The Role of Physical Activity Opportunities and Local Authority Engagement in Promoting Healthy Living and Increasing Life Expectancy
Abstract
1. Introduction
2. Theoretical Background and Hypotheses
2.1. Physical Activity and Its Impact on Health and Quality of Life
2.2. Physical Activity and Opportunities for Sports and Exercise
3. Materials and Methods
3.1. Research Design
3.2. Literature Review Methodology
3.3. Selected Variables
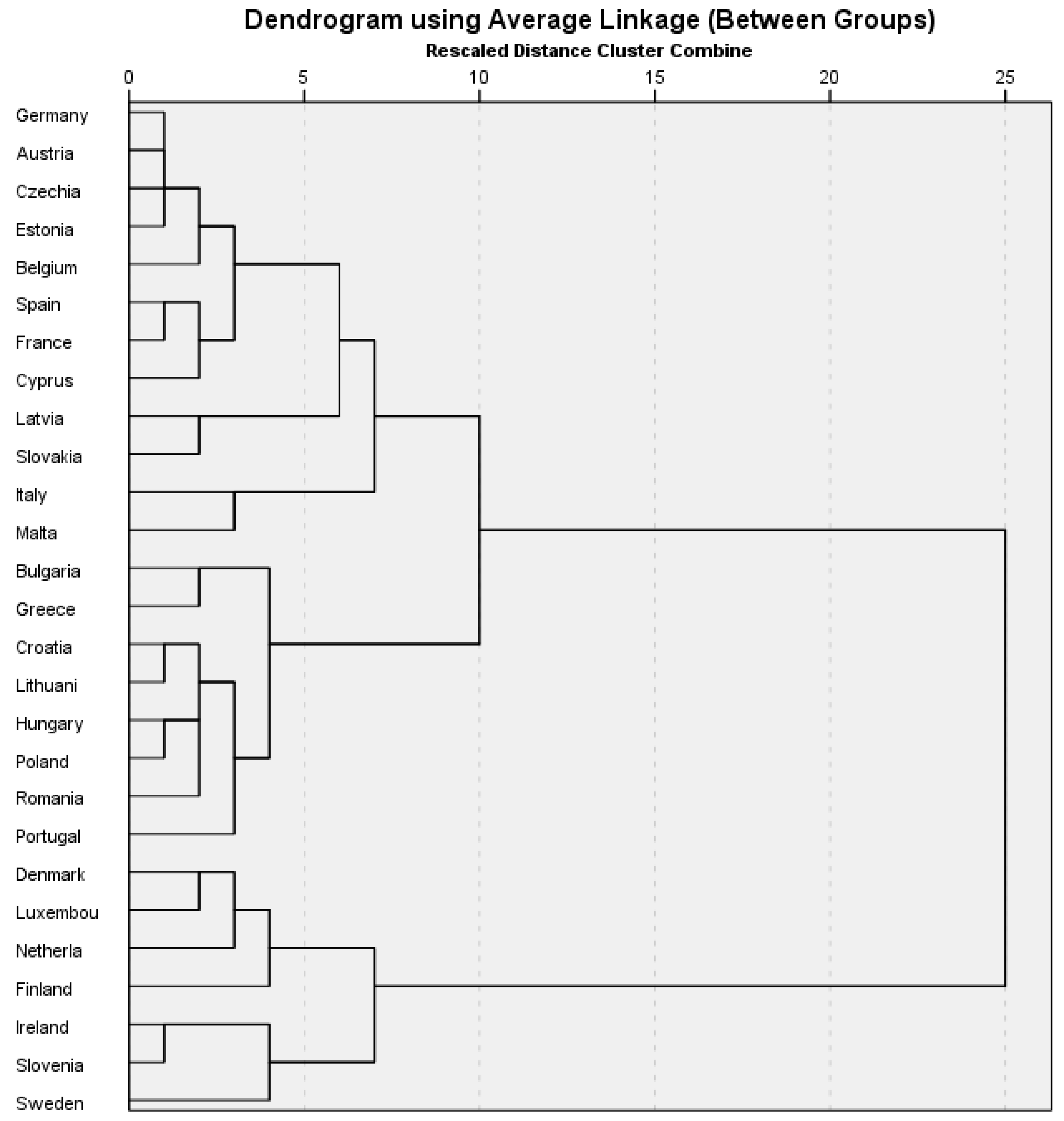
3.4. Research Methods
- n—input variables;
- f(n)—output variables.
- —observations from Cluster 1,
- —observations from Cluster 2,
- d(X,Y)—distance between a subject with observation vector x and a subject with observation vector,
- k,l—cases.
4. Results
5. Discussion
5.1. Theoretical and Practical Insights on Physical Activity Determinants
5.2. Policy and Community-Level Strategies for Promoting Physical Activity
5.3. Limitations and Further Research
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| HLYB | LEB | EPS_R | EPS_WSR | EPS_S | EPS_N | AO_TA | LP_TA | LA_TA | |
|---|---|---|---|---|---|---|---|---|---|
| Denmark | 55.9 | 81.3 | 11 | 48 | 21 | 20 | 89 | 87 | 37 |
| Luxembourg | 60.2 | 83.0 | 13 | 50 | 16 | 21 | 87 | 83 | 47 |
| Netherlands | 58.5 | 81.7 | 7 | 53 | 15 | 25 | 91 | 91 | 30 |
| Finland | 57.9 | 81.2 | 18 | 53 | 21 | 8 | 84 | 84 | 20 |
| Ireland | 66.0 | 82.6 | 13 | 41 | 11 | 35 | 82 | 83 | 45 |
| Slovenia | 66.7 | 81.3 | 11 | 41 | 23 | 25 | 80 | 74 | 49 |
| Sweden | 66.5 | 83.1 | 9 | 50 | 29 | 12 | 89 | 86 | 42 |
| Cluster 1 means | 61.7 | 82.0 | 11.7 | 48.0 | 19.4 | 20.9 | 86.0 | 84.0 | 38.6 |
| EU means | 62.1 | 79.9 | 7.6 | 32.8 | 19.6 | 40.0 | 73.6 | 70.4 | 43.6 |
| Germany | 61.1 | 80.7 | 8 | 35 | 25 | 32 | 85 | 81 | 27 |
| Austria | 60.9 | 81.4 | 7 | 35 | 23 | 35 | 78 | 67 | 30 |
| Czechia | 61.8 | 79.0 | 7 | 37 | 30 | 26 | 77 | 72 | 40 |
| Estonia | 59.3 | 78.1 | 8 | 34 | 28 | 30 | 78 | 74 | 27 |
| Belgium | 63.7 | 81.8 | 4 | 39 | 29 | 28 | 83 | 84 | 47 |
| Spain | 61.2 | 83.2 | 11 | 31 | 11 | 47 | 79 | 80 | 50 |
| France | 64.4 | 82.3 | 8 | 33 | 14 | 45 | 81 | 75 | 31 |
| Cyprus | 66.0 | 81.6 | 11 | 29 | 14 | 46 | 64 | 57 | 53 |
| Latvia | 54.2 | 74.5 | 9 | 30 | 28 | 33 | 66 | 67 | 36 |
| Slovakia | 57.3 | 77.0 | 6 | 29 | 22 | 43 | 59 | 50 | 51 |
| Italy | 67.4 | 82.8 | 3 | 31 | 10 | 56 | 65 | 62 | 57 |
| Malta | 70.2 | 82.4 | 7 | 25 | 37 | 31 | 67 | 85 | 66 |
| Cluster 2 means | 62.3 | 80.4 | 7.4 | 32.3 | 22.6 | 37.7 | 73.5 | 71.2 | 42.9 |
| EU means | 62.1 | 79.9 | 7.6 | 32.8 | 19.6 | 40.0 | 73.6 | 70.4 | 43.6 |
| Bulgaria | 66.7 | 74.2 | 4 | 17 | 18 | 61 | 41 | 41 | 46 |
| Greece | 67.0 | 80.8 | 4 | 19 | 9 | 68 | 61 | 54 | 45 |
| Croatia | 60.3 | 77.7 | 6 | 24 | 30 | 40 | 62 | 58 | 57 |
| Lithuania | 60.3 | 75.8 | 9 | 23 | 15 | 53 | 73 | 56 | 37 |
| Hungary | 62.6 | 76.0 | 4 | 22 | 15 | 59 | 74 | 69 | 48 |
| Poland | 62.4 | 77.2 | 2 | 21 | 12 | 65 | 73 | 62 | 52 |
| Portugal | 59.1 | 81.8 | 4 | 18 | 5 | 73 | 67 | 67 | 54 |
| Romania | 59.0 | 75.1 | 2 | 18 | 18 | 62 | 53 | 51 | 54 |
| Cluster 3 means | 62.2 | 77.3 | 4.4 | 20.3 | 15.3 | 60.1 | 63.0 | 57.3 | 49.1 |
| EU means | 62.1 | 79.9 | 7.6 | 32.8 | 19.6 | 40.0 | 73.6 | 70.4 | 43.6 |
References
- Gil-Lacruz, M.; Gil-Lacruz, A.I.; Domingo-Torrecilla, P.; Cañete-Lairla, M.A. Health-Related Quality of Life and Physical Activity in a Community Setting. Int. J. Environ. Res. Public Health 2021, 18, 7301. [Google Scholar] [CrossRef]
- Peng, B.; Ng, J.Y.Y.; Ha, A.S. Barriers and facilitators to physical activity for young adult women: A systematic review and thematic synthesis of qualitative literature. Int. J. Behav. Nutr. Phys. Act. 2023, 20, 23. [Google Scholar] [CrossRef]
- Franco, S.; Godinho, C.; Silva, C.S.; Avelar-Rosa, B.; Santos, R.; Mendes, R.; Silva, M.N. Assessment of Good Practices in Community-Based Interventions for Physical Activity Promotion: Development of a User-Friendly Tool. Int. J. Environ. Res. Public Health 2021, 18, 4734. [Google Scholar] [CrossRef] [PubMed]
- Ominyi, J.; Clifton, A.; Cushen-Brewster, N. Long-term effectiveness of physical activity interventions for adults across income contexts: A systematic review of strategies and outcomes. Bull. Fac. Phys. Flier. 2024, 29, 90. [Google Scholar] [CrossRef]
- Rinaldi, A.; Viviani, S.; Busciantella-Ricci, D. Urban Furniture Design Strategies to Build Healthy and Inclusive Neighborhoods. Sustainability 2025, 17, 859. [Google Scholar] [CrossRef]
- World Health Organization. Nearly 1.8 Billion Adults Are at Risk of Disease from Insufficient Physical Activity. 2024. Available online: https://www.who.int/news/item/26-06-2024-nearly-1.8-billion-adults-at-risk-of-disease-from-not-doing-enough-physical-activity (accessed on 18 January 2025).
- Biddle, S.J.H.; Asare, M. Physical activity and mental health in children and adolescents: A review of reviewers. Br. J. Sports Med. 2011, 45, 886–895. [Google Scholar] [CrossRef]
- Martinez-Gómez, D.; Martínez-De-Haro, V.; Del-Campo, J.; Zapatera, B.; Welk, G.J.; Villagra, A.; Veiga, Ó.L. Validez de cuatro cuestionarios para valorar la actividad física en adolescentes españoles. Gac. Sanit. 2009, 23, 512–517. [Google Scholar] [CrossRef]
- Krzepota, J.; Biernat, E.; Florkiewicz, B. The relationship between levels of physical activity and quality of life among students of the University of the Third Age. Cent. Eur. J. Public Health 2015, 23, 335–339. [Google Scholar] [CrossRef]
- Puciato, D.; Rozpara, M.; Borysiuk, Z. Physical Activity as a Determinant of Quality of Life in Working-Age People in Wrocław, Poland. Int. J. Environ. Res. Public Health 2018, 15, 623. [Google Scholar] [CrossRef]
- Saakslahti, A.; Numminen, P.; Niinikoski, H.; Rask-Nissila, L.; Viikari, J.; Tuominen, J.; Välimäki, I. Is physical activity related to body size, fundamental motor skills, and CHD risk factors in early childhood? Pediatric Exerc. Sci. 1999, 11, 327–340. [Google Scholar] [CrossRef]
- Janz, K.F.; Burns, T.L.; Torner, J.C.; Levy, S.M.; Paulos, R.; Willing, M.C.; Warren, J.J. Physical activity and bone measures in young children: The Iowa bone development study. Pediatrics 2001, 207, 1387–1393. [Google Scholar] [CrossRef] [PubMed]
- Colwell, M.; Lindsey, E. Preschool children’s pretend and physical play and sex of play partner: Connections to peer competence. Sex Roles 2005, 52, 497–509. [Google Scholar] [CrossRef]
- Warburton, D.E.; Bredin, S.S. Health benefits of physical activity: A systematic review of current systematic reviews. Curr. Opin. Cardiol. 2017, 32, 541–556. [Google Scholar] [CrossRef]
- Tomporowski, P.D.; McCullick, B.; Pendleton, D.M.; Pesce, C. Exercise and children’s cognition: The role of exercise characteristics and a place for metacognition. J. Sport Health Sci. 2015, 4, 47–55. [Google Scholar] [CrossRef]
- Singh, A.; Uijtdewilligen, L.; Twisk, J.R.; van Mechelen, W.; Chinapaw, M.M. Physical activity and performance at school: A systematic review of the literature including a methodological quality assessment. Arch. Pediatrics Adolesc. Med. 2012, 266, 49–55. [Google Scholar] [CrossRef]
- Moss, S.; Gu, X. Home- and Community-Based Interventions for Physical Activity and Early Child Development: A Systematic Review of Effective Strategies. Int. J. Environ. Res. Public Health 2022, 19, 11968. [Google Scholar] [CrossRef]
- Asmundson, G.J.; Fetzner, M.G.; DeBoer, L.B.; Powers, M.B.; Otto, M.W.; Smits, J.A. Let’s get physical: A contemporary review of the anxiolytic effects of exercise for anxiety and its disorders. Depress. Anxiety 2013, 30, 362–373. [Google Scholar] [CrossRef]
- European Commission. Sport and Physical Activity-Annex. Special Eurobarometer 525. 2022. Available online: https://europa.eu/eurobarometer/api/deliverable/download/file?deliverableId=83675 (accessed on 2 February 2025).
- Laurin, D.; Verreauli, R.; Lindsay, J.; MacPherson, K.; Rockwood, K. Physical activity and risk of cognitive impairment and dementia in elderly persons. Arch. Neurol. 2001, 58, 498–504. [Google Scholar] [CrossRef]
- Hallal, P.C.; Andersen, L.B.; Bull, F.C.; Guthold, R.; Haskell, W.L.; Ekelund, U. Global physical activity levels: Surveillance progress, pitfalls and prospects. Lancet 2012, 380, 247–257. [Google Scholar] [CrossRef] [PubMed]
- Mikkelsen, K.; Stojanovska, L.; Polenakovic, M.; Bosevski, M.; Apostolopoulos, V. Exercise and mental health. Maturitas 2017, 106, 48–56. [Google Scholar] [CrossRef] [PubMed]
- Varma, V.R.; Tan, E.J.; Wang, T.; Xue, Q.L.; Fried, L.P.; Seplaki, C.L.; King, A.C.; Seeman, T.E.; Rebok, G.W.; Carlson, M.C. Low-intensity walking activity is associated with better health. J. Appl. Gerontol. 2014, 33, 870–887. [Google Scholar] [CrossRef]
- Kiełtyka-Słowik, A.; Michalik-Marcinkowska, U.; Zawadzka, B. The association between physical activity and quality of life among people aged 60–89 living in own homes and nursing homes. BMC Geriatr. 2024, 24, 280. [Google Scholar] [CrossRef] [PubMed]
- Hao, H.; Yuan, Y.; Li, J.; Zhao, D.; Li, P.; Sun, J.; Zhou, C. Association between physical activity and health-related quality of life among adults in China: The moderating role of age. Front. Public Health 2024, 12, 1334081. [Google Scholar] [CrossRef]
- Aichberger, M.C.; Busch, M.A.; Reischies, F.M.; Ströhle, A.; Heinz, A.; Rapp, M.A. Effect of physical inactivity on cognitive performance after 2.5 years of follow-up: Longitudinal results from the survey of health, ageing, and retirement (SHARE). GeroPsych 2010, 23, 7–15. [Google Scholar] [CrossRef]
- Sluik, D.; Buijsse, B.; Muckelbauer, R.; Kaaks, R.; Teucher, B.; Tj, A.; Overvad, K.; Amiano, P.; Ardanaz, E.; Bendinelli, B.; et al. Physical activity and mortality in individuals with diabetes mellitus: A prospective study and meta-analysis. Arch. Intern. Med. 2012, 172, 1285–1295. [Google Scholar] [CrossRef] [PubMed]
- Soares-Miranda, L.; Siscovick, D.S.; Psaty, B.M.; Longstreth, W.T.; Mozaffarian, D. Physical activity and risk of coronary heart disease and stroke in older adults. The Cardiovascular Health Study. Circulation 2016, 133, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Currier, D.; Lindner, R.; Spittal, M.J.; Cvetkoviski, S.; Pirkis, J. Physical activity and depression in men: Increased activity duration and intensity associated with lower likelihood of current depression. J. Affect. Disord. 2020, 260, 426–431. [Google Scholar] [CrossRef]
- Sanchez-Lastra, M.A.; del Pozo Cruz, B.; Ekelund, U.; Tarp, J.; Ding, D. Journal of Physical Activity and Health. Physical activity and life expectancy free of cancer: Prospective evidence from the UK Biobank study. J. Phys. Act. Health 2025, 22, 636–639. [Google Scholar] [CrossRef]
- Asztalos, M.; De Bourdeaudhuij, I.; Cardon, G. The relationship between physical activity and mental health varies across activity intensity levels and dimensions of mental health among women and men. Public Health Nutr. 2010, 13, 1207–1214. [Google Scholar] [CrossRef]
- Roychowdhury, D. A comprehensive measure of participation motivation: Examining and validating the Physical Activity and Leisure Motivation Scale. J. Hum. Sport Exerc. 2018, 23, 231–247. [Google Scholar] [CrossRef]
- Swartz, T. Women should start exercising by this age for better quality of life. New York Post. 2 May 2024. Available online: https://nypost.com/2024/05/02/women-should-start-exercising-by-this-age-for-better-quality-of-life/ (accessed on 10 May 2025).
- Chastin, S.F.M.; Van Cauwenberg, J.; Menhout, L.; Gardon, G.; Lambert, E.V.; Van Dyck, D. Inequality in physical activity, global trends by income inequality and gender in adults. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 142. [Google Scholar] [CrossRef] [PubMed]
- Gorman, B.K.; Read, J.G. Gender disparities in adult health: An examination of three measures of morbidity. J. Health Soc. Behav. 2006, 47, 95–110. [Google Scholar] [CrossRef]
- Hallgren, M.; Herring, M.P.; Owen, N.; Dunstan, D.; Ekblom, Ö.; Helgadottir, B.; Nakitanda, O.A.; Forsell, Y. Exercise, physical activity, and sedentary behavior in the treatment of depression: Broadening the scientific perspectives and clinical opportunities. Front. Psychiatry 2016, 7, 36. [Google Scholar] [CrossRef]
- Gregory, A. Healthy lifestyle may offset genetics by 60% and add five years to life, study says. The Guardian. 30 April 2024. Available online: https://www.theguardian.com/science/2024/apr/30/healthy-lifestyle-may-offset-genetics-by-60-and-add-five-years-to-life-study-says (accessed on 10 May 2025).
- Westenhöfer, J.; Nouri, E.; Reschke, M.L.; Seebach, F.; Buchcik, J. Walkability and urban built environments—A systematic review of health impact assessments (HIA). BMC Public Health 2023, 23, 518. [Google Scholar] [CrossRef]
- Paglione, L.; Donato, M.A.; Cofone, L.; Sabato, M.; Appolloni, L.; D’Alessandro, D. The Healthy City Reimagined: Walkability, Active Mobility, and the Challenges of Measurement and Evaluation. Urban Sci. 2024, 8, 157. [Google Scholar] [CrossRef]
- Althoff, T.; Ivanovic, B.; Hicks, J.L.; Delp, S.L.; King, A.C.; Leskovec, J. Countrywide natural experiment reveals impact of built environment on physical activity. arXiv 2024, arXiv:2406.04557. [Google Scholar] [CrossRef]
- Trentini, C.; Wagner, G.; Chachamovich, E.; Figueiredo, M.; da Silva, L.; Hirakata, V.; Fleck, M. Subjective perception of health in elderly inpatients. Int. J. Psychol. 2012, 47, 279–286. [Google Scholar] [CrossRef]
- Li, X.; Wang, P.; Jiang, Y.; Yang, Y.; Wang, F.; Yan, F.; Li, M.; Peng, W.; Wang, Y. Physical activity and health-related quality of life in older adults: Depression as a mediator. BMC Geriatr. 2024, 24, 26. [Google Scholar] [CrossRef]
- Corazon, S.; Stitgsdotter, U.; Ekholm, O.; Pedersen, P.; Scopelliti, M.; Giuliani, M. Activities to alleviate stress and association with leisure time activities, socioeconomic status and general health. J. Appl. Behav. Res. 2010, 15, 161–174. [Google Scholar] [CrossRef]
- Mynarski, W.; Psurek, A.; Borek, Z.; Rozpara, M.; Grabara, M.; Strojek, K. Declared and real physical activity in patients with type 2 diabetes mellitus as assessed by the International Physical Activity Questionnaire and Caltrac accelerometer monitor: A potential tool for physical activity assessment in patients with type 2 diabetes mellitus. Diabetes Res. Clin. Pract. 2012, 98, 46–50. [Google Scholar] [CrossRef] [PubMed]
- Dikareva, A.; Andersen, R. Physical activity programming for clients with obesity. Considerations for exercise professionals. ACSMS Health Fit. J. 2016, 20, 21–27. [Google Scholar] [CrossRef]
- Heiestad, H.; Rustaden, A.; Bo, K.; Haakstad, L. Effect of regular resistance training on motivation, self-perceived health, and quality of life in previously inactive overweight women: A randomized, controlled trial. BioMed Res. Int. 2016, 2016, 3815976. [Google Scholar] [CrossRef] [PubMed]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide trends in insufficient physical activity from 2001 to 2016; a pooled analysis of 358 population-based surveys with 19 million participants. Lancet Glob. Health 2018, 6, E1077–E1086. [Google Scholar] [CrossRef] [PubMed]
- Lee, R.E.; Cubbin, C. Striding Toward Social Justice: The Ecologic Milieu of Physical Activity. Exerc. Sport Sci. Rev. 2009, 37, 10–17. [Google Scholar] [CrossRef]
- Ominyi, J.; Clifton, A. Barriers and Enablers to Physical Activity Participation Among Women in Underserved Communities: A Mixed-Methods Study. Women 2025, 5, 5. [Google Scholar] [CrossRef]
- Freire, R.C.; Fernandes, T.G.; Borges, G.F.; Guerra, R.O.; de Abreu, D.C.C. Factors associated with low levels of physical activity among elderly residents in a small urban area in the interior of the Brazilian Amazon. Arch. Gerontol. Geriatr. 2018, 75, 37–43. [Google Scholar] [CrossRef]
- Whitfield, G.; Carlson, S.; Ussery, E.; Watson, K.; Adams, M.; James, P.; Brownson, R.; Berrigan, D.; Fulton, J. Environmental supports for physical activity, National Health Interview Survey-2015. Am. J. Prev. Med. 2018, 54, 294–298. [Google Scholar] [CrossRef] [PubMed]
- Høyer-Kruse, J.; Schmidt, E.B.; Hansen, A.F.; Pedersen, M.R.L. The interplay between social environment and opportunities for physical activity within the built environment: A scoping review. BMC Public Health 2024, 24, 2361. [Google Scholar] [CrossRef]
- Busciantella-Ricci, D.; Macchi, A.; Viviani, S.; Rinaldi, A. Healthy and Inclusive Neighbourhoods: A Design Research Toolkit for the Promotion of Healthy Behaviours. Sustainability 2024, 16, 3059. [Google Scholar] [CrossRef]
- Wang, Y.; Steenbergen, B.; van der Krabben, E.; Kooij, H.-J.; Raaphorst, K.; Hoekman, R. The Impact of the Built Environment and Social Environment on Physical Activity: A Scoping Review. Int. J. Environ. Res. Public Health 2023, 20, 6189. [Google Scholar] [CrossRef]
- Macchi, A.; Busciantella-Ricci, D.; Caruso, E.; Setola, N. Healthy Neighbourhoods Hub (HNH) Framework: A Practical Guide for Fostering Healthy and Inclusive Living in Florence’s Urban Environment. Sustainability 2024, 16, 4423. [Google Scholar] [CrossRef]
- Tang, X. Research on Urban Furniture Design in Communities from a Health Promotion Perspective. J. Humanit. Arts Soc. Sci. 2023, 7, 1451–1459. [Google Scholar] [CrossRef]
- Zhang, Y.; Koene, M.; Reijneveld, S.A.; Tuinstra, J.; Broekhuis, M.; van der Spek, S. The impact of interventions in the built environment on physical activity levels: A systematic umbrella review. Int. J. Behav. Nutr. Phys. Act. 2022, 19, 156. [Google Scholar] [CrossRef] [PubMed]
- Deng, Y.; Liang, J.; Chen, Q. Greenway interventions effectively enhance physical activity levels: A systematic review with meta-analysis. Front. Public Health 2023, 11, 1268502. [Google Scholar] [CrossRef]
- Haldane, V.; Chuah, F.L.H.; Srivastava, A.; Singh, S.R.; Koh, G.C.H.; Seng, C.K.; Legido-Quigley, H. Community participation in health services development, implementation, and evaluation: A systematic review of empowerment, health, community, and process outcomes. PLoS ONE 2019, 14, e0216112. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, R.A.; McKenzie, G.; Holmes, C.; Shields, N. Social Support Initiatives That Facilitate Exercise Participation in Community Gyms for People with Disability: A Scoping Review. Int. J. Environ. Res. Public Health 2023, 20, 699. [Google Scholar] [CrossRef]
- Lee, Y.; Yun, L.; Kim, M.L.; Washington, M. A qualitative systematic review of public-private partnerships in promoting physical activity. Eval. Health Prof. 2020, 43, 90–104. [Google Scholar] [CrossRef]
- Parker, L.A.; Zaragoza, G.A.; Hernández-Aguado, I. Promoting population health with public-private partnerships: Where’s the evidence? BMC Public Health 2019, 19, 1438. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC). Strategies for Access to Places for Physical Activity. 2025. Available online: https://www.cdc.gov/physical-activity/php/strategies/access-to-places.html (accessed on 23 January 2025).
- Kuvaja-Köllner, V.; Kankaanpää, E.; Laine, J.; Borodulin, K. Municipal resources to promote adult physical activity: A multilevel follow-up study. BMC Public Health 2022, 22, 1213. [Google Scholar] [CrossRef]
- Bauman, A.E.; Reis, R.S.; Sallis, J.F.; Wells, J.C.; Loos, R.J.; Martín, B.W. Correlates of physical activity: Why are some people physically active and others not? Lancet 2012, 380, 258–271. [Google Scholar] [CrossRef]
- Noël Racine, A.; Garbarino, J.-M.; Massiera, B.; Vuillemin, A. Analysis of the local health-enhancing physical activity policies on the French Riviera. Int. J. Environ. Res. Public Health 2021, 18, 156. [Google Scholar] [CrossRef]
- Czwikla, G.; Boen, F.; Cook, D.G.; de Jong, J.; Harris, T.; Hilz, L.K.; Iliffe, S.; Morris, R.; Muellmann, S.; Peels, D.A.; et al. Equity-Specific Effects of Interventions to Promote Physical Activity among Middle-Aged and Older Adults: Development of a Collaborative Equity-Specific Re-Analysis Strategy. Int. J. Environ. Res. Public Health 2019, 16, 3195. [Google Scholar] [CrossRef]
- Alghannam, A.F.; Malkin, J.D.; Al-Hazzaa, H.M.; AlAhmed, R.; Evenson, K.R.; Rakic, S.; Alsukait, R.; Herbst, C.H.; Alqahtani, S.A.; Finkelstein, E.A. Public policies to increase physical activity and reduce sedentary behavior: A narrative synthesis of “reviews of reviews”. Glob. Health Action 2023, 16, 2194715. [Google Scholar] [CrossRef]
- Eurostat. Healthy Life Years by Sex. Available online: https://ec.europa.eu/eurostat/databrowser/view/hlth_hlye__custom_15379604/default/table?lang=en (accessed on 2 February 2025).
- I.B.M. Neural Networks. Available online: https://www.ibm.com/products/spss-statistics/neural-networks (accessed on 7 February 2025).
- PennState, Eberly College of Science. Agglomerative Hierarchical Clustering. Available online: https://online.stat.psu.edu/stat505/lesson/14/14.4 (accessed on 6 February 2025).
- Everitt, B.S.; Landau, S.; Leese, M. Cluster Analysis, 4th ed.; Wiley Publishing: Hoboken, NJ, USA, 2009. [Google Scholar]
- Noël Racine, A.; Garbarino, J.-M.; Massiera, B.; Vuillemin, A. Modeling the Development of Local Health-Enhancing Physical Activity Policies from Empirical Data and Policy Science Theories. Int. J. Environ. Res. Public Health 2022, 19, 1213. [Google Scholar] [CrossRef]
- World Health Organization. Global Action Plan on Physical Activity. 2018. Available online: https://iris.who.int/bitstream/handle/10665/272722/9789241514187-eng.pdf (accessed on 17 January 2025).
- Brown, W.J.; Heesch, K.C.; Miller, Y.D. Life events and changing physical activity patterns in women at different life stages. Ann. Behav. Med. 2009, 37, 294–305. [Google Scholar] [CrossRef]
- Nobles, J.; Thomas, C.; Banks Gross, Z.; Hamilton, M.; Trinder-Widdess, Z.; Speed, C.; Gibson, A.; Davies, R.; Farr, M.; Jago, R.; et al. “Let’s Talk about Physical Activity”: Understanding the Preferences of Under-Served Communities when Messaging Physical Activity Guidelines to the Public. Int. J. Environ. Res. Public Health 2020, 17, 2782. [Google Scholar] [CrossRef] [PubMed]
- Gelius, P.; Messing, S.; Forberger, S.; Lakerveld, J.; Mansergh, F.; Wendel-Vos, W.; Zukowska, J.; Woods, C. The added value of using the HEPA PAT for physical activity policy monitoring: A four-country comparison. Health Res. Policy Syst. 2021, 19, 22. [Google Scholar] [CrossRef] [PubMed]
- Bull, F.; Milton, K.; Kahlmeier, S. Health-Enhancing Physical Activity (HEPA) Policy Audit Tool (PAT)–Version 2; World Health Organization: Geneva, Switzerland, 2015; Available online: https://iris.who.int/handle/10665/369593 (accessed on 10 January 2025).
- Lee, K.; Ding, D.; Grunseit, A.; Wolfenden, L.; Milat, A.; Bauman, A. Many papers but limited policy impact? A bibliometric review of physical activity research. Transl. J. Am. Coll. Sports Med. 2021, 6, e000167. [Google Scholar] [CrossRef]
- Pringle, A.; Kime, N. Interventions to Promote Physical Activity and Healthy Ageing: An Editorial. Int. J. Environ. Res. Public Health 2024, 21, 1225. [Google Scholar] [CrossRef] [PubMed]
- Rozzek-Piechura, K.; Ignasiak, Z.; Slawirrska, T.; Piechura, J.; Ignasiak, T. Respiratory function, physical activity and body composition in adult rural population. Ann. Agric. Environ. Med. 2014, 21, 369–374. [Google Scholar] [CrossRef] [PubMed]
- Roychowdhury, D. Using Physical Activity to Enhance Health Outcomes Across the Life Span. J. Funct. Morphol. Kinesiol. 2020, 5, 2. [Google Scholar] [CrossRef] [PubMed]
- Ding, D.; Lawson, K.D.; Kolbe-Alexander, T.L.; Finkelstein, E.A.; Katzmarzyk, P.T.; van Mechelen, W.; Pratt, M. The economic burden of physical inactivity: A global analysis of major non-communicable diseases. Lancet 2016, 388, 1311–1324. [Google Scholar] [CrossRef] [PubMed]


| Variable | Dataset | Measures | References |
|---|---|---|---|
| EPS_R | Exercise or play sports—Regularly | Percentage | [19] |
| EPS_WSR | Exercise or play sports—With some regularity | Percentage | [19] |
| EPS_S | Exercise or play sports—Seldom | Percentage | [19] |
| EPS_N | Exercise or play sports—Never | Percentage | [19] |
| AO_TA | Area opportunities to be physically active | Percentage | [19] |
| LP_TA | Local provider opportunities to be physically active | Percentage | [19] |
| LA_TA | Lack of local authority efforts in relation to PA | Percentage | [19] |
| HLYB | Health expectancy in absolute values at birth | Years | [69] |
| LEB | Life expectancy in absolute values at birth | Years | [69] |
| Predictor | Predicted | Importance | Normalized Importance | ||||
|---|---|---|---|---|---|---|---|
| Hidden Layer 1 | Output Layer | ||||||
| H(1:1) | H(1:2) | HLYB | LEB | ||||
| Input Layer | (Bias) | −0.230 | −0.570 | ||||
| EPS_R | 2.366 | 1.169 | 0.233 | 44.7% | |||
| EPS_WSR | 4.282 | 1.804 | 0.521 | 100.0% | |||
| EPS_S | −0.296 | −0.112 | 0.035 | 6.8% | |||
| EPS_N | −1.689 | −1.704 | 0.211 | 40.5% | |||
| Hidden Layer 1 | (Bias) | 0.152 | −0.177 | ||||
| H(1:1) | 0.332 | 2.395 | |||||
| H(1:2) | −0.516 | −0.952 | |||||
| Predictor | Predicted | Importance | Normalized Importance | |||||
|---|---|---|---|---|---|---|---|---|
| Hidden Layer 1 | Output Layer | |||||||
| H(1:1) | EPS_R | EPS_WSR | EPS_S | EPS_N | ||||
| Input Layer | (Bias) | −1.583 | ||||||
| AO_TA | 3.179 | 0.446 | 100.0% | |||||
| LP_TA | 3.112 | 0.405 | 90.8% | |||||
| LA_TA | −1.342 | 0.148 | 33.3% | |||||
| Hidden Layer 1 | (Bias) | −0.970 | −2.826 | −0.934 | 1.658 | |||
| H(1:1) | 1.613 | 3.609 | 1.263 | −2.552 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mangra, M.G.; Mangra, G.I.; Bocean, C.G.; Vărzaru, A.A.; Rotea, C.C.; Văduva, C.-C. The Role of Physical Activity Opportunities and Local Authority Engagement in Promoting Healthy Living and Increasing Life Expectancy. Healthcare 2025, 13, 2110. https://doi.org/10.3390/healthcare13172110
Mangra MG, Mangra GI, Bocean CG, Vărzaru AA, Rotea CC, Văduva C-C. The Role of Physical Activity Opportunities and Local Authority Engagement in Promoting Healthy Living and Increasing Life Expectancy. Healthcare. 2025; 13(17):2110. https://doi.org/10.3390/healthcare13172110
Chicago/Turabian StyleMangra, Mădălina Giorgiana, Gabriel Ioan Mangra, Claudiu George Bocean, Anca Antoaneta Vărzaru, Cristina Claudia Rotea, and Constantin-Cristian Văduva. 2025. "The Role of Physical Activity Opportunities and Local Authority Engagement in Promoting Healthy Living and Increasing Life Expectancy" Healthcare 13, no. 17: 2110. https://doi.org/10.3390/healthcare13172110
APA StyleMangra, M. G., Mangra, G. I., Bocean, C. G., Vărzaru, A. A., Rotea, C. C., & Văduva, C.-C. (2025). The Role of Physical Activity Opportunities and Local Authority Engagement in Promoting Healthy Living and Increasing Life Expectancy. Healthcare, 13(17), 2110. https://doi.org/10.3390/healthcare13172110










