Personalizing Patient Education for Pancreatic Cancer Patients Receiving Multidisciplinary Care with Integration of Novel Digital Tools
Abstract
1. Introduction
2. Materials and Methods
3. Results
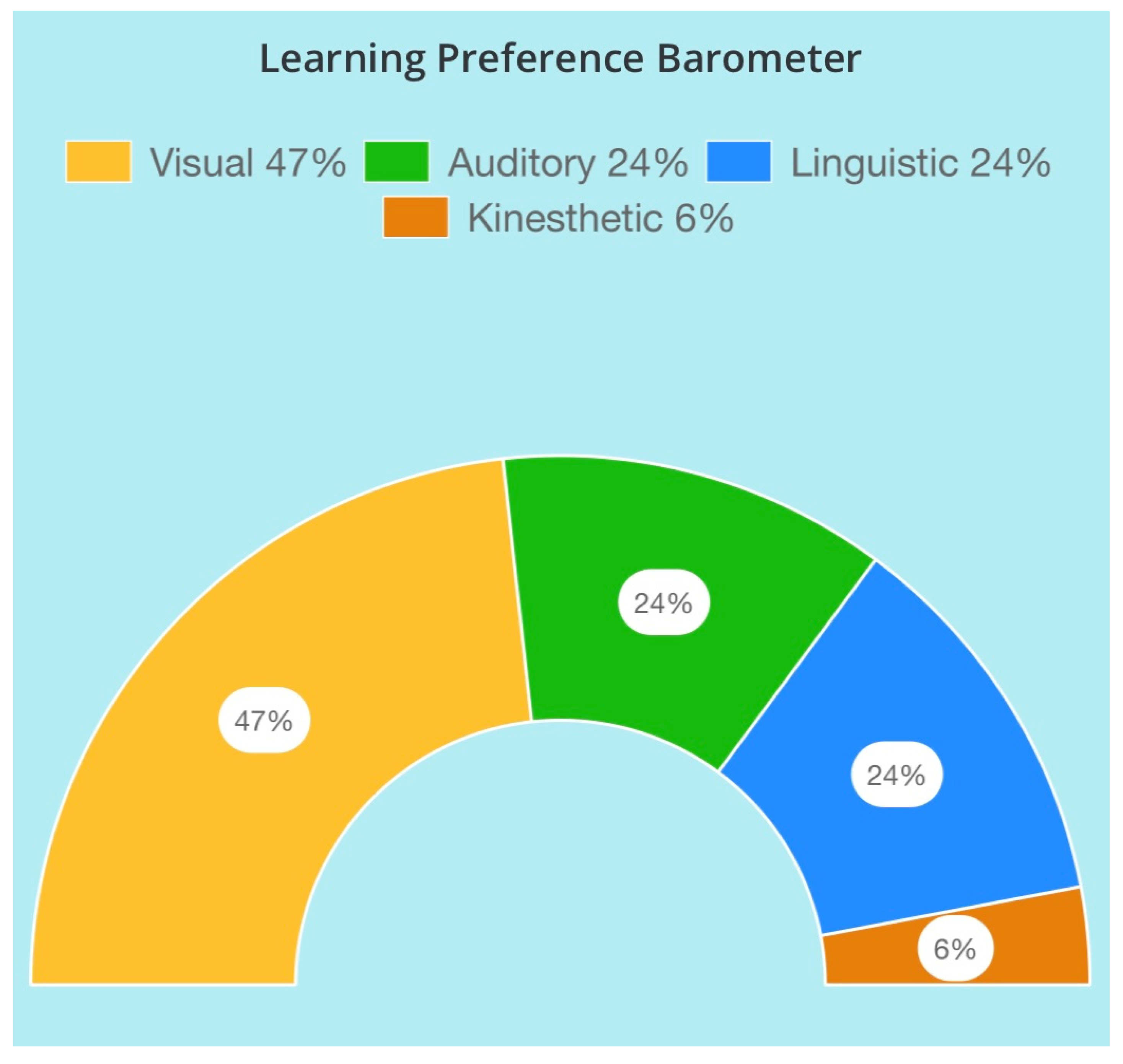
3.1. Learning Preference Barometer
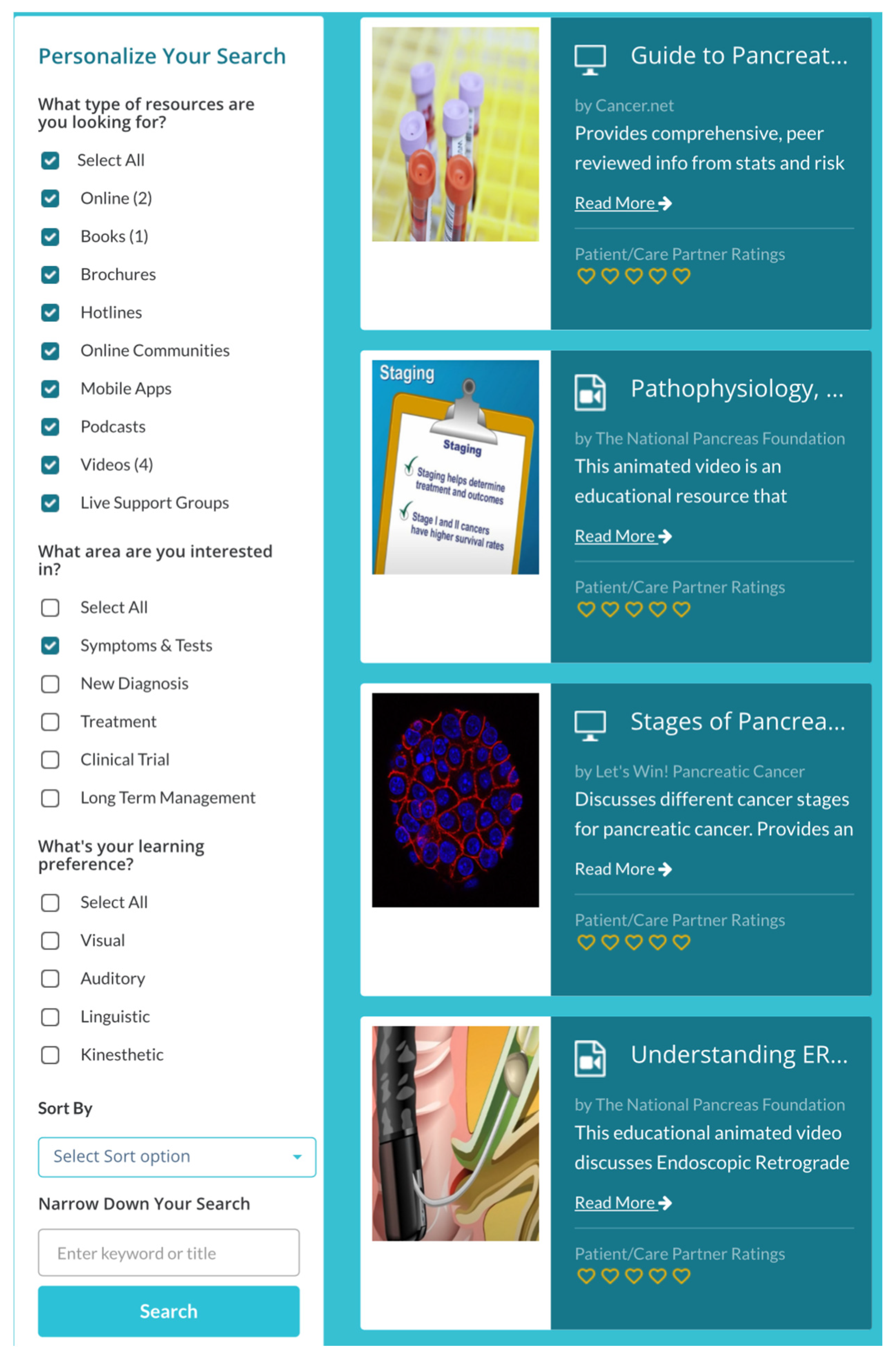
3.2. Prescription to Learn®
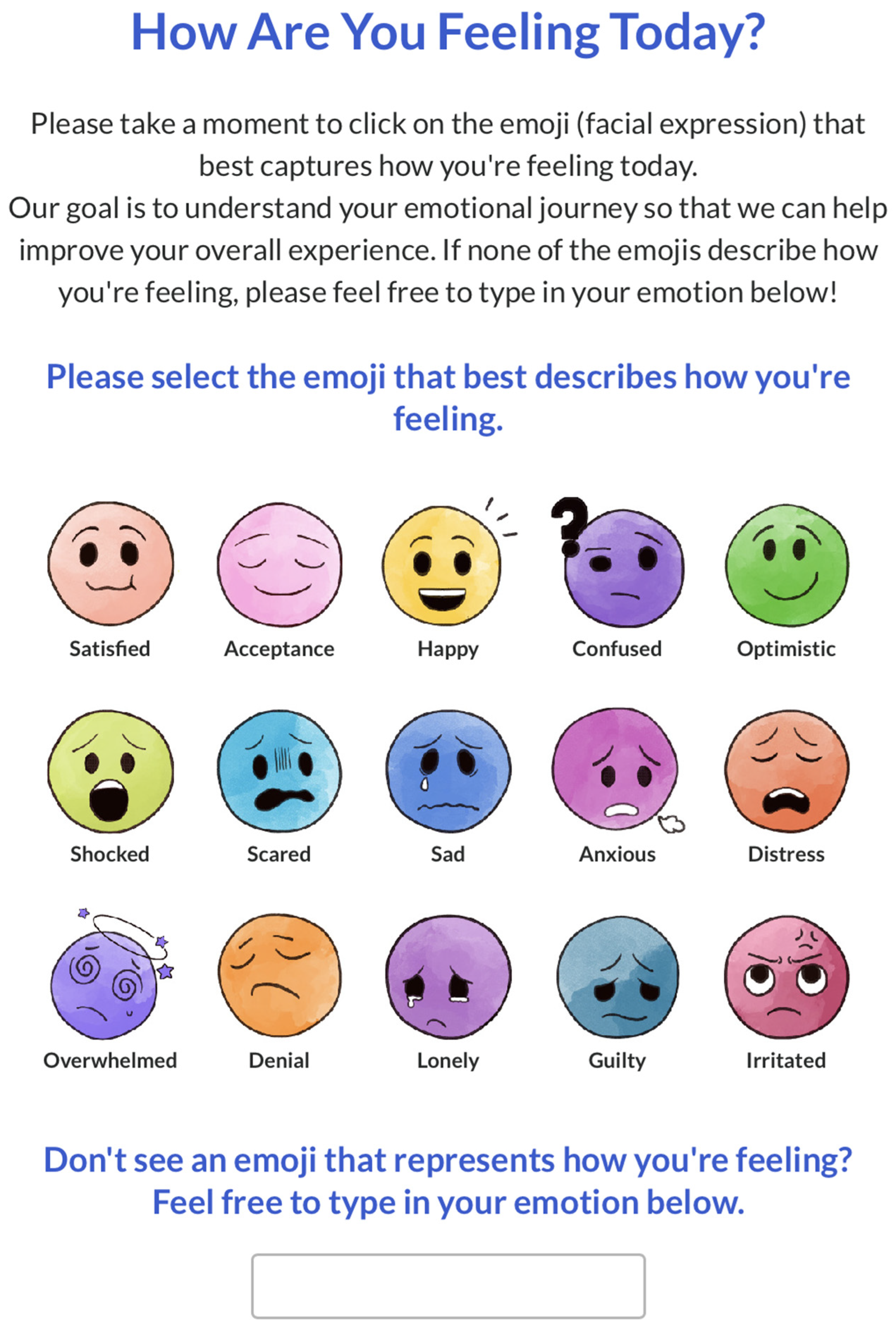
3.3. Emotional Journey Barometer
4. Discussion
4.1. Learning Preferences (LPs)
4.2. Emotional States
4.3. Shared Decision Making
4.4. Project Implications
4.4.1. Practical Implications
4.4.2. Conceptual Implications
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PC | Pancreatic cancer |
| LPB | Learning preference barometer |
| EJB | Emotional journey barometer |
| C101 | CANCER101 |
| LP | Learning preference |
| P2L | Prescription to Learn® |
| POC | Point of care |
| CCI | Charlson Comorbidity Index |
| ADI | Area Depravation Index |
| ECOG | Eastern Cooperative Oncology Group |
| NCCN-DT | National Comprehensive Cancer Network Distress Thermometer |
| SDM | Shared decision making |
| AI | Artificial Intelligence |
Appendix A
Appendix A.1. Learning Preference Barometer (LPB)
Appendix A.2. Emotional Journey Barometer (EJB)
Appendix A.3. Prescription to Learn®
Appendix A.4. Area Depravation Index (ADI)
| Characteristic | ADI Score Median (Range) | ||
|---|---|---|---|
| Learning Preference | Auditory (n = 5) | 6 (4–10) | |
| Kinesthetic (n = 4) | 5 (2–7) | ||
| Linguistic (n = 21) | 6 (1–10) | ||
| Visual (n = 16) | 8 (2–10) | ||
| Visual/Auditory (n = 1) | 5 | ||
| Baseline ADI | Assessment 2 ADI | ||
| Emoji Responses | Acceptance | 5 (1–8) (n = 5) | 8 (1–9) (n = 7) |
| Acceptance/Optimistic | 2 (n = 1) | - | |
| Alright | - | 4 (n = 1) | |
| Angry | 8 (n = 1) | - | |
| Anxious | 6.5 (4–6) (n = 2) | - | |
| Confused | 9 (n = 1) | - | |
| Happy | 9 (2–10) (n = 3) | 7.5 (5–10) (n = 2) | |
| Irate | - | 2 (n = 1) | |
| Optimistic | 7 (2–10) (n = 20) | 5 (2–10) (n = 7) | |
| Overwhelmed | 3 (2–6) (n = 3) | 3 (n = 1) | |
| Satisfied | 8 (3–10) (n = 9) | 6 (5–7) (n = 2) | |
| Scared | 9 (n = 1) | - | |
| Stress | 2 (n = 1) | - | |
References
- Rowe, D.G.; O’Callaghan, E.; Yoo, S.; Dalton, J.C.; Woo, J.; Owolo, E.; Dalton, T.; Johnson, M.O.; Goodwin, A.N.; Crowell, K.-A.; et al. Perioperative trends in distress among cancer patients: A systematic review and meta-analysis. Cancer Med. 2025, 14, e70456. [Google Scholar] [CrossRef] [PubMed]
- Herschbach, P.; Britzelmeir, I.; Dinkel, A.; Giesler, J.M.; Herkommer, K.; Nest, A.; Pichler, T.; Reichelt, R.; Tanzer-Küntzer, S.; Weis, J.; et al. Distress in cancer patients: Who are the main groups at risk? Psychooncology 2020, 29, 703–710. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Ren, Z.; Wakefield, C.E.; Hui, B.P.H.; Akechi, T.; Shi, C.; Du, X.; Chen, W.; Lai, L.; Zhao, C.; et al. Are digital psychological interventions for psychological distress and quality of life in cancer patients effective? A systematic review and network meta-analysis. Clin. Psychol. Rev. 2025, 115, 102520. [Google Scholar] [CrossRef]
- MacKay, T.M.; Latenstein, E.J.; Sprangers, M.A.G.; van der Geest, L.G.; Creemers, G.-J.; van Dieren, S.; de Groot, J.-W.B.; Koerkamp, B.G.; de Hingh, I.H.; Homs, M.Y.; et al. Relationship between quality of life and survival in patients with pancreatic and periampullary cancer: A multicenter cohort analysis. JNCCN J. Natl. Compr. Cancer Netw. 2020, 18, 1354–1363. [Google Scholar] [CrossRef]
- Main, C.J.; Ballengee, L.A.; George, S.Z.; Beneciuk, J.M.; Greco, C.M.; Simon, C.B. Psychologically informed practice: The importance of communication in clinical implementation. Phys. Ther. 2023, 103, pzad047. [Google Scholar] [CrossRef]
- Hyatt, A.; Shelly, A.; Cox, R.; Humphries, E.; Lock, G.; Varlow, M. How can we improve information for people affected by cancer? A national survey exploring gaps in current information provision, and challenges with accessing cancer information online. Patient Educ. Couns. 2022, 105, 2763–2770. [Google Scholar] [CrossRef]
- Lie, H.C.; Juvet, L.K.; Street, R.L.; Gulbrandsen, P.; Mellblom, A.V.; Brembo, E.A.; Eide, H.; Heyn, L.; Saltveit, K.H.; Strømme, H.; et al. Effects of physicians’ information giving on patient outcomes: A systematic review. J. Gen. Intern. Med. 2021, 37, 651–663. [Google Scholar] [CrossRef]
- Talevski, J.; Wong Shee, A.; Rasmussen, B.; Kemp, G.; Beauchamp, A. Teach-back: A systematic review of implementation and impacts. PLoS ONE 2020, 15, e0231350. [Google Scholar] [CrossRef]
- Williams, C. Innovative Solutions for Surgical Education. J. Perioper. Nurs. 2024, 37, e12–e17. [Google Scholar] [CrossRef]
- Sethares, K.A.; Westlake, C.; Viveiros, J.D.; Elliott, K. Correlation of health literacy and learning style preference in persons with heart failure. Patient Educ. Couns. 2024, 127, 108367. [Google Scholar] [CrossRef] [PubMed]
- Tzenois, N. Clustering Students for Personalized Health Education Based on Learning Styles. Sage Sci. Rev. Educ. Technol. 2020, 3, 22–36. [Google Scholar]
- Dantas, L.A.; Cunha, A. An integrative debate on learning styles and the learning process. Soc. Sci. Amp Humanit. Open 2020, 2, 100017. [Google Scholar] [CrossRef]
- Deale, C.S. Learning Preferences Instead of Learning Styles: A Case Study of Hospitality Management Students’ Perceptions of How They Learn Best and Implications for Teaching and Learning. Int. J. Scholarsh. Teach. Learn. 2019, 13, 11. [Google Scholar] [CrossRef]
- Cabual, R.A. Learning styles and preferred learning modalities in the new normal. OALib 2021, 8, 1–14. [Google Scholar] [CrossRef]
- Kunselman, A.R. A brief overview of pilot studies and their sample size justification. Fertil. Steril. 2024, 121, 899–901. [Google Scholar] [CrossRef]
- Hennink, M.; Kaiser, B.N. Sample sizes for saturation in qualitative research: A systematic review of empirical tests. Soc. Sci. Amp Med. 2022, 292, 114523. [Google Scholar] [CrossRef] [PubMed]
- Hong, Y.; Yadav, S.; Suk, R.; Khanijahani, A.; Erim, D.; Turner, K. Patient–provider discussion about emotional and social needs, mental health outcomes, and benefit finding among U.S. adults living with cancer. Cancer Med. 2021, 10, 3622–3634. [Google Scholar] [CrossRef]
- Ennis, R.D.; Corn, B.W.; Krug, S.; Vapiwala, N.; Hoffe, S.E. Decision making in health care: Embracing the real people comprising the patient-doctor relationship. JCO Oncol. Pract. 2024, 20, 614–616. [Google Scholar] [CrossRef] [PubMed]
- Montori, V.M.; Ruissen, M.M.; Hargraves, I.G.; Brito, J.P.; Kunneman, M. Shared decision-making as a method of care. BMJ Evid. Based Med. 2023, 28, 213–217. [Google Scholar] [CrossRef] [PubMed]
- Leech, M.; Katz, M.S.; Kazmierska, J.; McCrossin, J.; Turner, S. Empowering patients in decision-making in radiation oncology—Can we do better? Mol. Oncol. 2020, 14, 1442–1460. [Google Scholar] [CrossRef]
- Mundle, R.; Afenya, E.; Agarwal, N. The effectiveness of psychological intervention for depression, anxiety, and distress in prostate cancer: A systematic review of literature. Prostate Cancer Prostatic Dis. 2021, 24, 674–687. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Percent of Patients | |
|---|---|---|
| Social Determinants | Lifestyle Concerns | 30% |
| Education Level of High School/GED or Trade School | 29% | |
| Financial Concerns | 20% | |
| Dependent Children in the Household | 14% | |
| Insurance/Employment Disability | 9% | |
| Insurance | Medicare | 60% |
| Commercial | 25% | |
| VA (veterans) | 4% | |
| Out of Network or Not Insured | 11% | |
| Regionalization | Northwest Florida | 2% |
| Central West Florida | 41% | |
| Central East Florida | 19% | |
| Southwest Florida | 30% | |
| Southeast Florida | 4% | |
| Out of State | 4% | |
| Secondary Preference | Primary Learning Preference | ||||
|---|---|---|---|---|---|
| Visual (n = 16) | Linguistic (n = 21) | Auditory (n = 5) | Kinesthetic (n = 4) | Auditory/Visual Combination (n = 1) | |
| Visual | - | 19% | 0% | 50% | - |
| (n = 4) | (n = 0) | (n = 2) | |||
| Linguistic | 31% (n = 5) | - | 40% | 25% | 0% |
| (n = 2) | (n = 1) | (n = 0) | |||
| Auditory | 19% (n = 3) | 29% | - | 25% | - |
| (n = 6) | (n = 1) | ||||
| Kinesthetic | 6% (n = 1) | - | 0% | - | 0% |
| (n = 0) | (n = 0) | ||||
| Nursing Assessment Learning Preference | Number of Patients | Primary Learning Preference from LPB |
|---|---|---|
| Demonstration, reading, video/visual | 3% (n = 1/38) | Linguistic |
| Demonstration, reading, verbal | 5% (n = 2/38) | Auditory = 1 Visual = 1 |
| Demonstration, verbal, video/visual | 3% (n = 1/38) | Visual |
| Reading, verbal | 5% (n = 2/38) | Auditory = 1 Visual = 1 |
| Reading, verbal, video/visual | 76% (n = 29/38) | Auditory = 2 Kinesthetic = 3 Linguistic = 16 Visual = 7 Visual/Auditory = 1 |
| Verbal | 8% (n = 3/38) | Linguistic = 1 Visual = 2 |
| Number of Resources Accesses | Age | Gender | ||||
|---|---|---|---|---|---|---|
| 50–60 Years | 61–70 Years | 71–80 Years | 81–90 Years | Male | Female | |
| (n = 4) | (n = 12) | (n = 10) | (n = 5) | |||
| 1 (n = 15) | 100% | 42% | 30% | 60% | 33% | 67% |
| (n = 4) | (n = 5) | (n = 3) | (n = 3) | (n = 5) | (n = 10) | |
| 2 (n = 13) | 0% | 50% | 50% | 40% | 54% | 46% |
| (n = 0) | (n = 6) | (n = 5) | (n = 2) | (n = 7) | (n = 6) | |
| 3 (n = 1) | 0% | 0% | 10% | 0% | 100% | 0% |
| (n = 0) | (n = 0) | (n = 1) | (n = 0) | (n = 1) | (n = 0) | |
| 6 (n = 1) | 0% | 8% | 0% | 0% | 100% | 0% |
| (n = 0) | (n = 1) | (n = 0) | (n = 0) | (n = 1) | (n = 0) | |
| 8 (n = 1) | 0% | 0% | 10% | 0% | 0% | 100% |
| (n = 0) | (n = 0) | (n = 1) | (n = 0) | (n = 0) | (n = 1) | |
| Chosen Emotion | Transcribed Responses |
|---|---|
| Acceptance | I’m starting to feel more relaxed with the procedures as I go through them, [both] with the radiation and the other doctors that I’m going to meet to converse about my plan. So, I think things are heading in the right direction. |
| Satisfied | I chose “satisfied.” I felt that was the best [answer] because I came in confused, unsure, not knowing, and I got answers. |
| Overwhelmed | I am not overly distressed. I do have some grave concerns but basically [I have] a whole lot of information I have to sort through to digest. |
| Angry | I am angry, I am pissed off, because I didn’t do any of the [things] to get this, and I got it, and I’m as mad as I can be. |
| Scared | [The reason] why I’m scared is the unknown. I don’t know how long I’m going to live and what the pain is going to be like. I don’t know what else. |
| Stressed | I am feeling stressed because it’s all at once and it’s hitting me. I know how serious this is because I’m an RN and things can always go wrong. I’m afraid that I won’t make it through surgery. |
| Anxious | I’m worried about things I shouldn’t be worried about. Things that are coming up in my care. Anxious about the next chemo treatment, this one didn’t go very well. |
| Optimistic | I’m optimistic that this is going to work and give me a few more months. |
| Happy | I’m happy because I have a plan and I’m going to beat this. |
| EJB Assessment | Emoji Response | Treatment State |
|---|---|---|
| Assessment 1 (n = 47) | Acceptance | 40% treatment naive |
| 20% on chemotherapy | ||
| 20% pre radiation | ||
| 20% on radiation | ||
| Acceptance/Optimistic | 100% treatment naive | |
| Angry | 100% treatment naive | |
| Anxious | 50% on chemotherapy | |
| 50% pre radiation | ||
| Confused | 100% on chemotherapy | |
| Happy | 34% treatment naive | |
| 33% on chemotherapy | ||
| 33% pre radiation | ||
| Optimistic | 40% treatment naive | |
| 50% on chemotherapy | ||
| 5% pre radiation | ||
| 5% on radiation | ||
| Overwhelmed | 34% treatment naive | |
| 33% pre radiation | ||
| 33% on radiation | ||
| Satisfied | 33% treatment naive | |
| 45% on chemotherapy | ||
| 22% pre radiation | ||
| Scared | 100% treatment naive | |
| Stress | 100% treatment naive | |
| Assessment 2 (n = 21) | Acceptance | 14% treatment naive |
| 14% pre radiation | ||
| 72% on radiation | ||
| Alright | 100% on chemotherapy | |
| Happy | 100% post radiation | |
| Irate | 100% on chemotherapy | |
| Optimistic | 34% treatment naive | |
| 14% on chemotherapy | ||
| 29% on radiation | ||
| 14% post radiation | ||
| Overwhelmed | 100% on radiation | |
| Satisfied | 50% on chemotherapy | |
| 50% on radiation | ||
| Assessment 3 (n = 5) | Acceptance | 100% on radiation |
| Confused | 100% treatment naive | |
| Nervous | 100% on radiation | |
| Optimistic | 100% pre radiation | |
| Satisfied | 100% treatment naive | |
| Assessment 4 (n = 1) | Happy | 100% post radiation |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nardella, N.; Adams, M.; Oraiqat, A.; Gonzalez, B.D.; Thomas, C.; Goodchild, S.; Adamson, S.; Sandoval, M.; Frakes, J.; Palm, R.F.; et al. Personalizing Patient Education for Pancreatic Cancer Patients Receiving Multidisciplinary Care with Integration of Novel Digital Tools. Healthcare 2025, 13, 1929. https://doi.org/10.3390/healthcare13151929
Nardella N, Adams M, Oraiqat A, Gonzalez BD, Thomas C, Goodchild S, Adamson S, Sandoval M, Frakes J, Palm RF, et al. Personalizing Patient Education for Pancreatic Cancer Patients Receiving Multidisciplinary Care with Integration of Novel Digital Tools. Healthcare. 2025; 13(15):1929. https://doi.org/10.3390/healthcare13151929
Chicago/Turabian StyleNardella, Nicole, Matt Adams, Adrianna Oraiqat, Brian D. Gonzalez, Corinne Thomas, Sarah Goodchild, Sonia Adamson, Maria Sandoval, Jessica Frakes, Russell F. Palm, and et al. 2025. "Personalizing Patient Education for Pancreatic Cancer Patients Receiving Multidisciplinary Care with Integration of Novel Digital Tools" Healthcare 13, no. 15: 1929. https://doi.org/10.3390/healthcare13151929
APA StyleNardella, N., Adams, M., Oraiqat, A., Gonzalez, B. D., Thomas, C., Goodchild, S., Adamson, S., Sandoval, M., Frakes, J., Palm, R. F., Stricker, C., Herman, J., Hodul, P., Krüg, S., & Hoffe, S. (2025). Personalizing Patient Education for Pancreatic Cancer Patients Receiving Multidisciplinary Care with Integration of Novel Digital Tools. Healthcare, 13(15), 1929. https://doi.org/10.3390/healthcare13151929







