Exploring the Interplay Among a Health-Promoting Lifestyle, Wellbeing, and Sociodemographic Characteristics in Italy: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Ethical Considerations
2.2. Sample Size Calculation
2.3. Participants
2.4. Measurements
2.5. Data Preparation
- Standardization: Continuous variables (HPLP II total score, WHO-5 total score, NUTR, PHACT, SPGRO, INTRE, HRESP, BMI, and age) were standardized to z-scores to allow for comparison on a common scale. This transformation was crucial for interpreting the relative importance of predictors in the regression analysis;
- Creation of Dummy Variables: The categorical variables (sociodemographics) were converted to dummy variables. This encoding allows for the inclusion of categorical data in the regression model, with one category (the reference category) being excluded to avoid multicollinearity.
2.6. Data Analysis
3. Results
3.1. Descriptive Statistics of the Sample
3.2. Mean HPLP II Scores, Subscales, and Sociodemographic Differences
3.3. Mean WHO-5 Index Score and Cut-Off Point Variations by Sociodemographics
3.4. Correlations Among Health-Promoting Lifestyle, Wellbeing, Age, and BMI
3.5. Regression Analyses of Wellbeing and Health Behaviors
4. Discussion
4.1. Sample Distribution
4.2. HPLB Practice Across Sociodemographics and Wellbeing
4.3. Practical Implications
- Prioritizing the center, the south, and the islands, where HPLBs are less prevalent, by increasing access to healthcare services, encouraging community involvement, and promoting health professional education;
- Boosting health education in middle and high schools, as well as free-access workplace welfare programs across Italy, to foster long-term improvements in HPLBs, particularly among individuals with lower levels of formal education;
- Promoting inclusive and meaningful free activities all over Italy, such as community sports, mindfulness, and volunteer programs, given that PHACT, SPGRO, and INTRE significantly predict wellbeing;
- Encouraging participation in wellness initiatives through economic and environmental policies, including free annual access to personalized physical activity or nutritional plans;
- Building more functional exercise spaces accessible to all ages and increasing the availability of green areas and natural environments in urban settings;
- Enhancing digital literacy among older adults or designing tailored health interventions still using non-digital methods;
- These strategies would reduce health disparities, mortality rates, and hospitalization costs.
4.4. Limits
4.5. Perspectives
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| HPLBs | Health-Promoting Lifestyle Behaviors |
| HPLP II | Health-Promoting Lifestyle Profile II |
| WHO-5 | WHO-5 Wellbeing Index |
| NUTR | Nutrition |
| PHACT | Physical Activity |
| HRESP | Health Responsibility |
| SPGRO | Spiritual Growth |
| INTRE | Interpersonal Relationships |
References
- Brivio, F.; Viganò, A.; Paterna, A.; Palena, N.; Greco, A. Narrative Review and Analysis of the Use of “Lifestyle” in Health Psychology. Int. J. Environ. Res. Public Health 2023, 20, 4427. [Google Scholar] [CrossRef]
- Savarese, G.; Carpinelli, L.; Cavallo, P.; Vitale, M.P. Italian Psychometric Validation of the Multidimensional Students’ Health-Promoting Lifestyle Profile Scale. Health 2018, 10, 1554–1575. [Google Scholar] [CrossRef]
- McLeroy, K.R.; Bibeau, D.; Cavallo, P.; Steckler, A.; Glanz, K. An Ecological Perspective on Health Promotion Programs. Health Educ. Q. 1988, 15, 351–377. [Google Scholar] [CrossRef]
- Bronfenbrenner, U. Ecological Models of Human Development. In International Encyclopedia of Education; Elsevier: Oxford, UK, 1994; Volume 3. [Google Scholar]
- World Health Organization. Social Determinants of Health. Available online: https://www.who.int/health-topics/social-determinants-of-health (accessed on 7 August 2025).
- Marino, P.; Mininni, M.; Deiana, G.; Marino, G.; Divella, R.; Bochicchio, I.; Giuliano, A.; Lapadula, S.; Lettini, A.R.; Sanseverino, F. Healthy Lifestyle and Cancer Risk: Modifiable Risk Factors to Prevent Cancer. Nutrients 2024, 16, 800. [Google Scholar] [CrossRef]
- Dominguez, L.J.; Veronese, N.; Vernuccio, L.; Catanese, G.; Inzerillo, F.; Salemi, G.; Barbagallo, M. Nutrition, Physical Activity, and Other Lifestyle Factors in the Prevention of Cognitive Decline and Dementia. Nutrients 2021, 13, 4080. [Google Scholar] [CrossRef]
- Wang, J.; Chen, C.; Zhou, J.; Ye, L.; Li, Y.; Xu, L.; Xu, Z.; Li, X.; Wei, Y.; Liu, J.; et al. Healthy Lifestyle in Late-Life, Longevity Genes, and Life Expectancy among Older Adults: A 20-Year, Population-Based, Prospective Cohort Study. Lancet Healthy Longev. 2023, 4, e535–e543. [Google Scholar] [CrossRef]
- Moscatelli, F.; De Maria, A.; Marinaccio, L.A.; Monda, V.; Messina, A.; Monacis, D.; Toto, G.; Limone, P.; Monda, M.; Messina, G.; et al. Assessment of Lifestyle, Eating Habits and the Effect of Nutritional Education among Undergraduate Students in Southern Italy. Nutrients 2023, 15, 2894. [Google Scholar] [CrossRef]
- Carballo-Fazanes, A.; Rico-Díaz, J.; Barcala-Furelos, R.; Rey, E.; Rodríguez-Fernández, J.E.; Varela-Casal, C.; Abelairas-Gómez, C. Physical Activity Habits and Determinants, Sedentary Behaviour and Lifestyle in University Students. Int. J. Environ. Res. Public Health 2020, 17, 3272. [Google Scholar] [CrossRef]
- Müller, C.; El-Ansari, K.; El Ansari, W. Health-Promoting Behavior and Lifestyle Characteristics of Students as a Function of Sex and Academic Level. Int. J. Environ. Res. Public Health 2022, 19, 7539. [Google Scholar] [CrossRef]
- Flesia, L.; Cavalieri, F.; Angelini, S.; Bottesi, G.; Ghisi, M.; Tonon, E.; Roldan, A.P.; Di Nisio, A.; Garolla, A.; Ferlin, A.; et al. Health-Related Lifestyles, Substance-Related Behaviors, and Sexual Habits Among Italian Young Adult Males: An Epidemiologic Study. Sex. Med. 2020, 8, 361–369. [Google Scholar] [CrossRef]
- Christodoulou, E.; Poutli, E.; Andreou, D.; Laoutari, S.; Athanasiou, F.; Kourkoutas, Y.; Koutelidakis, A.E. Towards a Thriving Workplace: A Feasibility Study on Mindfulness and the Mediterranean Lifestyle for Corporate Wellness. Healthcare 2025, 13, 9. [Google Scholar] [CrossRef]
- Deslippe, A.L.; Soanes, A.; Bouchaud, C.C.; Beckenstein, H.; Slim, M.; Plourde, H.; Cohen, T.R. Barriers and Facilitators to Diet, Physical Activity and Lifestyle Behavior Intervention Adherence: A Qualitative Systematic Review of the Literature. Int. J. Behav. Nutr. Phys. Act. 2023, 20, 14. [Google Scholar] [CrossRef]
- Italia, Regioni, Province. ISTAT Istituto Nazionale di Statistica. 2025. Available online: https://esploradati.istat.it (accessed on 1 May 2025).
- Unequal Italy: Regional Socio-Economic Disparities in Italy. Foundation for European Progressive Studies (FEPS). 2021. Available online: https://feps-europe.eu/wp-content/uploads/2021/07/Unequal-Italy-Regional-socio-economic-disparities-in-Italy.pdf (accessed on 5 August 2025).
- Well-Being and Inequalities. Istat Istituto Nazionale di Statistica. 2024. Available online: https://www.istat.it/wp-content/uploads/2024/11/Well-being-and-inequalities.pdf (accessed on 5 August 2025).
- Petrelli, A.; Ventura, M.; Di Napoli, A.; Pappagallo, M.; Simeoni, S.; Frova, L. Socioeconomic Inequalities in Avoidable Mortality in Italy: Results from a Nationwide Longitudinal Cohort. BMC Public Health 2024, 24, 757. [Google Scholar] [CrossRef]
- Battel-Kirk, B.; Barry, M.M. Implementation of Health Promotion Competencies in Ireland and Italy—A Case Study. Int. J. Environ. Res. Public Health 2019, 16, 4992. [Google Scholar] [CrossRef]
- Abatemarco, A.; Aria, M.; Beraldo, S.; Collaro, M. Measuring Health Care Access and Its Inequality: A Decomposition Approach. Econ. Model. 2024, 132, 106659. [Google Scholar] [CrossRef]
- Antonelli, M.A.; Marini, G. Do Institutions Matter for Citizens’ Health Status? Empirical Evidence from Italy. Eur. J. Health Econ. 2024, 26, 95–115. [Google Scholar] [CrossRef] [PubMed]
- Miola, L.; Pazzaglia, F. Perceived Restorativeness and Environment Quality in Relation to Well-Being, Residential Satisfaction, and Sense of Community: An Analysis in Northeast Italy. Front. Psychol. 2025, 16, 1522098. [Google Scholar] [CrossRef]
- Serdar, C.C.; Cihan, M.; Yücel, D.; Serdar, M.A. Sample Size, Power and Effect Size Revisited: Simplified and Practical Approachin Pre-Clinical, Clinical and Laboratory Studies. Biochem. Med. 2021, 31, 27–53. [Google Scholar] [CrossRef]
- Lau, F.; Kuziemsky, C. Handbook of EHealth Evaluation: An Evidence-Based Approach; University of Victoria: Victoria, BC, Canada, 2017. Available online: https://www.ncbi.nlm.nih.gov/books/NBK481590/ (accessed on 5 August 2025).
- Fink, A. The Survey Handbook; Sage Publications: Thousand Oaks, CA, USA, 2003. [Google Scholar]
- Fink, A. How to Sample in Surveys; Sage Publications: Thousand Oaks, CA, USA, 2005. [Google Scholar]
- Fowler, F.J. Survey Research Methods, 4th ed.; Sage Publications: Thousand Oaks, CA, USA, 2009. [Google Scholar]
- Sedgwick, P. Snowball Sampling. BMJ 2013, 347, f7511. [Google Scholar] [CrossRef]
- Chambers, M.; Bliss, K.; Rambur, B. Recruiting Research Participants via Traditional Snowball vs Facebook Advertisements and a Website. West. J. Nurs. Res. 2020, 42, 846–851. [Google Scholar] [CrossRef]
- Moghimi, A.; Saberi Isfeedvajani, M.; Javanbakht, M.; Khedmat, L. Health-Promoting Lifestyle Behaviors and Its Association with Sociodemographic Characteristics in Hospital Clinical Staff. Front. Public Health 2024, 12, 1391094. [Google Scholar] [CrossRef]
- Link, E.; Baumann, E.; Linn, A.; Fahr, A.; Schulz, P.; Abuzahra, M.E. Influencing Factors of Online Health Information Seeking in Selected European Countries. Eur. J. Health Commun. 2021, 2, 29–55. [Google Scholar] [CrossRef]
- Walker, S.N.; Sechrist, K.R.; Pender, N.J. Health Promotion Model-Instruments to Measure Health Promoting Lifestyle: Health-Promoting Lifestyle Profile [HPLP II]. 1995. Available online: https://deepblue.lib.umich.edu/handle/2027.42/85349 (accessed on 5 August 2025).
- Topp, C.W.; Østergaard, S.D.; Søndergaard, S.; Bech, P. The WHO-5 Well-Being Index: A Systematic Review of the Literature. Psychother. Psychosom. 2015, 84, 167–176. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: New York, NY, USA, 2013. [Google Scholar]
- Cureton, E.E. Rank-biserial correlation. Psychometrika 1956, 21, 287–290. [Google Scholar] [CrossRef]
- Cohen, J. A Power Primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef]
- Tomczak, M.; Tomczak, E. The Need to Report Effect Size Estimates Revisited. An Overview of Some Recommended Measures of Effect Size. Trends Sport. Sci. 2014, 1, 19–25. [Google Scholar]
- Yigit, S.; Mendes, M. Which Effect Size Measure Is Appropriate for One-Way and Two-Way ANOVA Models? REVSTAT-Stat. J. 2018, 16, 295–313. [Google Scholar] [CrossRef]
- Mukaka, M.M. Statistics Corner: A Guide to Appropriate Use of Correlation Coefficient in Medical Research. Malawi Med. J. 2012, 24, 69–71. [Google Scholar]
- Cramér, H. Mathematical Methods of Statistics (PMS-9); Princeton University Press: Princeton, NJ, USA, 2016. [Google Scholar]
- Bilancio Demografico Mensile Gennaio 2025. ISTAT Istituto Nazionale di Statistica. 2025. Available online: https://www.istat.it (accessed on 1 May 2025).
- Becker, R. Gender and Survey Participation an Event History Analysis of the Gender Effects of Survey Participation in a Probability-Based Multi-Wave Panel Study with a Sequential Mixed-Mode Design. GESIS-Leibniz Inst. Soc. Sci. 2022, 16. [Google Scholar] [CrossRef]
- Bussola, M.; Cecconi, N.; Donati, E.; Porciani, L. Respondents and Non Respondents to Population and Housing Census: Some Strategies for Data Collection Design in the Era of Low Response Rate and High Response Burden. An Application of a Decision Tree Model. Riv. Ital. Econ. Demogr. Stat. 2024, 31–42. [Google Scholar] [CrossRef]
- Competenze Digitali e Caratteristiche Socio-Culturali Della Popolazione: Forti Divari. CITTADINI E ICT|ANNO 2023. ISTAT Istituto Nazionale di Statistica. 2023. Available online: www.istat.it (accessed on 1 May 2025).
- Golinelli, D.; Bucci, A.; Boetto, E.; Maietti, E.; Toscano, F.; Fantini, M.P. Gender Differences and Multiple Determinants of Perceived Physical and Mental Health in Italy. Ann. Ig. 2021, 33, 456–473. [Google Scholar] [CrossRef]
- Mistura, L.; Donne, C.L.; D’Addezio, L.; Ferrari, M.; Comendador, F.J.; Piccinelli, R.; Martone, D.; Sette, S.; Catasta, G.; Turrini, A. The Italian IV SCAI Dietary Survey: Main Results on Food Consumption. Nutr. Metab. Cardiovasc. Dis. 2025, 35, 103863. [Google Scholar] [CrossRef]
- Bojang, K.P.; Manchana, V. Nutrition and Healthy Aging: A Review. Curr. Nutr. Rep. 2023, 12, 369–375. [Google Scholar] [CrossRef] [PubMed]
- Gropper, S.S. The Role of Nutrition in Chronic Disease. Nutrients 2023, 15, 664. [Google Scholar] [CrossRef] [PubMed]
- Pellerone, M.; Martinez Torvisco, J.; Razza, S.G.; Lo Piccolo, A.; Guarnera, M.; La Rosa, V.L.; Commodari, E. Relational Competence, School Adjustment and Emotional Skills: A Cross-Sectional Study in a Group of Junior and High School Students of the Sicilian Hinterland. Int. J. Environ. Res. Public Health 2023, 20, 2182. [Google Scholar] [CrossRef] [PubMed]
- Nomaguchi, K.; Milkie, M.A. Parenthood and Well-Being: A Decade in Review. J. Marriage Fam. 2020, 82, 198–223. [Google Scholar] [CrossRef]
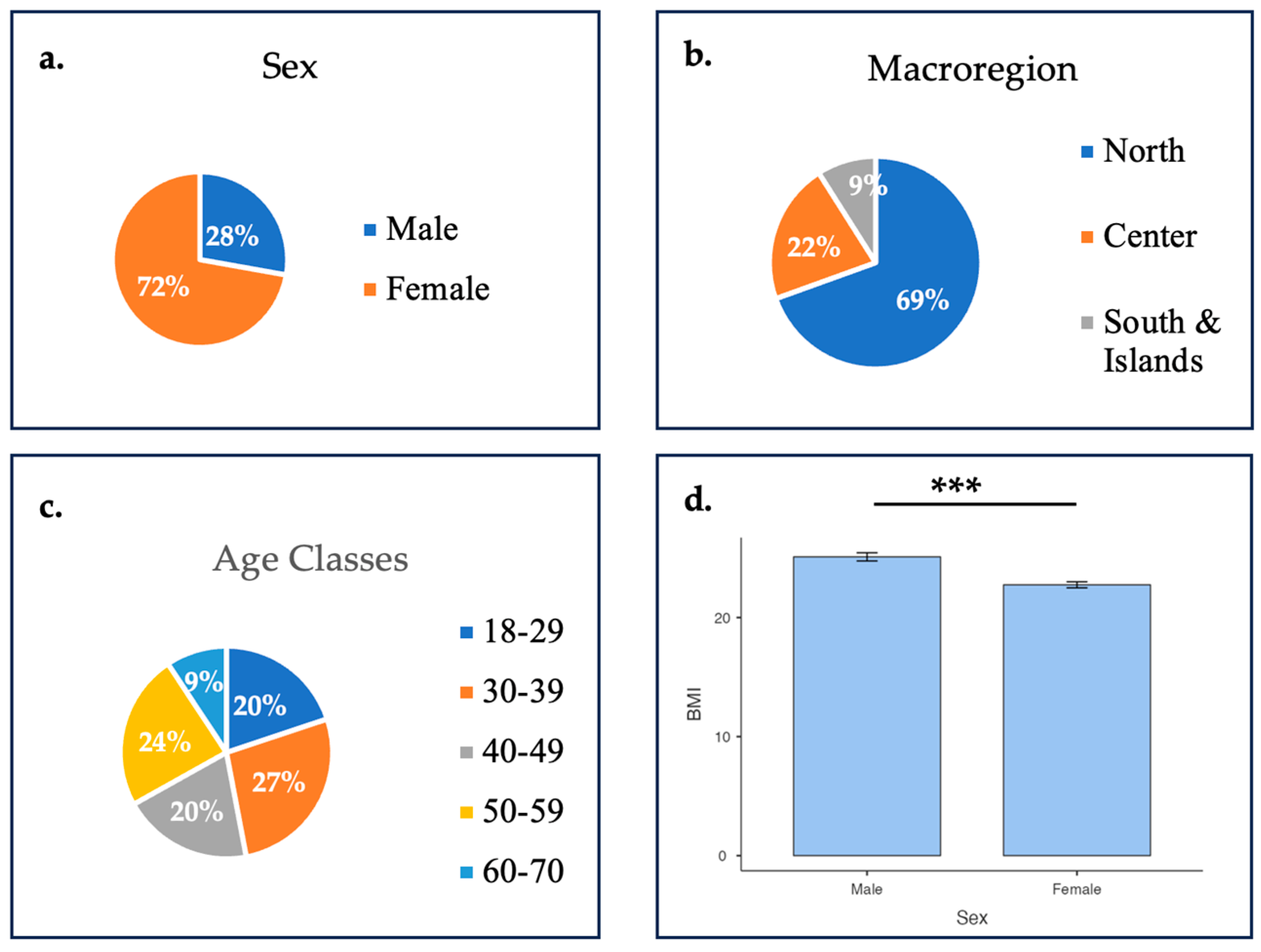
| Sociodemographic Factor | Percentage (N) |
|---|---|
| Sex | |
| Male | 27.8% (84) |
| Female | 72.2% (218) |
| Age classes | |
| 18–29 | 19.9% (60) |
| 30–39 | 27.1% (82) |
| 40–49 | 19.9% (60) |
| 50–59 | 23.8% (72) |
| 60–70 | 9.3% (28) |
| Macroregions | |
| North | 69.5% (210) |
| Center | 21.5% (65) |
| South and Islands | 8.9% (27) |
| Education | |
| Middle school | 2.3% (7) |
| High school | 29.8% (90) |
| University | 68% (205) |
| Employment | |
| Student | 8.9% (27) |
| Unemployed | 2.6% (8) |
| Employed | 85.1% (257) |
| Retired | 3.3% (10) |
| Housing | |
| Living with u18 and other adults | 8% (25) |
| Living with u18 | 9% (28) |
| Living with other adults | 58% (174) |
| Living alone | 25% (75) |
| Financial status | |
| Worsened | 9% (28) |
| Unchanged | 69% (207) |
| Improved | 22% (67) |
| Chronic disease | |
| Yes | 14% (41) |
| No | 86% (261) |
| Questionnaire Results | Total Score Mean ± SD (% ON MAX Scoring) |
|---|---|
| WHO-5 total score | 16 ± 3.63 (64.4%) |
| HPLP II total score | 69.1 ± 11.3 (66%) |
| HPLP II subscales | |
| NUTR | 2.57 ± 0.62 |
| SPGRO | 2.87 ± 0.58 |
| PHACT | 2.37 ± 0.70 |
| INTRE | 2.92 ± 0.48 |
| HRESP | 2.39 ± 0.65 |
| Variable | HPLP II Total Score | NUTR | PHACT | INTRE | HRESP | SPGRO |
|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean± SD | Mean ± SD | Mean ± SD | Mean ± SD | |
| Sex | ||||||
| Male | 69.5 ± 11.00 | 2.51 ± 0.60 | 2.49 ± 0.67 | 2.87 ± 0.48 | 2.23 ± 0.65 | 2.98 ± 0.57 |
| Female | 68.9 ± 11.4 | 2.59 ± 0.62 | 2.32 ± 0.71 | 2.93 ± 0.48 | 2.45 ± 0.64 | 2.83 ± 0.58 |
| p-value 1 | p = 0.72 | p = 0.26 | p = 0.056 | p = 0.25 | p = 0.002 ** | p = 0.098 |
| ES | d = 0.05 | r = 0.08 | r = −0.14 | r = 0.08 | r = 0.22 | r = −0.12 |
| Age Classes | ||||||
| 18–29 | 67.5 ± 12.0 | 2.39 ± 0.65 a | 2.37 ± 0.77 | 3.00 ± 0.50 | 2.31 ± 0.67 | 2.79 ± 0.62 |
| 30–39 | 70.3 ± 11.30 | 2.60 ± 0.64 ab | 2.32 ± 0.72 | 2.97 ± 0.45 | 2.47 ± 0.64 | 2.93 ± 0.56 |
| 40–49 | 69.0 ± 10.70 | 2.49 ± 0.65 a | 2.36 ± 0.65 | 2.94 ± 0.42 | 2.35 ± 0.71 | 2.98 ± 0.53 |
| 50–59 | 68.4 ± 11.60 | 2.64 ± 0.53 ab | 2.38 ± 0.69 | 2.80 ± 0.50 | 2.36 ± 0.61 | 2.85 ± 0.59 |
| 60–70 | 70.6 ± 9.92 | 2.87 ± 0.50 b | 2.48 ± 0.60 | 2.84 ± 0.52 | 2.50 ± 0.57 | 2.70 ± 0.56 |
| p-value 2 | p = 0.583 | p = 0.008 ** | p = 0.875 | p = 0.111 | p = 0.387 | p = 0.118 |
| ES | ω2 = −0.004 | ε2 = 0.05 # | ε2 = 0.004 | ε2 = 0.02 | ε2 = 0.01 | ε2 = 0.02 |
| Macroregions | ||||||
| North | 70.3 ± 11.00 | 2.64 ± 0.62 a | 2.41 ± 0.70 | 2.96 ± 0.46 | 2.42 ± 0.63 | 2.89 ± 0.57 |
| Center | 66.6 ± 11.90 | 2.45 ± 0.56 b | 2.26 ± 0.68 | 2.82 ± 0.55 | 2.36 ± 0.71 | 2.78 ± 0.62 |
| South and Islands | 65.6 ± 10.70 | 2.30 ± 0.60 b | 2.26 ± 0.73 | 2.79 ± 0.46 | 2.22 ± 0.65 | 2.91 ± 0.55 |
| p-value 2 | p = 0.017 N.S. | p = 0.005 ** | p = 0.192 | p = 0.063 | p = 0.354 | p = 0.205 |
| ES | ω2 = 0.02 | ε2 = 0.04 | ε2 = 0.01 | ε2 = 0.02 | ε2 = 0.01 | ε2 = 0.01 |
| Education | ||||||
| Middle school | 61.1 ± 5.93 | 2.17 ± 0.45 | 1.91 ± 0.65 | 2.54 ± 0.30 a | 2.03 ± 0.49 | 2.74 ± 0.55 |
| High school | 67.3 ± 10.80 | 2.54 ± 0.61 | 2.38 ± 0.67 | 2.83 ± 0.47 ab | 2.28 ± 0.60 | 2.79 ± 0.53 |
| University | 70.1 ± 11.40 | 2.60 ± 0.62 | 2.38 ± 0.71 | 2.97 ± 0.48 b | 2.45 ± 0.66 | 2.91 ± 0.60 |
| p-value 2 | p = 0.022 N.S. | p = 0.179 | p = 0.234 | p= 0.006 ** | p = 0.025 N.S. | p = 0.123 |
| ES | ω2 = 0.02 | ε2 = 0.01 | ε2 = 0.01 | ε2 = 0.03 | ε2 = 0.02 | ε2 = 0.01 |
| Employment | ||||||
| Student | 70.0 ± 12.30 | 2.43 ± 0.67 | 2.50 ± 0.72 | 3.09 ± 0.55 | 2.35 ± 0.73 | 2.92 ± 0.67 |
| Unemployed | 67.3 ± 13.10 | 2.52 ± 0.89 | 2.50 ± 0.71 | 2.75 ± 0.32 | 2.52 ± 0.79 | 2.60 ± 0.59 |
| Employed | 69.1 ± 11.20 | 2.58 ± 0.61 | 2.35 ± 0.71 | 2.92 ± 0.47 | 2.40 ± 0.64 | 2.89 ± 0.56 |
| Retired | 67.1 ± 8.75 | 2.80 ± 0.39 | 2.45 ± 0.49 | 2.64 ± 0.39 | 2.29 ± 0.54 | 2.56 ± 0.73 |
| p-value 2 | p = 0.876 | p = 0.352 | p = 0.718 | p = 0.044 N.S. | p = 0.750 | p = 0.150 |
| ES | ω2 = −0.01 | ε2 = 0.01 | ε2 = 0.004 | ε2 = 0.03 | ε2 = 0.004 | ε2 = 0.02 |
| Housing | ||||||
| Living with u18 and other adults | 73.5 ± 10.30 | 2.74 ± 0.51 | 2.42 ± 0.76 | 3.06 ± 0.43 | 2.73 ± 0.65 a | 3.09 ± 0.45 |
| Living with u18 | 70.3 ± 12.20 | 2.46 ± 0.52 | 2.38 ± 0.63 | 3.09 ± 0.47 | 2.46 ± 0.72 ab | 3.10 ± 0.62 |
| Living with other adults | 68.4 ± 11.00 | 2.56 ± 0.62 | 2.33 ± 0.69 | 2.88 ± 0.48 | 2.35 ± 0.64 b | 2.84 ± 0.57 |
| Living alone | 68.8 ± 11.60 | 2.58 ± 0.66 | 2.44 ± 0.74 | 2.89 ± 0.48 | 2.34 ± 0.61 c | 2.79 ± 0.60 |
| p-value 2 | p = 0.177 | p = 0.256 | p = 0.665 | p = 0.057 | p = 0.038 * | p = 0.016 N.S. |
| ES | ω2 = 0.006 | ε2 = 0.01 | ε2 = 0.005 | ε2 = 0.02 | ε2 = 0.03 | ε2 = 0.03 |
| Financial Status | ||||||
| Worsened | 62.9 ± 10.90 a | 2.47 ± 0.64 | 2.23 ± 0.66 | 2.56 ± 0.45 a | 2.34 ± 0.65 | 2.38 ± 0.51 a |
| Unchanged | 68.8 ± 10.80 b | 2.57 ± 0.60 | 2.35 ± 0.68 | 2.89 ± 0.46 b | 2.41 ± 0.65 | 2.86 ± 0.55 b |
| Improved | 72.5 ± 11.70 c | 2.60 ± 0.65 | 2.48 ± 0.78 | 3.16 ± 0.43 c | 2.37 ± 0.64 | 3.10 ± 0.53 c |
| p-value 2 | p < 0.001 *** | p = 0.567 | p = 0.192 | p< 0.001 *** | p = 0.711 | p< 0.001 *** |
| ES | ω2 = 0.04 | ε2 = 0.003 | ε2 = 0.01 | ε2 = 0.10 # | ε2 = 0.002 | ε2 = 0.09 # |
| Chronic Disease | ||||||
| Yes | 70.2 ± 9.90 | 2.79 ± 0.55 | 2.36 ± 0.68 | 2.99 ± 0.47 | 2.50 ± 0.677 | 2.84 ± 0.60 |
| No | 68.9 ± 11.50 | 2.54 ± 0.62 | 2.37 ± 0.70 | 2.91 ± 0.48 | 2.37 ± 0.642 | 2.88 ± 0.58 |
| p-value 1 | p = 0.498 | p= 0.014 * | p = 0.943 | p = 0.172 | p = 0.309 | p = 0.562 |
| ES | d = −0.11 | r = 0.24 | r = 0.007 | r = 0.13 | r = 0.09822 | r = −0.05 |
| WHO-5 Cut-Off Point | Worsened (Expected) | Unchanged (Expected) | Improved (Expected) | χ2 | V | p-VALUE | EFFECT |
|---|---|---|---|---|---|---|---|
| >13 | 16 (21.9) | 163 (162.4) | 58 (52.6) | ||||
| % | 6.8 (9.2) | 68.8 (68.5) | 24.5 (22.2) | ||||
| <13 | 12 (6) | 44 (44.6) | 9 (14.4) | ||||
| % | 18.5 (9%) | 67.7 (68.6) | 13.8 (22.1) | ||||
| 10.1 | 0.18 | 0.006 | Strong |
| Variables | WHO-5 TS | HPLP II TS | PHACT | INTRE | HRESP | SPGRO |
|---|---|---|---|---|---|---|
| Ρ | r | ρ | ρ | ρ | ρ | |
| AGE | 0.116 * | 0.001 | ||||
| BMI | 0.017 | −0.090 | ||||
| HPLP II TOTAL SCORE | 0.246 *** | - | ||||
| NUTR | 0.133 * | - | 0.487 *** | 0.254 *** | 0.359 *** | 0.313 *** |
| PHACT | 0.164 ** | - | - | 0.275 *** | 0.228 *** | 0.429 *** |
| INTRE | 0.146 ** | - | - | 0.379 *** | 0.616 *** | |
| HRESP | 0.034 | - | - | 0.310 *** | ||
| SPGRO | 0.360 *** | - |
| Coefficients a | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Model | Unstandardized Coefficients | Standardized Coefficient | t | Sig. | 95.0% Confidence Interval for B | Collinearity Statistics | ||||
| B | Std. Error | Beta | Lower Bound | Upper Bound | Tolerance | VIF | ||||
| 1 | (Constant) | 76.832 | 2.610 | 29.439 | 0.000 | 71.695 | 81.969 | |||
| Macroregion_of_residence_2 | −4.255 | 1.572 | −0.156 | −2.707 | 0.007 | −7.349 | −1.161 | 0.915 | 1.092 | |
| Macroregion_of_residence_3 | −5.014 | 2.292 | −0.127 | −2.188 | 0.030 | −9.526 | −0.503 | 0.893 | 1.119 | |
| Education_1 | −7.137 | 4.199 | −0.096 | −1.699 | 0.090 | −15.403 | 1.129 | 0.957 | 1.045 | |
| Education_2 | −3.179 | 1.450 | −0.129 | −2.192 | 0.029 | −6.033 | −0.324 | 0.869 | 1.151 | |
| Employment_1 | 3.903 | 2.549 | 0.099 | 1.531 | 0.127 | −1.115 | 8.921 | 0.722 | 1.385 | |
| Employment_2 | 2.124 | 4.007 | 0.030 | 0.530 | 0.596 | −5.763 | 10.011 | 0.923 | 1.084 | |
| Employment_4 | −2.137 | 3.751 | −0.034 | −0.570 | 0.569 | −9.521 | 5.247 | 0.848 | 1.179 | |
| Chronic_desease_2 | −2.136 | 1.874 | −0.065 | −1.140 | 0.255 | −5.826 | 1.553 | 0.927 | 1.079 | |
| Housing_1 | 0.745 | 1.528 | 0.029 | 0.488 | 0.626 | −2.262 | 3.752 | 0.877 | 1.140 | |
| Housing_3 | 2.936 | 2.308 | 0.076 | 1.272 | 0.204 | −1.608 | 7.480 | 0.852 | 1.173 | |
| Housing_4 | 5.111 | 2.356 | 0.125 | 2.169 | 0.031 | 0.473 | 9.749 | 0.906 | 1.103 | |
| Financial_status_1 | −9.546 | 2.531 | −0.246 | −3.772 | 0.000 | −14.527 | −4.565 | 0.709 | 1.410 | |
| Financial_status_2 | −3.923 | 1.593 | −0.162 | −2.463 | 0.014 | −7.058 | −0.788 | 0.698 | 1.432 | |
| Sex_2 | −1.474 | 1.528 | −0.059 | −0.965 | 0.335 | −4.481 | 1.533 | 0.815 | 1.226 | |
| Z-score: Age | 1.116 | 0.786 | 0.099 | 1.420 | 0.157 | −0.431 | 2.664 | 0.620 | 1.612 | |
| Z-score: BMI | −1.239 | 0.678 | −0.110 | −1.829 | 0.068 | −2.573 | 0.094 | 0.835 | 1.197 | |
| Coefficients a | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Model | Unstandardized Coefficients | Standardized Coefficient | t | Sig. | 95.0% Confidence Interval for B | Collinearity Statistics | ||||
| B | Std. Error | Beta | Lower Bound | Upper Bound | Tolerance | VIF | ||||
| 1 | (Constant) | 16.811 | 0.874 | 19.231 | 0.000 | 15.090 | 18.532 | |||
| Sex_2 | −0.812 | 0.512 | −0.100 | −1.588 | 0.113 | −1.820 | 0.195 | 0.815 | 1.226 | |
| Macroregion_of_residence_2 | 0.460 | 0.527 | 0.052 | 0.874 | 0.383 | −0.576 | 1.497 | 0.915 | 1.092 | |
| Macroregion_of_residence_3 | 1.266 | 0.768 | 0.100 | 1.649 | 0.100 | −0.245 | 2.777 | 0.893 | 1.119 | |
| Education_1 | −0.977 | 1.407 | −0.041 | −0.695 | 0.488 | −3.746 | 1.791 | 0.957 | 1.045 | |
| Education_2 | −0.643 | 0.486 | −0.081 | −1.323 | 0.187 | −1.599 | 0.313 | 0.869 | 1.151 | |
| Employment_1 | −0.458 | 0.854 | −0.036 | −0.537 | 0.592 | −2.139 | 1.223 | 0.722 | 1.385 | |
| Employment_2 | −1.451 | 1.342 | −0.064 | −1.081 | 0.281 | −4.092 | 1.191 | 0.923 | 1.084 | |
| Employment_4 | 1.463 | 1.256 | 0.072 | 1.164 | 0.245 | −1.010 | 3.936 | 0.848 | 1.179 | |
| Chronic_disease_2 | 0.771 | 0.628 | 0.073 | 1.229 | 0.220 | −0.464 | 2.007 | 0.927 | 1.079 | |
| Housing_1 | −0.470 | 0.512 | −0.056 | −0.918 | 0.359 | −1.477 | 0.537 | 0.877 | 1.140 | |
| Housing_3 | −0.315 | 0.773 | −0.025 | −0.407 | 0.684 | −1.837 | 1.207 | 0.852 | 1.173 | |
| Housing_4 | −0.068 | 0.789 | −0.005 | −0.086 | 0.931 | −1.621 | 1.485 | 0.906 | 1.103 | |
| Financial_status_1 | −1.608 | 0.848 | −0.129 | −1.897 | 0.059 | −3.277 | 0.060 | 0.709 | 1.410 | |
| Financial_status_2 | −0.697 | 0.534 | −0.089 | −1.307 | 0.192 | −1.748 | 0.353 | 0.698 | 1.432 | |
| Z-score: Age | 0.506 | 0.263 | 0.139 | 1.922 | 0.056 | −0.012 | 1.024 | 0.620 | 1.612 | |
| Z-score: BMI | −0.043 | 0.227 | −0.012 | −0.189 | 0.850 | −0.490 | 0.404 | 0.835 | 1.197 | |
| Coefficients a | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Model | Unstandardized Coefficients | Standardized Coefficient | t | Sig. | 95,0% Confidence Interval for B | Collinearity Statistics | ||||
| B | Std. Error | Beta | Lower Bound | Upper Bound | Tolerance | VIF | ||||
| 1 | (Constant) | 69.086 | 0.123 | 560.955 | 0.000 | 68.844 | 69.328 | |||
| Z-score: Nutrition | 3.815 | 0.146 | 0.339 | 26.041 | 0.000 | 3.526 | 4.103 | 0.709 | 1.410 | |
| Z-score: Spiritual Growth | 3.176 | 0.167 | 0.282 | 18.994 | 0.000 | 2.847 | 3.505 | 0.544 | 1.837 | |
| Z-score: Physical Activity | 3.588 | 0.148 | 0.319 | 24.259 | 0.000 | 3.297 | 3.879 | 0.696 | 1.438 | |
| Z-score: Interpersonal Relationships | 2.605 | 0.163 | 0.232 | 15.977 | 0.000 | 2.284 | 2.926 | 0.573 | 1.747 | |
| Z-score: Health Responsibility | 2.492 | 0.141 | 0.222 | 17.691 | 0.000 | 2.215 | 2.770 | 0.767 | 1.304 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Strassoldo di Villanova, F.; Morganti, G.; Vitarelli, M.; Quarantelli, M.; Andrieu, B.; Ruscello, B.; Padua, E. Exploring the Interplay Among a Health-Promoting Lifestyle, Wellbeing, and Sociodemographic Characteristics in Italy: A Cross-Sectional Study. Healthcare 2025, 13, 2128. https://doi.org/10.3390/healthcare13172128
Strassoldo di Villanova F, Morganti G, Vitarelli M, Quarantelli M, Andrieu B, Ruscello B, Padua E. Exploring the Interplay Among a Health-Promoting Lifestyle, Wellbeing, and Sociodemographic Characteristics in Italy: A Cross-Sectional Study. Healthcare. 2025; 13(17):2128. https://doi.org/10.3390/healthcare13172128
Chicago/Turabian StyleStrassoldo di Villanova, Francesca, Gabriele Morganti, Matteo Vitarelli, Matteo Quarantelli, Bernard Andrieu, Bruno Ruscello, and Elvira Padua. 2025. "Exploring the Interplay Among a Health-Promoting Lifestyle, Wellbeing, and Sociodemographic Characteristics in Italy: A Cross-Sectional Study" Healthcare 13, no. 17: 2128. https://doi.org/10.3390/healthcare13172128
APA StyleStrassoldo di Villanova, F., Morganti, G., Vitarelli, M., Quarantelli, M., Andrieu, B., Ruscello, B., & Padua, E. (2025). Exploring the Interplay Among a Health-Promoting Lifestyle, Wellbeing, and Sociodemographic Characteristics in Italy: A Cross-Sectional Study. Healthcare, 13(17), 2128. https://doi.org/10.3390/healthcare13172128


_MD__MPH_PhD.png)







