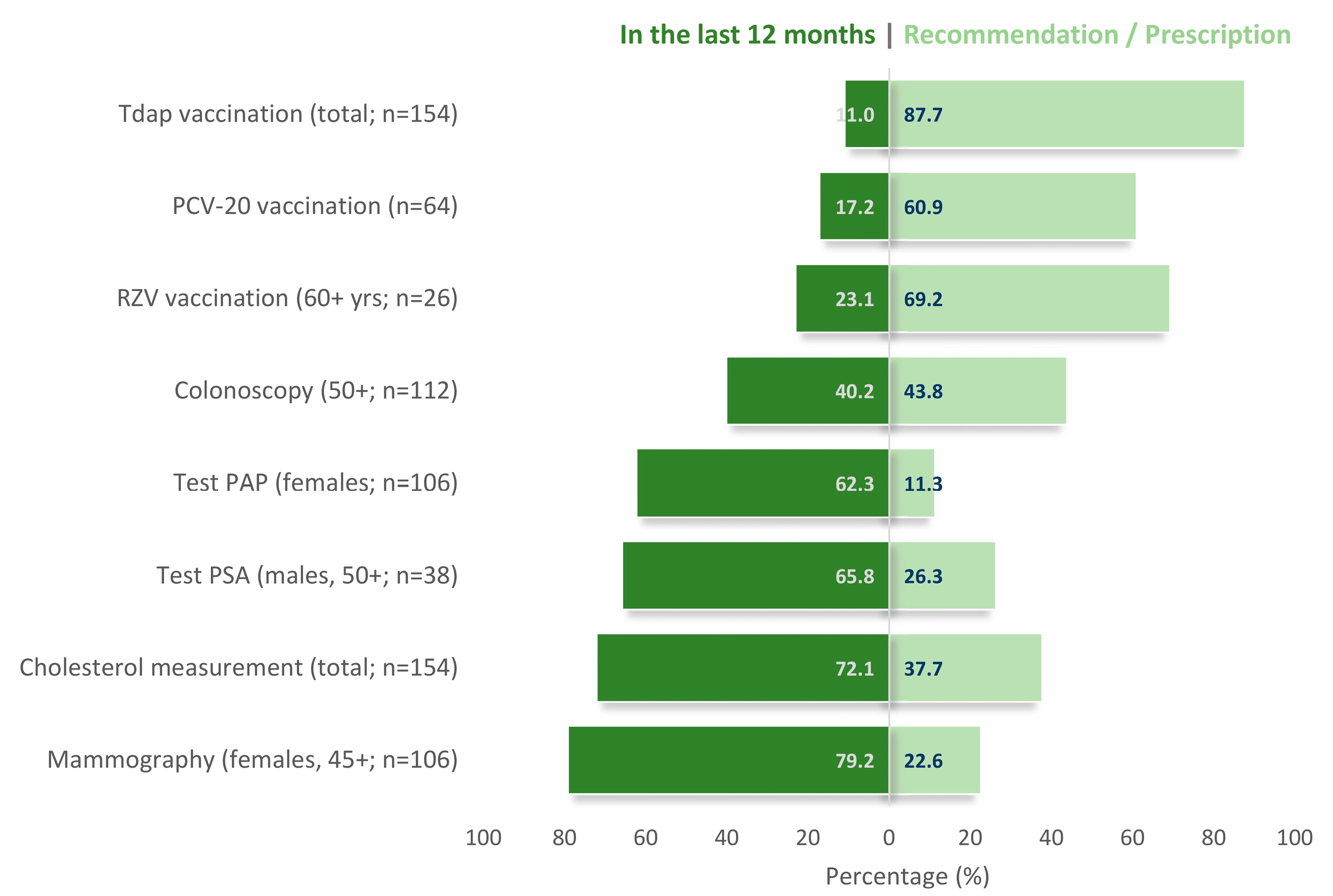
3.5. Diagnostic and Preventive Action Patterns
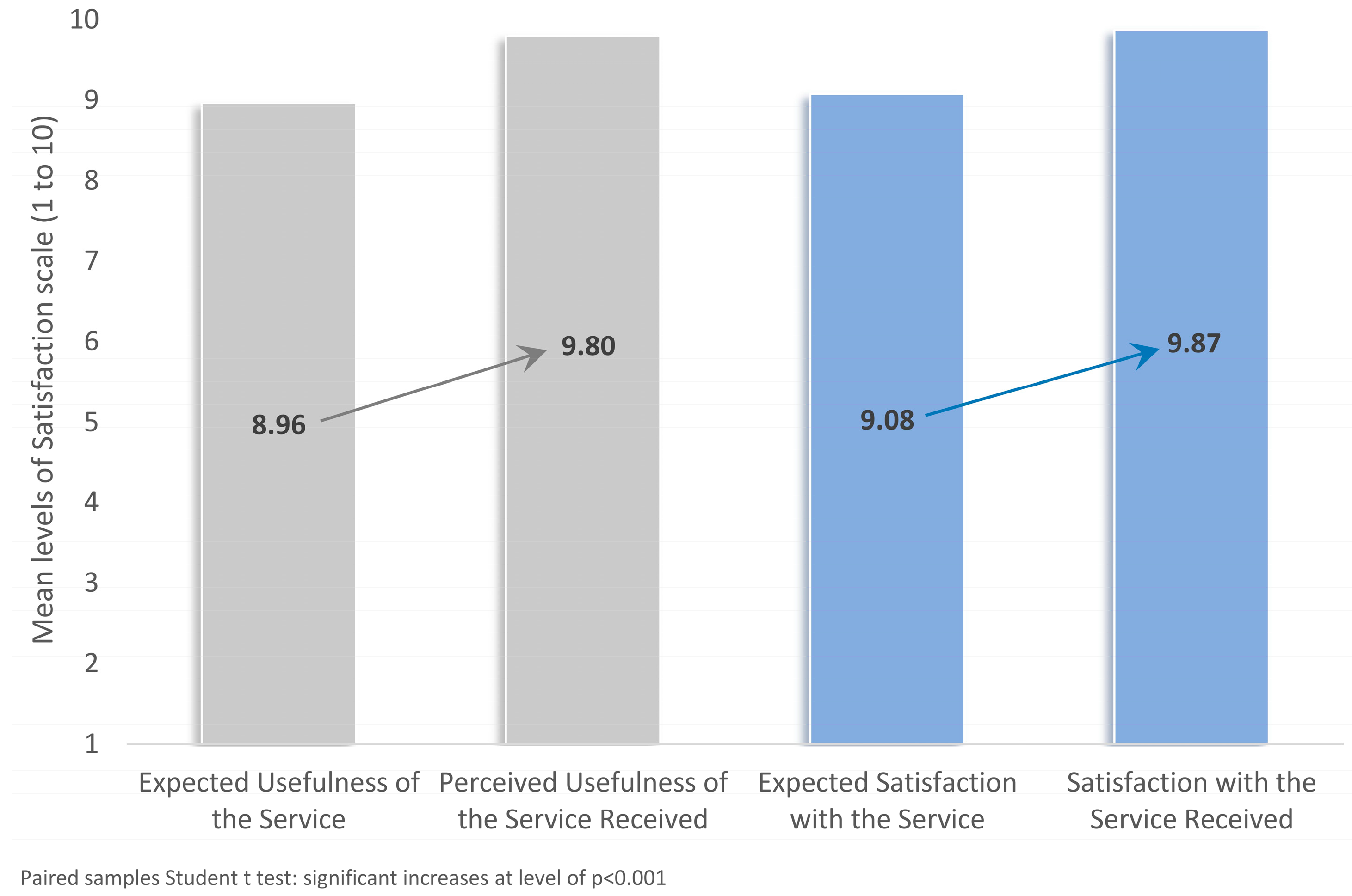
3.6. Service Satisfaction
4. Discussion
4.1. Main Findings in the Context of Existing Literature
4.2. Strengths, Limitations, and Directions for Future Research
4.3. Implications for Practice and Policy
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Global Status Report on Noncommunicable Diseases. 2014. Available online: https://www.who.int/publications/i/item/9789241564854 (accessed on 21 July 2025).
- Healthy Workplaces: A Model for Action. Available online: https://www.who.int/publications/i/item/9789241599313 (accessed on 21 July 2025).
- Cancelliere, C.; Cassidy, J.D.; Ammendolia, C.; Côté, P. Are Workplace Health Promotion Programs Effective at Improving Presenteeism in Workers? A Systematic Review and Best Evidence Synthesis of the Literature. BMC Public Health 2011, 11, 395. [Google Scholar] [CrossRef]
- Economou, C.; Kaitelidou, D.; Kentikelenis, A.; Maresso, A.; Sissouras, A. The Impact of the Crisis on the Health System and Health in Greece. In Economic Crisis, Health Systems and Health in Europe: Country Experience [Internet]; European Observatory on Health Systems and Policies: Copenhagen, Denmark, 2015. [Google Scholar]
- Zavras, D.; Tsiantou, V.; Pavi, E.; Mylona, K.; Kyriopoulos, J. Impact of Economic Crisis and Other Demographic and Socio-Economic Factors on Self-Rated Health in Greece. Eur. J. Public Health 2013, 23, 206–210. [Google Scholar] [CrossRef]
- Myloneros, T.; Sakellariou, D. The Effectiveness of Primary Health Care Reforms in Greece towards Achieving Universal Health Coverage: A Scoping Review. BMC Health Serv. Res. 2021, 21, 628. [Google Scholar] [CrossRef]
- Economou, C. Barriers and Facilitating Factors in Access to Health Services in Greece; World Health Organization Regional Office for Europe: Copenhagen, Denmark, 2015. [Google Scholar]
- LaMontagne, A.D.; Keegel, T.; Louie, A.M.; Ostry, A.; Landsbergis, P.A. A Systematic Review of the Job-Stress Intervention Evaluation Literature, 1990-2005. Int. J. Occup. Environ. Health 2007, 13, 268–280. [Google Scholar] [CrossRef]
- Eiden, A.L.; Barratt, J.; Nyaku, M.K. Drivers of and Barriers to Routine Adult Vaccination: A Systematic Literature Review. Hum. Vaccin. Immunother. 2022, 18, 2127290. [Google Scholar] [CrossRef]
- Guglielmi, V.; Colangeli, L.; Parrotta, M.E.; Ciammariconi, A.; Milani, I.; D’Adamo, M.; Sbraccia, P.; Capoccia, D. Social Isolation and Loneliness in Non-Communicable Chronic Diseases: Impact of COVID-19 Pandemic, Population Aging and Technological Progress. Nutr. Metab. Cardiovasc. Dis. 2025, 35, 104015. [Google Scholar] [CrossRef]
- Filip, R.; Gheorghita Puscaselu, R.; Anchidin-Norocel, L.; Dimian, M.; Savage, W.K. Global Challenges to Public Health Care Systems during the COVID-19 Pandemic: A Review of Pandemic Measures and Problems. J. Pers. Med. 2022, 12, 1295. [Google Scholar] [CrossRef]
- Overview of the Implementation of COVID-19 Vaccination Strategies and Deployment Plans in the EU/EEA. Available online: https://www.ecdc.europa.eu/en/publications-data/overview-implementation-covid-19-vaccination-strategies-and-deployment-plans (accessed on 21 July 2025).
- Vardavas, C.; Nikitara, K.; Aslanoglou, K.; Lagou, I.; Marou, V.; Phalkey, R.; Leonardi-Bee, J.; Fernandez, E.; Vivilaki, V.; Kamekis, A.; et al. Social Determinants of Health and Vaccine Uptake During the First Wave of the COVID-19 Pandemic: A Systematic Review. Prev. Med. Rep. 2023, 35, 102319. [Google Scholar] [CrossRef]
- Dermitzakis, I.; Evangelidis, N.; Evangelidis, P.; Anestis, A. Knowledge, Attitudes, and Perceptions Regarding COVID-19 Outbreak in Greece in September 2020: A Cross-Sectional Web-Based Survey. Hippokratia 2021, 25, 15–21. [Google Scholar]
- Galanis, P.; Moisoglou, I.; Vraka, I.; Siskou, O.; Konstantakopoulou, O.; Katsiroumpa, A.; Kaitelidou, D. Predictors of COVID-19 Vaccine Uptake in Healthcare Workers: A Cross-Sectional Study in Greece. J. Occup. Environ. Med. 2021, 64, e191. [Google Scholar] [CrossRef]
- Bouloukaki, I.; Christoforaki, A.; Christodoulakis, A.; Krasanakis, T.; Lambraki, E.; Pateli, R.; Markakis, M.; Tsiligianni, I. Vaccination Coverage and Associated Factors of COVID-19 Uptake in Adult Primary Health Care Users in Greece. Healthcare 2023, 11, 341. [Google Scholar] [CrossRef]
- Tan, L.; Wang, M.J.; Modini, M.; Joyce, S.; Mykletun, A.; Christensen, H.; Harvey, S.B. Preventing the Development of Depression at Work: A Systematic Review and Meta-Analysis of Universal Interventions in the Workplace. BMC Med. 2014, 12, 74. [Google Scholar] [CrossRef]
- Lassen, A.D.; Fagt, S.; Lennernäs, M.; Nyberg, M.; Haapalar, I.; Thorsen, A.V.; Møbjerg, A.C.M.; Beck, A.M. The Impact of Worksite Interventions Promoting Healthier Food and/or Physical Activity Habits among Employees Working ‘around the Clock’ Hours: A Systematic Review. Food Nutr. Res. 2018, 2, 62. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A Global Measure of Perceived Stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef]
- Antoniou, M.; Fradelos, E.C.; Roumeliotaki, T.; Malli, F.; Emmanouil, K.S.; Papagiannis, D. Assessing Mental Resilience with Individual and Lifestyle Determinants among Nursing Students: An Observational Study from Greece. AIMS Public Health 2024, 11, 946–961. [Google Scholar] [CrossRef]
- Lionis, C.; Symvoulakis, E.K.; Markaki, A.; Petelos, E.; Papadakis, S.; Sifaki-Pistolla, D.; Papadakakis, M.; Souliotis, K.; Tziraki, C. Integrated People-Centred Primary Health Care in Greece: Unravelling Ariadne’s Thread. Prim. Health Care Res. Dev. 2019, 20, e113. [Google Scholar] [CrossRef]
- Tsiligianni, I.; Bouloukaki, I.; Papazisis, G.; Paganas, A.; Chatzimanolis, E.; Kalatharas, M.; Platakis, I.; Tirodimos, I.; Dardavesis, T.; Tsimtsiou, Z. Vaccination Coverage and Predictors of Influenza, Pneumococcal, Herpes Zoster, Tetanus, Measles, and Hepatitis B Vaccine Uptake among Adults in Greece. Public Health 2023, 224, 195–202. [Google Scholar] [CrossRef]
- Tsachouridou, O.; Georgiou, A.; Naoum, S.; Vasdeki, D.; Papagianni, M.; Kotoreni, G.; Forozidou, E.; Tsoukra, P.; Gogou, C.; Chatzidimitriou, D.; et al. Factors Associated with Poor Adherence to Vaccination against Hepatitis Viruses, Streptococcus Pneumoniae and Seasonal Influenza in HIV-Infected Adults. Hum. Vaccin Immunother. 2019, 15, 295–304. [Google Scholar] [CrossRef]
- Papagiannis, D.; Rachiotis, G.; Mariolis, A.; Zafiriou, E.; Gourgoulianis, K.I. Vaccination Coverage of the Elderly in Greece: A Cross-Sectional Nationwide Study. Can. J. Infect. Dis. Med. Microbiol. 2020, 2020, 5459793. [Google Scholar] [CrossRef]
- Koloverou, E.; Panagiotakos, D.B.; Pitsavos, C.; Chrysohoou, C.; Georgousopoulou, E.N.; Pitaraki, E.; Metaxa, V.; Stefanadis, C. 10-Year Incidence of Diabetes and Associated Risk Factors in Greece: The ATTICA Study (2002–2012). Rev. Diabet. Stud. 2014, 11, 181–189. [Google Scholar] [CrossRef]
- Kollia, N.; Panagiotakos, D.B.; Chrysohoou, C.; Georgousopoulou, E.; Tousoulis, D.; Stefanadis, C.; Papageorgiou, C.; Pitsavos, C. Determinants of Healthy Ageing and Its Relation to 10-Year Cardiovascular Disease Incidence: The Attica Study. Cent. Eur. J. Public Health 2018, 26, 3–9. [Google Scholar] [CrossRef]
- Petridou, E.; Syrigou, E.; Toupadaki, N.; Zavitsanos, X.; Willett, W.; Trichopoulos, D. Determinants of Age at Menarche as Early Life Predictors of Breast Cancer Risk. Int. J. Cancer 1996, 68, 193–198. [Google Scholar] [CrossRef]
- Faka, A.; Damigou, E.; Chrysohoou, C.; Barkas, F.; Vlachopoulou, E.; Dalmyras, D.; Vafia, C.; Michelis, E.; Loukina, A.; Mentzantonakis, G.; et al. Twenty-Year Incidence Rates of Cardiovascular Disease in Greece: A Geospatial Analysis in the Attica Study Context, 2002–2022. J. Atheroscler. Prev. Treat. 2023, 14, 97–102. [Google Scholar] [CrossRef]
- Kapantais, E.; Tzotzas, T.; Ioannidis, I.; Mortoglou, A.; Bakatselos, S.; Kaklamanou, M.; Lanaras, L.; Kaklamanos, I. First National Epidemiological Survey on the Prevalence of Obesity and Abdominal Fat Distribution in Greek Adults. Ann. Nutr. Metab. 2006, 50, 330–338. [Google Scholar] [CrossRef]
- Tzanakis, N.; Koulouris, N.; Dimakou, K.; Gourgoulianis, K.; Kosmas, E.; Chasapidou, G.; Konstantinidis, A.; Kyriakopoulos, C.; Kontakiotis, T.; Rapti, A.; et al. Classification of COPD Patients and Compliance to Recommended Treatment in Greece According to GOLD 2017 Report: The RELICO Study. BMC Pulm. Med. 2021, 21, 216. [Google Scholar] [CrossRef]
- Zagkas, D.G.; Chrousos, G.P.; Bacopoulou, F.; Kanaka-Gantenbein, C.; Vlachakis, D.; Tzelepi, I.; Darviri, C. Stress and Well-Being of Greek Primary School Educators: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2023, 20, 5390. [Google Scholar] [CrossRef]
- Baez, A.S.; Ortiz-Whittingham, L.R.; Tarfa, H.; Osei Baah, F.; Thompson, K.; Baumer, Y.; Powell-Wiley, T.M. Social Determinants of Health, Health Disparities, and Adiposity. Prog. Cardiovasc. Dis. 2023, 78, 17–26. [Google Scholar] [CrossRef]
- Kivimäki, M.; Nyberg, S.T.; Batty, G.D.; Fransson, E.I.; Heikkilä, K.; Alfredsson, L.; Bjorner, J.B.; Borritz, M.; Burr, H.; Casini, A.; et al. Job Strain as a Risk Factor for Coronary Heart Disease: A Collaborative Meta-Analysis of Individual Participant Data. Lancet 2012, 380, 1491–1497. [Google Scholar] [CrossRef]
- National Cholesterol Education Program Expert Panel on Detection Evaluation and Treatment of High Blood Cholesterol in Adults. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Final Report. Circulation 2002, 106, 3143–3564. [Google Scholar] [CrossRef]
- National Adult Vaccination Program 2025. Timetable and Recommendations. Available online: https://www.moh.gov.gr/articles/health/dieythynsh-dhmosias-ygieinhs/emboliasmoi/ethniko-programma-emboliasmwn-epe-enhlikwn/13219-ethniko-programma-emboliasmwn-enhlikwn-2025-xronodiagramma-kai-systaseis (accessed on 4 August 2025).
- Karekla, M.; Pilipenko, N.; Feldman, J. Patient Health Questionnaire: Greek Language Validation and Subscale Factor Structure. Compr. Psychiatry 2012, 53, 1217–1226. [Google Scholar] [CrossRef]
- Katsarou, A.; Panagiotakos, D.; Zafeiropoulou, A.; Vryonis, M.; Ioannis Skoularigis; Filippos Tryposkiadis; Papageorgiou, C. Validation of a Greek Version of PSS-14; A Global Measure of Perceived Stress. Cent. Eur. J. Public Health 2012, 20, 104–109. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9: Validity of a Brief Depression Severity Measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Iriti, M.; Varoni, E.M.; Vitalini, S. Healthy Diets and Modifiable Risk Factors for Non-Communicable Diseases-The European Perspective. Foods 2020, 9, 940. [Google Scholar] [CrossRef]
- Valenzuela, P.L.; Santos-Lozano, A.; Saco-Ledo, G.; Castillo-García, A.; Lucia, A. Obesity, Cardiovascular Risk, and Lifestyle: Cross-Sectional and Prospective Analyses in a Nationwide Spanish Cohort. Eur. J. Prev. Cardiol. 2023, 30, 1493–1501. [Google Scholar] [CrossRef]
- Castillo-García, A.; Valenzuela, P.L.; Saco-Ledo, G.; Carrera-Bastos, P.; Ruilope, L.M.; Santos-Lozano, A.; Lucia, A. Lifestyle and Cardiovascular Risk in Working Young Adults: Insights from a Nationwide Spanish Cohort. Rev. Española De Cardiol. íA (Engl. Ed.) 2024, 77, 821–831. [Google Scholar] [CrossRef]
- Yusuf, P.S.; Hawken, S.; Ôunpuu, S.; Dans, T.; Avezum, A.; Lanas, F.; McQueen, M.; Budaj, A.; Pais, P.; Varigos, J.; et al. Effect of Potentially Modifiable Risk Factors Associated with Myocardial Infarction in 52 Countries (the INTERHEART Study): Case-Control Study. Lancet 2004, 364, 937–952. [Google Scholar] [CrossRef]
- Gallucci, G.; Tartarone, A.; Lerose, R.; Lalinga, A.V.; Capobianco, A.M. Cardiovascular Risk of Smoking and Benefits of Smoking Cessation. J. Thorac. Dis. 2020, 12, 3866–3876. [Google Scholar] [CrossRef]
- Milionis, C.; Ilias, I.; Tselebis, A.; Pachi, A. Psychological and Social Aspects of Vaccination Hesitancy—Implications for Travel Medicine in the Aftermath of the COVID-19 Crisis: A Narrative Review. Medicina 2023, 59, 1744. [Google Scholar] [CrossRef]
- Goje, O.; Kapoor, A. Meeting the Challenge of Vaccine Hesitancy. Cleve Clin. J. Med. 2024, 91, S50–S56. [Google Scholar] [CrossRef]
- Singh, P.; Dhalaria, P.; Kashyap, S.; Soni, G.K.; Nandi, P.; Ghosh, S.; Mohapatra, M.K.; Rastogi, A.; Prakash, D. Strategies to Overcome Vaccine Hesitancy: A Systematic Review. Syst. Rev. 2022, 11, 78. [Google Scholar] [CrossRef]
- Fotiadis, K.; Dadouli, K.; Avakian, I.; Bogogiannidou, Z.; Mouchtouri, V.A.; Gogosis, K.; Speletas, M.; Koureas, M.; Lagoudaki, E.; Kokkini, S.; et al. Factors Associated with Healthcare Workers’ (HCWs) Acceptance of COVID-19 Vaccinations and Indications of a Role Model towards Population Vaccinations from a Cross-Sectional Survey in Greece, May 2021. Int. J. Environ. Res. Public Health 2021, 18, 10558. [Google Scholar] [CrossRef]
- Papagiannis, D.; Rachiotis, G.; Malli, F.; Papathanasiou, I.V.; Kotsiou, O.; Fradelos, E.C.; Giannakopoulos, K.; Gourgoulianis, K.I. Acceptability of Covid-19 Vaccination among Greek Health Professionals. Vaccines 2021, 9, 200. [Google Scholar] [CrossRef]
- Pennisi, F.; Genovese, C.; Gianfredi, V. Lessons from the COVID-19 Pandemic: Promoting Vaccination and Public Health Resilience, a Narrative Review. Vaccines 2024, 12, 891. [Google Scholar] [CrossRef]
- Rongen, A.; Robroek, S.J.W.; Van Lenthe, F.J.; Burdorf, A. Workplace Health Promotion: A Meta-Analysis of Effectiveness. Am. J. Prev. Med. 2013, 44, 406–415. [Google Scholar] [CrossRef]
- Proper, K.I.; Van Oostrom, S.H. The Effectiveness of Workplace Health Promotion Interventions on Physical and Mental Health Outcomes—A Systematic Review of Reviews. Scand. J. Work Environ. Health 2019, 45, 546–559. [Google Scholar] [CrossRef]
- Joyce, S.; Modini, M.; Christensen, H.; Mykletun, A.; Bryant, R.; Mitchell, P.B.; Harvey, S.B. Workplace Interventions for Common Mental Disorders: A Systematic Meta-Review. Psychol. Med. 2016, 46, 683–697. [Google Scholar] [CrossRef]
- Sorensen, G.; Landsbergis, P.; Hammer, L.; Amick, B.C.; Linnan, L.; Yancey, A.; Welch, L.S.; Goetzel, R.Z.; Flannery, K.M.; Pratt, C. Preventing Chronic Disease in the Workplace: A Workshop Report and Recommendations. Am. J. Public Health 2011, 101, S196–S207. [Google Scholar] [CrossRef]
- The New European Framework for Action on Integrated Health Services Delivery. Available online: https://www.who.int/europe/multi-media/item/the-new-european-framework-for-action-on-integrated-health-services-delivery (accessed on 21 July 2025).
- Ammendolia, C.; Côté, P.; Cancelliere, C.; Cassidy, J.D.; Hartvigsen, J.; Boyle, E.; Soklaridis, S.; Stern, P.; Amick, B. Healthy and Productive Workers: Using Intervention Mapping to Design a Workplace Health Promotion and Wellness Program to Improve Presenteeism. BMC Public Health 2016, 16, 1190. [Google Scholar] [CrossRef]
- Poscia, A.; Moscato, U.; La Milia, D.I.; Milovanovic, S.; Stojanovic, J.; Borghini, A.; Collamati, A.; Ricciardi, W.; Magnavita, N. Workplace Health Promotion for Older Workers: A Systematic Literature Review. BMC Health Serv. Res. 2016, 16, 415–428. [Google Scholar] [CrossRef]
- Bergerman, L.; Corabian, P.; Harstall, C. Effectiveness of Organizational Interventions for the Prevention of Workplace Stress. IHE Rep. 2009. [Google Scholar]
- Proper, K.; Van Mechelen, W. Effectiveness and Economic Impact of Worksite Interventions to Promote Physical Activity and Healthy Diet; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Caring for Those Who Care: Guide for the Development and Implementation of Occupational Health and Safety Programmes for Health Workers. Available online: https://www.who.int/publications/i/item/9789240040779 (accessed on 21 July 2025).
- Good Practice in Occupational Health Services: A Contribution to Workplace Health. Available online: https://iris.who.int/handle/10665/107448 (accessed on 21 July 2025).
- Global Strategy on Occupational Health for All: The Way to Health at Work. Available online: https://wkc.who.int/resources/publications/i/item/global-strategy-on-occupational-health-for-all-the-way-to-health-at-work (accessed on 21 July 2025).
- Buijs, P.; Gunnyeon, B.; Van Weel, C. Primary Health Care: What Role for Occupational Health? Br. J. Gen. Pract. 2012, 62, 623–624. [Google Scholar] [CrossRef]
- Safe and Healthy Workplaces in Europe: Where Do We Stand in 2023?|Safety and Health at Work EU-OSHA. Available online: https://osha.europa.eu/en/publications/safe-and-healthy-workplaces-europe-where-do-we-stand-2023 (accessed on 21 July 2025).
- European Agency for Safety & Health at Work—Information, Statistics, Legislation and Risk Assessment Tools. Available online: https://osha.europa.eu/en (accessed on 21 July 2025).
- Health Services Delivery Programme, Division of Health Systems and Public Health. The European Framework for Action on Integrated Health Services Delivery: An Overview; WHO: Copenhagen Ø, Denmark, 2016. [Google Scholar]
- Mental Health and Work: Impact, Issues and Good Practices. Available online: https://iris.who.int/handle/10665/42346 (accessed on 21 July 2025).
- Psychosocial Risks in Europe: Prevalence and Strategies for Prevention | European Foundation for the Improvement of Living and Working Conditions. Available online: https://www.eurofound.europa.eu/en/publications/2014/psychosocial-risks-europe-prevalence-and-strategies-prevention (accessed on 21 July 2025).
- Sun, L.; Booth, A.; Sworn, K. Adaptability, Scalability and Sustainability (ASaS) of Complex Health Interventions: A Systematic Review of Theories, Models and Frameworks. Implement Sci. 2024, 19, 52. [Google Scholar] [CrossRef]
- Anders, C.; Moorthy, P.; Svensson, L.; Müller, J.; Heinze, O.; Knaup, P.; Wallwiener, M.; Deutsch, T.M.; Le, T.-V.; Weinert, L. Usability and User Experience of an MHealth App for Therapy Support of Patients with Breast Cancer: Mixed Methods Study Using Eye Tracking. JMIR Hum. Factors 2024, 11, e50926. [Google Scholar] [CrossRef]
- Overdijkink, S.B.; Velu, A.V.; Rosman, A.N.; van Beukering, M.D.M.; Kok, M.; Steegers-Theunissen, R.P.M. The Usability and Effectiveness of Mobile Health Technology–Based Lifestyle and Medical Intervention Apps Supporting Health Care during Pregnancy: Systematic Review. JMIR Mhealth Uhealth 2018, 6, e109. [Google Scholar] [CrossRef]
- Regan, C.; Von Rosen, P.; Andermo, S.; Hagströmer, M.; Johansson, U.B.; Rossen, J. The Acceptability, Usability, Engagement and Optimisation of a MHealth Service Promoting Healthy Lifestyle Behaviours: A Mixed Method Feasibility Study. Digit Health 2024, 10, 20552076241247935. [Google Scholar] [CrossRef]
- Rowland, S.; Ramos, A.K.; Trinidad, N.; Quintero, S.; Johnson Beller, R.; Struwe, L.; Pozehl, B. Feasibility, Usability and Acceptability of a MHealth Intervention to Reduce Cardiovascular Risk in Rural Hispanic Adults: Descriptive Study. JMIR Form. Res. 2022, 6, e40379. [Google Scholar] [CrossRef]
- Bergevi, J.; Andermo, S.; Woldamanuel, Y.; Johansson, U.B.; Hagströmer, M.; Rossen, J. User Perceptions of EHealth and MHealth Services Promoting Physical Activity and Healthy Diets: Systematic Review. JMIR Hum. Factors 2022, 9, e34278. [Google Scholar] [CrossRef]
- Spanakis, M.; Sfakianakis, S.; Kallergis, G.; Spanakis, E.G.; Sakkalis, V. PharmActa: Personalized Pharmaceutical Care EHealth Platform for Patients and Pharmacists. J. Biomed. Inf. 2019, 100, 103336. [Google Scholar] [CrossRef]
- Olawade, D.B.; Wada, O.J.; David-Olawade, A.C.; Kunonga, E.; Abaire, O.; Ling, J. Using Artificial Intelligence to Improve Public Health: A Narrative Review. Front. Public Health 2023, 11, 1196397. [Google Scholar] [CrossRef]
- Iribarren, S.J.; Akande, T.O.; Kamp, K.J.; Barry, D.; Kader, Y.G.; Suelzer, E. Effectiveness of Mobile Apps to Promote Health and Manage Disease: Systematic Review and Meta-Analysis of Randomized Controlled Trials. JMIR Mhealth Uhealth 2021, 9, e21563. [Google Scholar] [CrossRef]
- Mezzalira, E.; Canzan, F.; Marini, G.; Longhini, J.; Leardini, C.; Saiani, L.; Ambrosi, E. Introduction of Novel Complex Integrated Care Models Supported by Digital Health Interventions in European Primary Settings: A Scoping Review. Health Policy Technol. 2024, 13, 100896. [Google Scholar] [CrossRef]
- Oh, A.; Abazeed, A.; Chambers, D.A. Policy Implementation Science to Advance Population Health: The Potential for Learning Health Policy Systems. Front. Public Health 2021, 9, 681602. [Google Scholar] [CrossRef]
- Newman, M.W. Value Added? A Pragmatic Analysis of the Routine Use of PHQ-9 and GAD-7 Scales in Primary Care. Gen. Hosp. Psychiatry 2022, 79, 15–18. [Google Scholar] [CrossRef] [PubMed]
- Carroll, H.A.; Hook, K.; Perez, O.F.R.; Denckla, C.; Vince, C.C.; Ghebrehiwet, S.; Ando, K.; Touma, M.; Borba, C.P.C.; Fricchione, G.L.; et al. Establishing Reliability and Validity for Mental Health Screening Instruments in Resource-Constrained Settings: Systematic Review of the PHQ-9 and Key Recommendations. Psychiatry Res. 2020, 291, 113236. [Google Scholar] [CrossRef]
- Ford, J.; Thomas, F.; Byng, R.; McCabe, R. Use of the Patient Health Questionnaire (PHQ-9) in Practice: Interactions between Patients and Physicians. Qual. Health Res. 2020, 30, 2146–2159. [Google Scholar] [CrossRef]
- Iles, R.; Sheppard, D.M. Establishing Key Domains for Measuring Workplace Mental Health: The Indicators of A Thriving Workplace Survey. J. Occup. Rehabil. 2025. [Google Scholar] [CrossRef]
- Wagner, S.L.; Koehn, C.; White, M.I.; Harder, H.G.; Schultz, I.Z.; Williams-Whitt, K.; Wärje, O.; Dionne, C.E.; Koehoorn, M.; Pasca, R.; et al. Mental Health Interventions in the Workplace and Work Outcomes: A Best-Evidence Synthesis of Systematic Reviews. Int. J. Occup. Environ. Med. 2016, 7, 1–14. [Google Scholar] [CrossRef]
- Pearl, R.L. Weight Bias and Stigma: Public Health Implications and Structural Solutions. Soc. Issues Policy Rev. 2018, 12, 146–182. [Google Scholar] [CrossRef]
- Gray, N.S.; Davies, H.; Snowden, R.J. Reducing Stigma and Increasing Workplace Productivity Due to Mental Health Difficulties in a Large Government Organization in the UK: A Protocol for a Randomised Control Treatment Trial (RCT) of a Low Intensity Psychological Intervention and Stigma Reduction Programme for Common Mental Disorder (Prevail). BMC Public Health 2020, 20, 896. [Google Scholar] [CrossRef]
- Biswas, A.; Begum, M.; Van Eerd, D.; Johnston, H.; Smith, P.M.; Gignac, M.A.M. Integrating Safety and Health Promotion in Workplaces: A Scoping Review of Facilitators, Barriers, and Recommendations. Health Promot. Pr. 2022, 23, 984–998. [Google Scholar] [CrossRef]
- Wilcox, A.; Koontz, A. Workplace Well-Being: Shifting from an Individual to an Organizational Framework. Sociol. Compass 2022, 16, e13035. [Google Scholar] [CrossRef]
- Guest, D.E. Human Resource Management and Employee Well-Being: Towards a New Analytic Framework. Hum. Resour. Manag. J. 2017, 27, 22–38. [Google Scholar] [CrossRef]
- Motalebi G., M.; Keshavarz Mohammadi, N.; Kuhn, K.; Ramezankhani, A.; Azari, M.R. How Far Are We from Full Implementation of Health Promoting Workplace Concepts? A Review of Implementation Tools and Frameworks in Workplace Interventions. Health Promot. Int. 2018, 33, 488–504. [Google Scholar] [CrossRef]
- Review of Social Determinants and the Health Divide in the WHO European Region. Available online: https://www.who.int/publications/i/item/9789289000307 (accessed on 5 September 2025).
- Andersen, J.H.; Malmros, P.; Ebbehoej, N.E.; Flachs, E.M.; Bengtsen, E.; Bonde, J.P. Systematic Literature Review on the Effects of Occupational Safety and Health (OSH) Interventions at the Workplace. Scand. J. Work Environ. Health 2019, 45, 103–113. [Google Scholar] [CrossRef]
- Bondebjerg, A.; Filges, T.; Pejtersen, J.H.; Kildemoes, M.W.; Burr, H.; Hasle, P.; Tompa, E.; Bengtsen, E. Occupational Health and Safety Regulatory Interventions to Improve the Work Environment: An Evidence and Gap Map of Effectiveness Studies. Campbell Syst. Rev. 2023, 19, e1371. [Google Scholar] [CrossRef]
- Walters, D.; Johnstone, R. Improving Compliance with Occupational Safety and Health Regulations: An Overarching Review European Risk Observatory Literature Review; European Agency for Safety and Health at Work: Bilbao, Spain, 2021. [Google Scholar]
- Brenner, H.; Heisser, T.; Cardoso, R.; Hoffmeister, M. Reduction in Colorectal Cancer Incidence by Screening Endoscopy. Nat. Rev. Gastroenterol. Hepatol. 2024, 21, 125–133. [Google Scholar] [CrossRef]
- Heisser, T.; Sergeev, D.; Hoffmeister, M.; Brenner, H. Contributions of Early Detection and Cancer Prevention to Colorectal Cancer Mortality Reduction by Screening Colonoscopy: A Validated Modeling Study. Gastrointest. Endosc. 2024, 100, 710–717.e9. [Google Scholar] [CrossRef] [PubMed]
- Shattock, A.J.; Johnson, H.C.; Sim, S.Y.; Carter, A.; Lambach, P.; Hutubessy, R.C.W.; Thompson, K.M.; Badizadegan, K.; Lambert, B.; Ferrari, M.J.; et al. Contribution of Vaccination to Improved Survival and Health: Modelling 50 Years of the Expanded Programme on Immunization. Lancet 2024, 403, 2307–2316. [Google Scholar] [CrossRef] [PubMed]
- Braveman, P.; Gottlieb, L. The Social Determinants of Health: It’s Time to Consider the Causes of the Causes. Public Health Rep. 2014, 129, 19–31. [Google Scholar] [CrossRef] [PubMed]
- Verra, S.E.; Benzerga, A.; Jiao, B.; Ruggeri, K. Health Promotion at Work: A Comparison of Policy and Practice Across Europe. Saf. Health Work 2018, 10, 21. [Google Scholar] [CrossRef]
- Gagliardi, D.; Marinaccio, A.; Valenti, A.; Iavicoli, S. Occupational Safety and Health in Europe: Lessons from the Past, Challenges and Opportunities for the Future. Ind. Health 2012, 50, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Baicker, K.; Cutler, D.; Song, Z. Workplace Wellness Programs Can Generate Savings. Health Aff. 2010, 29, 304–311. [Google Scholar] [CrossRef]
- Tsiligianni, I.; Anastasiou, F.; Antonopoulou, M.; Chliveros, K.; Dimitrakopoulos, S.; Duijker, G.; Kounalakis, D.; Makri, K.; Petraki, C.; Prokopiadou, D.; et al. Greek Rural Gps’ Opinions on How Financial Crisis Influences Health, Quality of Care and Health Equity. Rural Remote Health 2013, 13, 309–312. [Google Scholar]
- Carter, M.W.; Simone, P.M.; Houry, D.E.; Reynolds, S.L.; Patterson, S.S.; Carlson, J.E.; Dauphin, L.A. Centers for Disease Control and Prevention’s Public Health Infrastructure Grant: A Better Approach to Empowering More State and Local Decision Making and Strengthening the Public Health Workforce and Infrastructure. J. Public Health Manag. Pr. 2024, 31, E88. [Google Scholar] [CrossRef]
- Committee on Public Health Strategies to Improve Health. Funding Sources and Structures to Build Public Health; National Academies Press: Washington, DC, USA, 2012. [Google Scholar]
- Spanakis, M.; Stamou, M.; Boultadaki, S.; Liantis, E.; Lionis, C.; Marinos, G.; Mariolis, A.; Matthaiou, A.M.; Mihas, C.; Mouchtouri, V.; et al. Enhancing Competencies and Professional Upskilling of Mobile Healthcare Unit Personnel at the Hellenic National Public Health Organization. Healthcare 2025, 13, 1706. [Google Scholar] [CrossRef]
- Empowerment Through Digital Health. Available online: https://www.who.int/europe/initiatives/empowerment-through-digital-health (accessed on 21 July 2025).
- Odone, A.; Buttigieg, S.; Ricciardi, W.; Azzopardi-Muscat, N.; Staines, A. Public Health Digitalization in Europe. Eur. J. Public Health 2019, 29, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Alderwick, H.; Hutchings, A.; Briggs, A.; Mays, N. The Impacts of Collaboration between Local Health Care and Non-Health Care Organizations and Factors Shaping How They Work: A Systematic Review of Reviews. BMC Public Health 2021, 21, 753. [Google Scholar] [CrossRef] [PubMed]
- Higgins, O.; Short, B.L.; Chalup, S.K.; Wilson, R.L. Artificial Intelligence (AI) and Machine Learning (ML) Based Decision Support Systems in Mental Health: An Integrative Review. Int. J. Ment. Health Nurs. 2023, 32, 966–978. [Google Scholar] [CrossRef]
- Tabrizi, J.S.; Azami-aghdash, S.; Gharaee, H. Public-Private Partnership Policy in Primary Health Care: A Scoping Review. J. Prim. Care Community Health 2020, 11, 2150132720943769. [Google Scholar] [CrossRef]
- Awad, A.; Trenfield, S.J.; Pollard, T.D.; Ong, J.J.; Elbadawi, M.; McCoubrey, L.E.; Goyanes, A.; Gaisford, S.; Basit, A.W. Connected Healthcare: Improving Patient Care Using Digital Health Technologies. Adv. Drug Deliv. Rev. 2021, 178, 113958. [Google Scholar] [CrossRef]
- Plans-Rubió, P. Strategies to Increase the Percentages of Vaccination Coverage. Vaccines 2022, 10, 2103. [Google Scholar] [CrossRef] [PubMed]
- WHO. Mental Health at Work. Available online: https://www.who.int/news-room/fact-sheets/detail/mental-health-at-work (accessed on 21 July 2025).
| n | % | |||
|---|---|---|---|---|
| Gender | males/females | 48/106 | 31.2/68.8 | |
| Age, years | mean ± stand. dev. | 54.0 ± 6.1 | ||
| 50+ years | 112 | 72.7 | ||
| 60+ years | 26 | 16.2 | ||
| Education level | High school | 25 | 16.2 | |
| University/Technical School | 66 | 42.9 | ||
| MSc | 53 | 34.4 | ||
| PhD | 10 | 6.5 | ||
| Smoking | nonsmokers | 80 | 51.9 | |
| ex | 36 | 23.4 | ||
| current | 38 | 24.7 | ||
| Cigarettes/day | median (IQR) | 15 (10, 20) | ||
| Years of smoking | median (IQR) | 29 (20.0, 35.0) | ||
| Alcohol consumption (at least half of drink per day) | yes | 15 | 9.8 | |
| Sleep hours at night | mean ± stand. dev. | 6.5 ± 1.2 | ||
| Body Mass Index, kg/m2 | mean ± stand. dev. | 28.3 ± 5.8 | ||
| Overweight/obese | 62/45 | 40.3/29.2 | ||
| Total (n = 130) | Males (n = 32) | Females (n = 88) | |||
|---|---|---|---|---|---|
| Risk Factors & MetS Criteria a | Mean ± Stand. dev. | p-Value b | |||
| SBP (mmHg) | 134.4 ± 17.4 | 143.0 ± 19.0 | 130.2 ± 15.0 | <0.001 | |
| DBP (mmHg) | 86.7 ± 11.6 | 89.8 ± 11.7 | 85.2 ± 11.4 | 0.037 | |
| >130/85 | 72.3% | 83.3% | 67.0% | 0.052 | |
| Fasting glucose (mg/dL) | 99.3 ± 15.3 | 102.4 ± 17.5 | 97.8 ± 14.0 | 0.103 | |
| ≥100 | 35.4% | 45.2% | 30.7% | 0.105 | |
| Triglycerides (mg/dL) | 98.5 ± 47.3 | 108.2 ± 55.9 | 93.9 ± 42.2 | 0.106 | |
| ≥150 | 13.1% | 16.7% | 11.4% | 0.402 | |
| HDL cholesterol (mg/dL) | 59.1 ± 12.8 | 52.5 ± 12.6 | 62.3 ± 11.6 | <0.001 | |
| <40 (M), <50 (F) | 16.9% | 19.0% | 15.9% | 0.655 | |
| Waist circumference (cm) | 98.3 ± 18.6 | 110.6 ± 17.9 | 92.4 ± 16.0 | <0.001 | |
| >102 (M), >88 (F) | 59.2% | 73.8% | 52.3% | 0.019 | |
| MetS risk factors | none | 15.4% | 7.2% | 19.3% | 0.029 |
| 1 | 22.3% | 19.0% | 23.9% | ||
| 2 | 29.2% | 23.8% | 31.8% | ||
| 3+ or MetS | 33.1% | 50.0% | 25.0% | ||
| Vaccine Type | Vaccination Status | n | % | |
|---|---|---|---|---|
| TD or Tdap or Tdap-IPV | Initial Vaccination | 94 | 61.0 | |
| Booster dose at age 18–25 with Tdap or Tdap-IPV | 43 | 27.9 | ||
| Booster dose in the last decade with TD or Tdap | 17 | 11.0 | ||
| RZV (>60 years & immunocompromised) | no | 20 | 76.9 | |
| yes | 6 | 23.1 | ||
| PCV20 or prior (PCV13, PPSV23) * | no | 53 | 82.8 | |
| yes | 11 | 17.2 | ||
| Scales | Mean | Stand. Dev. | Median |
|---|---|---|---|
| PSS Score a | 23.7 | 7.4 | 24.0 |
| low (0–13) | n = 10 or 6.6% | ||
| moderate (14–26) | n = 88 or 58.3% | ||
| high (27–42) | n = 53 or 35.1% | ||
| PHQ-9 Score b | 4.3 | 4.3 | 3.0 |
| none-minimal (0–4) | n = 92 or 60.9% | ||
| mild (5–9) | n = 43 or 28.5% | ||
| moderate to severe (10–27) | n = 16 or 10.6% | ||
| Proactive Action/Recommendation/Prescription | n | % |
|---|---|---|
| Vaccination | 141 | 91.6 |
| Biochemical blood test | 106 | 68.8 |
| Lifestyle Counseling | 97 | 63.0 |
| Socio-demographic screenings & preventive tests | 69 | 44.8 |
| Pharmacological intervention/prescription | 49 | 31.8 |
| Other actions | 14 | 9.1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Frantzeskakis, N.; Tziraki, M.; Spanakis, M.; Katsarou, S.D.; Papadopoulos, N.; Linardakis, M.; Vova-Chatzi, C.; Kamekis, A.; Pitsoulis, G.; Papadakis, A.; et al. Implementing a Mixed Health Service Model as an Informed Modality to Enhance Prevention and Promote Workplace Health in the Greek Regional Public Sector: A Pilot Study in Crete. Healthcare 2025, 13, 2337. https://doi.org/10.3390/healthcare13182337
Frantzeskakis N, Tziraki M, Spanakis M, Katsarou SD, Papadopoulos N, Linardakis M, Vova-Chatzi C, Kamekis A, Pitsoulis G, Papadakis A, et al. Implementing a Mixed Health Service Model as an Informed Modality to Enhance Prevention and Promote Workplace Health in the Greek Regional Public Sector: A Pilot Study in Crete. Healthcare. 2025; 13(18):2337. https://doi.org/10.3390/healthcare13182337
Chicago/Turabian StyleFrantzeskakis, Nikos, Maria Tziraki, Marios Spanakis, Spyridoula D. Katsarou, Nikolaos Papadopoulos, Manolis Linardakis, Charikleia Vova-Chatzi, Apostolos Kamekis, George Pitsoulis, Antonios Papadakis, and et al. 2025. "Implementing a Mixed Health Service Model as an Informed Modality to Enhance Prevention and Promote Workplace Health in the Greek Regional Public Sector: A Pilot Study in Crete" Healthcare 13, no. 18: 2337. https://doi.org/10.3390/healthcare13182337
APA StyleFrantzeskakis, N., Tziraki, M., Spanakis, M., Katsarou, S. D., Papadopoulos, N., Linardakis, M., Vova-Chatzi, C., Kamekis, A., Pitsoulis, G., Papadakis, A., & Symvoulakis, E. K. (2025). Implementing a Mixed Health Service Model as an Informed Modality to Enhance Prevention and Promote Workplace Health in the Greek Regional Public Sector: A Pilot Study in Crete. Healthcare, 13(18), 2337. https://doi.org/10.3390/healthcare13182337









