Enhancing Dentists’ Resilience and Occupational Sustainability Through Physical Activity: A Systematic Review in the Post-Pandemic Context
Abstract
1. Introduction
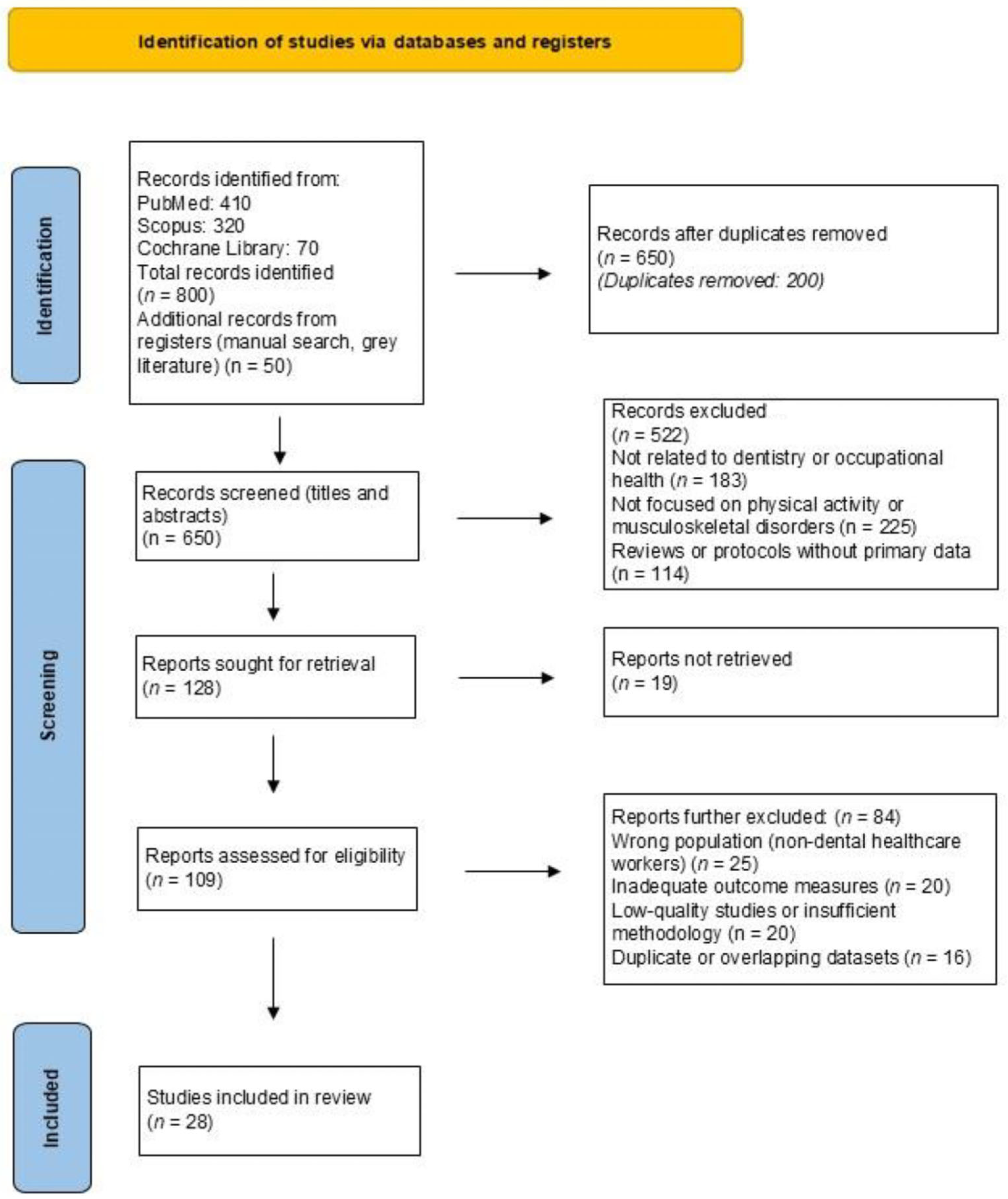
2. Materials and Methods
3. Results
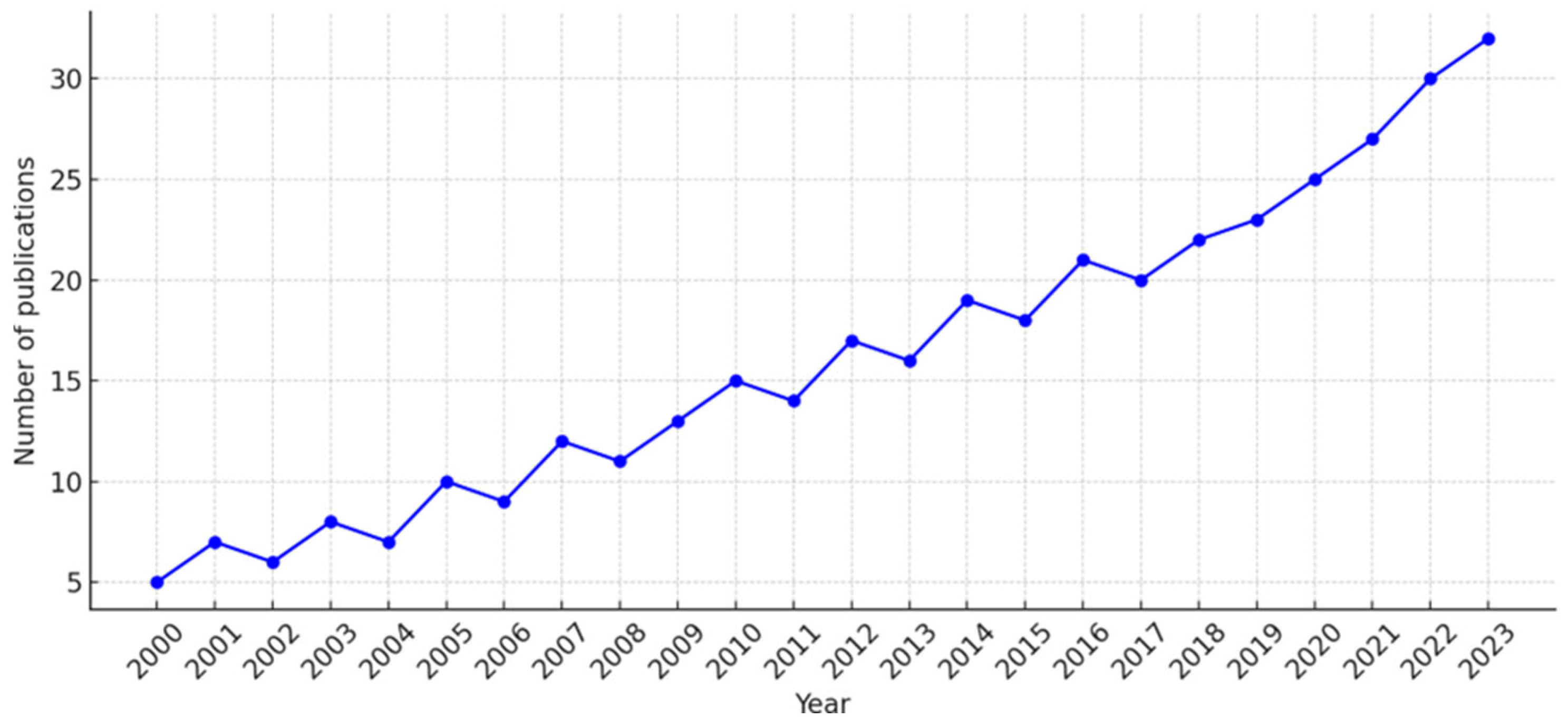
3.1. Trends in Research on Physical Activity and Dental Health
3.2. Geographic and Sectoral Distribution of Included Studies
3.3. Population and Sample Size
3.4. Data Collection Methods
3.5. Statistical Analysis Methods
3.6. Cultural Diversities
3.7. Prevalence and Risk Factors of Musculoskeletal Disorders (MSDs)
3.8. Physical Activity as a Protective Factor
3.9. The Role of Physical Activity in Regulating Sleep, Coping with Stress, and Building Resilience
3.10. Stress Management and Holistic Interventions in Dentistry
3.11. Tailored Interventions and Cultural Approaches to Occupational Health
3.12. The Importance of Education and Continuous Professional Development
3.13. Sensitivity Analysis
4. Discussion
4.1. Practical Recommendations for Dental Professionals and Institutions
4.2. Professional Identity and Role Modeling
4.3. Contextualizing Interventions by Culture and Resources
4.4. Long-Term Sustainability of Wellness Practices
4.5. Limitations and Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kelly, D.; Shorthouse, F.; Roffi, V.; Tack, C. Exercise therapy and work-related musculoskeletal disorders in sedentary workers. Occup. Med. 2018, 68, 262–272. [Google Scholar] [CrossRef]
- Large, A. Managing patient expectations. BDJ Team 2020, 7, 31. [Google Scholar] [CrossRef]
- Tonni, I.; Gadbury-Amyot, C.C.; Govaerts, M.; Ten Cate, O.; Davis, J.; Garcia, L.T.; Valachovic, R.W. ADEA-ADEE Shaping the Future of Dental Education III: Assessment in competency-based dental education: Ways forward. J. Dent. Educ. 2020, 84, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Azimi, S.; Azimi, S.; Azami, M. Occupational Hazards/Risks among Dental Staff in Afghanistan. Int. Intern. Med. J. 2024, 2, 1–6. [Google Scholar] [CrossRef]
- Antoniadou, M. Estimation of factors affecting burnout in Greek dentists before and during the COVID-19 pandemic. Dent. J. 2022, 10, 108. [Google Scholar] [CrossRef] [PubMed]
- Antoniadou, M.; Mangoulia, P.; Myrianthefs, P. Quality of life and wellbeing parameters of academic dental and nursing personnel vs. quality of services. Healthcare 2023, 11, 2792. [Google Scholar] [CrossRef]
- Miron, C.; Colosi, H.A. Work stress, health behaviours and coping strategies of dentists from Cluj-Napoca, Romania. Int. Dent. J. 2018, 68, 152–161. [Google Scholar] [CrossRef]
- Arslan, S.S.; Alemdaroğlu, İ.; Karaduman, A.A.; Yilmaz, Ö.T. The effects of physical activity on sleep quality, job satisfaction, and quality of life in office workers. Work 2019, 63, 3–7. [Google Scholar] [CrossRef]
- Kurtović, A.; Talapko, J.; Bekić, S.; Škrlec, I. The relationship between sleep, chronotype, and dental caries: A narrative review. Clocks Sleep 2023, 5, 295–312. [Google Scholar] [CrossRef]
- Gandolfi, M.G.; Zamparini, F.; Spinelli, A.; Risi, A.; Prati, C. Musculoskeletal disorders among Italian dentists and dental hygienists. Int. J. Environ. Res. Public Health 2021, 18, 2705. [Google Scholar] [CrossRef]
- Stults-Kolehmainen, M.A.; Sinha, R. The effects of stress on physical activity and exercise. Sports Med. 2014, 44, 81–121. [Google Scholar] [CrossRef]
- Serra, M.V.G.B.; Camargo, P.R.; Zaia, J.E.; Tonello, M.G.M.; Quemelo, P.R.V. Effects of physical exercise on musculoskeletal disorders, stress and quality of life in workers. Int. J. Occup. Saf. Ergon. 2018, 24, 62–67. [Google Scholar] [CrossRef]
- Martín-Rodríguez, A.; Gostian-Ropotin, L.A.; Beltrán-Velasco, A.I.; Belando-Pedreño, N.; Simón, J.A.; López-Mora, C.; Navarro-Jiménez, E.; Tornero-Aguilera, J.F.; Clemente-Suárez, V.J. Sporting mind: The interplay of physical activity and psychological health. Sports 2024, 12, 37. [Google Scholar] [CrossRef] [PubMed]
- Basso, J.C.; Suzuki, W.A. The effects of acute exercise on mood, cognition, neurophysiology, and neurochemical pathways: A review. Brain Plast. 2017, 2, 127–152. [Google Scholar] [CrossRef] [PubMed]
- Alnawwar, M.A.; Alraddadi, M.I.; Algethmi, R.A.; Salem, G.A.; Salem, M.A.; Alharbi, A.A. The Effect of Physical Activity on Sleep Quality and Sleep Disorder: A Systematic Review. Cureus 2023, 15, e43595. [Google Scholar] [CrossRef] [PubMed]
- Dhuli, K.; Naureen, Z.; Medori, M.C.; Fioretti, F.; Caruso, P.; Perrone, M.A.; Nodari, S.; Manganotti, P.; Xhufi, S.; Bushati, M.; et al. Physical activity for health. J. Prev. Med. Hyg. 2022, 63 (Suppl. S3), E150–E159. [Google Scholar] [CrossRef]
- Militello, R.; Luti, S.; Gamberi, T.; Pellegrino, A.; Modesti, A.; Modesti, P.A. Physical Activity and Oxidative Stress in Aging. Antioxidants 2024, 13, 557. [Google Scholar] [CrossRef]
- Yang, J.; Luo, J.; Tian, X.; Zhao, Y.; Li, Y.; Wu, X. Progress in Understanding Oxidative Stress, Aging, and Aging-Related Diseases. Antioxidants 2024, 13, 394. [Google Scholar] [CrossRef]
- Burini, R.C.; Anderson, E.; Durstine, J.L.; Carson, J.A. Inflammation, physical activity, and chronic disease: An evolutionary perspective. Sports Med. Health Sci. 2020, 2, 1–6. [Google Scholar] [CrossRef]
- Núñez-Cortés, R.; Salazar-Méndez, J.; Nijs, J. Physical Activity as a Central Pillar of Lifestyle Modification in the Management of Chronic Musculoskeletal Pain: A Narrative Review. J. Funct. Morphol. Kinesiol. 2025, 10, 183. [Google Scholar] [CrossRef]
- Nilsen, P.; Seing, I.; Ericsson, C.; Birken, S.A.; Schildmeijer, K. Characteristics of successful changes in health care organizations: An interview study with physicians, registered nurses and assistant nurses. BMC Health Serv. Res. 2020, 20, 147. [Google Scholar] [CrossRef]
- Asaduzzaman, M.; Ara, R.; Afrin, S.; Meiring, J.E.; Saif-Ur-Rahman, K.M. Planetary Health Education and Capacity Building for Healthcare Professionals in a Global Context: Current Opportunities, Gaps and Future Directions. Int. J. Environ. Res. Public Health 2022, 19, 11786. [Google Scholar] [CrossRef]
- Dahlgren, A.; Tucker, P.; Epstein, M.; Gustavsson, P.; Söderström, M. Randomised control trial of a proactive intervention supporting recovery in relation to stress and irregular work hours: Effects on sleep, burn-out, fatigue and somatic symptoms. Occup. Environ. Med. 2022, 79, 460–468. [Google Scholar] [CrossRef]
- Sakzewski, L.; Naser-ud-Din, S. Work-related musculoskeletal disorders in dentists and orthodontists: A review of the literature. Work 2014, 48, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Țâncu, A.M.C.; Didilescu, A.C.; Pantea, M.; Sfeatcu, R.; Imre, M. Aspects regarding sustainability among private dental practitioners from Bucharest, Romania: A pilot study. Healthcare 2023, 11, 1326. [Google Scholar] [CrossRef] [PubMed]
- Mekhemar, M.; Attia, S.; Dörfer, C.; Conrad, J. The psychological impact of the COVID-19 pandemic on dentists in Germany. J. Clin. Med. 2021, 10, 1008. [Google Scholar] [CrossRef] [PubMed]
- Vered, Y.; Zaken, Y.; Ovadia-Gonen, H.; Mann, J.; Zini, A. Professional burnout: Its relevance and implications for the general dental community. Quintessence Int. 2014, 45, 87–90. [Google Scholar] [CrossRef]
- Plessas, A.; Paisi, M.; Bryce, M.; Burns, L.; O’Brien, T.; Hanoch, Y.; Witton, R. Mental health and wellbeing interventions in the dental sector: A systematic review. Evid. Based Dent. 2022, 7, 1–8. [Google Scholar] [CrossRef]
- Almeida, M.B.; Póvoa, R.; Tavares, D.; Alves, P.M.; Oliveira, R. Prevalence of musculoskeletal disorders among dental students: A systematic review and meta-analysis. Heliyon 2023, 9, e19956. [Google Scholar] [CrossRef]
- Carapeto, P.V.; Aguayo-Mazzucato, C. Effects of exercise on cellular and tissue aging. Aging 2021, 13, 14522–14543. [Google Scholar] [CrossRef]
- Scott, J.; Etain, B.; Miklowitz, D.; Crouse, J.J.; Carpenter, J.; Marwaha, S.; Smith, D.; Merikangas, K.; Hickie, I. A systematic review and meta-analysis of sleep and circadian rhythms disturbances in individuals at high-risk of developing or with early onset of bipolar disorders. Neurosci. Biobehav. Rev. 2022, 135, 104585. [Google Scholar] [CrossRef] [PubMed]
- McDonald, J.M.; Paganelli, C. Exploration of Mental Readiness for Enhancing Dentistry in an Inter-Professional Climate. Int. J. Environ. Res. Public Health 2021, 18, 7038. [Google Scholar] [CrossRef] [PubMed]
- Siddiqui, M.F.; Jabeen, S.; Alwazzan, A.; Vacca, S.; Dalal, L.; Al-Haddad, B.; Jaber, A.; Ballout, F.F.; Zeid, H.K.A.; Haydamous, J.; et al. Integration of Augmented Reality, Virtual Reality, and Extended Reality in Healthcare and Medical Education: A Glimpse into the Emerging Horizon in LMICs-A Systematic Review. J. Med. Educ. Curric. Dev. 2025, 12, 23821205251342315. [Google Scholar] [CrossRef] [PubMed]
- Schiavo, J.H. PROSPERO: An international register of systematic review protocols. Med. Ref. Serv. Q. 2019, 38, 171–180. [Google Scholar] [CrossRef]
- IBM Corp. IBM SPSS Statistics for Windows, Version 28.0; IBM Corp: Armonk, NY, USA, 2022; Available online: https://www.ibm.com/products/spss-statistics (accessed on 20 March 2025).
- Asaduzzaman, M.; Arbia, L.; Tasdika, T.; Mondol, A.; Ray, P.; Hossain, T.; Hossain, M. Assessing the awareness on occupational health hazards among dentists of different private dental clinics in Dhaka, Bangladesh. J. Biol. Agric. Healthc. 2022, 12, 18. [Google Scholar] [CrossRef]
- Al-Huthaifi, B.H.; Al Moaleem, M.M.; Alwadai, G.S.; Nassar, J.A.; Sahli, A.A.A.; Khawaji, A.H.; Juraybi, A.K.; Alsheri, Y.A.; Aldhorae, K.; Yaqoub, A.A.; et al. High prevalence of musculoskeletal disorders among dental professionals: A study on ergonomics and workload in Yemen. Med. Sci. Monit. 2023, 29, e942294. [Google Scholar] [CrossRef]
- Eminoğlu, D.Ö.; Kaşali, K.; Şeran, B.; Burmaoğlu, G.E.; Aydin, T.; Bircan, H.B. An assessment of musculoskeletal disorders and physical activity levels in dentists: A cross-sectional study. Work 2025, 80, 396–406. [Google Scholar] [CrossRef]
- Al-Emara, Z.; Karaharju-Suvanto, T.; Furu, P.; Furu, H. Musculoskeletal disorders and work ability among dentists and dental students in Finland. Work 2024, 78, 73–81. [Google Scholar] [CrossRef]
- Matur, Z.; Zengin, T.; Bolu, N.E.; Oge, A.E. Prevalence of carpal tunnel syndrome symptoms among young dentists. Cureus 2023, 15, e43358. [Google Scholar] [CrossRef]
- Macrì, M.; Flores, N.V.G.; Stefanelli, R.; Pegreffi, F.; Festa, F. Interpreting the prevalence of musculoskeletal pain impacting Italian and Peruvian dentists likewise: A cross-sectional study. Front. Public Health 2023, 11, 1090683. [Google Scholar] [CrossRef]
- Javed, H.R.; Tariq, H.T.; Lodhi, A.A.; Iftikhar, R.; Khanzada, S.K.; Arshad, K.; Sehar, H.; Fatima, K.; Rafique, H.; Aslam, I. Prevalence of carpel tunnel syndrome among dentists: A cross-sectional study. J. Health Rehabil. Res. 2023, 3, 384–388. [Google Scholar] [CrossRef]
- Chenna, D.; Pentapati, K.C.; Kumar, M.; Madi, M.; Siddiq, H. Prevalence of musculoskeletal disorders among dental healthcare providers: A systematic review and meta-analysis. F1000Research 2022, 11, 1062. [Google Scholar] [CrossRef] [PubMed]
- Alamri, A.; ElSharkawy, M.F.; Alafandi, D. Occupational Physical Hazards and Safety Practices at Dental Clinics. Eur. J. Dent. 2023, 17, 439–449. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Aldhaen, E. Awareness of occupational health hazards and occupational stress among dental care professionals: Evidence from the GCC region. Front. Public Health 2022, 10, 922748. [Google Scholar] [CrossRef]
- Zhou, Y.; Zhou, W.; Aisaiti, A.; Wang, B.; Zhang, J.; Svensson, P.; Wang, K. Dentists have a high occupational risk of neck disorders with impact on somatosensory function and neck mobility. J. Occup. Health 2021, 63, e12269. [Google Scholar] [CrossRef]
- Alnaser, M.Z.; Almaqsied, A.M.; Alshatti, S.A. Risk factors for work-related musculoskeletal disorders of dentists in Kuwait and the impact on health and economic status. Work 2021, 68, 213–221. [Google Scholar] [CrossRef]
- Berdouses, E.B.; Sifakaki, M.; Katsantoni, A.; Oulis, C.J. Work-related musculoskeletal disorders among Greek dentists: A nationwide survey. Dent. Res. Oral Health 2020, 4, 169–182. [Google Scholar] [CrossRef]
- Pavičin, I.S.; Lovrić, Ž.; Çeshko, A.Z.; Vodanović, M. Occupational injuries among dentists in Croatia. Acta Stomatol. Croat. 2020, 54, 51–59. [Google Scholar] [CrossRef]
- Alabdulwahab, S.; Kachanathu, S.; Alaulami, A. Health-related quality of life among dentists in Middle-East countries: A cross-sectional study. J. Indian Assoc. Public Health Dent. 2020, 18, 168. [Google Scholar] [CrossRef]
- Harris, M.L.; Sentner, S.M.; Doucette, H.J.; Brillant, M.G.S. Musculoskeletal disorders among dental hygienists in Canada. Can. J. Dent. Hyg. 2020, 54, 61–67. [Google Scholar]
- Ahmad, W.; Taggart, F.; Shafique, M.S.; Muzafar, Y.; Abidi, S.; Ghani, N.; Malik, Z.; Zahid, T.; Waqas, A.; Ghaffar, N. Diet, exercise and mental-wellbeing of healthcare professionals in Pakistan. PeerJ 2015, 3, e1250. [Google Scholar] [CrossRef]
- Memarpour, M.; Badakhsh, S.; Khosroshahi, S.S.; Vossoughi, M. Work-related musculoskeletal disorders among Iranian dentists. Work 2013, 45, 465–474. [Google Scholar] [CrossRef] [PubMed]
- Hashim, R.; Al-Ali, K. Health of dentists in United Arab Emirates. Int. Dent. J. 2013, 63, 26–29. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Purohit, B. Physical activity, sedentary lifestyle, and obesity among Indian dental professionals. J. Phys. Act. Health 2012, 9, 563–570. [Google Scholar] [CrossRef]
- Ellapen, T.J.; Narsigan, S.; van Herdeen, H.J.; Pillay, K.; Rugbeer, N. Impact of poor dental ergonomical practice. SADJ 2011, 66, 272–277. [Google Scholar] [PubMed]
- Sharma, P.; Golchha, V. Awareness among Indian dentists regarding the role of physical activity in prevention of work-related musculoskeletal disorders. Indian J. Dent. Res. 2011, 22, 381–384. [Google Scholar] [CrossRef]
- Kierklo, A.; Kobus, A.; Jaworska, M.; Botuliński, B. Work-related musculoskeletal disorders among dentists: A questionnaire survey. Ann. Agric. Environ. Med. 2011, 18, 79–84. [Google Scholar]
- Lietz, J.; Kozak, A.; Nienhaus, A. Prevalence and occupational risk factors of musculoskeletal diseases and pain among dental professionals in Western countries: A systematic literature review and meta-analysis. PLoS ONE 2018, 13, e0208628. [Google Scholar] [CrossRef]
- Alhusain, F.A.; Almohrij, M.; Althukeir, F.; Alshater, A.; Alghamdi, B.; Masuadi, E.; Basudan, A. Prevalence of carpal tunnel syndrome symptoms among dentists working in Riyadh. Ann. Saudi. Med. 2019, 39, 104–111. [Google Scholar] [CrossRef]
- Mehta, A.; Gupta, M.; Upadhyaya, N. Status of occupational hazards and their prevention among dental professionals in Chandigarh, India: A comprehensive questionnaire survey. Dent. Res. J. 2013, 10, 446–451. [Google Scholar]
- Bozkurt, S.; Demirsoy, N.; Günendi, Z. Risk factors associated with work-related musculoskeletal disorders in dentistry. Clin. Investig. Med. 2016, 39, 27527. [Google Scholar] [CrossRef]
- Feng, B.; Liang, Q.; Wang, Y.; Andersen, L.L.; Szeto, G. Prevalence of work-related musculoskeletal symptoms of the neck and upper extremity among dentists in China. BMJ Open 2014, 4, e006451. [Google Scholar] [CrossRef] [PubMed]
- Meyerson, J.; Gelkopf, M.; Eli, I.; Uziel, N. Burnout and professional quality of life among Israeli dentists: The role of sensory processing sensitivity. Int. Dent. J. 2020, 70, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Meyerson, J.; Gelkopf, M.; Eli, I.; Uziel, N. Stress coping strategies, burnout, secondary traumatic stress, and compassion satisfaction amongst Israeli dentists: A cross-sectional study. Int. Dent. J. 2022, 72, 476–483. [Google Scholar] [CrossRef] [PubMed]
- Singh, P.; Aulak, D.S.; Mangat, S.S.; Aulak, M.S. Systematic review: Factors contributing to burnout in dentistry. Occup. Med. 2016, 66, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Szalai, E.; Hallgató, J.; Kunovszki, P.; Tóth, Z. Burnout among Hungarian dentists. Orv. Hetil. 2021, 162, 419–424. [Google Scholar] [CrossRef]
- White, R.L.; Vella, S.; Biddle, S.; Sutcliffe, J.; Guagliano, J.M.; Uddin, R.; Burgin, A.; Apostolopoulos, M.; Nguyen, T.; Young, C.; et al. Physical activity and mental health: A systematic review and best-evidence synthesis of mediation and moderation studies. Int. J. Behav. Nutr. Phys. Act. 2024, 21, 134. [Google Scholar] [CrossRef]
- Horowitz, A.M.; Fan, X.; Bieri, G.; Smith, L.K.; Sanchez-Diaz, C.I.; Schroer, A.B.; Gontier, G.; Casaletto, K.B.; Kramer, J.H.; Williams, K.E.; et al. Blood factors transfer beneficial effects of exercise on neurogenesis and cognition to the aged brain. Science 2020, 369, 167–173. [Google Scholar] [CrossRef]
- Reddy, V.; Bennadi, D. Occupational hazards among dentists: A descriptive study. J. Oral Hyg. Health 2015, 3, 185. [Google Scholar] [CrossRef]
- Kızılcı, E.; Kızılay, F.; Mahyaddinova, T.; Muhtaroğlu, S.; Kolçakoğlu, K. Stress levels of a group of dentists while providing dental care under clinical, deep sedation, and general anesthesia. Clin. Oral Investig. 2023, 27, 3601–3609. [Google Scholar] [CrossRef]
- Neumann, R.J.; Ahrens, K.F.; Kollmann, B.; Goldbach, N.; Chmitorz, A.; Weichert, D.; Fiebach, C.J.; Wessa, M.; Kalisch, R.; Lieb, K.; et al. The impact of physical fitness on resilience to modern life stress and the mediating role of general self-efficacy. Eur. Arch. Psychiatry Clin. Neurosci. 2022, 272, 679–692. [Google Scholar] [CrossRef]
- Mulimani, P.; Hoe, V.C.W.; Hayes, M.J.; Idiculla, J.J.; Abas, A.B.L.; Karanth, L. Ergonomic interventions for preventing musculoskeletal disorders in dental care practitioners. Cochrane Database Syst. Rev. 2018, 10, CD011261. [Google Scholar] [CrossRef] [PubMed]
- Papagerakis, S.; Zheng, L.; Schnell, S.; Sartor, M.; Somers, E.; Marder, W.; McAlpin, B.; Kim, D.; McHugh, J.; Papagerakis, P. The circadian clock in oral health and diseases. J. Dent. Res. 2014, 93, 27–35. [Google Scholar] [CrossRef] [PubMed]
- de Grado, G.F.; Denni, J.; Musset, A.-M.; Offner, D. Back pain prevalence, intensity and associated factors in French dentists: A national study among 1004 professionals. Eur. Spine J. 2019, 28, 2510–2516. [Google Scholar] [CrossRef] [PubMed]
- Le, V.N.T.; Dang, M.-H.; Kim, J.-G.; Yang, Y.-M.; Lee, D.-W. Mental health in dentistry: A global perspective. Int. Dent. J. 2020, 71, 369–371. [Google Scholar] [CrossRef]
- Moro, J.D.S.; Soares, J.P.; Massignan, C.; Oliveira, L.B.; Ribeiro, D.M.; Cardoso, M.; Canto, G.D.L.; Bolan, M. Burnout syndrome among dentists: A systematic review and meta-analysis. J. Evid. Based Dent. Pract. 2022, 22, 101724. [Google Scholar] [CrossRef]
- Scheepers, R.A.; Emke, H.; Epstein, R.M.; Lombarts, K.M.J.M.H. The impact of mindfulness-based interventions on doctors’ well-being and performance: A systematic review. Med. Educ. 2020, 54, 138–149. [Google Scholar] [CrossRef]
- Lee, C.Y.; Wu, J.H.; Du, J.K. Work stress and occupational burnout among dental staff in a medical center. J. Dent. Sci. 2019, 14, 295–301. [Google Scholar] [CrossRef]
- World Health Organization. Global Oral Health Status Report: Towards Universal Health Coverage for Oral Health by 2030; WHO: Switzerland, Geneva, 2022; Available online: https://www.who.int/publications/i/item/9789240061484 (accessed on 20 March 2025).
- Alyousefy, M.A.; Shaiban, A.S.; Alaajam, W.H.; Bakri, M.M.H.; Alhazmi, Y.A.; Aljabri, M.Y.; Al Moaleem, M.M.; Al-Huthaifi, B.H.; Al-Bahr, H.F.; Alhaj, A.M. Questionnaire-based study on the prevalence, awareness, and preventive measures of occupational hazards among dental professionals. Med. Sci. Monit. 2022, 28, e938084. [Google Scholar] [CrossRef]
- Chen, X.; Yi, Z.; Wong, G.T.; Hasan, K.M.M.; Kwan, J.S.; Ma, A.C.; Chang, R.C. Is exercise a senolytic medicine? A systematic review. Aging Cell 2021, 20, e13294. [Google Scholar] [CrossRef]
- Zábó, V.; Lehoczki, A.; Fekete, M.; Szappanos, Á.; Varga, P.; Moizs, M.; Giovannetti, G.; Loscalzo, Y.; Giannini, M.; Polidori, M.C.; et al. The role of purpose in life in healthy aging: Implications for the Semmelweis Study and the Semmelweis-EUniWell Workplace Health Promotion Model Program. Geroscience 2025, 47, 2817–2833. [Google Scholar] [CrossRef]
- Saintila, J.; Javier-Aliaga, D.; Gálvez-Díaz, N.D.C.; Barreto-Espinoza, L.A.; Buenaño-Cervera, N.A.; Calizaya-Milla, Y.E. Association of sleep hygiene knowledge and physical activity with sleep quality in nursing and medical students: A cross-sectional study. Front. Sports Act. Living 2025, 7, 1453404. [Google Scholar] [CrossRef]
- Praditpapha, A.; Mattheos, N.; Pisarnturakit, P.P.; Pimkhaokham, A.; Subbalekha, K. Dentists′ Stress During the COVID-19 Pandemic: A Repeated Cross-Sectional Study. Int. Dent. J. 2023, 74, 294–302. [Google Scholar] [CrossRef] [PubMed]
- Cano, Y.M.Y.; Dávila-Ruiz, D.; Cuilty-Esquivel, K. Burnout resilience in the face of the COVID-19 pandemic. TEC Empres. 2025, 19, 36–50. [Google Scholar] [CrossRef]
- Negucioiu, M.; Buduru, S.; Ghiz, S.; Kui, A.; Șoicu, S.; Buduru, R.; Sava, S. Prevalence and Management of Burnout Among Dental Professionals Before, During, and After the COVID-19 Pandemic: A Systematic Review. Healthcare 2024, 12, 2366. [Google Scholar] [CrossRef] [PubMed]
- Adsett, J.A.; Mudge, A.M. Interventions to Promote Physical Activity and Reduce Functional Decline in Medical Inpatients: An Umbrella Review. J. Am. Med. Dir. Assoc. 2024, 25, 105052. [Google Scholar] [CrossRef]
- Gallagher, J.; Colonio-Salazar, F.; White, S. Supporting dentists’ health and wellbeing: A qualitative study of coping strategies in ’normal times′. Br. Dent. J. 2021. [Google Scholar] [CrossRef]
- Sezer, B.; Sıddıkoğlu, D. Relationship between work-related musculoskeletal symptoms and burnout symptoms among preclinical and clinical dental students: A cross-sectional study. BMC Musculoskelet. Disord. 2025, 26, 561. [Google Scholar] [CrossRef]
- Antoniadou, M. Leadership and Managerial Skills in Dentistry: Characteristics and Challenges Based on a Preliminary Case Study. Dent. J. 2022, 10, 146. [Google Scholar] [CrossRef]
- Karami, M.; Drouri, S.; Al Jalil, Z.; Ettaki, S.; Jabri, M. Musculoskeletal disorders and stress among Moroccan dentists: A cross-sectional study. Integr. J. Med. Sci. 2023, 10, 15342. [Google Scholar] [CrossRef]
- Caron, R.M.; Noel, K.; Reed, R.N.; Sibel, J.; Smith, H.J. Health Promotion, Health Protection, and Disease Prevention: Challenges and Opportunities in a Dynamic Landscape. AJPM Focus 2023, 3, 100167. [Google Scholar] [CrossRef]
- Lu, X.; Chen, Y.; Shi, Y.; Su, X.; Chen, P.; Wu, D.; Shi, H. Exercise and exerkines: Mechanisms and roles in anti-aging and disease prevention. Exp. Gerontol. 2025, 200, 112685. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Huang, X.; Dou, L.; Yan, M.; Shen, T.; Tang, W.; Li, J. Aging and aging-related diseases: From molecular mechanisms to interventions and treatments. Sig. Transduct. Target. Ther. 2022, 7, 391. [Google Scholar] [CrossRef] [PubMed]
- Gao, G.; Xie, Z.; Huang, H. Mitochondrial function maintenance and mitochondrial training in ageing and related diseases. J. Holist. Integr. Pharm. 2025, 6, 159–174. [Google Scholar] [CrossRef]
- Małkowska, P. Positive Effects of Physical Activity on Insulin Signaling. Curr. Issues Mol. Biol. 2024, 46, 5467–5487. [Google Scholar] [CrossRef]
- Almuraikhy, S.; Sellami, M.; Al-Amri, H.S.; Domling, A.; Althani, A.A.; Elrayess, M.A. Impact of Moderate Physical Activity on Inflammatory Markers and Telomere Length in Sedentary and Moderately Active Individuals with Varied Insulin Sensitivity. J. Inflamm. Res. 2023, 16, 5427–5438. [Google Scholar] [CrossRef]
- Erickson, K.I.; Hillman, C.; Stillman, C.M.; Ballard, R.M.; Bloodgood, B.; Conroy, D.E.; Macko, R.; Marquez, D.X.; Petruzzello, S.J.; Powell, K.E.; et al. For 2018 physical activity guidelines advisory commitee. Physical Activity, Cognition, and Brain Outcomes: A Review of the 2018 Physical Activity Guidelines. Med. Sci. Sports Exerc. 2019, 51, 1242–1251. [Google Scholar] [CrossRef]
- Dhahbi, W.; Briki, W.; Heissel, A.; Schega, L.; Dergaa, I.; Guelmami, N.; EL Omri, A.; Chaabene, H. Physical Activity to Counter Age-Related Cognitive Decline: Benefits of Aerobic, Resistance, and Combined Training—A Narrative Review. Sports Med. Open 2025, 11, 56. [Google Scholar] [CrossRef]
- Pontes, C.C.; Stanley, K.; Molayem, S. Understanding the Dental Profession’s Stress Burden: Prevalence and Implications. Compend. Contin. Educ. Dent. 2024, 45, 236–241. [Google Scholar]
- Gkintoni, E.; Vassilopoulos, S.P.; Nikolaou, G.; Boutsinas, B. Digital and AI-Enhanced Cognitive Behavioral Therapy for Insomnia: Neurocognitive Mechanisms and Clinical Outcomes. J. Clin. Med. 2025, 14, 2265. [Google Scholar] [CrossRef]
- Kim, N.; Ka, S.; Park, J. Effects of exercise timing and intensity on physiological circadian rhythm and sleep quality: A systematic review. Phys. Act. Nutr. 2023, 27, 52–63. [Google Scholar] [CrossRef]
- Woo, D.; Shafiee, R.; Manton, J.W.; Huang, J.; Fa, B.A. Self-care and wellness in dentistry—A mini review. J. Oral Maxillofac. Anesth. 2024, 3, 5. [Google Scholar] [CrossRef]
- Harris, M.; Eaton, K. Exploring dental professionals′ perceptions of resilience to dental environment stress: A qualitative study. Br. Dent. J. 2025, 238, 395–402. [Google Scholar] [CrossRef]
- McColl, E.; Paisi, M.; Plessas, A.; Ellwood, F.; Witton, R. An individual-level approach to stress management in dentistry. BDJ Team 2022, 9, 6–13. [Google Scholar] [CrossRef]
- de Lisser, R.; Dietrich, M.S.; Spetz, J.; Ramanujam, R.; Lauderdale, J.; Stolldorf, D.P. Psychological safety is associated with better work environment and lower levels of clinician burnout. Health Aff. Sch. 2024, 2, qxae091. [Google Scholar] [CrossRef] [PubMed]
- Teisberg, E.; Wallace, S.; O′Hara, S. Defining and Implementing Value-Based Health Care: A Strategic Framework. Acad. Med. 2020, 95, 682–685. [Google Scholar] [CrossRef]
- Cillekens, B.; Huysmans, M.A.; Holtermann, A.; van Mechelen, W.; Straker, L.; Krause, N.; van der Beek, A.J.; Coenen, P. Physical activity at work may not be health enhancing. A systematic review with meta-analysis on the association between occupational physical activity and cardiovascular disease mortality covering 23 studies with 655 892 participants. Scand J. Work Environ. Health 2022, 48, 86–98, Erratum in Scand J. Work Environ. Health 2023, 49, 231–244. [Google Scholar] [CrossRef]
- Marklund, S.; Mienna, C.S.; Wahlström, J.; Englund, E.; Wiesinger, B. Work ability and productivity among dentists: Associations with musculoskeletal pain, stress, and sleep. Int. Arch. Occup. Environ. Health 2020, 93, 271–278. [Google Scholar] [CrossRef]
- Isper Garbin, A.J.; Soares, G.B.; Arcieri, R.M.; Saliba Garbin, C.A.; Siqueira, C.E. Musculoskeletal disorders and perception of working conditions: A survey of Brazilian dentists in São Paulo. Int. J. Occup. Med. Environ. Health 2017, 30, 367–377. [Google Scholar] [CrossRef]
- Safi, A.; Cole, M.; Kelly, A.L.; Zariwala, M.G.; Walker, N.C. Workplace Physical Activity Barriers and Facilitators: A Qualitative Study Based on Employees Physical Activity Levels. Int. J. Environ. Res. Public Health 2022, 19, 9442. [Google Scholar] [CrossRef]
- Huttunen, M.; Kämppi, A.; Soudunsaari, A.; Päkkilä, J.; Tjäderhane, L.; Laitala, M.-L.; Anttonen, V.; Patinen, P.; Tanner, T. The association between dental caries and physical activity, physical fitness, and background factors among Finnish male conscripts. Odontology 2023, 111, 192–200. [Google Scholar] [CrossRef]
- Calvo, J.M.; Kwatra, J.; Yansane, A.; Tokede, O.; Gorter, R.C.; Kalenderian, E. Burnout and work engagement among US dentists. J. Patient Saf. 2021, 17, 398–404. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Boussuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Aki, E.A.; Brennan, S.A.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
| No | Authors, Country, Year | Study Design | Sample and Population | Setting | Outcomes and Key Findings |
|---|---|---|---|---|---|
| 1 | Eminoğlu et al., Turkey, 2025 [38] | Cross-sectional | 234 dentists | Clinical | Dentists reporting regular PA had significantly lower prevalence and intensity of MSDs, particularly neck and back, compared to sedentary peers. |
| 2 | Sezer & Sıddıkoğlu, Turkey, 2025 [30] | Cross-sectional | 298 dental students | Academic | Clinical students had higher WMS and burnout than preclinical students, linked to workload, long clinical hours, and poor posture. |
| 3 | Al-Emara et al., Finland, 2024 [39] | Cross-sectional | 255 dentists | Clinical | MSDs associated with reduced work ability, higher absenteeism and lower productivity; exercise and loupes partially mitigated effects. |
| 4 | Azimi et al., Afghanistan, 2024 [4] | Cross-sectional | 206 dentists | Clinical | High fatigue, stress, and back pain; regular PA reduced both physical and psychological symptoms. |
| 5 | Matur et al., Turkey, 2023 [40] | Case–control | 74 dentists and 61 office staff | Clinical | Dentists had higher CTS symptoms than office staff; risk linked to repetitive hand motions and static postures. |
| 6 | Al-Huthaifi et al., Yemen, 2023 [37] | Cross-sectional | 150 dentists | Clinical | Poor ergonomic knowledge and high workload contributed to elevated MSDs, especially shoulders and lower back. |
| 7 | Macrì et al., Italy and Peru, 2023 [41] | Cross-sectional | 700 dentists | Clinical | Similar MSD patterns in both countries; neck and back pain most common; cultural/systemic factors influenced severity. |
| 8 | Javed et al., Pakistan, 2023 [42] | Cross-sectional | 190 dentists | Clinical | Female dentists reported higher CTS symptoms, mental distress and lower PA than males; mental health support inadequate. |
| 9 | Almeida et al., Portugal, 2023 [29] | Systematic review | 19 studies (students) | -- | Review: dental students had high MSD prevalence, especially cervical and lumbar, often beginning in training; posture and stress were key. |
| 10 | Chenna et al., India, 2022 [43] | Systematic review | 21 studies | -- | Meta-analysis: global MSD prevalence among dentists 64–93%; neck, shoulders and back most affected; PA and ergonomics recommended. |
| 11 | Daou et al., Lebanon, 2022 [44] | Experimental | 300 dentists | Clinical | High MSD prevalence due to long hours and poor ergonomics; dentists recommended better training and equipment. |
| 12 | Asaduzzaman et al., Bangladesh, 2022 [36] | Cross-sectional | 170 dentists | Clinical | Senior dentists reported higher MSDs and more ergonomic strain than juniors, suggesting cumulative exposure effects. |
| 13 | AlDhae, Bahrain, 2022 [45] | Cross-sectional | 320 dentists | Clinical | High occupational stress and low PA rates; poor awareness of ergonomic practices contributed to widespread MSD complaints. |
| 14 | Zhou et al., China, 2021 [46] | Cross-sectional | 200 dentists and office workers | Hospital | Dentists had higher neck pain intensity and reduced pain thresholds than office workers, due to static postures and precision tasks. |
| 15 | Gandolfi et al., Italy, 2021 [10] | Cross-sectional | 310 dentists | Clinical | MSD prevalence higher in women and experienced dentists; PA protective against symptoms. |
| 16 | Alnaser et al., Kuwait, 2021 [47] | Cross-sectional | 250 dentists | Clinical | High workload, poor posture and insufficient breaks were main predictors of MSDs; absenteeism had economic impact. |
| 17 | Berdouses et al., Greece, 2020 [48] | Cross-sectional | 300 dentists | Clinical | Over 50% of dentists reported MSDs, especially lower back and shoulders; poor posture and dental noise contributed. |
| 18 | Pavičin et al., Croatia, 2020 [49] | Cross-sectional | 350 dentists | Clinical | High injury rates (needlestick, back strain, eye injury) among dentists, linked to posture, noise and stress. |
| 19 | AlAbdulwahab et al., Saudi Arabia, 2020 [50] | Cross-sectional | 290 dentists | Clinical | Sedentary behavior linked to MSDs and obesity; lack of PA worsened quality of life. |
| 20 | Harris et al., Canada, 2020 [51] | Cross-sectional | 500 dental hygienists | Clinical | 83% of hygienists experienced ≥ 1 MSD; symptoms worsened with years of practice; CTS and tendinitis most common. |
| 21 | Miron et al., Romania, 2018 [7] | Cross-sectional | 180 dentists | Clinical | High psychological stress and unhealthy coping (e.g., smoking); PA associated with better emotional resilience. |
| 22 | Ahmad et al., Pakistan, 2015 [52] | Cross-sectional | 150 dentists | Clinical | Female dentists reported lower PA and more mental health complaints than male colleagues. |
| 23 | Memarpour et al., Iran and UAE, 2013 [53] | Cross-sectional | 210 dentists | Clinical | High burnout and stress among dentists; PA, rest breaks and improved ergonomics reduced complaints. |
| 24 | Hashim & Al-Ali, Dubai and UAE, 2013 [54] | Cross-sectional | 200 dentists | Clinical | Low PA, poor diet and high smoking prevalence associated with systemic health problems and MSDs. |
| 25 | Singh & Purohit, India, 2012 [55] | Cross-sectional | 150 dentists and students | Academic | Students and interns had higher PA and fewer MSDs than senior faculty; lifestyle and hierarchy influenced outcomes. |
| 26 | Ellapen et al., South Africa, 2011 [56] | Retrospective | 94 dentists | Clinical | Widespread back, neck and shoulder pain attributed to poor ergonomics, high patient loads and lack of recovery. |
| 27 | Sharma & Golchha, India, 2011 [57] | Cross-sectional-Questionnaire | 102 dentists | Clinical | Awareness of PA benefits linked to fewer MSD symptoms and better prevention practices. |
| 28 | Kierklo et al., Poland, 2011 [58] | Cross-sectional-Questionnaire | 220 dentists | Clinical | >80% of dentists reported MSDs, especially neck and back; years of practice and lack of breaks correlated with severity. |
| Sensitivity Condition | Impact on Findings | Effect Description |
|---|---|---|
| Exclusion of small sample studies (<100 participants) | Low to moderate | Trends remain consistent, with minor statistical shifts |
| Inclusion of studies with standardized MSD diagnostics only | Minimal | Findings confirm reliability across consistent diagnostics |
| Exclusion of studies from LMICs | Moderate to high | Contextual insights reduced, skew toward high-income settings |
| Inclusion of studies specifying sector (public/private) | Significant (data reduction) | Weaker conclusions due to limited data |
| Inclusion of studies published after 2020 only | Shift in thematic focus (less emphasis on MSDs) | More focus on mental health; traditional MSD patterns diluted |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kalogerakou, T.; Antoniadou, M. Enhancing Dentists’ Resilience and Occupational Sustainability Through Physical Activity: A Systematic Review in the Post-Pandemic Context. Healthcare 2025, 13, 1985. https://doi.org/10.3390/healthcare13161985
Kalogerakou T, Antoniadou M. Enhancing Dentists’ Resilience and Occupational Sustainability Through Physical Activity: A Systematic Review in the Post-Pandemic Context. Healthcare. 2025; 13(16):1985. https://doi.org/10.3390/healthcare13161985
Chicago/Turabian StyleKalogerakou, Theodora, and Maria Antoniadou. 2025. "Enhancing Dentists’ Resilience and Occupational Sustainability Through Physical Activity: A Systematic Review in the Post-Pandemic Context" Healthcare 13, no. 16: 1985. https://doi.org/10.3390/healthcare13161985
APA StyleKalogerakou, T., & Antoniadou, M. (2025). Enhancing Dentists’ Resilience and Occupational Sustainability Through Physical Activity: A Systematic Review in the Post-Pandemic Context. Healthcare, 13(16), 1985. https://doi.org/10.3390/healthcare13161985


_MD__MPH_PhD.png)




