Mediating Effect of Team Effectiveness of the Nursing Unit on the Nursing Work Environment and Patient-Centered Nursing: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Measures
2.2.1. Patient-Centered Nursing
2.2.2. Team Effectiveness of the Nursing Unit
2.2.3. Nursing Working Environment
2.2.4. Covariates
2.3. Data Collection
2.4. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Correlation Analysis of Patient-Centered Nursing, Nursing Unit Team Effectiveness, and Nursing Work Environment
3.3. Relationships Between General Characteristics and Patient-Centered Nursing
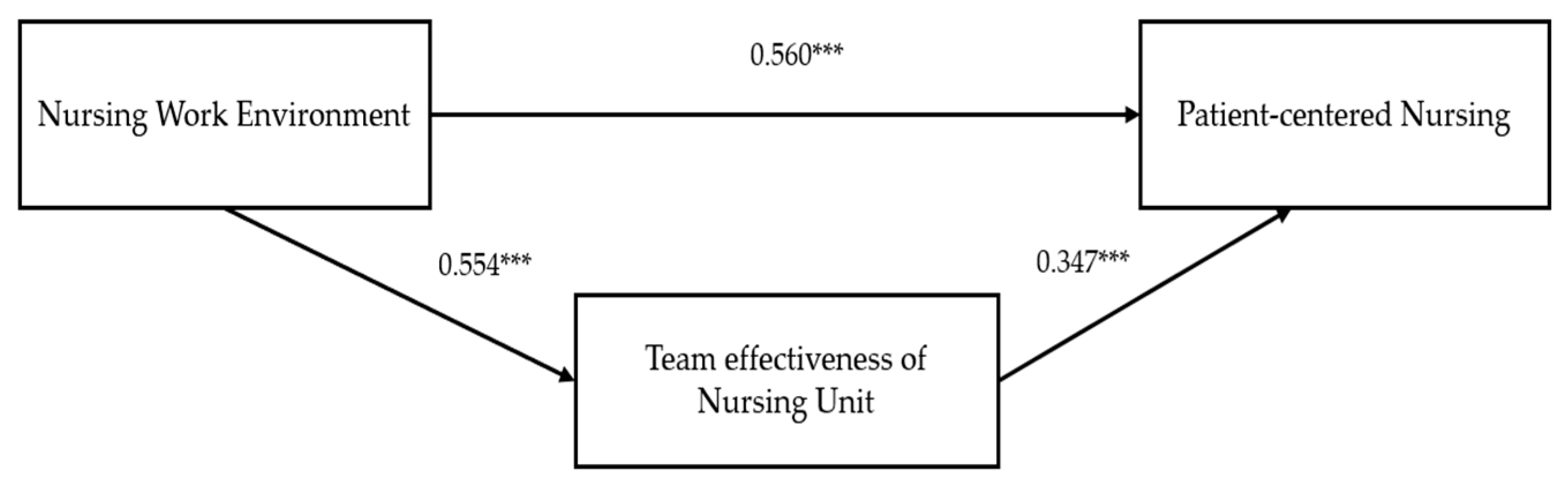
3.4. Mediating Effects of Nursing Unit Team Effectiveness on Nursing Working Environment and Patient-Centered Nursing
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century; National Academies Press: Washington, DC, USA, 2001. [Google Scholar]
- Lusk, J.M.; Fater, K. A concept analysis of patient-centered care. Nurs. Forum 2013, 48, 89–98. [Google Scholar] [CrossRef] [PubMed]
- Kitson, A.; Marshall, A.; Bassett, K.; Zeitz, K. What are the core elements of patient-centred care? A narrative review and synthesis of the literature from health policy, medicine and nursing. J. Adv. Nurs. 2013, 69, 4–15. [Google Scholar] [CrossRef]
- Bolster, D.; Manias, E. Person-centred interactions between nurses and patients during medication activities in an acute hospital setting: Qualitative observation and interview study. Int. J. Nurs. Stud. 2010, 47, 154–165. [Google Scholar] [CrossRef]
- Kim, J.; Kim, M. The impact of patient-centered care on the patient experience according to patients in a tertiary hospital. J. Korean Acad. Nurs. Adm. 2023, 29, 288–297. [Google Scholar] [CrossRef]
- Abugre, D.; Bhengu, B.R. Nurse managers’ perceptions of patient-centred care and its influence on quality nursing care and nurse job satisfaction: Empirical research qualitative. Nurs. Open 2024, 11, e2071. [Google Scholar] [CrossRef]
- McCormack, B.; McCance, T. Person-Centred Nursing: Theory, Models and Methods; Wiley-Blackwell: Oxford, UK, 2010. [Google Scholar]
- Charalambous, A.; Katajisto, J.; Välimäki, M.; Leino-Kilpi, H.; Suhonen, R. Individualised care and the professional practice environment: Nurses’ perception. Int. Nurs. Rev. 2010, 57, 500–507. [Google Scholar] [CrossRef] [PubMed]
- Naseri, S.; Ghafourifard, M.; Ghahramanian, A. The impact of work environment on nurses’ compassion: A multicenter cross-sectional study. SAGE Open Nurs. 2022, 8, 23779608221119124. [Google Scholar] [CrossRef]
- Scheepers, R.A.; Vollmann, M.; Cramm, J.M.; Nieboer, A.P. Empathic nurses with sufficient job resources are work-engaged professionals who deliver more individualized care. J. Clin. Nurs. 2023, 32, 7321–7329. [Google Scholar] [CrossRef]
- Boudreau, C.; Rhéaume, A. Impact of the work environment on nurse outcomes: A mediation analysis. West. J. Nurs. Res. 2024, 46, 210–218. [Google Scholar] [CrossRef]
- Li, L.Z.; Yang, P.; Singer, S.J.; Pfeffer, J.; Mathur, M.B.; Shanafelt, T. Nurse burnout and patient safety, satisfaction, and quality of care: A systematic review and meta-analysis. JAMA Netw. Open 2024, 7, e2443059. [Google Scholar] [CrossRef] [PubMed]
- Jung, M.S.; Kim, E.K.; Kim, S.Y.; Kim, J.K.; Park, E.J.; Yu, M. Nursing Management, 5th ed.; Hyunmoonsa: Seoul, Republic of Korea, 2023. [Google Scholar]
- Baek, H.; Han, K.; Cho, H.; Ju, J. Nursing teamwork is essential in promoting patient-centered care: A cross-sectional study. BMC Nurs. 2023, 22, 433. [Google Scholar] [CrossRef]
- Jeong, H.; Park, M. A predictive model on patient-centered care of hospital nurses in Korea. J. Korean Acad. Nurs. 2019, 49, 191–202. [Google Scholar] [CrossRef]
- Ilgen, D.R.; Hollenbeck, J.R.; Johnson, M.; Jundt, D. Teams in organizations: From input-process-output models to IMOI models. Annu. Rev. Psychol. 2005, 56, 517–543. [Google Scholar] [CrossRef]
- Lemieux-Charles, L.; McGuire, W.L. What do we know about health care team effectiveness? a review of the literature. Med. Care Res. Rev. 2006, 63, 263–300. [Google Scholar] [CrossRef] [PubMed]
- Brittain, A.C.; Carrington, J.M. Organizational health and patient safety: A systematic review. J. Hosp. Manag. Health Policy 2021, 5, 2. [Google Scholar] [CrossRef]
- Seo, M.H.; Kim, E.A.; Kim, H.R. How the nursing work environment moderates the relationship between clinical judgment and person-centered care among intensive care unit nurses. PLoS ONE 2025, 20, e0316654. [Google Scholar] [CrossRef] [PubMed]
- Rosen, M.A.; DiazGranados, D.; Dietz, A.S.; Benishek, L.E.; Thompson, D.; Pronovost, P.J.; Weaver, S.J. Teamwork in healthcare: Key discoveries enabling safer, high-quality care. Am. Psychol. 2018, 73, 433–450. [Google Scholar] [CrossRef] [PubMed]
- Joo, Y.S.; Jang, Y. Predictors of person-centered care among nurses in adult intensive care units. J. Korean Clin. Nurs. Res. 2022, 28, 34–43. [Google Scholar] [CrossRef]
- Shin, E.; Yoon, S. Development of the patient-centered nursing culture scale for hospitals. J. Korean Acad. Nurs. 2019, 49, 613–630. [Google Scholar] [CrossRef]
- Kim, Y.M.; Kim, S.Y. Development of a team effectiveness scale for nursing units. J. Korean Acad. Nurs. Adm. 2018, 24, 328–338. [Google Scholar] [CrossRef]
- Kim, S.Y.; Kim, J.K.; Jung, M.S.; Kim, E.K.; You, S.J. A literature review of team effectiveness on hospital nursing units. J. Korean Acad. Nurs. Adm. 2017, 23, 18–31. [Google Scholar] [CrossRef][Green Version]
- Kim, S.Y.; Ko, Y.; Sim, B.H.; Yoon, Y.O.; Jhang, C. Refinement and validation of Team Effectiveness Scale for Nursing Units. Risk Manag. Healthc. Policy 2024, 17, 2385–2396. [Google Scholar] [CrossRef]
- Kramer, M.; Hafner, L. Shared values: Impact on staff nurse job satisfaction and perceived productivity. Nurs. Res. 1989, 38, 172–177. [Google Scholar] [CrossRef]
- Aiken, L.H.; Patrician, P.A. Measuring organizational traits of hospitals: The revised nursing work index. Nurs. Res. 2000, 49, 146–153. [Google Scholar] [CrossRef]
- Lake, E.T. Development of the practice environment scale of the nursing work index. Res. Nurs. Health 2002, 25, 176–188. [Google Scholar] [CrossRef]
- Cho, E.; Choi, M.; Kim, E.Y.; Yoo, I.Y.; Lee, N.J. Construct validity and reliability of the Korean version of the practice enviornment scale of nursing work index of Korean nurses. J. Korean Acad. Nurs. 2011, 41, 325–332. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.Y.; Kim, Y.; Kim, J. The combined effect of bed-to-nurse ratio and nurse turnover rate on in-hospital mortality based on South Korean administrative data: A cross-sectional study. BMC Nurs. 2025, 24, 124. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation and Conditional Process Analysis: A Regression-Based Approach; The Guilford Press: New York, NY, USA, 2013. [Google Scholar]
- Lee, J.; Kim, G.M.; Kim, E.; Chang, S.J. Factors affecting patient-centered nursing in regional public hospital. J. East-West Nurs. Res. 2020, 26, 185–195. [Google Scholar] [CrossRef]
- Suhonen, R.; Lahtinen, K.; Stolt, M.; Pasanen, M.; Lemetti, T. Validation of the patient-centred care competency scale instrument for Finnish nurses. J. Pers. Med. 2021, 11, 583. [Google Scholar] [CrossRef]
- Suhonen, R.; Papastavrou, E.; Efstathiou, G.; Lemonidou, C.; Kalafati, M.; da Luz, M.D.; Idvall, E.; Berg, A.; Acaroglu, R.; Sendir, M.; et al. Nurses’ perceptions of individualized care: An international comparison. J. Adv. Nurs. 2011, 67, 895–907. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Shin, S.; Yeom, H. The effects of the nursing practice environment and self-leadership on person-centered care provided by oncology nurses. J. Hosp. Palliat. Care 2021, 24, 174–183. [Google Scholar] [CrossRef]
- Yang, K.S.; Song, M.O. The effects of patient-centered nursing competency, safety climate and job satisfaction of clinical nurses on patient participation. J. Korea Acad.-Ind. Coop. Soc. 2023, 24, 569–580. [Google Scholar] [CrossRef]
- Ministry of Government Legislation Regulations on the Designation and Evaluation of Tertiary General Hospitals. Available online: https://www.law.go.kr/ (accessed on 20 June 2025).
- Health Insurance Review & Assessment Service. 2023 Patient Experience Evaluation Result; Health Insurance Review & Assessment Service: Wonju, Republic of Korea, 2024. [Google Scholar]
- Jung, S.M.; Yoon, S.H. Comparative analysis research of inpatient satisfaction with nursing on comprehensive nursing service units & general units and nurse’s work stress. J. Korean Acad. Nurs. Adm. 2017, 23, 229–238. [Google Scholar] [CrossRef]
- Chung, S.; Hwang, J. Hospital nurses’ experience of patient-centered nursing. Qual. Improv. Health Care 2021, 27, 26–42. [Google Scholar] [CrossRef]
- Cho, K.; Kim, M. Effects of nursing professionalism, job stress and nursing work environment of clinical nurses on person-centered care. J. Muscle Jt. Health 2022, 29, 176–184. [Google Scholar] [CrossRef]
- Jiang, N.; Sun, M.M.; Zhou, Y.Y.; Feng, X.X. Significance of patient participation in nursing care. Altern. Ther. Health Med. 2021, 27, 115–119. [Google Scholar] [PubMed]
- Heidari, S.; Parizad, N.; Goli, R.; Mam-Qaderi, M.; Hassanpour, A. Job satisfaction and its relationship with burnout among nurses working in COVID-19 wards: A descriptive correlational study. Ann. Med. Surg. 2022, 82, 104591. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.W.; Fan, L. Emotional labor and job satisfaction among nurses: The mediating effect of nurse-patient relationship. Front. Psychol. 2023, 14, 1094358. [Google Scholar] [CrossRef]
| Variables | Category | n (%) | M (SD) |
|---|---|---|---|
| Sex, n (%) | Male | 16 (4.9) | |
| Female | 311 (95.1) | ||
| Age (years), n (%) | ≤29 | 229 (70.0) | |
| 30–39 | 79 (24.2) | ||
| ≥40 | 19 (8.8) | ||
| Age (years), M (SD) | 29.23 (5.04) | ||
| Marital status, n (%) | Not married | 263 (80.4) | |
| Married | 64 (18.6) | ||
| Education, n (%) | Associated degree | 90 (30.3) | |
| Bachelor’s degree | 213 (65.1) | ||
| Master’s degree | 15 (4.6) | ||
| Clinical experience (years), n (%) | ≤3 | 73 (22.3) | |
| 3–5 | 100 (30.6) | ||
| >5 | 154 (47.1) | ||
| Clinical experience (years), M (SD) | 6.19 (5.04) | ||
| Work experience in current unit (years), n (%) | ≤1 | 57 (17.4) | |
| 1–3 | 101 (30.9) | ||
| >3 | 169 (51.7) | ||
| Work experience in current unit (years), M (SD) | 3.96 (3.56) | ||
| Position, n (%) | Staff nurse | 300 (91.7) | |
| Charge nurse | 27 (8.3) | ||
| Type of nursing unit | General nursing care unit | 167 (51.1) | |
| Comprehensive nursing care unit | 160 (48.9) | ||
| Type of hospital, n (%) | Tertiary general hospital | 126 (38.5) | |
| General hospital | 201 (61.5) | ||
| Ward bed-to-nurse ratio, M (SD), Range = [0.19, 3.85] | 1.91 (0.77) | ||
| Patient-centered nursing activities score, M (SD) Range = [2.64, 5.00] | 3.96 (0.50) | ||
| TES-NU, M (SD), Range = [1.87, 3.82] | 3.06 (0.35) | ||
| PES-NWI-Korean version, M (SD), Range = [1.48, 3.90] | 2.75 (0.41) |
| Variables | Category | M (SD) | t or F | p |
|---|---|---|---|---|
| Sex | Male | 3.95 (0.50) | −1.60 | 0.111 |
| Female | 4.15 (0.54) | |||
| Age (years) | ≤29 | 3.97 (0.48) | 1.79 | 0.169 |
| 30–39 | 3.88 (0.56) | |||
| ≥40 | 4.10 (0.54) | |||
| Marital status | Not married | 3.95 (0.47) | −0.24 | 0.810 |
| Married | 3.97 (0.61) | |||
| Education | Associated degree | 4.02 (0.53) | 1.44 | 0.239 |
| Bachelor’s degree | 4.10 (0.43) | |||
| Master’s degree | 3.93 (0.48) | |||
| Clinical experience (years) † | ≤3 a | 4.10 (0.43) | 3.71 | 0.025 |
| 3–5 b | 3.93 (0.48) | (a > c) | ||
| >5 c | 3.91 (0.54) | |||
| Work experience in current unit (years) † | ≤1 a | 3.98 (0.55) | 1.67 | 0.191 |
| 1–3 b | 4.02 (0.46) | |||
| >3 c | 3.91 (0.51) | |||
| Position | Staff nurse | 3.98 (0.49) | 2.74 | 0.007 |
| Charge nurse | 3.70 (0.58) | |||
| Type of nursing unit | General nursing care unit | 3.97 (0.50) | 0.48 | 0.630 |
| Comprehensive nursing care unit | 3.94 (0.40) | |||
| Type of hospital | Tertiary general hospital | 4.12 (0.52) | 4.83 | <0.001 |
| General hospital | 3.86 (0.47) |
| Variables | Patient-Centered Nursing (Y) | 95% CI | ||||
|---|---|---|---|---|---|---|
| β | SE | t | p | LLCI | ULCI | |
| Team effectiveness of the nursing unit (M) | 0.347 | 0.071 | 4.90 | <0.001 | 0.207 | 0.486 |
| Nursing work environment (X) | 0.560 | 0.082 | 6.80 | <0.001 | 0.398 | 0.722 |
| R2 | 0.39 | |||||
| F | 35.35 | |||||
| p | <0.001 | |||||
| Categories | Effect | SE | t | p | 95% CI | |
|---|---|---|---|---|---|---|
| LLCI | ULCI | |||||
| Total effect | 0.657 | 0.058 | 11.37 | <0.001 | 0.544 | 0.771 |
| Direct effect | 0.347 | 0.071 | 4.90 | <0.001 | 0.207 | 0.486 |
| Indirect effect | 0.311 | 0.053 | 0.208 | 0.419 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.Y.; Ko, Y. Mediating Effect of Team Effectiveness of the Nursing Unit on the Nursing Work Environment and Patient-Centered Nursing: A Cross-Sectional Study. Healthcare 2025, 13, 2080. https://doi.org/10.3390/healthcare13172080
Kim SY, Ko Y. Mediating Effect of Team Effectiveness of the Nursing Unit on the Nursing Work Environment and Patient-Centered Nursing: A Cross-Sectional Study. Healthcare. 2025; 13(17):2080. https://doi.org/10.3390/healthcare13172080
Chicago/Turabian StyleKim, Se Young, and Young Ko. 2025. "Mediating Effect of Team Effectiveness of the Nursing Unit on the Nursing Work Environment and Patient-Centered Nursing: A Cross-Sectional Study" Healthcare 13, no. 17: 2080. https://doi.org/10.3390/healthcare13172080
APA StyleKim, S. Y., & Ko, Y. (2025). Mediating Effect of Team Effectiveness of the Nursing Unit on the Nursing Work Environment and Patient-Centered Nursing: A Cross-Sectional Study. Healthcare, 13(17), 2080. https://doi.org/10.3390/healthcare13172080






