Abstract
Telemedicine has transformed obstetrics and gynecology (OB/GYN), accelerated by the COVID-19 pandemic. This study aims to synthesize evidence on the adoption, effectiveness, barriers, and technological innovations of telemedicine in OB/GYN across diverse healthcare settings. This scoping review synthesized 63 peer-reviewed studies (2010–2023) using PRISMA-ScR guidelines to map global applications, outcomes, and challenges. Key modalities included synchronous consultations, remote monitoring, AI-assisted triage, tele-supervision, and asynchronous communication. Results demonstrated improved access to routine care and mental health support, with outcomes for low-risk pregnancies comparable to in-person services. Adoption surged >500% during pandemic peaks, stabilizing at 9–12% of services in high-income countries. However, significant disparities persisted: 43% of rural Sub-Saharan clinics lacked stable internet, while socioeconomic, linguistic, and cultural barriers disproportionately affected vulnerable populations (e.g., non-English-speaking, transgender, and refugee patients). Providers reported utility but also screen fatigue (41–68%) and diagnostic uncertainty. Critical barriers included fragmented policies, reimbursement variability, data privacy concerns, and limited evidence from conflict-affected regions. Sustainable integration requires equity-centered design, robust policy frameworks, rigorous longitudinal evaluation, and ethically validated AI to address clinical complexity and systemic gaps.
1. Introduction
Telemedicine, broadly defined as the remote delivery of clinical services through telecommunication technologies, has emerged as a critical innovation in modern healthcare, particularly amplified by the COVID-19 pandemic [1]. The rapid shift to virtual care models addressed immediate healthcare access challenges caused by physical distancing, resource constraints, and overloaded health systems [2]. This global acceleration has underscored telemedicine’s potential to overcome geographical barriers and enhance healthcare accessibility, particularly in underserved and rural populations [3,4].
The universal benefits of telemedicine include improving access to timely care, reducing travel burdens, and facilitating the continuity of services during public health crises [5,6]. Economic evaluations demonstrate cost savings and increased efficiency, especially through provider-to-provider consultations and asynchronous “store-and-forward” modalities [5]. Additionally, telemedicine platforms have increasingly incorporated artificial intelligence (AI), enabling dynamic patient monitoring and decision support, which has improved triage efficiency by up to 35% in some settings [7,8]. These innovations support personalized care models and optimize resource allocation in complex clinical environments [9].
Despite its transformative promise, telemedicine faces persistent challenges globally. Common barriers include limited digital literacy, poor internet connectivity, infrastructural deficits, and policy gaps that hinder implementation and sustainability [9,10]. For example, digital divides remain stark in low-resource settings such as Bangladesh, where patients’ lack of awareness and infrastructural weaknesses delay adoption [11,12]. In the Middle East, despite progress in telemedicine initiatives, policy fragmentation and insufficient infrastructure restrict broader uptake [13]. Similarly, rural China encounters challenges related to healthcare provider readiness and patient attitudes, highlighting the need for targeted community engagement and capacity-building [14]. Cultural acceptance and regulatory issues further complicate deployment in diverse regions, including India, where government initiatives coexist with significant operational hurdles [15].
Telemedicine’s expansion post-COVID-19 has extended across multiple specialties worldwide. For instance, Latin America has seen telehealth innovations improve rheumatology care by enhancing patient monitoring and access [16]. Similarly, virtual respiratory care exemplifies adaptive strategies that maintain service continuity during pandemic disruptions [6]. However, despite widespread adoption, concerns about exacerbating healthcare disparities persist. Inequities in access related to socioeconomic status, language barriers, and marginalized populations—such as transgender individuals—demand culturally competent and inclusive telehealth frameworks [17,18,19,20].
Within this broad context, obstetrics and gynecology (OB/GYN) represent a particularly vital domain for telemedicine integration. Prenatal and postnatal care are highly dependent on timely access, monitoring, and patient adherence, all areas where telehealth has demonstrated substantial benefits [21,22]. Remote antenatal monitoring using wearable devices, virtual consultations for low-risk pregnancies, tele-ultrasound interpretation, tele-abortion services, and digital patient education platforms have been implemented to various degrees globally [21,22,23]. These interventions reduce patient burden, improve care continuity, and support the early detection of complications [22,24].
Empirical evidence affirms that telemedicine interventions in OB/GYN improve maternal and fetal outcomes, especially among high-risk pregnancies, by facilitating timely monitoring and multidisciplinary consultation [22,24]. For example, studies of telemedicine for medical abortion in Australia report patient satisfaction rates between 78% and 92%, highlighting benefits such as privacy, convenience, and reduced travel [23,25]. During the pandemic, telehealth models ensured the safe and effective management of gestational hypertension and diabetes, achieving outcomes comparable to in-person care [24]. Patient and clinician satisfaction with prenatal telemedicine consultations was generally high, reflecting the growing acceptance of virtual perinatal care [26,27].
The rapid integration of telemedicine in OB/GYN care settings required operational adaptations, including workflow redesign and clinician training [27,28,29]. Variations in physician telemedicine provision are influenced by factors such as specialty, geography, and patient demographics [30]. Data suggest that rural patients more often utilize voice or SMS-based consultations, while urban populations favor video-enabled platforms, emphasizing the need for adaptable technological solutions to meet diverse patient preferences [31]. Telemedicine also plays a growing role in medical education, facilitating clinical exposure and training continuity amid social distancing [32,33].
Looking forward, telemedicine’s sustained adoption depends on addressing persistent infrastructure gaps, regulatory challenges, and digital literacy barriers, especially in resource-constrained settings [34,35,36]. Strategies involving community engagement, policy reform, and the integration of AI and mHealth technologies promise to optimize service delivery and equity [37,38,39]. The continuous evaluation of telemedicine quality, safety, and patient satisfaction remains essential to refining these models and mitigating potential disparities [39,40,41].
This review aims to synthesize current evidence on telemedicine adoption, effectiveness, barriers, and technological innovations in obstetrics and gynecology across diverse global contexts, highlighting both successes and ongoing challenges in this evolving field.
2. Materials and Methods
2.1. Study Design
This scoping review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) guidelines. The approach enabled a comprehensive mapping of telemedicine applications within obstetrics and gynecology (OB/GYN) care, focusing on adoption, clinical effectiveness, technological integration, and equity across diverse healthcare settings. As a secondary research study, it synthesizes evidence from the existing literature without involving primary data collection or clinical interventions.
2.2. Information Sources and Search Strategy
A systematic literature search was performed across multiple scientific databases, including PubMed, Scopus, and Google Scholar. Additionally, targeted manual searches were conducted in high-impact journals such as The New England Journal of Medicine, The Lancet, JAMA, PLoS ONE, and SAGE digital archives to capture relevant studies potentially not indexed in broader databases. The search covered publications from January 2010 to December 2023.
Search terms combined Medical Subject Headings (MeSH) and free-text keywords, including “telemedicine”, “telehealth”, “obstetrics”, “gynecology”, “digital health”, “rural healthcare”, “artificial intelligence”, and “wearable devices.” Boolean operators (AND, OR) and filters were applied to refine the results to peer-reviewed journal articles. Reference lists of included studies were screened to identify the additional relevant literature. These studies are summarized in Table A1 (see Appendix A). The full search strategy for each database is detailed in Appendix B. The initial search yielded 447 articles. After applying inclusion and exclusion criteria, 142 articles were selected for screening. Following exclusion by title and abstract, 94 articles were chosen for full-text review. Finally, 63 articles were included for data extraction. A PRISMA flowchart (Figure A1) illustrates the study selection process (see Appendix C).
2.3. Eligibility Criteria
Studies were eligible if they met the following criteria:
- Published in English in peer-reviewed journals between 2010 and 2023.
- Focused explicitly on telemedicine or digital health interventions within obstetrics and/or gynecology.
- Reported empirical data from rural and/or urban healthcare settings.
- Included application or evaluation of advanced technologies such as artificial intelligence (AI), mobile health (mHealth), or wearable devices.
- For COVID-19-era studies (2020–2023), explicit reference to the pandemic context or impact was required.
Exclusion criteria included the following:
- Publications not in English.
- Studies focusing exclusively on telemedicine in unrelated specialties.
- Non-empirical works such as reviews without original data.
2.4. Study Selection and Data Extraction
Two independent reviewers screened titles and abstracts for relevance, followed by a full-text assessment against the inclusion criteria. Discrepancies were resolved through discussion or consultation with a third reviewer. Inter-rater reliability was evaluated using Cohen’s kappa coefficient (κ = 0.84), indicating substantial agreement.
A standardized data extraction form was developed and pilot-tested to capture key study characteristics, including author information, publication year, geographic setting, study design, healthcare context, telemedicine modalities, technological components, implementation outcomes, barriers and facilitators, and insights related to COVID-19 adaptations.
2.5. Quality Appraisal
Included studies were appraised for methodological quality using validated critical appraisal tools appropriate to their study designs (e.g., CASP checklists for qualitative studies, Joanna Briggs Institute tools for observational studies). Quality assessment results are summarized in Table A2 (see Appendix D).
2.6. Data Synthesis and Analysis
Thematic synthesis was conducted using NVivo 14 2023 software to inductively identify recurrent themes across studies. Themes were categorized into overarching domains, including telemedicine benefits, challenges, equity of access, technological readiness, and clinical effectiveness. Comparative analyses explored variations between rural and urban settings and examined the role of AI and wearable devices in enhancing remote OB/GYN care.
A subgroup analysis focused on studies published during the COVID-19 pandemic (March 2020–December 2023), assessing how pandemic-related factors influenced telemedicine adoption, service continuity, and policy innovations.
2.7. Ethical Considerations
As this study involved a secondary analysis of the published literature without direct human participant involvement, ethical approval was not required. All sources were cited appropriately, and the review adhered to PRISMA-ScR guidelines to ensure transparency and reproducibility.
2.8. Limitations
This review is limited by the exclusion of the non-English literature, potentially underrepresenting non-English-speaking regions. Publication bias is a concern, as unsuccessful or unpublished telemedicine initiatives may be underreported. Additionally, heterogeneity in study designs and outcome measures limited opportunities for quantitative synthesis.
3. Results
3.1. COVID-19 as a Catalyst for Structural Transformation
The onset of COVID-19 triggered an unprecedented surge in tele-OB/GYN services. Utilization increased by over 500% during the early pandemic period [13], with U.S. OB/GYN visits conducted virtually rising from <1% to 17% [24], and 82% of Indian obstetricians adopting telecare by mid-2020 [15]. In the Middle East, widespread uptake was similarly reported [14], while digital health investment soared by 1818% to USD 788 million in Q1 2020 alone [39]. In Latin America, previously absent platforms saw rapid adoption, transforming telehealth into a structural component of care [16]. By 2022, hybrid care models were adopted by 71% of OB/GYN clinics in high-income countries [42], with routine remote consultations accounting for 9–12% of services [43], signaling a shift from emergency response to sustained delivery mode [12] (Table 1).
3.2. Modalities and Technological Innovations
Tele-OB/GYN services span five main modalities. The most widespread—video and phone consultations—accounted for 60–90% of antenatal and postnatal visits during the pandemic’s peak across India, the U.S., and several Middle Eastern countries [1,5,10,11,24,27,30,44,45]. Remote monitoring innovations—such as home BP cuffs and wearable fetal monitors—enabled the early detection of preeclampsia, increasing detection rates by 22% [3,16,21,22]. In Brazil, nearly half of patients with gestational diabetes used mobile glucose tracking [46], while in Canada, virtual monitoring improved adherence in high-risk pregnancies [23].
Artificial intelligence (AI) technologies have enhanced diagnostic capacity. AI-supported triage and imaging tools achieved 89–92% concordance for fetal anomalies and gynecologic cancers [7,8,20,39,47]. Labor admission AI tools shortened triage times by 35% [48]. Remote procedural supervision, such as guided ultrasound in rural India and Ethiopia, reduced unnecessary referrals by 31% [26,29,34]. Store-and-forward platforms supported 20–35% of asynchronous consults in Ghana, Spain, and Canada, with diagnostic concordance above 80% [5,6,13,49] (Figure 1, Figure 2 and Figure 3).
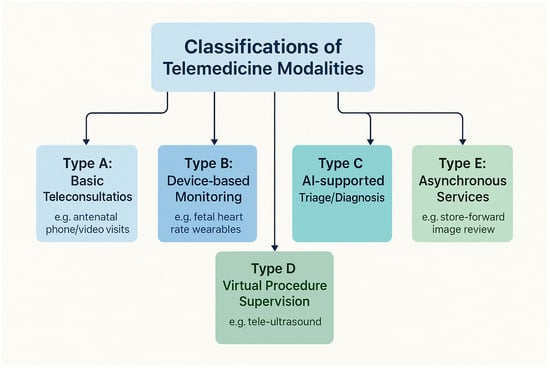
Figure 1.
Classification framework of telemedicine modalities in obstetrics and gynecology.
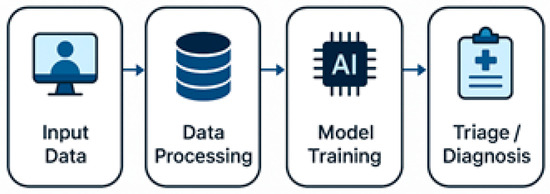
Figure 2.
AI-powered triage and diagnosis pipeline in obstetrics and gynecology.
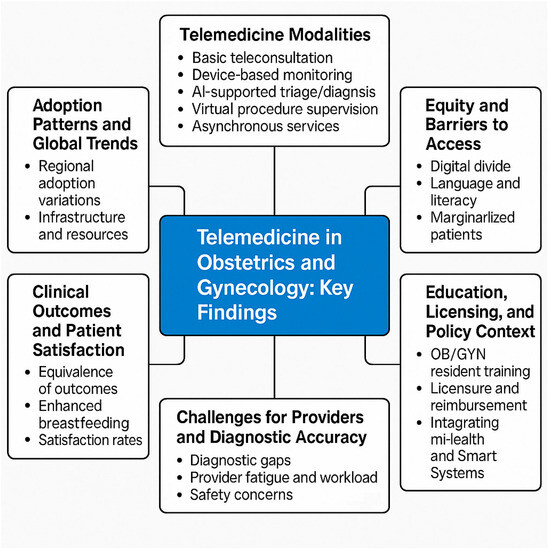
Figure 3.
Conceptual framework of telemedicine in obstetrics and gynecology: key themes and findings.
3.3. Utilization Patterns and Health System Integration
National policy support and infrastructure significantly influenced uptake. In Saudi Arabia, app-based reminders improved OB/GYN appointment adherence from 68% to 89% [38], while Nigeria reported only 29.3% telehealth availability in tertiary centers [35]. Ethiopia’s integration into smart health platforms reduced no-show rates by 30% [7], and Ghana’s expanded telehealth network improved emergency OB/GYN responses by 40% [34,50].
Adolescent reproductive services also transitioned online. In Kenya and the U.S., 41% of young women preferred virtual consultations for contraception [51,52], while mobile apps in Saudi Arabia and Brazil raised appointment adherence by up to 42% [37,46] (Table 1).
3.4. Health Equity and Digital Divide
Barriers to equitable access remain substantial. In Uganda, 57% of pregnant women missed virtual antenatal appointments due to unreliable connectivity [53], and 43% of rural Sub-Saharan African facilities lacked sufficient internet [36,54]. A study in North Carolina found that 15% of OB/GYN patients missed virtual visits due to a lack of devices [27], while urban Senegalese women were 2.7× more likely to access telehealth than their rural counterparts [34].
Language, literacy, and cultural dynamics compound inequity. In the U.S., non-English speakers were 2.2× less likely to complete video visits [55], and in Arab countries, 35% of women avoided teleconsultation due to privacy and modesty concerns [56]. Transgender individuals (47%) and refugee populations in Lebanon reported discomfort or fear in using tele-OB/GYN platforms [18,57]. Racial disparities were evident in the U.S., where Black and Latinx women were 30–36% less likely to complete video consultations [19,28,56] (Table 1; Figure 3).
3.5. Clinical Effectiveness and Health Outcomes
Tele-OB/GYN services showed comparable outcomes to in-person care in several domains. Studies in Canada, the U.S., and Brazil reported no significant differences in blood pressure control, gestational weight gain, or neonatal outcomes [3,24,40,43,46]. In Bangladesh and Nigeria, digital maternal mental health tools reduced PHQ-9 scores by an average of 3.1 points [4,25,31]. Behavioral nudges (e.g., SMS reminders) increased postpartum follow-up compliance by 26% and breastfeeding initiation by 15–20% in Saudi Arabia and India [11,14,22,38].
3.6. Provider Experience and Readiness
Provider acceptance is generally favorable, with 80% of OB/GYN clinicians in Saudi Arabia and the U.S. reporting positive experiences [2,5,15,28,29]. Nonetheless, 41–68% cited fatigue, loss of nonverbal cues, and reduced patient connection [5,15]. Diagnostic concordance for OB/GYN conditions in virtual settings was 89.5% at the Mayo Clinic—lower than for dermatology or psychiatry [59]—and 7% of fetal distress cases in India were missed during remote triage [27].
Training remains inadequate in many settings. While 95% of U.S. residents were exposed to telemedicine, only 48% felt prepared for emotionally complex OB/GYN consults [17,32,33]. In Pakistan, fewer than 25% of OB/GYN students received formal training [60], limiting sustainable adoption (Table 1; Figure 3).
3.7. Policy, Regulation, and Sustainability
Policy frameworks strongly shaped telemedicine’s sustainability. Only 30% of Latin American countries had comprehensive telehealth legislation by 2022 [61,62], and state licensure laws in the U.S. created barriers to cross-state OB/GYN care [61]. Post-pandemic policy retraction in Canada led 74% of OB/GYNs to scale back virtual offerings [13,39].
Privacy concerns persisted across regions. In Europe and Africa, 28% and 43% of OB/GYN patients, respectively, reported reluctance due to confidentiality fears [9,63]. These legal and ethical limitations continue to hinder full-scale digital integration (Table 1; Figure 3).

Table 1.
Thematic summary of telemedicine in obstetrics and gynecology: applications, outcomes, and evidence sources.
Table 1.
Thematic summary of telemedicine in obstetrics and gynecology: applications, outcomes, and evidence sources.
| Theme | Telemedicine Modality/Key Findings | Clinical or System Outcomes | Geographic Focus | References |
|---|---|---|---|---|
| Modalities and Innovations | Synchronous (video/audio), asynchronous (store-and-forward), remote monitoring, AI triage, tele-guided ultrasound | +89% diagnostic concordance (AI); 35% faster triage; 22% improved hypertension detection | US, India, Brazil, Ethiopia | [1,14,15,22,26,27,34,46,50] |
| Utilization and Adoption | >500% increase during COVID-19; sustained 9–12% post-pandemic use; <30% coverage in some LMICs | Improved continuity; increased prenatal visit adherence | US, UK, Nigeria, Saudi Arabia | [5,13,14,24,27,35,38,43] |
| Equity and Accessibility | Barriers: internet access, language, digital literacy, cultural norms | 2.2× lower use in non-English speakers; 57% missed visits due to connectivity; 43% of rural clinics lacked internet | US, Senegal, Lebanon, Uganda, Sub-Saharan Africa | [18,19,27,28,54,55,56,57] |
| Clinical Effectiveness | Virtual prenatal/postnatal care; SMS/mHealth interventions | Equivalent maternal/neonatal outcomes; −3.1 PHQ-9 depression score; +15–20% breastfeeding rates | US, Brazil, Bangladesh, Nigeria, India | [4,11,14,22,24,31,38,40,46] |
| Provider Experience | Satisfaction, burnout, training gaps | 80% perceived benefit; 41–68% screen fatigue; <50% felt emotionally prepared | US, Saudi Arabia, Pakistan | [2,5,15,28,29,32,33,59] |
| Policy and Reimbursement | Licensing constraints; legal frameworks; reimbursement; data privacy | Limited cross-border services; 74% reduced telehealth post-funding | US, Latin America, Canada, Europe | [9,13,16,39,54,61,62] |
| Technology and AI Integration | mHealth apps; AI diagnostics; smart city platforms | +25–42% adherence; >90% cervical cancer AI sensitivity; 34% fewer transfers | Brazil, Saudi Arabia, Ethiopia, Ghana | [7,34,37,38,46,47,48] |
| COVID-19 as Catalyst | Pandemic-driven expansion; emergency tool implementation | 1818% funding increase; sustained hybrid models; 27% oncology treatment delays | Global and US | [24,39,41,42,43,58] |
| Reproductive Health in Adolescents | Tele-contraceptive and educational services | 41% adolescent preference for virtual visits; increased access in underserved areas | Kenya and US | [51,52] |
4. Discussion
The COVID-19 pandemic acted as a powerful catalyst, accelerating the adoption of telemedicine in obstetrics and gynecology (tele-OB/GYN) worldwide. Our review confirms an explosive growth in tele-OB/GYN services, with utilization increasing by over 500% during the pandemic and sustained adoption rates of approximately 10% in high-income countries [5,13,24,27,43]. This surge demonstrated telemedicine’s capacity to maintain continuity of care amid crisis conditions, particularly for low-risk prenatal and postnatal consultations. However, this rapid expansion also highlighted critical ambiguities regarding the clinical boundaries of virtual care and the risks associated with extending telehealth into diagnosis-intensive and procedural domains.
While tele-OB/GYN facilitated effective remote monitoring and routine care, evidence of diagnostic delays and discordances, albeit sparse, calls for caution. Only a minority of studies reported adverse outcomes such as missed fetal distress or delayed cancer diagnoses [41,58,59], and these were typically framed as secondary findings. The conspicuous absence of focused investigations into telemedicine failures or program discontinuations reveals a publication bias skewed toward success narratives. This gap impairs the field’s ability to critically assess safety thresholds and to develop evidence-based guidelines that integrate risk stratification and hybrid care models optimized for maternal and reproductive health.
Despite promises of democratizing access, tele-OB/GYN has not fully addressed persistent inequities. Structural barriers—limited internet infrastructure, digital illiteracy, language obstacles, and cultural constraints—significantly hindered access, especially for marginalized groups [18,19,27,28,54,55,56]. Our synthesis found that populations in rural Sub-Saharan Africa and South Asia experienced disproportionately high rates of missed telehealth visits due to connectivity issues and sociocultural norms. Similarly, ethnic minorities and non-English speakers in high-income countries faced lower tele-visit completion rates. Vulnerable groups such as transgender individuals and refugees expressed unique psychological and privacy concerns, underscoring the necessity for culturally sensitive, inclusive telehealth platform designs that center equity and user agency.
A major limitation identified is the underrepresentation of fragile and low-resource contexts, which bear the greatest maternal health burdens globally. The paucity of studies from conflict-affected or resource-limited settings impedes the generation of context-specific evidence critical for scaling tele-OB/GYN in these environments. Unique challenges—unstable power supplies, weak digital infrastructure, workforce shortages, and policy gaps—are seldom addressed, rendering most current telehealth frameworks technocentric and ill-suited for such fragile health systems. Intentional inclusion of these settings in future research is essential to develop resilient, context-adaptive telemedicine models.
Tele-OB/GYN has redefined the clinical workflow and provider–patient interactions, but not without unintended consequences. While approximately 80% of providers reported perceived benefits, a substantial proportion experienced screen fatigue, emotional detachment, and heightened diagnostic uncertainty [5,15,17,28,29,32,33,58,59]. Training programs largely emphasize technical competencies, with an insufficient focus on communication skills, ethical dilemmas, and emotional intelligence—skills vital for sensitive maternal care. The psychosocial demands of virtual care, including delivering bad news and managing patient distress, remain underexplored and inadequately addressed in curricula, limiting providers’ holistic preparedness.
The sustainable integration of tele-OB/GYN requires more than technological readiness; legal, regulatory, and reimbursement frameworks remain fragmented. Licensing restrictions constrain cross-border consultations, and inconsistent reimbursement policies lead to reduced telehealth usage post-pandemic emergency funding [13,16,39,61,62]. Concerns about data privacy and security persist, particularly among vulnerable populations, and the lack of robust governance in many low- and middle-income countries hinders the transition from pilot projects to scale [9,54,63]. Addressing these policy gaps with equity-focused, rights-based approaches will be crucial for ethical mainstreaming and long-term sustainability.
The evidence base is characterized predominantly by descriptive studies and program evaluations with variable methodological rigor. Longitudinal designs, randomized controlled trials, and comparative effectiveness research are rare. Moreover, there is a lack of synthesis frameworks distinguishing intervention types, contextual factors, and patient subgroups. For tele-OB/GYN to mature as a research field, future studies must adopt rigorous, thematically structured methodologies capable of elucidating not only what works, but why, how, and for whom. Transparent reporting of both successes and failures will enhance learning and inform adaptive implementation strategies.
Telemedicine in obstetrics and gynecology has demonstrated remarkable potential to extend care, improve outcomes, and enhance patient convenience, particularly during public health emergencies. Yet, the clinical, ethical, and equity challenges illuminated by our review underscore that tele-OB/GYN is not a panacea. Achieving safe, equitable, and sustainable virtual maternal healthcare demands robust evidence, inclusive design, comprehensive provider training, and cohesive policy frameworks. Only through a balanced appraisal of both achievements and shortcomings can telemedicine fulfill its promise to transform maternal health globally.
5. Conclusions
Telemedicine in obstetrics and gynecology has rapidly evolved from a crisis-driven innovation to an integral component of contemporary maternal healthcare. This review highlights the diverse modalities underpinning tele-OB/GYN services and their demonstrated potential to enhance access, improve clinical outcomes, and support patient-centered care. However, significant challenges remain, including unresolved clinical boundaries for remote care, critical gaps in addressing implementation failures, and persistent inequities driven by intersecting social determinants.
To realize the full promise of tele-OB/GYN, future research must adopt rigorous, evidence-based methodologies that systematically evaluate both successes and failures across varied settings, with particular attention to low-resource and marginalized populations. The integration of advanced AI-driven tools holds promise but requires careful validation to ensure equity, safety, and acceptability. Furthermore, sustainable expansion depends on cohesive policy frameworks addressing legal, reimbursement, and data privacy concerns.
Ultimately, tele-OB/GYN offers a transformative opportunity to reimagine reproductive healthcare delivery. Achieving this potential demands a holistic, equity-centered approach that balances technological innovation with ethical imperatives and clinical prudence.
Author Contributions
I.E.M.: Conceptualization, writing—original draft preparation, writing—review and editing, writing—original draft preparation; B.R.: Conceptualization, writing—original draft preparation, data curation, resources; A.A.: methodology, software; U.H.C.: validation, writing—review and editing; A.S.: resources, formal analysis, supervision; A.M.H.: original draft preparation, funding acquisition; N.M.A.: formal analysis; M.F.: investigation; B.R., I.E.M. and A.A.: visualization; K.N.H.: original draft preparation, funding acquisition; A.M.D.: writing—review and editing; N.M.Y.: resources, writing—review and editing; N.M.H.: resources, writing—review and editing; N.A.A.: project administration; A.A.R.: writing—review and editing, funding acquisition. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the deanship of scientific research at Jazan University.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data was included in the article.
Acknowledgments
We extend our appreciation to the Deanship of Scientific Research, Jazan University, Saudi Arabia for supporting this research work through the Research Units Support Program We thank all those who made this study possible.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
| STROBE | Strengthening the Reporting of Observational Studies in Epidemiology |
| MMAT | Mixed Methods Appraisal Tool |
| CASP | Critical Appraisal Skills Program |
| JBI | Joanna Briggs Institute Critical Appraisal Tools |
| AMSTAR 2 | A Measurement Tool to Assess Systematic Reviews |
Appendix A

Table A1.
Summary of key studies on telemedicine in obstetrics and gynecology.
Table A1.
Summary of key studies on telemedicine in obstetrics and gynecology.
| No. | Author (s) | Study Design | Year | Location | Main Findings (Concise) |
|---|---|---|---|---|---|
| [1] | Garg S et al. | Review/Commentary | 2020 | India | Telemedicine rapidly embraced during COVID-19, enhancing virtual care delivery. |
| [2] | Hollander JE, Carr BG | Commentary | 2020 | USA | Telemedicine seen as essential and nearly “perfect” solution during COVID-19. |
| [3] | Barbosa W et al. | Review | 2021 | USA | Telemedicine improves access across multiple medical specialties. |
| [4] | Mbunge E et al. | Systematic Review | 2022 | South Africa | Digital health and virtual services deployed effectively in South Africa during COVID-19. |
| [5] | López Seguí F et al. | Cost-Minimization Analysis | 2020 | Catalonia, Spain | Telemedicine more efficient and cost-effective compared to usual care. |
| [6] | Pinnock H et al. | Review | 2022 | UK | Telemedicine and virtual respiratory care expanded during COVID-19. |
| [7] | Burrell DN | Dynamic Evaluation Study | 2023 | USA | Evaluates telehealth tech and AI applications in healthcare organizations. |
| [8] | Chia MA, Turner AW | Review | 2022 | Australia | AI and telemedicine integration benefits outreach eye care. |
| [9] | Haleem A et al. | Review | 2021 | India | Discusses capabilities, barriers, and applications of telemedicine. |
| [10] | Anawade PA et al. | Comprehensive Review | 2024 | India | Telemedicine positively impacts healthcare accessibility. |
| [11] | Amin S et al. | Cross-Sectional | 2024 | Bangladesh | Awareness and barriers to telemedicine adoption among patients identified. |
| [12] | Zobair KM et al. | Cross-Sectional | 2020 | Bangladesh | Barriers to telemedicine adoption in rural areas identified. |
| [13] | Al-Samarraie H et al. | Review | 2020 | Middle East | Progress and policy gaps in telemedicine in Middle Eastern countries. |
| [14] | Du Y et al. | Mixed Methods Study | 2022 | China | Factors affecting telemedicine use in rural China examined. |
| [15] | Arora S et al. | Scoping Review | 2024 | India | Challenges and facilitators of telemedicine implementation described. |
| [16] | Graf C et al. | Review | 2023 | Latin America | Telemedicine adoption in Latin American rheumatology post-COVID. |
| [17] | Haimi M | Narrative Review | 2023 | Not specified | Paradoxical effects of telemedicine on healthcare disparities highlighted. |
| [18] | Hamnvik O-PR et al. | Review/Commentary | 2020 | USA | Telemedicine access inequities in transgender healthcare explored. |
| [19] | Haynes N et al. | Commentary | 2021 | USA | Racial and ethnic disparities in telehealth usage addressed. |
| [20] | Masterson Creber R et al. | Scientific Statement | 2023 | USA | Telehealth and equity considerations in heart failure care in older adults. |
| [21] | Brown HL, Denicola N | Review | 2020 | USA | Telehealth use in maternity care reviewed. |
| [22] | Denicola N et al. | Systematic Review | 2020 | USA | Telehealth interventions improve obstetric and gynecologic outcomes. |
| [23] | Fix L et al. | Qualitative Study | 2020 | Australia | Patient experiences with at-home telemedicine for abortion analyzed. |
| [24] | Gyamfi-Bannerman G et al. | Cohort Study | 2020 | USA | Telehealth effective for high-risk pregnancy management during COVID-19. |
| [25] | Schummers L et al. | Observational Study | 2022 | Canada | Safety and use of medical abortion with telemedicine confirmed. |
| [26] | Lapadula MC et al. | Cross-Sectional Survey | 2021 | USA | High satisfaction with telemedicine prenatal consults during COVID-19. |
| [27] | Fryer K et al. | Implementation Study | 2020 | USA | Obstetric telehealth rapidly implemented during COVID-19. |
| [28] | Sengupta A et al. | Qualitative Study | 2023 | Australia | Telemedicine in specialist outpatient care during COVID-19 explored. |
| [29] | Smith WR et al. | Implementation Guide | 2020 | USA | Rapid outpatient telemedicine program integration during pandemic described. |
| [30] | Apathy NC et al. | Observational Study | 2023 | USA | Physician telemedicine usage varies significantly. |
| [31] | Kung LH et al. | Empirical Study | 2024 | Taiwan | Usage differences in telemedicine by rural vs. urban patients studied. |
| [32] | Iancu AM et al. | Commentary/Experience | 2020 | USA | Telemedicine in medical education during COVID-19 enhances student engagement. |
| [33] | Jumreornvong O et al. | Commentary/Review | 2020 | USA | Telemedicine’s role in medical education during COVID-19 expanded. |
| [34] | Ly BA et al. | Descriptive Study | 2017 | Senegal | Physician perceptions and determinants of telemedicine use described. |
| [35] | Wubante SM et al. | Cross-Sectional | 2022 | Ethiopia | Readiness of health professionals to implement telemedicine assessed. |
| [36] | Olufunlayo TF et al. | Cross-Sectional | 2023 | Nigeria | Telemedicine maturity assessed in tertiary hospitals. |
| [37] | Mohammadzadeh Z et al. | Systematic Review | 2023 | Developing Nations | Smart city healthcare tech and indicators reviewed. |
| [38] | Taha AR et al. | Cross-Sectional | 2022 | UAE | Integration of mHealth in telemedicine during COVID-19 described. |
| [39] | Zobair KM et al. | Predictive Modeling Study | 2021 | Bangladesh | Machine learning predicts telemedicine patient satisfaction. |
| [40] | Baughman DJ et al. | Comparative Study | 2022 | USA | Quality of care measures comparable between telemedicine and in-person visits. |
| [41] | Abdulwahab S, Zedan H | Cross-Sectional | 2021 | Saudi Arabia | Factors influencing patient satisfaction with telemedicine identified. |
| [42] | Palmer KR et al. | Interrupted Time Series | 2021 | Australia | Low-cost antenatal telehealth widely implemented during COVID-19. |
| [43] | Patel SY et al. | Observational Study | 2021 | USA | Community factors influencing telemedicine use during COVID-19 analyzed. |
| [44] | Reed M et al. | Observational Study | 2021 | USA | Telemedicine visits linked to comparable follow-up and treatment as in-person visits. |
| [45] | Larsen SB et al. | Descriptive/Policy Paper | 2015 | Denmark | Proposal for shared telemedicine service center. |
| [46] | Silva AB et al. | Regulatory Review | 2020 | Brazil | Telemedicine regulatory framework mapped over 30 years. |
| [47] | Sageena G et al. | Review | 2021 | India | Evolution of telemedicine during COVID-19 described. |
| [48] | MacDonald SM, Berv J | Commentary | 2022 | USA | Telemedicine may risk weakening patient–provider relationship. |
| [49] | Ncube B et al. | Exploratory Study | 2023 | Botswana | Patient and provider attitudes toward telemedicine examined. |
| [50] | Khatana SAM et al. | Database Analysis | 2022 | USA | Predictors of telemedicine use during COVID-19 identified. |
| [51] | Waqas A et al. | Bibliometric Analysis | 2020 | UK | Telemedicine research trends analyzed. |
| [52] | Tye ML et al. | Perception Survey | 2020 | USA | School-based telemedicine model perceptions evaluated. |
| [53] | Chiu CY et al. | Survey Study | 2021 | USA (NYC) | Internal medicine residents’ telemedicine experiences during COVID-19 documented. |
| [54] | Stoltzfus M et al. | Review | 2023 | India | Comprehensive telemedicine role update. |
| [55] | Hsueh L et al. | Observational Study | 2021 | USA | Limited English proficiency patients face disparities in video telemedicine use. |
| [56] | Eberly LA et al. | Observational Study | 2020 | USA | Patient factors influencing telemedicine access during COVID-19 studied. |
| [57] | Reed ME et al. | Observational Study | 2020 | USA | Patient characteristics associated with telemedicine choice analyzed. |
| [58] | Waseem N et al. | Observational Study | 2022 | USA | Telemedicine success disparities linked to adverse outcomes in thoracic cancer patients. |
| [59] | Demaerschalk BM et al. | Diagnostic Concordance Study | 2022 | USA | High diagnostic concordance between video telemedicine and in-person consultations. |
| [60] | Scott AC et al. | Program Description | 2020 | Australia | Cardiovascular telemedicine program improves rural healthcare. |
| [61] | Mehrotra A, Uscher-Pines L | Commentary | 2022 | USA | Telemedicine reimbursement knowledge gaps highlighted. |
| [62] | Mehrotra A et al. | Commentary | 2021 | USA | Telemedicine medical licensure reform discussed. |
| [63] | Wang Y et al. | Case Analysis | 2021 | China | Telemedicine application during COVID-19 pandemic analyzed. |
Appendix B. Full Search String
- Databases Searched:
- PubMed.
- Scopus.
- Google Scholar.
- Search Period:
- January 2010–December 2023.
- Search Strategy (example used in PubMed):
- (“telemedicine”[MeSH Terms] OR “telemedicine”[All Fields] OR “telehealth”[All Fields] OR “remote consultation”[All Fields]).
- AND (“obstetrics”[MeSH Terms] OR “obstetrics”[All Fields] OR “gynecology”[MeSH Terms] OR “gynecology”[All Fields]).
- AND (“rural health”[MeSH Terms] OR “rural healthcare”[All Fields] OR “urban health”[MeSH Terms] OR “urban healthcare”[All Fields]).
- AND (“digital literacy”[All Fields] OR “health literacy”[MeSH Terms]).
- AND (“artificial intelligence”[MeSH Terms] OR “AI”[All Fields] OR “machine learning”[All Fields]).
- AND (“COVID-19”[MeSH Terms] OR “pandemic”[All Fields]).
- Filters Applied:
- Language: English.
- Article type: Peer-reviewed articles.
- Study types: Empirical studies, program evaluations, case studies.
- Population: Human subjects.
- Additional Sources:
- Manual screening of reference lists from included studies.
Appendix C
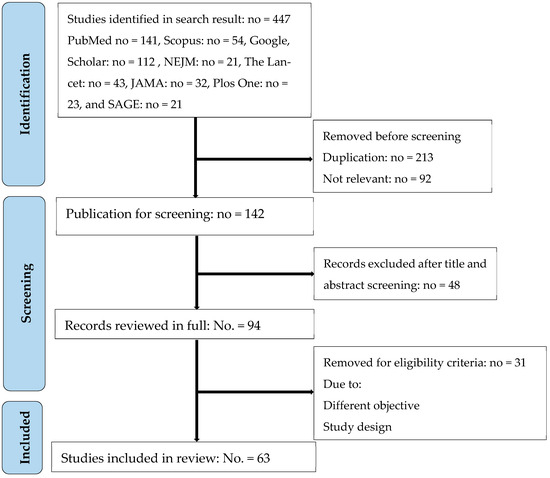
Figure A1.
PRISMA-ScR flowchart showing process for selection of included studies.
Appendix D

Table A2.
Example of study quality assessment table.
Table A2.
Example of study quality assessment table.
| Study ID | Author (s) | Country | Study Design | Quality Assessment Tool | Overall Quality Rating |
|---|---|---|---|---|---|
| S1 | [2] | Bangladesh | Cross-sectional | STROBE | Moderate |
| S2 | [4] | India | Mixed methods | MMAT | High |
| S3 | [11] | China | Mixed methods | MMAT | Moderate |
| S4 | [12] | Australia | Qualitative | CASP | High |
| S5 | [13] | USA | Observational | STROBE | High |
| S6 | [14] | USA | Case series | JBI | Moderate |
| S7 | [17] | USA | Survey | STROBE | Moderate |
| S8 | [24] | Multi-country | Cohort | STROBE | High |
| S9 | [25] | South Africa | Systematic review | AMSTAR 2 | High |
| S10 | [34] | Bangladesh | Survey | STROBE | Moderate |
References
- Garg, S.; Gangadharan, N.; Bhatnagar, N.; Singh, M.M.; Raina, S.K.; Galwankar, S. Telemedicine: Embracing virtual care during COVID-19 pandemic. J. Fam. Med. Prim. Care 2020, 9, 4516–4520. [Google Scholar] [CrossRef]
- Hollander, J.E.; Carr, B.G. Virtually perfect? Telemedicine for COVID-19. N. Engl. J. Med. 2020, 382, 1679–1681. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, W.; Dorsey, E.R.; Zhou, K.; Waddell, E.; Myers, T. Improving access to care: Telemedicine across medical domains. Annu. Rev. Public Health 2021, 42, 463–481. [Google Scholar] [CrossRef]
- Mbunge, E.; Batani, J.; Gaobotse, G.; Muchemwa, B. Virtual healthcare services and digital health technologies deployed during coronavirus disease 2019 (COVID-19) pandemic in South Africa: A systematic review. Glob. Health J. 2022, 6, 102–113. [Google Scholar] [CrossRef]
- López Seguí, F.; García Cuyàs, F.; Vidal-Alaball, J.; Mendioroz Peña, J.; Gironès García, X.; Adroher Mas, C.; García-Altés, A.; Vidal-Alaball, J. A cost-minimization analysis of a medical record-based, store and forward and provider-to-provider telemedicine compared to usual care in Catalonia: More agile and efficient, especially for users. Int. J. Environ. Res. Public Health 2020, 17, 2008. [Google Scholar] [CrossRef]
- Pinnock, H.; Vogiatzis, I.; Murphie, P.; Poberezhets, V. Telemedicine and virtual respiratory care in the era of COVID-19. ERJ Open Res. 2022, 8, 00111-2022. [Google Scholar] [CrossRef] [PubMed]
- Burrell, D.N. Dynamic evaluation approaches to telehealth technologies and artificial intelligence (AI) telemedicine applications in healthcare and biotechnology organizations. Merits 2023, 3, 700–721. [Google Scholar] [CrossRef]
- Chia, M.A.; Turner, A.W. Benefits of integrating telemedicine and artificial intelligence into outreach eye care: Stepwise approach and future directions. Front. Med. 2022, 9, 835804. [Google Scholar] [CrossRef]
- Haleem, A.; Javaid, M.; Singh, R.P.; Suman, R. Telemedicine for healthcare: Capabilities, features, barriers, and applications. Sens. Int. 2021, 2, 100117. [Google Scholar] [CrossRef] [PubMed]
- Anawade, P.A.; Sharma, D.; Gahane, S. A comprehensive review on exploring the impact of telemedicine on healthcare accessibility. Cureus 2024, 16, e55996. [Google Scholar] [CrossRef]
- Amin, S.; Mustofa, M.; Barman, H.; Rahman, A. An exploratory cross-sectional study of awareness and barriers to adoption of telemedicine services among patients in Bangladesh. Future Health 2024, 2, 107–113. [Google Scholar] [CrossRef]
- Zobair, K.M.; Sanzogni, L.; Sandhu, K. Telemedicine healthcare service adoption barriers in rural Bangladesh. Australas. J. Inf. Syst. 2020, 24. [Google Scholar] [CrossRef]
- Al-Samarraie, H.; Ghazal, S.; Alzahrani, A.I.; Moody, L. Telemedicine in Middle Eastern countries: Progress, barriers, and policy recommendations. Int. J. Med. Inform. 2020, 141, 104232. [Google Scholar] [CrossRef] [PubMed]
- Du, Y.; Tang, W.; Xue, H.; Sylvia, S.; Zhang, Z.; Hoelzer, S.; Zhou, Q.; Cheng, W.; Liang, Y.; Ma, X.; et al. Factors influencing adoption and use of telemedicine services in rural areas of China: Mixed methods study. JMIR Public Health Surveill. 2022, 8, e40771. [Google Scholar] [CrossRef]
- Arora, S.; Huda, R.K.; Verma, S.; Khetan, M.; Sangwan, R.K. Challenges, barriers, and facilitators in telemedicine implementation in India: A scoping review. Cureus 2024, 16, e67388. [Google Scholar] [CrossRef]
- Graf, C.; Soriano, E.R.; Fernández-Ávila, D.G.; Plazzotta, F. Telehealth and telemedicine in Latin American rheumatology, a new era after COVID-19. J. Clin. Rheumatol. 2023, 29, 165–169. [Google Scholar] [CrossRef]
- Haimi, M. The tragic paradoxical effect of telemedicine on healthcare disparities—A time for redemption: A narrative review. BMC Med. Inform. Decis. Mak. 2023, 23, 95. [Google Scholar] [CrossRef]
- Hamnvik, O.-P.R.; Ahnallen, C.G.; Agarwal, S.; Reisner, S.L.; Goldman, A.L. Telemedicine and inequities in health care access: The example of transgender health. Transgend. Health 2020, 7, 113–116. [Google Scholar] [CrossRef]
- Haynes, N.; Haynes, M.; Swain, J.; Nunes, K.; Gumbs, E.; Ezekwesili, A. “Can you see my screen?” Addressing racial and ethnic disparities in telehealth. Curr. Cardiol. Risk Rep. 2021, 15, 23. [Google Scholar] [CrossRef]
- Masterson Creber, R.; Bidwell, J.; Harmon Still, C.; Dodson, J.A.; Lyles, C.; Ooi, S.Y.; Breathett, K.; Yancy, C.; Kitsiou, S. Telehealth and health equity in older adults with heart failure: A scientific statement from the American Heart Association. Circ. Cardiovasc. Qual. Outcomes 2023, 16, e0000123. [Google Scholar] [CrossRef] [PubMed]
- Brown, H.L.; Denicola, N. Telehealth in maternity care. Obstet. Gynecol. Clin. N. Am. 2020, 47, 497–502. [Google Scholar] [CrossRef]
- Denicola, N.; Witkop, C.T.; Sonalkar, S.; Henderson, J.T.; Butler Tobah, Y.S.; Ganju, N.; Grossman, D.; Marko, K.; Butler, J.; Lowery, C.; et al. Telehealth interventions to improve obstetric and gynecologic health outcomes: A systematic review. Obstet. Gynecol. 2020, 135, 371–382. [Google Scholar] [CrossRef]
- Fix, L.; Mazza, D.; Sandhu, M.V.; Seymour, J.W.; Thompson, T.-A.; Melville, C. At-home telemedicine for medical abortion in Australia: A qualitative study of patient experiences and recommendations. BMJ Sex. Reprod. Health 2020, 46, 172–176. [Google Scholar] [CrossRef] [PubMed]
- Gyamfi-Bannerman, C.; Friedman, A.M.; Aziz, A.; Yates, H.S.; Miller, R.S.; Moroz, L.; Zork, N.; Aubey, J.J.; Baptiste, C.D.; D’Alton, M.E.; et al. Telehealth for high-risk pregnancies in the setting of the COVID-19 pandemic. Am. J. Perinatol. 2020, 37, 800–808. [Google Scholar] [CrossRef] [PubMed]
- Schummers, L.; Darling, E.K.; Dunn, S.; McGrail, K.; Gayowsky, A.; Law, M.R.; Laba, T.-L.; Kaczorowski, J.; Norman, W.V. Abortion safety and use with normally prescribed mifepristone in Canada. N. Engl. J. Med. 2022, 386, 57–67. [Google Scholar] [CrossRef]
- Lapadula, M.C.; Clark, T.; Makkar, A.; Szyld, E.G.; Rolfs, S.; Hallford, G.; McCoy, M.; McKnight, S. Evaluating patients’ and neonatologists’ satisfaction with the use of telemedicine for neonatology prenatal consultations during the COVID-19 pandemic. Front. Pediatr. 2021, 9, 642369. [Google Scholar] [CrossRef]
- Fryer, K.; Foti, T.; Delgado, A.; Reid, C.N.; Marshall, J. Implementation of obstetric telehealth during COVID-19 and beyond. Matern. Child Health J. 2020, 24, 1104–1110. [Google Scholar] [CrossRef]
- Sengupta, A.; Jenkins, C.R.; Pettigrew, S. Telemedicine in specialist outpatient care during COVID-19: A qualitative study. Intern. Med. J. 2023, 54, 54–61. [Google Scholar] [CrossRef]
- Smith, W.R.; Atala, A.J.; Terlecki, R.P.; Kelly, E.E.; Matthews, C.A. Implementation guide for rapid integration of an outpatient telemedicine program during the COVID-19 pandemic. J. Am. Coll. Surg. 2020, 231, 216–222.e2. [Google Scholar] [CrossRef] [PubMed]
- Apathy, N.C.; Dixit, R.A.; Boxley, C.L.; Adams, K.T.; Booker, E.; Ratwani, R.M. Variations in physician telemedicine provision. JAMA Netw. Open 2023, 6, e2321955. [Google Scholar] [CrossRef]
- Kung, L.H.; Yan, Y.H.; Kung, C.M. Empirical study on the usage of telemedicine by rural and urban health care consumers in Taiwan: Integrating the perspectives of technology acceptance model and theory of planned behavior. Telemed. J. E-Health 2024, 30, 2630–2636. [Google Scholar] [CrossRef]
- Iancu, A.M.; Alam, H.B.; Kemp, M.T. Unmuting medical students’ education: Utilizing telemedicine during the COVID-19 pandemic and beyond. J. Med. Internet Res. 2020, 22, e19667. [Google Scholar] [CrossRef]
- Jumreornvong, O.; Appel, J.; Race, J.; Yang, E. Telemedicine and medical education in the age of COVID-19. Acad. Med. 2020, 95, 1838–1843. [Google Scholar] [CrossRef]
- Ly, B.A.; Labonté, R.; Bourgeault, I.L.; Niang, M.N. The individual and contextual determinants of the use of telemedicine: A descriptive study of the perceptions of Senegal’s physicians and telemedicine projects managers. PLoS ONE 2017, 12, e0181070. [Google Scholar] [CrossRef]
- Wubante, S.M.; Nigatu, A.M.; Jemere, A.T. Health professionals’ readiness and its associated factors to implement telemedicine system at private hospitals in Amhara region, Ethiopia 2021. PLoS ONE 2022, 17, e0275133. [Google Scholar] [CrossRef] [PubMed]
- Olufunlayo, T.F.; Ojo, O.O.; Ozoh, O.B.; Agabi, O.P.; Opara, C.R.; Taiwo, F.T.; A Fasanmade, O.; Okubadejo, N.U. Telemedicine ready or not? A cross-sectional assessment of telemedicine maturity of federally funded tertiary health institutions in Nigeria. Digit. Health 2023, 9, 20552076221150072. [Google Scholar] [CrossRef] [PubMed]
- Mohammadzadeh, Z.; Saeidnia, H.R.; Lotfata, A.; Hassanzadeh, M.; Ghiasi, N. Smart city healthcare delivery innovations: A systematic review of essential technologies and indicators for developing nations. BMC Health Serv. Res. 2023, 23, 236. [Google Scholar] [CrossRef] [PubMed]
- Taha, A.R.; Shehadeh, M.; Alshehhi, A.; Altamimi, T.; Housser, E.; Simsekler, M.C.E.; Alfalasi, B.; Al Memari, S.; Al Hosani, F.; Al Zaabi, Y.; et al. The integration of mHealth technologies in telemedicine during the COVID-19 era: A cross-sectional study. PLoS ONE 2022, 17, e0264436. [Google Scholar] [CrossRef]
- Zobair, K.M.; Islam, M.Z.; Houghton, L.; Sanzogni, L. Forecasting care seekers’ satisfaction with telemedicine using machine learning and structural equation modelling. PLoS ONE 2021, 16, e0257300. [Google Scholar] [CrossRef]
- Baughman, D.J.; Jabbarpour, Y.; Westfall, J.M.; Jetty, A.; Zain, A.; Baughman, K.; Pollak, B.; Waheed, A. Comparison of quality performance measures for patients receiving in-person vs telemedicine primary care in a large integrated health system. JAMA Netw. Open 2022, 5, e2233267. [Google Scholar] [CrossRef]
- Abdulwahab, S.; Zedan, H. Factors affecting patient perceptions and satisfaction with telemedicine in outpatient clinics. J. Patient Exp. 2021, 8, 23743735211063780. [Google Scholar] [CrossRef]
- Palmer, K.R.; Tanner, M.; Davies-Tuck, M.; Rindt, A.; Papacostas, K.; Giles, M.L.; Brown, K.; Diamandis, H.; Fradkin, R.; E Stewart, A.; et al. Widespread implementation of a low-cost telehealth service in the delivery of antenatal care during the COVID-19 pandemic: An interrupted time-series analysis. Lancet 2021, 398, 41–52. [Google Scholar] [CrossRef]
- Patel, S.Y.; Rose, S.; Barnett, M.L.; Huskamp, H.A.; Uscher-Pines, L.; Mehrotra, A. Community factors associated with telemedicine use during the COVID-19 pandemic. JAMA Netw. Open 2021, 4, e2110330. [Google Scholar] [CrossRef] [PubMed]
- Reed, M.; Huang, J.; Graetz, I.; Muelly, E.; Millman, A.; Lee, C. Treatment and follow-up care associated with patient-scheduled primary care telemedicine and in-person visits in a large integrated health system. JAMA Netw. Open 2021, 4, e2132793. [Google Scholar] [CrossRef] [PubMed]
- Larsen, S.B.; Sørensen, N.S.; Petersen, M.G.; Kjeldsen, G.F. Towards a shared service center for telemedicine: Telemedicine in Denmark, and a possible way forward. Health Inform. J. 2015, 22, 815–827. [Google Scholar] [CrossRef] [PubMed]
- Silva, A.B.; da Silva, R.M.; Ribeiro, G.d.R.; Guedes, A.C.C.M.; Santos, D.L.; Nepomuceno, C.C.; Caetano, R.; Makkar, A. Three decades of telemedicine in Brazil: Mapping the regulatory framework from 1990 to 2018. PLoS ONE 2020, 15, e0242869. [Google Scholar] [CrossRef]
- Sageena, G.; Kapur, A.; Sharma, M. Evolution of smart healthcare: Telemedicine during COVID-19 pandemic. J. Inst. Eng. India Ser. B 2021, 102, 1319–1324. [Google Scholar] [CrossRef]
- MacDonald, S.M.; Berv, J. Losing contact—COVID-19, telemedicine, and the patient-provider relationship. N. Engl. J. Med. 2022, 387, 775–777. [Google Scholar] [CrossRef] [PubMed]
- Ncube, B.; Mars, M.; Scott, R.E. Perceptions and attitudes of patients and healthcare workers towards the use of telemedicine in Botswana: An exploratory study. PLoS ONE 2023, 18, e0281754. [Google Scholar] [CrossRef]
- Khatana, S.A.M.; Yang, L.; Eberly, L.A.; Julien, H.M.; Adusumalli, S.; Groeneveld, P.W. Predictors of telemedicine use during the COVID-19 pandemic in the United States: An analysis of a national electronic medical record database. PLoS ONE 2022, 17, e0269535. [Google Scholar] [CrossRef]
- Waqas, A.; Teoh, S.H.; Lapão, L.V.; Messina, L.A.; Correia, J.C. Harnessing telemedicine for the provision of health care: Bibliometric and scientometric analysis. J. Med. Internet Res. 2020, 22, e18835. [Google Scholar] [CrossRef] [PubMed]
- Tye, M.L.; Honey, M.; Day, K. School-based telemedicine: Perceptions about a telemedicine model of care. Health Inform. J. 2020, 26, 2030–2041. [Google Scholar] [CrossRef] [PubMed]
- Chiu, C.Y.; Sarwal, A.; Jawed, M.; Chemarthi, V.S.; Shabarek, N. Telemedicine experience of NYC internal medicine residents during COVID-19 pandemic. PLoS ONE 2021, 16, e0246762. [Google Scholar] [CrossRef]
- Stoltzfus, M.; Kaur, A.; Chawla, A.; Anamika, F.N.U.; Jain, R.; Gupta, V. The role of telemedicine in healthcare: An overview and update. Egypt. J. Intern. Med. 2023, 35, 26. [Google Scholar] [CrossRef]
- Hsueh, L.; Huang, J.; Millman, A.K.; Gopalan, A.; Parikh, R.K.; Teran, S.; Reed, M.E. Disparities in use of video telemedicine among patients with limited English proficiency during the COVID-19 pandemic. JAMA Netw. Open 2021, 4, e2133129. [Google Scholar] [CrossRef]
- Eberly, L.A.; Kallan, M.J.; Julien, H.M.; Haynes, N.; Khatana, S.A.M.; Nathan, A.S.; Snider, C.; Chokshi, N.P.; Eneanya, N.D.; Takvorian, S.U.; et al. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. JAMA Netw. Open 2020, 3, e2031640. [Google Scholar] [CrossRef]
- Reed, M.E.; Huang, J.; Graetz, I.; Lee, C.; Muelly, E.; Kennedy, C.; Kim, E. Patient characteristics associated with choosing a telemedicine visit vs office visit with the same primary care clinicians. JAMA Netw. Open 2020, 3, e205873. [Google Scholar] [CrossRef]
- Waseem, N.; Boulanger, M.; Yanek, L.R.; Feliciano, J.L. Disparities in telemedicine success and their association with adverse outcomes in patients with thoracic cancer during the COVID-19 pandemic. JAMA Netw. Open 2022, 5, e2220543. [Google Scholar] [CrossRef]
- Demaerschalk, B.M.; Pines, A.; Butterfield, R.; Haglin, J.M.; Haddad, T.C.; Yiannias, J.; Colby, C.E.; TerKonda, S.P.; Ommen, S.R.; Bushman, M.S.; et al. Assessment of clinician diagnostic concordance with video telemedicine in the integrated multispecialty practice at Mayo Clinic during the beginning of COVID-19 pandemic from March to June 2020. JAMA Netw. Open 2022, 5, e2229958. [Google Scholar] [CrossRef]
- Scott, A.C.; McDonald, A.; Roberts, T.; Martin, C.; Manns, T.; Webster, M.; Walker, D.; Sandford, A.; Scuffham, P.; Atherton, J.J. Cardiovascular telemedicine program in rural Australia. N. Engl. J. Med. 2020, 383, 883–884. [Google Scholar] [CrossRef] [PubMed]
- Mehrotra, A.; Uscher-Pines, L. Informing the debate about telemedicine reimbursement—What do we need to know? N. Engl. J. Med. 2022, 387, 1821–1823. [Google Scholar] [CrossRef] [PubMed]
- Mehrotra, A.; Nimgaonkar, A.; Richman, B. Telemedicine and medical licensure—Potential paths for reform. N. Engl. J. Med. 2021, 384, 687–690. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Yang, J.; Ma, H.; Dong, X.; Xie, G.; Ye, S.; Du, J. Application of telemedicine in the COVID-19 epidemic: An analysis of Gansu Province in China. PLoS ONE 2021, 16, e0249872. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).