Treatment Delay and Type of Retraction Affect the Surgical Treatment of Distal Biceps Tendon Ruptures: A Quantitative Analysis of 123 Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Surgical Technique Note
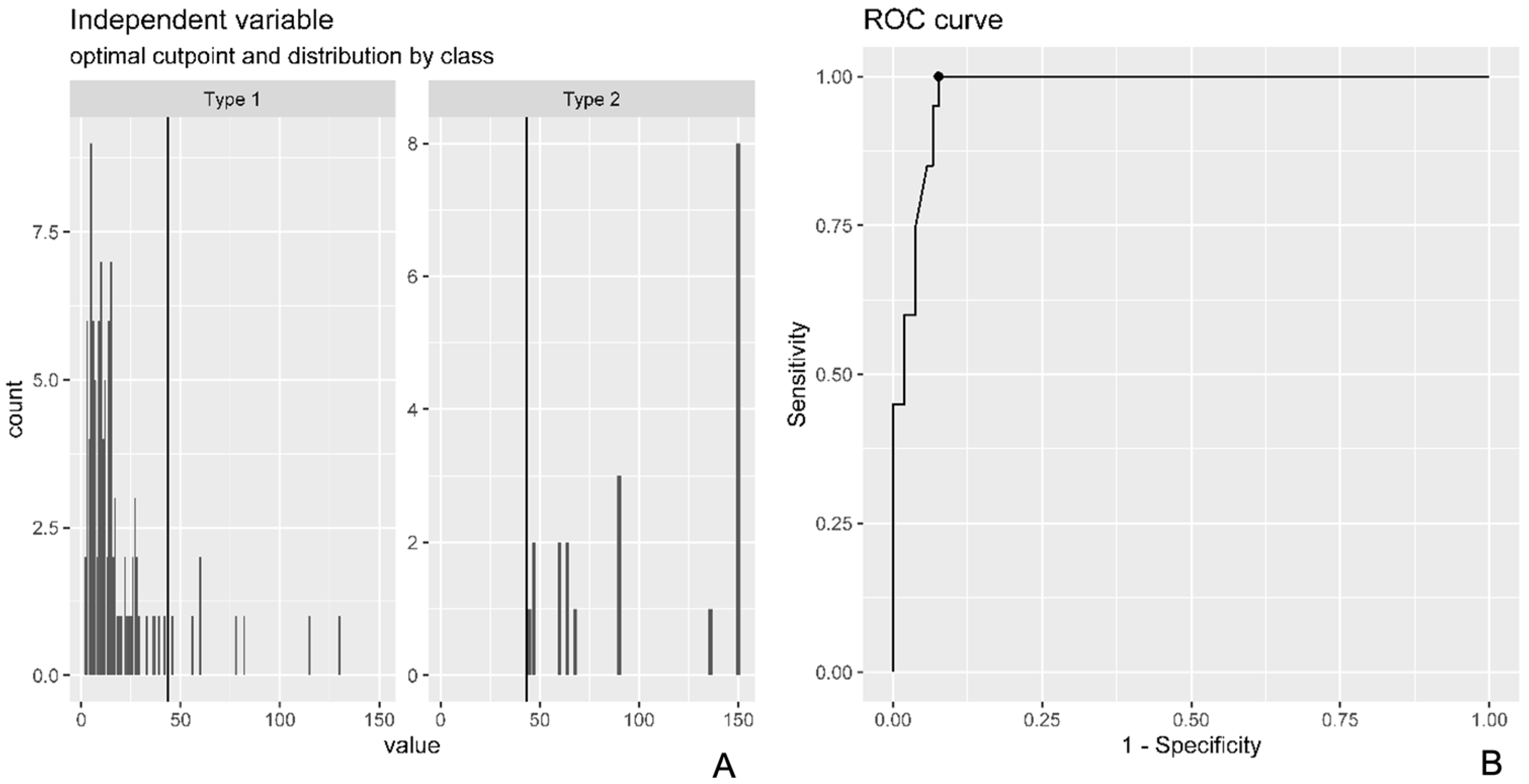
2.2. Statistical Analysis
2.3. Literature Review
3. Results
Literature Review Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kelly, M.P.; Perkinson, S.G.; Ablove, R.H.; Tueting, J.L. Distal Biceps Tendon Ruptures: An Epidemiological Analysis Using a Large Population Database. Am. J. Sports Med. 2015, 43, 2012–2017. [Google Scholar] [CrossRef]
- Freeman, C.R.; McCormick, K.R.; Mahoney, D.; Baratz, M.; Lubahn, J.D. Nonoperative treatment of distal biceps tendon ruptures compared with a historical control group. J. Bone Joint Surg. Am. 2009, 91, 2329–2334. [Google Scholar] [CrossRef]
- Morrey, B.F.; Askew, L.J.; An, K.N.; Dobyns, J.H. Rupture of the distal tendon of the biceps brachii. A biomechanical study. J. Bone Joint Surg. Am. 1985, 67, 418–421. [Google Scholar] [CrossRef]
- Cross, M.B.; Egidy, C.C.; Wu, R.H.; Osbahr, D.C.; Nam, D.; Dines, J.S. Single-incision chronic distal biceps tendon repair with tibialis anterior allograft. Int. Orthop. 2014, 38, 791–795. [Google Scholar] [CrossRef]
- Darlis, N.A.; Sotereanos, D.G. Distal biceps tendon reconstruction in chronic ruptures. J. Shoulder Elbow Surg. 2006, 15, 614–619. [Google Scholar] [CrossRef]
- Dillon, M.T.; Bollier, M.J.; King, J.C. Repair of acute and chronic distal biceps tendon ruptures using the EndoButton. Hand 2011, 6, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Frank, T.; Seltser, A.; Grewal, R.; King, G.J.W.; Athwal, G.S. Management of chronic distal biceps tendon ruptures: Primary repair vs. semitendinosus autograft reconstruction. J. Shoulder Elbow Surg. 2019, 28, 1104–1110. [Google Scholar] [CrossRef] [PubMed]
- Giacalone, F.; Dutto, E.; Ferrero, M.; Bertolini, M.; Sard, A.; Pontini, I. Treatment of distal biceps tendon rupture: Why, when, how? Analysis of literature and our experience. Musculoskelet. Surg. 2015, 99 (Suppl. S1), S67–S73. [Google Scholar] [CrossRef]
- Goyal, N.; Wilson, D.J.; Salzano, M.B.; Fernandez, J.J.; Cohen, M.S.; Wysocki, R.W. Restoration of peak strength and endurance following distal biceps reconstruction with allograft for chronic ruptures. J. Shoulder Elbow Surg. 2020, 29, 853–858. [Google Scholar] [CrossRef]
- Hallam, P.; Bain, G.I. Repair of chronic distal biceps tendon ruptures using autologous hamstring graft and the Endobutton. J. Shoulder Elbow Surg. 2004, 13, 648–651. [Google Scholar] [CrossRef] [PubMed]
- Haverstock, J.; Grewal, R.; King, G.J.W.; Athwal, G.S. Delayed repair of distal biceps tendon ruptures is successful: A case-control study. J. Shoulder Elbow Surg. 2017, 26, 1031–1036. [Google Scholar] [CrossRef]
- Hendy, B.A.; Padegimas, E.M.; Harper, T.; Lazarus, M.D.; Abboud, J.A.; Namdari, S. Outcomes of chronic distal biceps reconstruction with tendon grafting: A matched comparison with primary repair. JSES Int. 2020, 5, 302–306. [Google Scholar] [CrossRef]
- Morrell, N.T.; Mercer, D.M.; Moneim, M.S. Late reconstruction of chronic distal biceps tendon ruptures using fascia lata autograft and suture anchor fixation. Tech. Hand Up. Extrem. Surg. 2012, 16, 141–144. [Google Scholar] [CrossRef]
- Phadnis, J.; Flannery, O.; Watts, A.C. Distal biceps reconstruction using an Achilles tendon allograft, transosseous EndoButton, and Pulvertaft weave with tendon wrap technique for retracted, irreparable distal biceps ruptures. J. Shoulder Elbow Surg. 2016, 25, 1013–1019. [Google Scholar] [CrossRef]
- Samra, I.; Mati, W.; Blundell, C.; Lane, S.; Charalambous, C.P. Distal biceps tendon ruptures—The relation of radiological retraction and chronicity to the ability of tendon reattachment and long-term functional outcomes. J. Orthop. 2019, 20, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, G.J.; Dmochowski, J.M.; Gudeman, A.S.; Cage, E.S.; Greenberg, J.A.; Hoyer, R.W. Primary Repair of Chronic Distal Biceps Tendon Tears. HAND 2024, 19, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Snir, N.; Hamula, M.; Wolfson, T.; Meislin, R.; Strauss, E.J.; Jazrawi, L.M. Clinical outcomes after chronic distal biceps reconstruction with allografts. Am. J. Sports Med. 2013, 41, 2288–2295. [Google Scholar] [CrossRef] [PubMed]
- Wiley, W.B.; Noble, J.S.; Dulaney, T.D.; Bell, R.H.; Noble, D.D. Late reconstruction of chronic distal biceps tendon ruptures with a semitendinosus autograft technique. J. Shoulder Elbow Surg. 2006, 15, 440–444. [Google Scholar] [CrossRef]
- Zeman, C.A.; Mueller, J.D.; Sanderson, B.R.; Gluck, J.S. Chronic distal biceps avulsion treated with suture button. J. Shoulder Elbow Surg. 2020, 29, 1548–1553. [Google Scholar] [CrossRef]
- Cain, R.A.; Nydick, J.A.; Stein, M.I.; Williams, B.D.; Polikandriotis, J.A.; Hess, A.V. Complications following distal biceps repair. J. Hand Surg. Am. 2012, 37, 2112–2117. [Google Scholar] [CrossRef]
- Caputo, A.E.; Cusano, A.; Stannard, J.; Hamer, M.J. Distal biceps repair using the lacertus fibrosus as a local graft. J. Shoulder Elbow Surg. 2016, 25, 1189–1194. [Google Scholar] [CrossRef]
- Kelly, E.W.; Morrey, B.F.; O’Driscoll, S.W. Complications of repair of the distal biceps tendon with the modified two-incision technique. J. Bone Joint Surg. Am. 2000, 82, 1575–1581. [Google Scholar] [CrossRef] [PubMed]
- Luokkala, T.; Siddharthan, S.K.; Karjalainen, T.V.; Watts, A.C. Distal biceps hook test—Sensitivity in acute and chronic tears and ability to predict the need for graft reconstruction. Shoulder Elbow. 2020, 12, 294–298. [Google Scholar] [CrossRef]
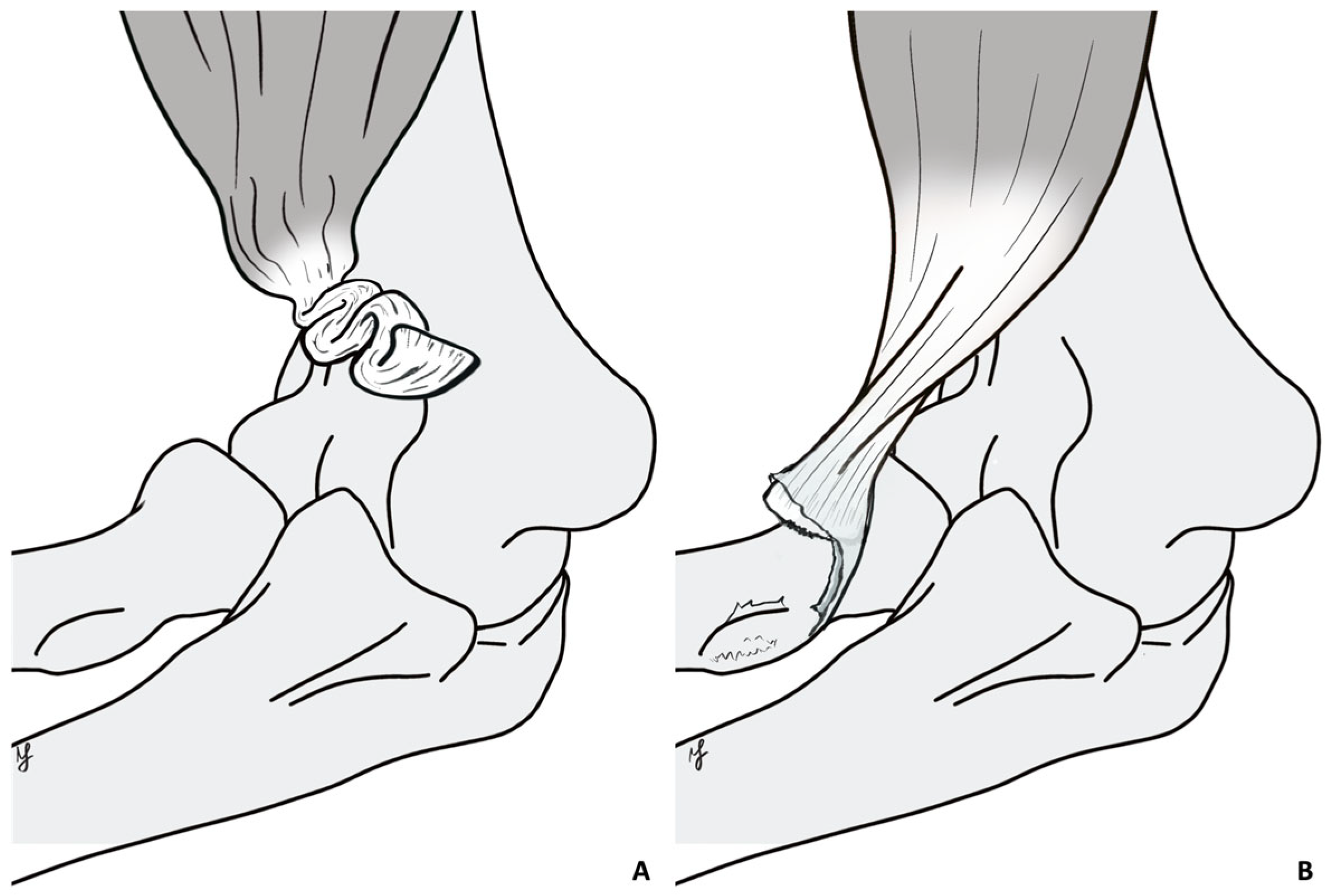
- Boonrod, A.; Harasymczuk, M.; Ramazanian, T.; Boonrod, A.; Smith, J.; O’Driscoll, S.W. The Turtle Neck Sign: Identification of Severe Retracted Distal Biceps Tendon Rupture. Orthop. J. Sports Med. 2022, 10, 23259671211065030. [Google Scholar] [CrossRef]
- Rantanen, J.; Orava, S. Rupture of the distal biceps tendon. A report of 19 patients treated with anatomic reinsertion, and a meta-analysis of 147 cases found in the literature. Am. J. Sports Med. 1999, 27, 128–132. [Google Scholar] [CrossRef]
- Maffulli, N.; Via, A.G.; Oliva, F. Chronic Achilles Tendon Rupture. Open Orthop. J. 2017, 11, 660–669. [Google Scholar] [CrossRef]
- Morrey, M.E.; Abdel, M.P.; Sanchez-Sotelo, J.; Morrey, B.F. Primary repair of retracted distal biceps tendon ruptures in extreme flexion. J. Shoulder Elbow Surg. 2014, 23, 679–685. [Google Scholar] [CrossRef]
- Woods, D.A.; Hoy, G.; Shimmin, A. A safe technique for distal biceps repair using a suture anchor and a limited anterior approach. Injury. 1999, 30, 233–237. [Google Scholar] [CrossRef] [PubMed]
- Legg, A.J.; Stevens, R.; Oakes, N.O.; Shahane, S.A. A comparison of nonoperative vs. Endobutton repair of distal biceps ruptures. J. Shoulder Elbow Surg. 2016, 25, 341–348. [Google Scholar] [CrossRef]
- Anakwenze, O.A.; Baldwin, K.; Abboud, J.A. Distal biceps tendon repair: An analysis of timing of surgery on outcomes. J. Athl. Train. 2013, 48, 9–11. [Google Scholar] [CrossRef] [PubMed]
- Bosman, H.A.; Fincher, M.; Saw, N. Anatomic direct repair of chronic distal biceps brachii tendon rupture without interposition graft. J. Shoulder Elbow Surg. 2012, 21, 1342–1347. [Google Scholar] [CrossRef] [PubMed]
- Butler, K.; Almigdad, A.; Kim, J.; Dodson, E.; Malhas, A. Outcomes of distal biceps repair at two-year follow-up. Eur. J. Orthop. Surg. Traumatol. 2024, 34, 989–993. [Google Scholar] [CrossRef]
- Ford, S.E.; Andersen, J.S.; Macknet, D.M.; Connor, P.M.; Loeffler, B.J.; Gaston, R.G. Major complications after distal biceps tendon repairs: Retrospective cohort analysis of 970 cases. J. Shoulder Elbow Surg. 2018, 27, 1898–1906. [Google Scholar] [CrossRef]
- Jain, S.; Patkar, H.; Mohan, R. Is the Complication Rate in the Surgical Repair of the Distal Biceps Tendon Rupture Influenced by the Timing, Type of Incision and Method of Fixation? Indian J. Orthop. 2023, 58, 79–88. [Google Scholar] [CrossRef]
- Khan, A.D.; Penna, S.; Yin, Q.; Sinopidis, C.; Brownson, P.; Frostick, S.P. Repair of distal biceps tendon ruptures using suture anchors through a single anterior incision. Arthroscopy 2008, 24, 39–45. [Google Scholar] [CrossRef]
- McKee, M.D.; Hirji, R.; Schemitsch, E.H.; Wild, L.M.; Waddell, J.P. Patient-oriented functional outcome after repair of distal biceps tendon ruptures using a single-incision technique. J. Shoulder Elbow Surg. 2005, 14, 302–306. [Google Scholar] [CrossRef] [PubMed]
- Reichert, P.; Królikowska, A.; Kentel, M.; Witkowski, J.; Gnus, J.; Satora, W.; Czamara, A. A comparative clinical and functional assessment of cortical button versus suture anchor in distal biceps brachii tendon repair. J. Orthop. Sci. 2019, 24, 103–108. [Google Scholar] [CrossRef] [PubMed]
- Austin, L.; Pepe, M.; VanBeek, C.; Tjoumakaris, F. Distal biceps rupture: The coil sign. Orthopedics 2014, 37, e605-7. [Google Scholar] [CrossRef]

| Variable (Range) | Whole Sample (n = 123) | Group I (n = 75) | Group II (n = 20) | Group III (n = 28) | p= |
|---|---|---|---|---|---|
| Age (range) | 46 (29–64) | 46.4 (31–63) | 44.4 (34–62) | 46.4 (29–64) | 0.59 |
| Sex | 0.53 | ||||
| M | 121 | 74 | 20 | 27 | |
| F | 2 | 1 | 0 | 1 | |
| Tt-Ts—days (range) | 53.9 (2–1095) | 9.5 (2–20) | 29.4 (22–42) | 196 (45–1095) | 0.001 I vs. II p = 0.7 I vs. III p = 0.001 II vs. III p = 0.001 |
| PR (n) | 101 | 75 | 18 | 8 | 0.001 |
| RG (n) | 22 | 0 | 2 | 20 |
| Groups | |||
|---|---|---|---|
| Variables | PR (n = 101) | RG (n = 22) | p= |
| Age (range) | 45.71 (31–62) | 48 (29–64) | 0.24 |
| Sex | 100 M; 1 F | 21 M; 1 F | 0.5 |
| Side | R 58; L 43 | R 13; L 9 | 0.88 |
| Arm dominance | 58 | 11 | 0.52 |
| Tt-Ts (range) | 18.16 | 224.5 (36–1095) | 0.001 |
| Variable | Whole Sample (n = 123) | Group I (n = 75) | Group II (n = 20) | Group III (n = 28) | p= | PR (n = 101) | RG (n = 22) | p= |
|---|---|---|---|---|---|---|---|---|
| Strength in flexion (range) | 4.9 (4–5) | 5 (5–5) | 5 (5–5) | 4,9 (4–5) | 0.005 I vs. II p = 0.1 I vs. III p = 0.004 II vs. III p = 0.04 | 4,98 (4–5) | 4,95 (4–5) | 0.48 |
| Strength in supination (range) | 4.9 (4–5) | 5 (5–5) | 4,9 (4–5) | 4.86 (4–5) | 0.001 I vs. II p = 0.17 I vs. III p = 0.001 II vs. III p = 0.45 | 4.97 (4–5) | 4.8 (4–5) | 0.005 |
| ROM E° (range) | 0° (0–10°) | 0° (0–10°) | 1° (0–10°) | 1° (0–10°) | 0.002 I vs. II p = 0.005 I vs. III p = 0.03 II vs. III p = 0.7 | 0.35° (0–10°) | 1.136° (0–10°) | 0.08 |
| ROM F° (range) | 136° (120–160°) | 137° (120–160°) | 136° (120–150°) | 135° (120–145°) | 0.5 | 136.7° (120–160°) | 135.9° (130–140°) | 0.71 |
| ROM P° (range) | 83° (30–90°) | 85° (30–90°) | 81° (70–90°) | 82° (50–90°) | 0.09 | 83.7° (60–90) | 83.18° (70–90°) | 0.8 |
| ROM S° (range) | 83° (0–90°) | 85° (0–90°) | 79° (60–90°) | 82° (60–90°) | 0.054 | 83.44° (60–90°) | 83.4° (70–90°) | 0.98 |
| MEPS (range) | 97 (70–100) | 98 (85–100) | 96 (85–100) | 95 (70–100) | 0.03 I vs. II p = 0.4 I vs. III p = 0.02 II vs. III p = 0.62 | 97.33 (70–100) | 96.59 (85–100) | 0.58 |
| DASH (range) | 1.25 (0–50.8) | 1.0 (0–50.8) | 0.3 (0–7.5) | 2.15 (0–10) | 0.92 | 1.13 (0–50.8) | 1.33 (0–6.7) | 0.92 |
| (A) Complications by treatment timing group | ||||
| Group | HO | LACN Paresthesia | Superficial Wound Infections | Total Complications |
| Acute | 3 | 4 | 0 | 7 |
| Subacute | 0 | 2 | 2 | 4 |
| Chronic | 0 | 3 | 0 | 3 |
| Total | 3 | 9 | 2 | 14 |
| (B) Complications by surgical technique | ||||
| Surgical Technique | HO | LACN Paresthesia | Superficial Wound Infections | Total Complications |
| Primary repair (PR) | 3 | 8 | 2 | 13 |
| Reconstruction with graft (RG) | 0 | 1 | 0 | 1 |
| Total | 3 | 9 | 2 | 14 |
| Article | Patients N° | PR vs. RG | Tt-Ts PR Mean (Range) | Tt-Ts RG Mean (Range) |
|---|---|---|---|---|
| Anakawaze et al., 2018 [30] | 18 | PR | 33 (9–75) | - |
| Bosman et al., 2012 [31] | 6 | PR | 78 (35–116) | - |
| Butler et al., 2023 [32] | 45 | PR | 20 (6–84) | - |
| Caputo et al., 2016 [21] | 12 | RG | - | 106 (14–617) |
| Cross et al., 2013 [4] | 7 | RG | - | 175 (84–392) |
| Darlis et al., 2006 [5] | 7 | RG | - | 196 (84–315) |
| Dillon et al., 2011 [6] | 27 | PR | 53 (5–182) | - |
| Ford et al., 2018 [33] | 970 (932 + 38) | PR and RG | 21 (7–35) | 59 (21–238) |
| Frank et al., 2019 [7] | 35 (16 + 19) | PR and RG | 37 (25–49) | 273 (30–571) |
| Giacalone et al., 2015 [8] | 23 | PR | 6 (1–19) | - |
| Goyal et al., 2020 [9] | 11 | RG | - | 152 (30–395) |
| Hallam et al., 2004 [10] | 9 | RG | - | 124 (76–197) |
| Haverstock et al., 2017 [11] | 48 | PR | 23 (4–49) | - |
| Hendy et al., 2020 [12] | 138 (92 + 46) | PR and RG | 35 (3–446) | 116 (15–1095) |
| Jain et al., 2024 [34] | 66 | PR | 33 (7–130) | - |
| Khan et al., 2008 [35] | 17 | PR | 19 (2–120) | - |
| McKee et al., 2005 [36] | 53 | PR | 16 (2–84) | - |
| Morrel et al., 2012 [13] | 12 | RG | - | 185 (42–476) |
| Morrey et al., 2014 [27] | 46 | PR | 53 (1–784) | - |
| Phadnis et al., 2016 [14] | 21 | RG | - | 760 (30–2920) |
| Samra et al., 2020 [15] | 24 | PR | 45 (4–284) | - |
| Schmidt et al., 2024 [16] | 30 | PR | 71 (42–204) | - |
| Snir et al., 2013 [17] | 90 | RG | - | 140 (37–244) |
| Wiley et al., 2006 [18] | 7 | RG | - | 119 (35–296) |
| Zeman et al., 2020 [19] | 20 | PR | 70 (28–294) | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giannicola, G.; Prigent, S.; Colozza, A.; Blonna, D.; Amura, A.; Sessa, P. Treatment Delay and Type of Retraction Affect the Surgical Treatment of Distal Biceps Tendon Ruptures: A Quantitative Analysis of 123 Patients. Healthcare 2025, 13, 1977. https://doi.org/10.3390/healthcare13161977
Giannicola G, Prigent S, Colozza A, Blonna D, Amura A, Sessa P. Treatment Delay and Type of Retraction Affect the Surgical Treatment of Distal Biceps Tendon Ruptures: A Quantitative Analysis of 123 Patients. Healthcare. 2025; 13(16):1977. https://doi.org/10.3390/healthcare13161977
Chicago/Turabian StyleGiannicola, Giuseppe, Sebastien Prigent, Alessandra Colozza, Davide Blonna, Andrea Amura, and Pasquale Sessa. 2025. "Treatment Delay and Type of Retraction Affect the Surgical Treatment of Distal Biceps Tendon Ruptures: A Quantitative Analysis of 123 Patients" Healthcare 13, no. 16: 1977. https://doi.org/10.3390/healthcare13161977
APA StyleGiannicola, G., Prigent, S., Colozza, A., Blonna, D., Amura, A., & Sessa, P. (2025). Treatment Delay and Type of Retraction Affect the Surgical Treatment of Distal Biceps Tendon Ruptures: A Quantitative Analysis of 123 Patients. Healthcare, 13(16), 1977. https://doi.org/10.3390/healthcare13161977






