Impact of a Multidomain Outdoor Exercise Intervention on Cardiovascular Health and Functional Capacity for Healthy Aging: A Randomized Controlled Trial (ACTIVA-Senior Study)
Abstract
1. Introduction
2. Materials and Methods
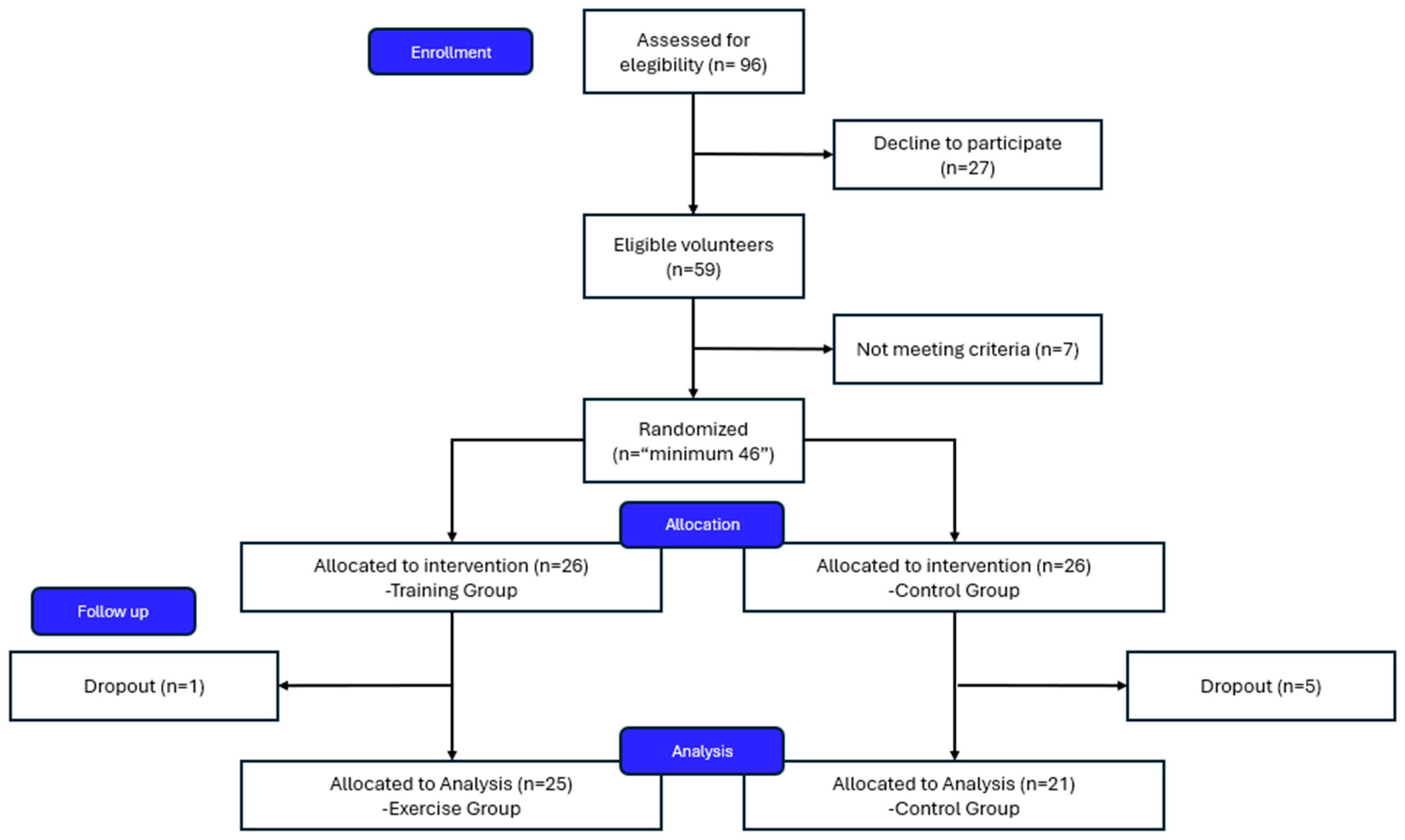
2.1. Study Design and Participants
2.2. Sample Size Calculation
2.3. Randomization and Blinding
2.4. Intervention Protocol
- Strength training: Progressive multi-joint exercises with bodyweight and resistance bands, incorporating isometric holds (30–60 s) in all sessions targeting major muscle groups [27].
- Cardiovascular training: Interval-based activities including brisk walking, stepping, and functional movements guided by the Borg Rating of Perceived Exertion scale (target intensity: 6–7/10) [24].
- Balance and coordination: Static and dynamic balance challenges, proprioceptive training, and functional movement patterns.
- Cognitive training: Dual-task exercises combining physical movement with cognitive challenges, memory games, and executive function tasks.
2.5. Control Group
2.6. Outcome Measures
2.6.1. Primary Outcomes
2.6.2. Secondary Outcomes
2.6.3. Statistical Analysis
3. Results
3.1. Participant Flow and Baseline Characteristics
3.2. Primary Outcomes
3.3. Secondary Outcomes
3.4. Clinical Significance and Number Needed to Treat
3.5. Adherence and Safety
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| IET | Isometric exercise training |
| 6MWT | Six-Minute Walk Test |
| ηp2 | Partial eta square |
| NNT | Number Needed to Treat |
| CI | Confidence interval |
References
- World Health Organization. World Report on Ageing and Health; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Gaidai, O.; Cao, Y.; Loginov, S. Global Cardiovascular Diseases Death Rate Prediction. Curr. Probl. Cardiol. 2023, 48, 101622. [Google Scholar] [CrossRef] [PubMed]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E., Jr.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018, 71, e13–e115. [Google Scholar] [CrossRef]
- Carrasco-Ribelles, L.A.; Cabrera-Bean, M.; Danés-Castells, M.; Zabaleta-Del-Olmo, E.; Roso-Llorach, A.; Violán, C. Contribution of Frailty to Multimorbidity Patterns and Trajectories: Longitudinal Dynamic Cohort Study of Aging People. JMIR Public Health Surveill. 2023, 9, e45848. [Google Scholar] [CrossRef]
- Alizaei Yousefabadi, H.; Niyazi, A.; Alaee, S.; Fathi, M.; Rahimi, G.R.M. Anti-Inflammatory Effects of Exercise on Metabolic Syndrome Patients: A Systematic Review and Meta-Analysis. Biol. Res. Nurs. 2021, 23, 280–292. [Google Scholar] [CrossRef]
- Nelson, M.E.; Rejeski, W.J.; Blair, S.N.; Duncan, P.W.; Judge, J.O.; King, A.C.; Macera, C.A.; Castaneda-Sceppa, C. Physical Activity and Public Health in Older Adults. Med. Sci. Sports Exerc. 2007, 39, 1435–1445. [Google Scholar] [CrossRef]
- Chen, Q.; Gao, X.; Wang, C.; Zhang, P. Influence of different exercise types on vascular endothelial function in middle-aged and older adults—A systematic review and network meta-analysis. Arch. Gerontol. Geriatr. 2025, 128, 105624. [Google Scholar] [CrossRef] [PubMed]
- Green, D.J.; Hopman, M.T.E.; Padilla, J.; Laughlin, M.H.; Thijssen, D.H.J. Vascular Adaptation to Exercise in Humans: Role of Hemodynamic Stimuli. Physiol. Rev. 2017, 97, 495–528. [Google Scholar] [CrossRef] [PubMed]
- García-Llorente, A.M.; Casimiro-Andújar, A.J.; Linhares, D.G.; Vale, R.G.D.S.; Marcos-Pardo, P.J. Multidomain interventions for sarcopenia and cognitive flexibility in older adults for promoting healthy aging: A systematic review and meta-analysis of randomized controlled trials. Aging Clin. Exp. Res. 2024, 36, 47. [Google Scholar] [CrossRef]
- Marcos-Pardo, P.J.; González-Gálvez, N.; Vaquero-Cristóbal, R.; Sagarra-Romero, L.; López-Vivancos, A.; Velázquez-Díaz, D.; García, G.M.G.; Ponce-González, J.G.; Esteban-Cornejo, I.; Jiménez-Pavón, D.; et al. Multidomain healthy-age programme. Recomendations for healthy ageing: On behalf of the healthy-age network. Cult. Cienc. Y Deporte 2021, 16, 311–320. [Google Scholar] [CrossRef]
- Montero-Odasso, M.; van der Velde, N.; Martin, F.C.; Petrovic, M.; Tan, M.P.; Ryg, J.; Aguilar-Navarro, S.; Alexander, N.B.; Becker, C.; Blain, H.; et al. World guidelines for falls prevention and management for older adults: A global initiative. Age Ageing 2022, 51, 1501. [Google Scholar] [CrossRef]
- Kim, D.; Ko, Y.; Jung, A. Longitudinal effects of exercise according to the World Health Organization guidelines on cognitive function in middle-aged and older adults. Front. Public Health 2022, 10, 1009775. [Google Scholar] [CrossRef]
- Cho, S.H.; Kang, H.J.; Park, Y.K.; Moon, S.Y.; Hong, C.H.; Na, H.R.; Song, H.-S.; Choi, M.; Jeong, S.; Park, K.W.; et al. SoUth Korean study to PrEvent cognitive impaiRment and protect BRAIN health through Multidomain interventions via facE-to-facE and video communication plaTforms in mild cognitive impairment (SUPERBRAIN-MEET): Protocol for a Multicenter Randomized Controlled Trial. Dement. Neurocogn. Disord. 2024, 23, 30. [Google Scholar] [CrossRef]
- Lehtisalo, J.; Rusanen, M.; Solomon, A.; Antikainen, R.; Laatikainen, T.; Peltonen, M.; Strandberg, T.; Tuomilehto, J.; Soininen, H.; Kivipelto, M.; et al. Effect of a multi-domain lifestyle intervention on cardiovascular risk in older people: The FINGER trial. Eur. Heart J. 2022, 43, 2054–2061. [Google Scholar] [CrossRef]
- Smart, N.A.; Way, D.; Carlson, D.; Millar, P.; McGowan, C.; Swaine, I.; Baross, A.; Howden, R.; Ritti-Dias, R.; Wiles, J.; et al. Effects of isometric resistance training on resting blood pressure. J. Hypertens. 2019, 37, 1927–1938. [Google Scholar] [CrossRef] [PubMed]
- Edwards, J.J.; Wiles, J.; O’Driscoll, J. Mechanisms for blood pressure reduction following isometric exercise training: A systematic review and meta-analysis. J. Hypertens. 2022, 40, 2299–2306. [Google Scholar] [CrossRef]
- Taylor, K.A.; Wiles, J.D.; Coleman, D.A.; Leeson, P.; Sharma, R.; O’dRiscoll, J.M. Neurohumoral and ambulatory haemodynamic adaptations following isometric exercise training in unmedicated hypertensive patients. J. Hypertens. 2019, 37, 827–836. [Google Scholar] [CrossRef] [PubMed]
- Moon, S.Y.; Hong, C.H.; Jeong, J.H.; Park, Y.K.; Na, H.R.; Song, H.-S.; Kim, B.C.; Park, K.W.; Park, H.K.; Choi, M.; et al. Facility-based and home-based multidomain interventions including cognitive training, exercise, diet, vascular risk management, and motivation for older adults: A randomized controlled feasibility trial. Aging 2021, 13, 15898–15916. [Google Scholar] [CrossRef]
- Marcos-Pardo, P.J.; Espeso-García, A.; Abelleira-Lamela, T.; Machado, D.R.L. Optimizing outdoor fitness equipment training for older adults: Benefits and future directions for healthy aging. Exp. Gerontol. 2023, 181, 112279. [Google Scholar] [CrossRef]
- Noseworthy, M.; Peddie, L.; Buckler, E.J.; Park, F.; Pham, M.; Pratt, S.; Singh, A.; Puterman, E.; Liu-Ambrose, T. The Effects of Outdoor versus Indoor Exercise on Psychological Health, Physical Health, and Physical Activity Behaviour: A Systematic Review of Longitudinal Trials. Int. J. Environ. Res. Public Health 2023, 20, 1669. [Google Scholar] [CrossRef] [PubMed]
- Giacomantonio, N.; Morrison, P.; Rasmussen, R.; MacKay-Lyons, M.J. Reliability and Validity of the 6-Minute Step Test for Clinical Assessment of Cardiorespiratory Fitness in People at Risk of Cardiovascular Disease. J. Strength Cond. Res. 2020, 34, 1376–1382. [Google Scholar] [CrossRef]
- Liu, L.; Ma, M.; Yang, X.; Yang, Y.; Huang, X.; Meng, L.; Ming, D. Impact of gender and age on 6-Minute Walking Test performance of patients with coronary heart disease compared to healthy elders. In Proceedings of the 2021 43rd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Virtual, 1–5 November 2021; IEEE: Piscataway, NJ, USA, 2021; pp. 6277–6280. [Google Scholar]
- Wang, Z.; Qi, K.; Zhang, P. Effect of physical activity interventions on physical and mental health of the elderly: A systematic review and meta-analysis. Aging Clin. Exp. Res. 2025, 37, 169. [Google Scholar] [CrossRef]
- García-Llorente, A.M.; Vaquero-Cristóbal, R.; Casimiro-Andújar, A.J.; Abraldes, J.A.; Marcos-Pardo, P.J. ACTIVA-Senior: Study Design and Protocol for a Preliminary Multidomain Outdoor Intervention Promoting Healthy Aging and Mitigating Psycho-Physiological Decline. Healthcare 2025, 13, 1110. [Google Scholar] [CrossRef]
- Liguori, G. ACSM’s Guidelines for Exercise Testing and Prescription; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2020. [Google Scholar]
- Marcos-Pardo, P.J.; González-Gálvez, N.; Gea-García, G.M.; López-Vivancos, A.; Espeso-García, A.; Gomes de Souza Vale, R. Sarcopenia as a Mediator of the Effect of a Gerontogymnastics Program on Cardiorespiratory Fitness of Overweight and Obese Older Women: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2020, 17, 7064. [Google Scholar] [CrossRef]
- Fragala, M.S.; Cadore, E.L.; Dorgo, S.; Izquierdo, M.; Kraemer, W.J.; Peterson, M.D.; Ryan, E.D. Resistance Training for Older Adults: Position Statement from the National Strength and Conditioning Association. J. Strength Cond. Res. 2019, 33, 2019–2052. [Google Scholar] [CrossRef] [PubMed]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef] [PubMed]
- Edwards, J.; De Caux, A.; Donaldson, J.; Wiles, J.; O’DRiscoll, J. Isometric exercise versus high-intensity interval training for the management of blood pressure: A systematic review and meta-analysis. Br. J. Sports Med. 2022, 56, 506–514. [Google Scholar] [CrossRef] [PubMed]
- Suematsu, Y.; Morita, H.; Abe, M.; Uehara, Y.; Koyoshi, R.; Fujimi, K.; Ideishi, A.; Takata, K.; Kato, Y.; Hirata, T.; et al. Differences in the effects of exercise on blood pressure depending on the physical condition of the subject and the type of exercise: A systematic review and meta-analysis. Hypertens. Res. 2025, 48, 720–732. [Google Scholar] [CrossRef]
- Li, B.; Li, Y.; Zhang, Y.; Liu, P.; Song, Y.; Zhou, Y.; Ma, L. Visceral Fat Obesity Correlates with Frailty in Middle-Aged and Older Adults. Diabetes Metab. Syndr. Obes. 2022, 15, 2877–2884. [Google Scholar] [CrossRef]
- Englund, D.A.; Kirn, D.R.; Koochek, A.; Zhu, H.; Travison, T.G.; Reid, K.F.; von Berens, Å.; Melin, M.; Cederholm, T.; Gustafsson, T.; et al. Nutritional Supplementation with Physical Activity Improves Muscle Composition in Mobility-Limited Older Adults, the VIVE2 Study: A Randomized, Double-Blind, Placebo-Controlled Trial. J. Gerontol. Ser. A 2018, 73, 95–101. [Google Scholar] [CrossRef]
- Duijvestijn, M.; de Wit, G.A.; van Gils, P.F.; Wendel-Vos, G.C.W. Impact of physical activity on healthcare costs: A systematic review. BMC Health Serv. Res. 2023, 23, 572. [Google Scholar] [CrossRef]
- Izquierdo, M.; de Souto Barreto, P.; Arai, H.; Bischoff-Ferrari, H.A.; Cadore, E.L.; Cesari, M.; Chen, L.-K.; Coen, P.M.; Courneya, K.S.; Duque, G.; et al. Global consensus on optimal exercise recommendations for enhancing healthy longevity in older adults (ICFSR). J. Nutr. Health Aging 2025, 29, 100401. [Google Scholar] [CrossRef] [PubMed]
- Hejazi, K.; Iraj, Z.A.; Saeidi, A.; Hackney, A.C.; Laziri, F.; Suzuki, K.; Laher, I.; Hassane, Z. Differential effects of exercise training protocols on blood pressures and lipid profiles in older adults patients with hypertension: A systematic review and meta-analysis. Arch. Gerontol. Geriatr. 2025, 131, 105737. [Google Scholar] [CrossRef] [PubMed]
- Hopewell, S.; Chan, A.W.; Collins, G.S.; Hróbjartsson, A.; Moher, D.; Schulz, K.F.; Tunn, R.; Aggarwal, R.; Berkwits, M.; Berlin, J.A.; et al. CONSORT 2025 Statement: Updated guideline for reporting randomised trials. BMJ 2025, 388, e081123. [Google Scholar] [CrossRef] [PubMed]

| Variable | Intervention (n = 25) | Control (n = 21) | p-Value |
|---|---|---|---|
| Age (years) | 65.6 ± 5.3 | 66.4 ± 4.9 | 0.609 |
| Female | 16 (64.0%) | 11 (52.4%) | 0.619 |
| CV medication use | 8 (32.0%) | 8 (38.1%) | 0.777 |
| Cardiovascular variables | |||
| Resting HR (bpm) | 76.0 ± 9.5 | 77.9 ± 13.2 | 0.591 |
| Systolic BP (mmHg) | 142.9 ± 15.7 | 139.2 ± 11.8 | 0.381 |
| Diastolic BP (mmHg) | 85.6 ± 8.6 | 84.0 ± 6.7 | 0.495 |
| Resting HR (bpm) | 76.0 ± 9.5 | 77.9 ± 13.2 | 0.591 |
| 6MWT distance (m) | 548.9 ± 61.8 | 586.4 ± 61.7 | 0.046 * |
| Body composition variables | |||
| Height (cm) | 160.4 ± 8.9 | 161.9 ± 9.2 | 0.577 |
| Weight (kg) | 71.7 ± 11.6 | 70.1 ± 14.2 | 0.668 |
| BMI (kg/m2) | 27.8 ± 3.5 | 26.5 ± 3.8 | 0.261 |
| Body fat (%) | 36.3 ± 6.8 | 33.3 ± 7.1 | 0.153 |
| Visceral fat level | 13.1 ± 3.9 | 11.2 ± 4.3 | 0.137 |
| Symptoms | |||
| Joint discomfort | 2 (8%) | 1 (5%) | 0.600 |
| Outcome | Group | Pre-Test | Post-Test | Change | 95% CI | Effect Size (d) | p-Value | F | η2p |
|---|---|---|---|---|---|---|---|---|---|
| Systolic BP (mmHg) | Intervention | 142.9 ± 15.7 | 125.5 ± 12.2 | −17.4 ± 11.0 | [−21.9 to −12.9] | 1.24 | <0.001 * | 26.49 | 0.376 |
| Control | 139.2 ± 11.8 | 136.2 ± 11.4 | −3.1 ± 7.2 | [−6.3 to 0.2] | 0.26 | 0.065 | |||
| Diastolic BP (mmHg) | Intervention | 85.6 ± 8.6 | 76.4 ± 7.3 | −9.2 ± 7.0 | [−12.1 to −6.3] | 1.15 | <0.001 * | 14.52 | 0.248 |
| Control | 84.0 ± 6.7 | 82.5 ± 6.9 | −1.6 ± 6.5 | [−4.5 to 1.4] | 0.23 | 0.281 | |||
| 6MWT (meters) | Intervention | 548.9 ± 61.8 | 613.6 ± 68.6 | 64.7 ± 45.6 | [45.9 to 83.5] | 0.99 | <0.001 * | 37.89 | 0.463 |
| Control | 586.4 ± 61.7 | 569.6 ± 67.8 | −16.8 ± 43.6 | [−36.6 to 3.1] | 0.26 | 0.093 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
García-Llorente, A.M.; Lopes Machado, D.R.; Casimiro-Andújar, A.J.; Marcos-Pardo, P.J. Impact of a Multidomain Outdoor Exercise Intervention on Cardiovascular Health and Functional Capacity for Healthy Aging: A Randomized Controlled Trial (ACTIVA-Senior Study). Healthcare 2025, 13, 1975. https://doi.org/10.3390/healthcare13161975
García-Llorente AM, Lopes Machado DR, Casimiro-Andújar AJ, Marcos-Pardo PJ. Impact of a Multidomain Outdoor Exercise Intervention on Cardiovascular Health and Functional Capacity for Healthy Aging: A Randomized Controlled Trial (ACTIVA-Senior Study). Healthcare. 2025; 13(16):1975. https://doi.org/10.3390/healthcare13161975
Chicago/Turabian StyleGarcía-Llorente, Antonio Manuel, Dalmo Roberto Lopes Machado, Antonio Jesús Casimiro-Andújar, and Pablo Jorge Marcos-Pardo. 2025. "Impact of a Multidomain Outdoor Exercise Intervention on Cardiovascular Health and Functional Capacity for Healthy Aging: A Randomized Controlled Trial (ACTIVA-Senior Study)" Healthcare 13, no. 16: 1975. https://doi.org/10.3390/healthcare13161975
APA StyleGarcía-Llorente, A. M., Lopes Machado, D. R., Casimiro-Andújar, A. J., & Marcos-Pardo, P. J. (2025). Impact of a Multidomain Outdoor Exercise Intervention on Cardiovascular Health and Functional Capacity for Healthy Aging: A Randomized Controlled Trial (ACTIVA-Senior Study). Healthcare, 13(16), 1975. https://doi.org/10.3390/healthcare13161975









