Treatment of Corneal Epithelium Lesions with Plasma Rich in Growth Factors: A Case Series and Implications
Abstract
1. Introduction
2. Case Description and Diagnostic Assessment
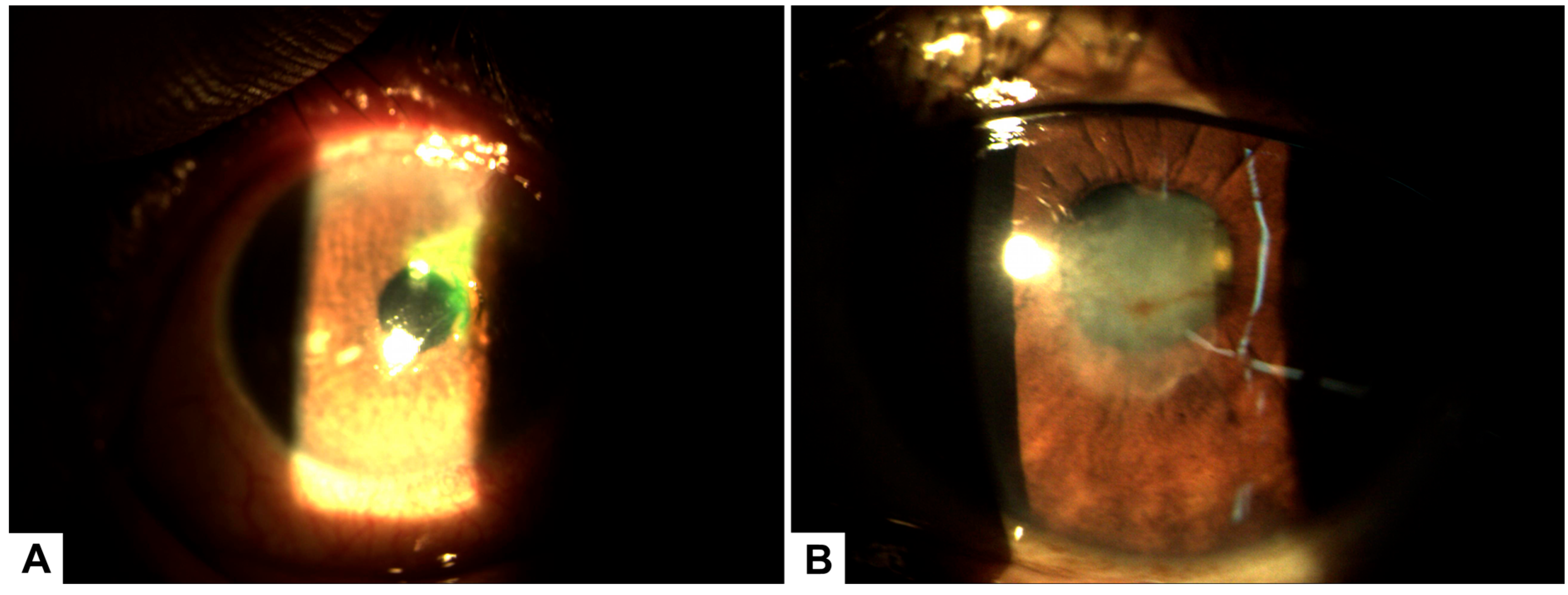
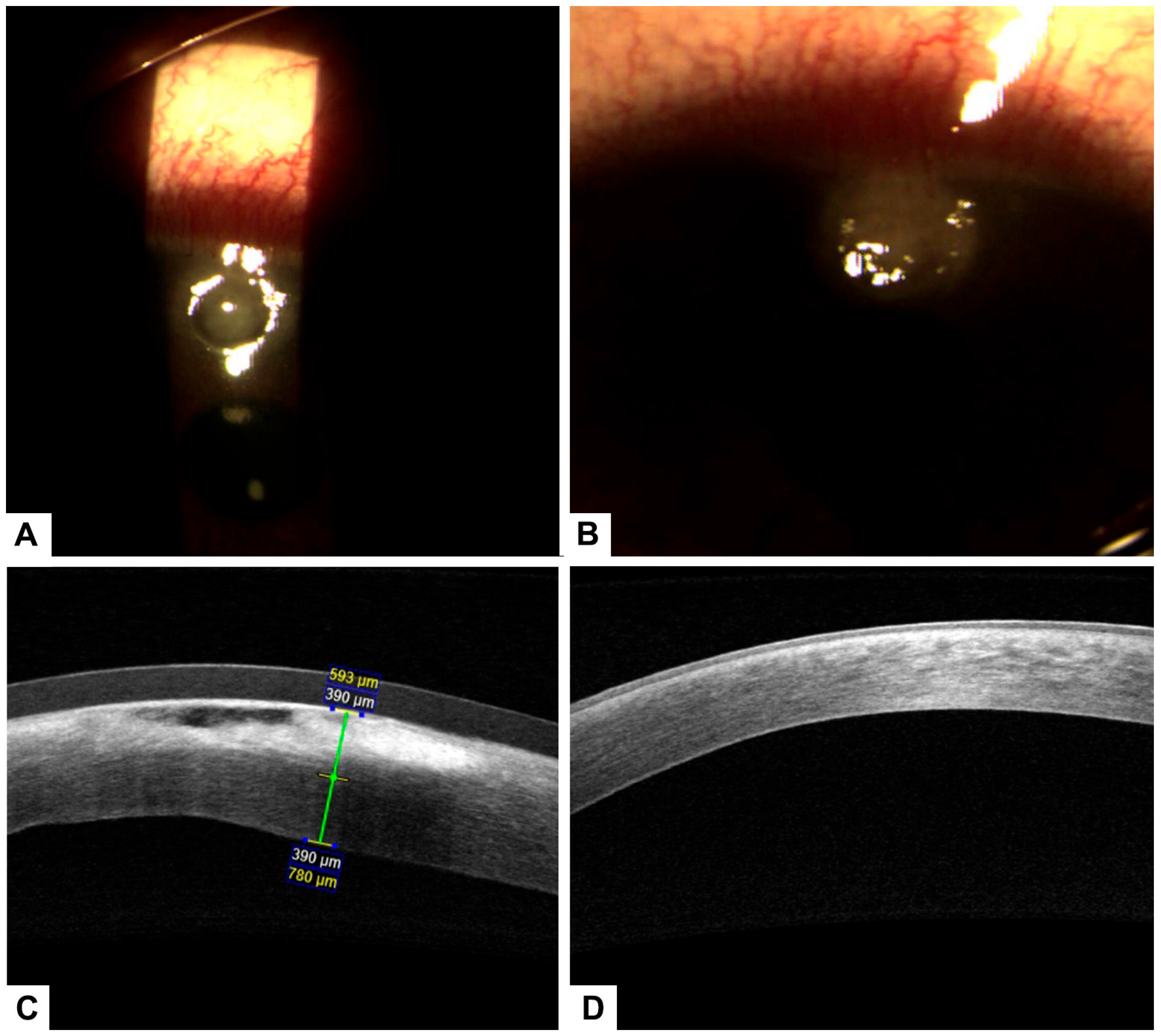
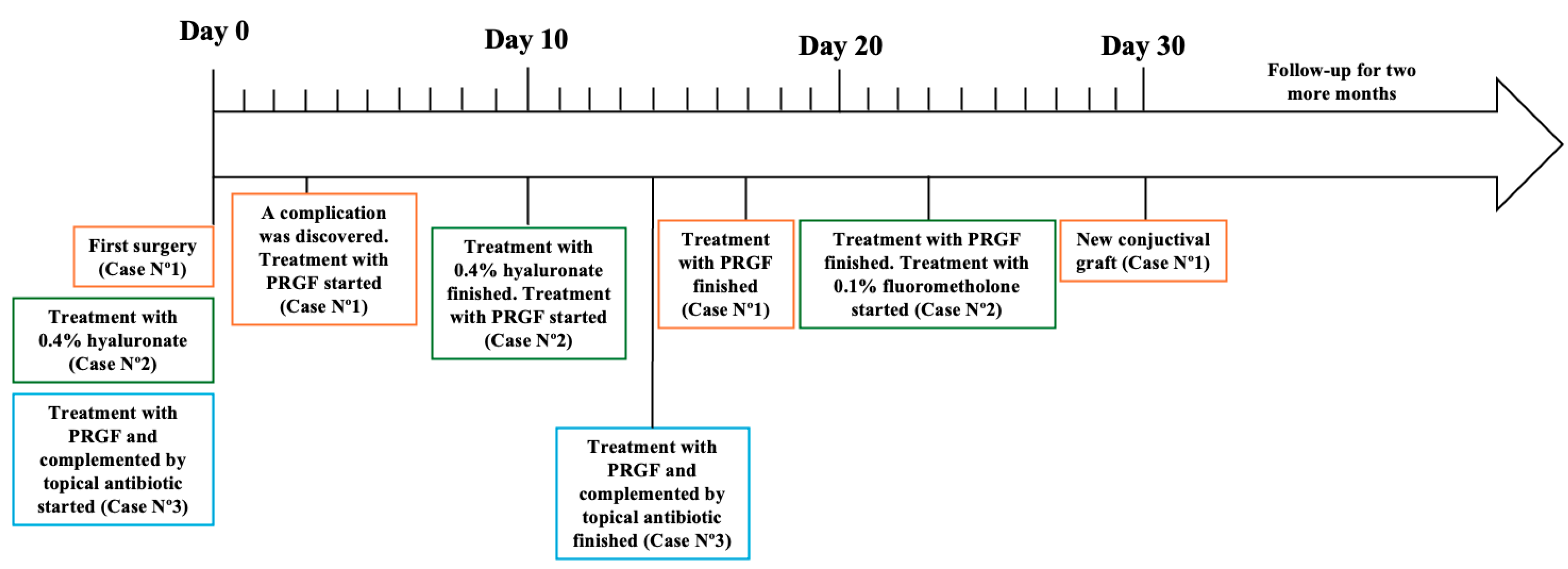
2.1. Clinical Case Nº1
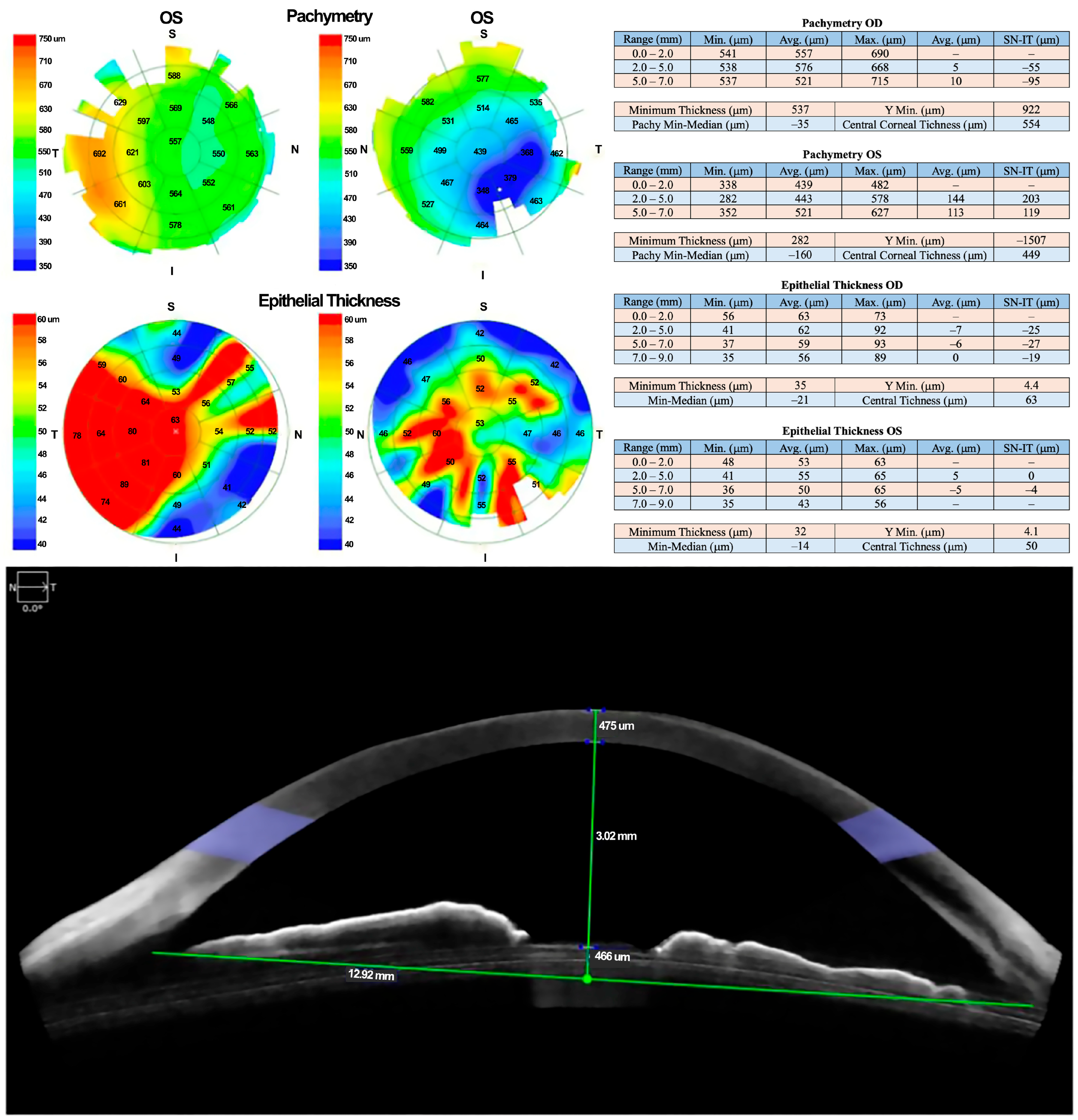
2.2. Clinical Case Nº2
2.3. Clinical Case Nº3
3. Treatment
4. PRGF Preparation
5. Follow-Up
6. Discussion
6.1. Corneal Ulcer Management and the Role of PRGF
6.2. Clinical Applications and Considerations
6.3. Limitations
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Graw, J. Eye development. Curr. Top. Dev. Biol. 2010, 90, 343–386. [Google Scholar] [CrossRef] [PubMed]
- Farghali, H.A.; AbdElKader, N.A.; AbuBakr, H.O.; Ramadan, E.S.; Khattab, M.S.; Salem, N.Y.; Emam, I.A. Corneal Ulcer in Dogs and Cats: Novel Clinical Application of Regenerative Therapy Using Subconjunctival Injection of Autologous Platelet-Rich Plasma. Front. Vet. Sci. 2021, 8, 641265. [Google Scholar] [CrossRef]
- Meer, E.; Grob, S.; Antonsen, E.L.; Sawyer, A. Ocular conditions and injuries, detection and management in spaceflight. npj Microgravity 2023, 9, 37. [Google Scholar] [CrossRef]
- Ahmed, F.; House, R.J.; Feldman, B.H. Corneal abrasions and corneal foreign bodies. Prim. Care 2015, 42, 363–375. [Google Scholar] [CrossRef]
- Bartimote, C.; Foster, J.; Watson, S. The spectrum of microbial keratitis: An updated review. Open Ophthalmol. J. 2019, 13, 100–130. [Google Scholar] [CrossRef]
- Gerstenblith, A.T.; Rabinowitz, M.P. The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2021. [Google Scholar]
- Yang, A.Y.; Chow, J.; Liu, J. Corneal Innervation and Sensation: The Eye and Beyond. Yale J. Biol. Med. 2018, 91, 13–21. [Google Scholar]
- Vacanti, C.A. The history of tissue engineering. J. Cell. Mol. Med. 2006, 10, 569–576. [Google Scholar] [CrossRef] [PubMed]
- Daftarian, N.; Kiani, S.; Zahabi, A. Regenerative therapy for retinal disorders. J. Ophthalmic Vis. Res. 2010, 5, 250–264. [Google Scholar]
- Polykandriotis, E.; Popescu, L.M.; Horch, R.E. Regenerative medicine: Then and now—An update of recent history into future possibilities. J. Cell. Mol. Med. 2010, 14, 2350–2358. [Google Scholar] [CrossRef]
- Jiang, Y.; Li, Y.; Liu, X.W.; Xu, J. A Novel Tectonic Keratoplasty with Femtosecond Laser Intrastromal Lenticule for Corneal Ulcer and Perforation. Chin. Med. J. 2016, 129, 1817–1821. [Google Scholar] [CrossRef]
- Ramaesh, K.; Stone, N.; Dhillon, B. Therapeutic Strategies in Ocular Tissue Regeneration: The Role of Stem Cells. In Strategies in Regenerative Medicine: Integrating Biology with Materials Design; Santin, M., Ed.; Springer: New York, NY, USA, 2009; pp. 1–25. [Google Scholar]
- Ip, M.S.; Domalpally, A.; Hopkins, J.J.; Wong, P.; Ehrlich, J.S. Long-term effects of ranibizumab on diabetic retinopathy severity and progression. Arch. Ophthalmol. 2012, 130, 1145–1152. [Google Scholar] [CrossRef] [PubMed]
- Ho, C.P.S.; Lai, T.Y.Y. Current management strategy of polypoidal choroidal vasculopathy. Indian J. Ophthalmol. 2018, 66, 1727–1735. [Google Scholar] [PubMed]
- Sarao, V.; Veritti, D.; Boscia, F.; Lanzetta, P. Intravitreal Steroids for the Treatment of Retinal Diseases. Sci. World J. 2014, 2014, 989501. [Google Scholar] [CrossRef]
- Gordon, K.; del Medico, A.; Sander, I.; Kumar, A.; Hamad, B. Gene therapies in ophthalmic disease. Nat. Rev. Drug Discov. 2019, 18, 415–416. [Google Scholar] [CrossRef] [PubMed]
- Ellis-Behnke, R.; Jonas, J.B. Redefining tissue engineering for nanomedicine in ophthalmology. Acta Ophthalmol. 2011, 89, e108–e114. [Google Scholar] [CrossRef]
- Zarbin, M.A.; Montemagno, C.; Leary, J.F.; Ritch, R. Regenerative nanomedicine and the treatment of degenerative retinal diseases. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2012, 4, 113–137. [Google Scholar] [CrossRef]
- Hick, S.; Demers, P.E.; Brunette, I.; La, C.; Mabon, M.; Duchesne, B. Amniotic membrane transplantation and fibrin glue in the management of corneal ulcers and perforations: A review of 33 cases. Cornea 2005, 24, 369–377. [Google Scholar] [CrossRef]
- Jhanji, V.; Young, A.L.; Mehta, J.S.; Sharma, N.; Agarwal, T.; Vajpayee, R.B. Management of corneal perforation. Surv. Ophthalmol. 2011, 56, 522–538. [Google Scholar] [CrossRef]
- Alio, J.L.; Rodriguez, A.E.; Wrobel-Dudzinska, D. Eye platelet-rich plasma in the treatment of ocular surface disorders. Curr. Opin. Ophthalmol. 2015, 26, 325–332. [Google Scholar] [CrossRef]
- Petznick, A.; Tong, L.; Chung, R.; Wang, J.C.; Koh, M.; Salleh, R.; Waduthantri, S. Autologous plasma eyedrops prepared in a closed system: A treatment for dry eye. Eye 2013, 27, 1102. [Google Scholar] [CrossRef]
- Alio, J.L.; Arnalich-Montiel, F.; Rodriguez, A.E. The role of “eye platelet rich plasma” (E-PRP) for wound healing in ophthalmology. Curr. Pharm. Biotechnol. 2012, 13, 1257–1265. [Google Scholar] [CrossRef] [PubMed]
- Arnalich, F.; Rodriguez, A.E.; Luque-Rio, A.; Alio, J.L. Solid Platelet Rich Plasma in Corneal Surgery. Ophthalmol. Ther. 2016, 5, 31–45. [Google Scholar] [CrossRef]
- Marx, R.E. Platelet-rich plasma (PRP): What is PRP and what is not PRP? Implant Dent. 2001, 10, 225–228. [Google Scholar] [CrossRef]
- Anitua, E.; Pelacho, B.; Prado, R.; Aguirre, J.J.; Sánchez, M.; Padilla, S.; Aranguren, X.L.; Abizanda, G.; Collantes, M.; Hernandez, M.; et al. Infiltration of plasma rich in growth factors enhances in vivo angiogenesis and improves reperfusion and tissue remodeling after severe hind limb ischemia. J. Control. Release 2015, 202, 31–39. [Google Scholar] [CrossRef]
- Nugent, R.B.; Lee, G.A. Ophthalmic use of blood-derived products. Surv. Ophthalmol. 2015, 60, 406–434. [Google Scholar] [CrossRef]
- Anitua, E.; Sanchez, M.; Orive, G.; Andia, I. Delivering growth factors for therapeutics. Trends Pharmacol. Sci. 2008, 29, 37–41. [Google Scholar] [CrossRef]
- Pavlovic, V.; Ciric, M.; Jovanovic, V.; Stojanovic, P. Platelet Rich Plasma: A short overview of certain bioactive components. Open Med. 2016, 11, 242–247. [Google Scholar] [CrossRef]
- You, J.; Hodge, C.; Hoque, M.; Petsoglou, C.; Sutton, G. Human Platelets and Derived Products in Treating Ocular Surface Diseases—A Systematic Review. Clin. Ophthalmol. 2020, 14, 3195–3210. [Google Scholar] [CrossRef]
- Dang, D.H.; Riaz, K.M.; Karamichos, D. Treatment of Non-Infectious Corneal Injury: Review of Diagnostic Agents, Therapeutic Medications, and Future Targets. Drugs 2022, 82, 145–167. [Google Scholar] [CrossRef]
- Riestra, A.C.; Alonso-Herreros, J.M.; Merayo-Lloves, J. Platelet rich plasma in ocular surface. Arch. Soc. Esp. Oftalmol. 2016, 91, 475–490. [Google Scholar] [CrossRef] [PubMed]
- Tuli, S.S.; Schultz, G.S.; Downer, D.M. Science and strategy for preventing and managing corneal ulceration. Ocul. Surf. 2007, 5, 23–39. [Google Scholar] [CrossRef]
- Bonini, S.; Rama, P.; Olzi, D.; Lambiase, A. Neurotrophic keratitis. Eye 2003, 17, 989–995. [Google Scholar] [CrossRef] [PubMed]
- Anitua, E.; Muruzabal, F.; de la Fuente, M.; Merayo, J.; Duran, J.; Orive, G. Plasma Rich in Growth Factors for the Treatment of Ocular Surface Diseases. Curr. Eye Res. 2016, 41, 875–882. [Google Scholar] [CrossRef]
- Troha, K.; Vozel, D.; Arko, M.; Bedina Zavec, A.; Dolinar, D.; Hočevar, M.; Jan, Z.; Kisovec, M.; Kocjančič, B.; Pađen, L.; et al. Autologous Platelet and Extracellular Vesicle-Rich Plasma as Therapeutic Fluid: A Review. Int. J. Mol. Sci. 2023, 24, 3420. [Google Scholar] [CrossRef] [PubMed]
- Freire, V.; Andollo, N.; Etxebarria, J.; Durán, J.A.; Morales, M.C. In Vitro Effects of Three Blood Derivatives on Human Corneal Epithelial Cells. Investig. Ophthalmol. Vis. Sci. 2012, 53, 5571–5578. [Google Scholar] [CrossRef] [PubMed]
- Anitua, E.; Sanchez, M.; Merayo-Lloves, J.; De la Fuente, M.; Muruzabal, F.; Orive, G. Plasma rich in growth factors (PRGF-Endoret) stimulates proliferation and migration of primary keratocytes and conjunctival fibroblasts and inhibits and reverts TGF-beta1-Induced myodifferentiation. Investig. Ophthalmol. Vis. Sci. 2011, 52, 6066–7603. [Google Scholar] [CrossRef]
- Kang, M.J.; Lee, J.H.; Hwang, J.; Chung, S.H. Efficacy and safety of platelet-rich plasma and autologous-serum eye drops for dry eye in primary Sjögren’s syndrome: A randomized trial. Sci. Rep. 2023, 13, 19279. [Google Scholar] [CrossRef]
- Alio, J.L.; Rodriguez, A.E.; Martinez, L.M. Bovine pericardium membrane (tutopatch) combined with solid platelet-rich plasma for the management of perforated corneal ulcers. Cornea 2013, 32, 619–624. [Google Scholar] [CrossRef] [PubMed]
- Alio, J.L.; Rodriguez, A.E.; Martinez, L.M.; Rio, A.L. Autologous fibrin membrane combined with solid platelet-rich plasma in the management of perforated corneal ulcers: A pilot study. JAMA Ophthalmol. 2013, 131, 745–751. [Google Scholar] [CrossRef]
- Alio, J.L.; Abad, M.; Artola, A.; Rodriguez-Prats, J.L.; Pastor, S.; Ruiz-Colecha, J. Use of autologous platelet-rich plasma in the treatment of dormant corneal ulcers. Ophthalmology 2007, 114, 1286–1293.e1. [Google Scholar] [CrossRef]
- Anitua, E.; Muruzabal, F.; de la Fuente, M.; Merayo-Lloves, J.; Orive, G. Effects of heat-treatment on plasma rich in growth factors-derived autologous eye drop. Exp. Eye Res. 2014, 119, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Avila, R.M.; Uribe-Badillo, E.; Fernandez-Vega Gonzalez, C.; Muruzabal, F.; De la Sen Corcuera, B.; Baamonde, B.; Quirós, L.M.; Anitua, E.; Merayo-Lloves, J. Use of Plasma Rich in Growth Factors and ReGeneraTing Agent Matrix for the Treatment of Corneal Diseases. Vision 2021, 5, 34. [Google Scholar] [CrossRef] [PubMed]
- Anitua, E.; Muruzabal, F.; Alcalde, I.; Merayo-Lloves, J.; Orive, G. Plasma rich in growth factors (PRGF-Endoret) stimulates corneal wound healing and reduces haze formation after PRK surgery. Exp. Eye Res. 2013, 115, 153–161. [Google Scholar] [CrossRef] [PubMed]
- Anitua, E.; Alonso, R.; Girbau, C.; Aguirre, J.J.; Muruzabal, F.; Orive, G. Antibacterial effect of plasma rich in growth factors (PRGF®- Endoret®) against Staphylococcus aureus and Staphylococcus epidermidis strains. Clin. Exp. Dermatol. 2012, 37, 652–657. [Google Scholar] [CrossRef]
- Anitua, E.; de la Fuente, M.; Riestra, A.; Merayo-Lloves, J.; Muruzábal, F.; Orive, G. Preservation of Biological Activity of Plasma and Platelet-Derived Eye Drops After Their Different Time and Temperature Conditions of Storage. Cornea 2015, 34, 1144–1148. [Google Scholar] [CrossRef]
- Anitua, E.; Muruzabal, F.; Pino, A.; Merayo-Lloves, J.; Orive, G. Biological Stability of Plasma Rich in Growth Factors Eye Drops After Storage of 3 Months. Cornea 2013, 32, 1380–1386. [Google Scholar] [CrossRef]
- Kamil, S.; Mohan, R.R. Corneal stromal wound healing: Major regulators and therapeutic targets. Ocul. Surf. 2021, 19, 290–306. [Google Scholar] [CrossRef]

| Parameter | Case Nº1 | Case Nº2 | Case Nº3 |
|---|---|---|---|
| Age/Sex | 65/male | 67/female | 55/male |
| Relevant history | Monocular (right eye phthisis bulbi from trauma) | Type 2 diabetes, left peripheral facial paralysis | Type 2 diabetes, poor control, no regular fundus exam |
| Initial symptoms | 6-month ocular pain, redness, decreased visual acuity in left eye | Five-day ocular pain, deep red eyes, low visual acuity (left eye) | Seven-day foreign body sensation, pain, discharge, decreased vision (left eye) |
| Visual acuity (initial) | Right: NA (phthisis)/left: 20/60 (corrected to 20/40) | Right: 20/40 → 20/20/left: 20/80 | Right: 20/30/left: 20/60 |
| Biomicroscopy | LE: nasal pterygium grade 3, clear cornea with mild involvement | LE: upper corneal ulcer, stromal involvement, pannus, no chamber reaction | LE: corneal ulcer with stromal involvement, foreign body removal attempted |
| OCT findings | Not performed | LE: stromal ulcer without perforation, 2/3 thickness loss | LE: stromal involvement with persistent ulcer |
| Treatment (initial) | Pterygium resection with autograft, tobramycin ointment | Ocular moisturizers (hyaluronate 0.4%) for 7 days | Antibiotics and 4% hyaluronic acid |
| Complications/failure | Graft displacement → scleral exposure → unsuccessful repositioning | No response to initial hydration therapy | No response after 72 h of antibiotic/hyaluronic acid |
| PRGF therapy | Initiated post-graft failure (1 drop q4h for 14 days), followed by autologous serum, then graft | PRGF 1 drop q4h for 14 days → epithelial healing with residual leucoma → steroid remodeling therapy | PRGF 1 drop q4h + antibiotics for 14 days |
| Follow-up findings | Granulation after 48 h serum, full recovery by 30 days | Response by 48–72 h, full healing in 14 days, corneal remodeling with fluorometholone | Ulcer improvement by day 2, VA improved to 20/30 by day 3 |
| Final visual acuity | Left eye: 20/30 | Left eye: 20/40 | Left eye: 20/30 |
| Outcome | Favorable graft recovery, stable IOP, and visual acuity | Leucoma formed but remodeling successful, complete recovery | Significant recovery with PRGF, no further complications |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ortiz, F.; Cárcamo, S.; Souza-Mello, V.; Echeverría, S.; Sandoval, C.; Caamaño, J. Treatment of Corneal Epithelium Lesions with Plasma Rich in Growth Factors: A Case Series and Implications. Healthcare 2025, 13, 2184. https://doi.org/10.3390/healthcare13172184
Ortiz F, Cárcamo S, Souza-Mello V, Echeverría S, Sandoval C, Caamaño J. Treatment of Corneal Epithelium Lesions with Plasma Rich in Growth Factors: A Case Series and Implications. Healthcare. 2025; 13(17):2184. https://doi.org/10.3390/healthcare13172184
Chicago/Turabian StyleOrtiz, Freddy, Sofía Cárcamo, Vanessa Souza-Mello, Sergio Echeverría, Cristian Sandoval, and José Caamaño. 2025. "Treatment of Corneal Epithelium Lesions with Plasma Rich in Growth Factors: A Case Series and Implications" Healthcare 13, no. 17: 2184. https://doi.org/10.3390/healthcare13172184
APA StyleOrtiz, F., Cárcamo, S., Souza-Mello, V., Echeverría, S., Sandoval, C., & Caamaño, J. (2025). Treatment of Corneal Epithelium Lesions with Plasma Rich in Growth Factors: A Case Series and Implications. Healthcare, 13(17), 2184. https://doi.org/10.3390/healthcare13172184








