Physical Training Protocols for Improving Dyspnea and Fatigue in Long COVID: A Systematic Review with Meta-Analysis
Abstract
1. Introduction
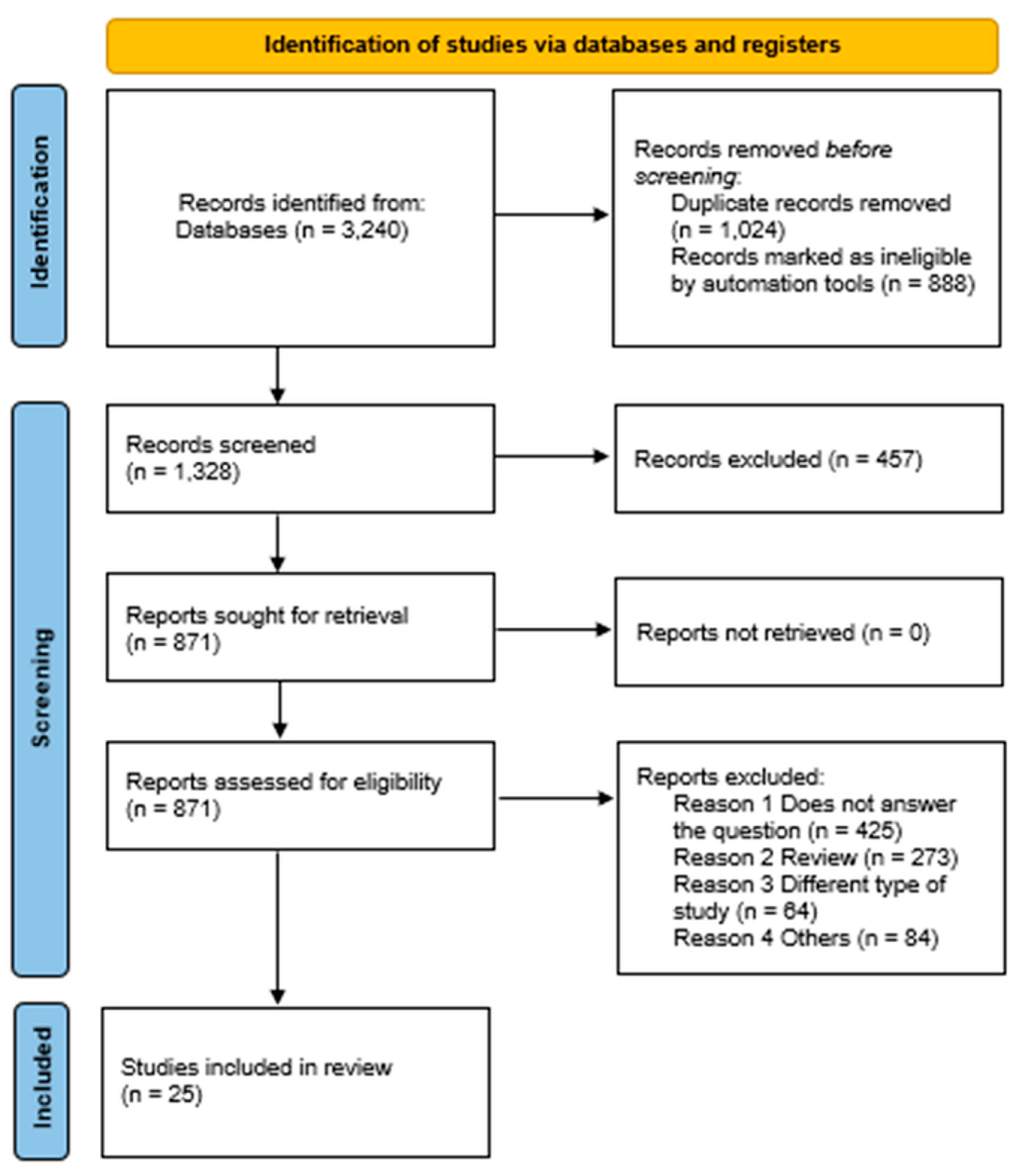
2. Materials and Methods
3. Results
3.1. Physical Training Protocols Used
3.2. Effect of Training Protocols on Fatigue and Dyspnea
3.3. Assessment of Dyspnea
3.4. Assessment of Fatigue
3.5. Methodological Quality of Included Articles
3.6. Meta-Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Astin, R.; Banerjee, A.; Baker, M.R.; Dani, M.; Ford, E.; Hull, J.H.; Lim, P.B.; McNarry, M.; Morten, K.; O'Sullivan, O.; et al. Long COVID: Mechanisms, risk factors and recovery. Exp. Physiol. 2023, 108, 12–27. [Google Scholar] [CrossRef] [PubMed]
- Edward, J.A.; Peruri, A.; Rudofker, E.; Shamapant, N.; Parker, H.; Cotter, R.; Sabin, K.; Lawley, J.; Cornwell, W. Characteristics and Treatment of Exercise Intolerance in Patients with Long COVID. J. Cardiopulm. Rehabil. Prev. 2023, 43, 400–406. [Google Scholar] [CrossRef]
- Singh, S.J.; Baldwin, M.M.; Daynes, E.; Evans, R.A.; Greening, N.J.; Jenkins, R.G.; Lone, N.I.; McAuley, H.; Mehta, P.; Newman, J.; et al. Respiratory sequelae of COVID-19: Pulmonary and extrapulmonary origins, and approaches to clinical care and rehabilitation. Lancet Respir. Med. 2023, 11, 709–725. [Google Scholar] [CrossRef]
- COVID-19 Rapid Guideline: Managing the Long-Term Effects of COVID-19; National Institute for Health and Care Excellence (NICE): London, UK, 2024. [PubMed]
- Cavigli, L.; Fusi, C.; Focardi, M.; Mandoli, G.E.; Pastore, M.C.; Cameli, M.; Valente, S.; Zorzi, A.; Bonifazi, M.; D’Andrea, A.; et al. Post-Acute Sequelae of COVID-19: The Potential Role of Exercise Therapy in Treating Patients and Athletes Returning to Play. J. Clin. Med. 2022, 12, 288. [Google Scholar] [CrossRef]
- Adidharma, N.C.; Dharma, B.D.I.; Negara, K.N.D.P.; Sudewa, I.G.A. Breathing exercise and chest physiotherapy in post-acute COVID-19 patient: A case report. Intisari Sains Medis 2022, 13, 293–296. [Google Scholar] [CrossRef]
- Fugazzaro, S.; Contri, A.; Esseroukh, O.; Kaleci, S.; Croci, S.; Massari, M.; Facciolong, N.C.; Besutti, G.; Iori, M.; Salvarani, C.; et al. Rehabilitation Interventions for Post-Acute COVID-19 Syndrome: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 5185. [Google Scholar] [CrossRef]
- Davis, H.E.; McCorkell, L.; Vogel, J.M.; Topol, E.J. Long COVID: Major findings, mechanisms and recommendations. Nat. Rev. Microbiol. 2023, 21, 133–146. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Chen, H.; Eldridge, S.M.; Emberson, J.R. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, l4898. [Google Scholar] [CrossRef] [PubMed]
- The Cochrane Collaboration. Review Manager (RevMan) [Computer Program], Version 5.4; The Cochrane Collaboration: London, UK, 2020; Available online: https://training.cochrane.org/online-learning/core-software-cochrane-reviews/revman (accessed on 5 August 2024).
- Vieira da Costa, K.; Tainá Cordeiro de Souza, I.; Felix, J.V.D.S.; Brandão, C.B.F.; Fernandes, V.M.S.; Favero, A.B.L.; Gouveia, M.L.A.; Lima, D.T.; Lima, J.H.M.; Pedrosa, R.; et al. Efficacy of a rehabilitation protocol on pulmonary and respiratory muscle function and ultrasound evaluation of diaphragm and quadriceps femoris in patients with post-COVID-19 syndrome: A series of cases. Monaldi Arch. Chest Dis. 2022, 93. [Google Scholar] [CrossRef] [PubMed]
- Dumitrescu, A.; Doros, G.; Lazureanu, V.E.; Septimiu-Radu, S.; Bratosin, F.; Rosca, O.; Patel, H.; Porosnicu, T.M.; Vitcu, G.M.; Mirea, A.; et al. Post-Severe-COVID-19 Cardiopulmonary Rehabilitation: A Comprehensive Study on Patient Features and Recovery Dynamics in Correlation with Workout Intensity. J. Clin. Med. 2023, 12, 4390. [Google Scholar] [CrossRef] [PubMed]
- Elhamrawy, M.Y.; El Sayed, M.E.; Mokhtar, M.M.; Mashaal, A.; Elkady, S.M.; Elsadany, S.M.; Said, M.T. Effect of Tai Chi versus aerobic training on improving hand grip strength, fatigue, and functional performance in older adults post-COVID-19: A randomized controlled trial. J. Phys. Ther. Clin. Pract. 2023, 30. [Google Scholar] [CrossRef]
- Espinoza-Bravo, C.; Arnal-Gómez, A.; Martínez-Arnau, F.M.; Núñez-Cortés, R.; Hernández-Guillén, D.; Flor-Rufino, C.; Cortes-Amador, S. Effectiveness of functional or aerobic exercise combined with breathing techniques in telerehabilitation for patients with long COVID: A randomized controlled trial. Phys. Ther. 2023, 103, pzad118. [Google Scholar] [CrossRef] [PubMed]
- Hasenoehrl, T.; Palma, S.; Huber, D.F.X.; Kastl, S.; Steiner, M.; Jordakieva, G.; Crevenna, R. Post-COVID: Effects of physical exercise on functional status and work ability in health care personnel. Disabil. Rehabil. 2023, 45, 2872–2878. [Google Scholar] [CrossRef]
- Ogonowska-Slodownik, A.; Labecka, M.K.; Maciejewska-Skrendo, A.; McNamara, R.J.; Kaczmarczyk, K.; Starczewski, M.; Gajewski, J.; Morgulec-Adamowicz, N. Effect of water-based vs. land-based exercise intervention (postCOVIDkids) on exercise capacity, fatigue, and quality of life in children with post-COVID-19 condition: A randomized controlled trial. J. Clin. Med. 2023, 12, 6244. [Google Scholar] [CrossRef]
- De La Plaza San Frutos, M.; Abuín Porras, V.; Blanco Morales, M.; Arrabé, M.G.; Estrada Barranco, C.; Rubio Alonso, M. Telemedicine in pulmonary rehabilitation—Benefits of a telerehabilitation program in post-COVID-19 patients: A controlled quasi-experimental study. Ther. Adv. Respir Dis. 2023, 17, 175346662311673. [Google Scholar] [CrossRef]
- Smith, J.L.; Deighton, K.; Innes, A.Q.; Holl, M.; Mould, L.; Liao, Z.; Doherty, P.; Whyte, G.; King, J.; Deniszczyc, D.; et al. Improved clinical outcomes in response to a 12-week blended digital and community-based long-COVID-19 rehabilitation programme. Front. Med. 2023, 10, 1149922. [Google Scholar] [CrossRef] [PubMed]
- Torres, G.; Rains, N.; Gradidge, P.; Constantinou, D. Exercise intervention for post-acute COVID-19 syndrome—Do FITT-VP principles apply? A case study. S. Afr J. Sports Med. 2023, 35. [Google Scholar] [CrossRef] [PubMed]
- Wahyuni, L.K.; Harini, M.; Sunarjo, P.; Ramadhany, M.; Fitriana, I.; Hidemi, O.; Wijayanti, I.; Tedjasukmana, D.; Tamin, T.T. The influence and feasibility of therapeutic exercise videos at home on the functional status of post-COVID-19 hospitalization. Kesmas J. Natl. Public Health 2023, 18 (Suppl. S1), 43. [Google Scholar] [CrossRef]
- Araújo, B.T.S.; Barros, A.E.V.R.; Nunes, D.T.X.; Remígio De Aguiar, M.I.; Mastroianni, V.W.; De Souza, J.A.F.; Fernades, J.; Campos, S.L.; Brandão, D.C.; Dornelas de Andrade , A. Effects of continuous aerobic training associated with resistance training on maximal and submaximal exercise tolerance, fatigue, and quality of life of patients post-COVID-19. Physiother. Res. Int. 2023, 28, e1972. [Google Scholar] [CrossRef]
- Binetti, J.; Real, M.; Renzulli, M.; Bertran, L.; Riesco, D.; Perpiñan, C.; Mohedano, A.; Segundo, R.S.; Ortiz, M.; Porras, J.A.; et al. Clinical and Biomarker Profile Responses to Rehabilitation Treatment in Patients with Long COVID Characterized by Chronic Fatigue. Viruses 2023, 15, 1452. [Google Scholar] [CrossRef]
- Calvo-Paniagua, J.; Díaz-Arribas, M.J.; Valera-Calero, J.A.; Gallardo-Vidal, M.I.; Fernández-de-las-Peñas, C.; López-de-Uralde-Villanueva, I.; Corral, T.; Plaza-Manzano, G. A tele-health primary care rehabilitation program improves self-perceived exertion in COVID-19 survivors experiencing Post-COVID fatigue and dyspnea: A quasi-experimental study. PLoS ONE 2022, 17, e0271802. [Google Scholar] [CrossRef]
- Campos, M.C.; Nery, T.; Speck, A.E.; Arpini, M.; Antunes, M.M.; de Bem Alves, A.C.; Diefenthaeler, F.; Kuriki, H.U.; Damin, V.; Da Rosa, R.O.; et al. Rehabilitation in Survivors of COVID-19 (RE2SCUE): A non-randomized, controlled and open study. medRxiv 2022. [Google Scholar] [CrossRef]
- Chikina, S.Y.; Kuleshov, A.V.; Nikitina, N.V.; Meshcheryakova, N.N. Effects of physical rehabilitation on exercise tolerance in post-COVID patients: Results of an open controlled trial. Pulʹmonologiâ 2022, 32, 728–736. [Google Scholar] [CrossRef]
- Colas, C.; Bayle, M.; Labeix, P.; Botelho-Nevers, E.; Gagneux-Brunon, A.; Cazorla, C.; Schein, F.; Breugnon, E.; Garcin, A.; Feasson, L.; et al. Management of Long COVID—The CoviMouv’ Pilot Study: Importance of Adapted Physical Activity for Prolonged Symptoms Following SARS-CoV2 Infection. Front. Sports Act. Living 2022, 4, 877188. [Google Scholar] [CrossRef] [PubMed]
- Compagno, S.; Palermi, S.; Pescatore, V.; Brugin, E.; Sarto, M.; Marin, R.; Calzavara, V.; Nizzetto, M.; Scevola, M.; Aloi, A.; et al. Physical and psychological reconditioning in long COVID syndrome: Results of an out-of-hospital exercise and psychological-based rehabilitation program. IJC Heart Vasc. 2022, 41, 101080. [Google Scholar] [CrossRef]
- Jimeno-Almazán, A.; Franco-López, F.; Buendía-Romero, Á.; Martínez-Cava, A.; Sánchez-Agar, J.A.; Sánchez-Alcaraz Martínez, B.J.; Courel-Ibáñez, J.; Pallarés, G. Rehabilitation for post-COVID-19 condition through a supervised exercise intervention: A randomized controlled trial. Scand. J. Med. Sci. Sports 2022, 32, 1791–1801. [Google Scholar] [CrossRef]
- Jimeno-Almazán, A.; Buendía-Romero, Á.; Martínez-Cava, A.; Franco-López, F.; Sánchez-Alcaraz, B.J.; Courel-Ibáñez, J.; Pallares, J. Effects of a concurrent training, respiratory muscle exercise, and self-management recommendations on recovery from post-COVID-19 conditions: The RECOVE trial. J. Appl. Physiol. 2023, 134, 95–104. [Google Scholar] [CrossRef]
- Longobardi, I.; Prado, D.M.L.D.; Goessler, K.F.; Oliveira Júnior, G.N.D.; De Andrade, D.C.O.; Gualano, B.; Roschel, H. Benefits of Home-Based Exercise Training Following Critical SARS-CoV-2 Infection: A Case Report. Front. Sports Act. Living 2022, 3, 791703. [Google Scholar] [CrossRef]
- Márquez-Silva, S.; Eslava-Osorio, O.; Valencia-Melo, S.; Patricio-Rafael, E. Application of a therapeutic exercise program to improve physical condition in patients with post-COVID-19 syndrome. J. Nutr. Therapeutics. 2022, 1–8. [Google Scholar] [CrossRef]
- Sari, F.; Bayram, S.; Pala, G.G.; Çömçe, F.; Küçük, H.; Oskay, D. Effects of Inspiratory Muscle Training in Patients with post-COVID-19. Harran Univ. Tip Fak Derg. 2022, 19, 581–588. [Google Scholar] [CrossRef]
- Takekawa, T.; Kashiwabara, K.; Yamada, N.; Watanabe, S.; Hama, M.; Hashimoto, G.; Abo, M.; Shinfuku, K. Rehabilitation therapy for a severe case of coronavirus disease 2019: A case report. J. Med. Case Rep. 2022, 16, 339. [Google Scholar] [CrossRef] [PubMed]
- Mayer, K.P.; Steele, A.K.; Soper, M.K.; Branton, J.D.; Lusby, M.L.; Kalema, A.G.; Dupont-Versteegden, E.; Montgomery-Yates, A.A. Physical Therapy Management of an Individual With Post-COVID Syndrome: A Case Report. Phys. Ther. 2021, 101, pzab098. [Google Scholar] [CrossRef]
- Stavrou, V.T.; Tourlakopoulos, K.N.; Vavougios, G.D.; Papayianni, E.; Kiribesi, K.; Maggoutas, S.; Nikolaidis, K.; Fradelos, E.C.; Dimeas, I.; Daniil, Z.; et al. Eight Weeks Unsupervised Pulmonary Rehabilitation in Previously Hospitalized of SARS-CoV-2 Infection. J. Pers. Med. 2021, 11, 806. [Google Scholar] [CrossRef]
- Chuang, Y.C.; Lin, K.P.; Wang, L.A.; Yeh, T.K.; Liu, P.Y. The impact of the COVID-19 pandemic on respiratory syncytial virus infection: A narrative review. Infect Drug Resist. 2023, 16, 661–675. [Google Scholar] [CrossRef]
- Daynes, E.; Gerlis, C.; Chaplin, E.; Gardiner, N.; Singh, S.J. Early experiences of rehabilitation for individuals post-COVID to improve fatigue, breathlessness exercise capacity and cognition—A cohort study. Chron. Respir. Dis. 2021, 18, 147997312110156. [Google Scholar] [CrossRef] [PubMed]
- Nantakool, S.; Sa-nguanmoo, P.; Konghakote, S.; Chuatrakoon, B. Effects of exercise rehabilitation on cardiorespiratory fitness in long-COVID-19 survivors: A meta-analysis. J. Clin. Med. 2024, 13, 3621. [Google Scholar] [CrossRef]
- Dantzer, R. Neuroimmune interactions: From the brain to the immune system and vice versa. Physiol. Rev. 2018, 98, 477–504. [Google Scholar] [CrossRef]
- Phetsouphanh, C.; Darley, D.R.; Wilson, D.B.; Howe, A.; Munier, C.M.L.; Patel, S.K.; Juno, J.; Burrel, L.; Kent, S.; Dore, G.; et al. Immunological dysfunction persists for 8 months following initial mild-to-moderate SARS-CoV-2 infection. Nat. Immunol. 2022, 23, 210–216. [Google Scholar] [CrossRef]
- Pouliopoulou, D.V.; Macdermid, J.C.; Saunders, E.; Peters, S.; Brunton, L.; Miller, E. Rehabilitation interventions for physical capacity and quality of life in adults with post–COVID-19 condition: A systematic review and meta-analysis. JAMA Netw. Open 2023, 6, e2333838. [Google Scholar] [CrossRef]
- Beaumont, M.; Mialon, P.; Le Ber, C.; Le Mevel, P.; Péran, L.; Meurisse, O.; Morelot-Panzini, C.; Dion, A.; Couturaud, F. Effects of inspiratory muscle training on dyspnoea in severe COPD patients during pulmonary rehabilitation: Controlled randomised trial. Eur. Respir. J. 2018, 51, 1701107. [Google Scholar] [CrossRef]
- Prabawa, I.M.Y.; Silakarma, D.; Manuaba, I.B.A.P.; Widnyana, M.; Jeviana, A. Chest therapy and breathing exercise in COVID-19 patient: A case report. Bali Med. J. 2021, 10, 495–498. [Google Scholar] [CrossRef]
- Sousa, O.A.; Gomide, E.; Mazzonetto, L.; Marchiori, G.; Cordeiro, J.; Tasinafo-Junior, M.; da Silva, L.; Venturini, A.; Moraes, C.; Mota, J.; et al. Impact of COVID-19 on physical activity, sedentary behavior, and general health status in adults and older adults: A retrospective observational study. Motricidade 2025, 21, e33549. [Google Scholar] [CrossRef]
- Mazzonetto, L.; Gomide, E.; Oliveira, A.; da Silva, L.; Cordeiro, J.; Abdalla, P.; Tasinafo Junior, M.; Venturini, A.; Trapá, A.; Mota, J.; et al. Increased risk for signs and clinical symptoms associated with sedentary behaviour in people diagnosed with COVID-19: A retrospective observational study. Motricidade 2024, 20. [Google Scholar] [CrossRef]
- Baldassano, S.; Alioto, A.; Amato, A.; Rossi, C.; Messina, G.; Bruno, M.R.; Stallone, R.; Proia, P. Fighting the Consequences of the COVID-19 Pandemic: Mindfulness, Exercise, and Nutrition Practices to Reduce Eating Disorders and Promote Sustainability. Sustainability 2023, 15, 2120. [Google Scholar] [CrossRef]



| Database | Search Strategy | Number of Studies Found |
|---|---|---|
| PubMed | (“Post-Acute COVID-19 Syndrome[Mesh]” OR “COVID-19 Syndrome, Post-Acute” OR “Post-Acute COVID-19 Syndromes” OR “Long Haul COVID-19” OR “COVID-19, Long Haul” OR “Long Haul COVID 19” OR “Long Haul COVID-19s” OR “Post Acute COVID-19 Syndrome” OR “Post Acute COVID 19 Syndrome” OR “Long COVID” OR “Post-Acute Sequelae of SARS-CoV-2 Infection” OR “Post Acute Sequelae of SARS-CoV 2 Infection” OR “Post-COVID Conditions” OR “Post COVID Conditions” OR “Post-COVID Condition” OR “Long-Haul COVID” OR “COVID, Long-Haul” OR “Long Haul COVID” OR “Long-Haul COVIDs”) AND (Exercise [Mesh] OR Exercises OR “Physical Activity” OR “Activities, Physical” OR “Activity, Physical” OR “Exercise, Physical” OR “Exercises, Physical” OR “Physical Exercise” OR “Physical Exercises” OR “Acute Exercise” OR “Acute Exercises” OR “Exercise, Acute” OR “Exercises, Acute” OR “Exercise, Isometric” OR “Exercises, Isometric” OR “Isometric Exercises” OR “Isometric Exercise” OR “Exercise, Aerobic” OR “Aerobic Exercise” OR “Aerobic Exercises” OR “Exercises, Aerobic” OR “Exercise Training” OR “Exercise Trainings” OR “Training, Exercise” OR “Trainings, Exercise”) AND (Fatigue [Mesh] OR Lassitude OR Dyspnea OR “Shortness of Breath” OR “Breath Shortness” OR Breathlessness OR Orthopnea OR “Recumbent Dyspnea” OR “Dyspnea, Recumbent” OR “Platypnea” OR Trepopnea OR “Rest Dyspnea” OR “Dyspnea, Rest” OR “Dyspneas, Rest”) | 260 |
| Web of Science | (“Post-Acute COVID-19 Syndrome” OR “COVID-19 Syndrome, Post-Acute” OR “Post-Acute COVID-19 Syndromes” OR “Long Haul COVID-19” OR “COVID-19, Long Haul” OR “Long Haul COVID 19” OR “Long Haul COVID-19s” OR “Post Acute COVID-19 Syndrome” OR “Post Acute COVID 19 Syndrome” OR “Long COVID” OR “Post-Acute Sequelae of SARS-CoV-2 Infection” OR “Post Acute Sequelae of SARS-CoV 2 Infection” OR “Post-COVID Conditions” OR “Post COVID Conditions” OR “Post-COVID Condition” OR “Long-Haul COVID” OR “COVID, Long-Haul” OR “Long Haul COVID” OR “Long-Haul COVIDs”) AND (Exercise OR Exercises OR “Physical Activity” OR “Activities, Physical” OR “Activity, Physical” OR “Exercise, Physical” OR “Exercises, Physical” OR “Physical Exercise” OR “Physical Exercises” OR “Acute Exercise” OR “Acute Exercises” OR “Exercise, Acute” OR “Exercises, Acute” OR “Exercise, Isometric” OR “Exercises, Isometric” OR “Isometric Exercises” OR “Isometric Exercise” OR “Exercise, Aerobic” OR “Aerobic Exercise” OR “Aerobic Exercises” OR “Exercises, Aerobic” OR “Exercise Training” OR “Exercise Trainings” OR “Training, Exercise” OR “Trainings, Exercise”) AND (Fatigue OR Lassitude OR Dyspnea OR “Shortness of Breath” OR “Breath Shortness” OR Breathlessness OR Orthopnea OR “Recumbent Dyspnea” OR “Dyspnea, Recumbent” OR “Platypnea” OR Trepopnea OR “Rest Dyspnea” OR “Dyspnea, Rest” OR “Dyspneas, Rest”) | 219 |
| Embase | (‘post-acute COVID-19 syndrome’/exp OR ‘post-acute COVID-19 syndrome’ OR ‘COVID-19 syndrome, post-acute’ OR ‘post-acute COVID-19 syndromes’ OR ‘long haul COVID-19’/exp OR ‘long haul COVID-19’ OR ‘COVID-19, long haul’ OR ‘long haul COVID 19’/exp OR ‘long haul COVID 19’ OR ‘long haul COVID-19s’ OR ‘post acute COVID-19 syndrome’/exp OR ‘post acute COVID-19 syndrome’ OR ‘post acute COVID 19 syndrome’/exp OR ‘post acute COVID 19 syndrome’ OR ‘long COVID’/exp OR ‘long COVID’ OR ‘post-acute sequelae of SARS-CoV-2 infection’/exp OR ‘post-acute sequelae of SARS-CoV-2 infection’ OR ‘post acute sequelae of SARS-CoV 2 infection’/exp OR ‘post acute sequelae of SARS-CoV 2 infection’ OR ‘post-COVID conditions’ OR ‘post COVID conditions’ OR ‘post-COVID condition’/exp OR ‘post-COVID condition’ OR ‘long-haul COVID’/exp OR ‘long-haul COVID’ OR ‘COVID, long-haul’ OR ‘long haul COVID’/exp OR ‘long haul COVID’ OR ‘long-haul COVIDS’) AND (‘exercise’/exp OR exercise OR exercises OR ‘physical activity’/exp OR ‘physical activity’ OR ‘activities, physical’ OR ‘activity, physical’/exp OR ‘activity, physical’ OR ‘exercise, physical’ OR ‘exercises, physical’ OR ‘physical exercise’/exp OR ‘physical exercise’ OR ‘physical exercises’ OR ‘acute exercise’/exp OR ‘acute exercise’ OR ‘acute exercises’ OR ‘exercise, acute’ OR ‘exercises, acute’ OR ‘exercise, isometric’/exp OR ‘exercise, isometric’ OR ‘exercises, isometric’ OR ‘isometric exercises’ OR ‘isometric exercise’/exp OR ‘isometric exercise’ OR ‘exercise, aerobic’/exp OR ‘exercise, aerobic’ OR ‘aerobic exercise’/exp OR ‘aerobic exercise’ OR ‘aerobic exercises’ OR ‘exercises, aerobic’ OR ‘exercise training’/exp OR ‘exercise training’ OR ‘exercise trainings’ OR ‘training, exercise’ OR ‘trainings, exercise’) AND (‘fatigue’/exp OR fatigue OR ‘lassitude’/exp OR lassitude OR ‘dyspnea’/exp OR dyspnea OR ‘shortness of breath’/exp OR ‘shortness of breath’ OR ‘breath shortness’ OR ‘breathlessness’/exp OR breathlessness OR ‘orthopnea’/exp OR orthopnea OR ‘recumbent dyspnea’ OR ‘dyspnea, recumbent’ OR ‘platypnea’/exp OR ‘platypnea’ OR trepopnea OR ‘rest dyspnea’ OR ‘dyspnea, rest’ OR ‘dyspneas, rest’) | 904 |
| Scopus | (“Post-Acute COVID-19 Syndrome” OR “COVID-19 Syndrome, Post-Acute” OR “Post-Acute COVID-19 Syndromes” OR “Long Haul COVID-19” OR “COVID-19, Long Haul” OR “Long Haul COVID 19” OR “Long Haul COVID-19s” OR “Post Acute COVID-19 Syndrome” OR “Post Acute COVID 19 Syndrome” OR “Long COVID” OR “Post-Acute Sequelae of SARS-CoV-2 Infection” OR “Post Acute Sequelae of SARS-CoV 2 Infection” OR “Post-COVID Conditions” OR “Post COVID Conditions” OR “Post-COVID Condition” OR “Long-Haul COVID” OR “COVID, Long-Haul” OR “Long Haul COVID” OR “Long-Haul COVIDs”) AND (Exercise OR Exercises OR “Physical Activity” OR “Activities, Physical” OR “Activity, Physical” OR “Exercise, Physical” OR “Exercises, Physical” OR “Physical Exercise” OR “Physical Exercises” OR “Acute Exercise” OR “Acute Exercises” OR “Exercise, Acute” OR “Exercises, Acute” OR “Exercise, Isometric” OR “Exercises, Isometric” OR “Isometric Exercises” OR “Isometric Exercise” OR “Exercise, Aerobic” OR “Aerobic Exercise” OR “Aerobic Exercises” OR “Exercises, Aerobic” OR “Exercise Training” OR “Exercise Trainings” OR “Training, Exercise” OR “Trainings, Exercise”) AND (Fatigue OR Lassitude OR Dyspnea OR “Shortness of Breath” OR “Breath Shortness” OR Breathlessness OR Orthopnea OR “Recumbent Dyspnea” OR “Dyspnea, Recumbent” OR “Platypnea” OR Trepopnea OR “Rest Dyspnea” OR “Dyspnea, Rest” OR “Dyspneas, Rest”) | 473 |
| LILACS | (“Post-Acute COVID-19 Syndrome” OR “COVID-19 Syndrome, Post-Acute” OR “Post-Acute COVID-19 Syndromes” OR “Long Haul COVID-19” OR “COVID-19, Long Haul” OR “Long Haul COVID 19” OR “Long Haul COVID-19s” OR “Post Acute COVID-19 Syndrome” OR “Post Acute COVID 19 Syndrome” OR “Long COVID” OR “Post-Acute Sequelae of SARS-CoV-2 Infection” OR “Post Acute Sequelae of SARS-CoV 2 Infection” OR “Post-COVID Conditions” OR “Post COVID Conditions” OR “Post-COVID Condition” OR “Long-Haul COVID” OR “COVID, Long-Haul” OR “Long Haul COVID” OR “Long-Haul COVIDs”) AND (Exercise OR Exercises OR “Physical Activity” OR “Activities, Physical” OR “Activity, Physical” OR “Exercise, Physical” OR “Exercises, Physical” OR “Physical Exercise” OR “Physical Exercises” OR “Acute Exercise” OR “Acute Exercises” OR “Exercise, Acute” OR “Exercises, Acute” OR “Exercise, Isometric” OR “Exercises, Isometric” OR “Isometric Exercises” OR “Isometric Exercise” OR “Exercise, Aerobic” OR “Aerobic Exercise” OR “Aerobic Exercises” OR “Exercises, Aerobic” OR “Exercise Training” OR “Exercise Trainings” OR “Training, Exercise” OR “Trainings, Exercise”) AND (Fatigue OR Lassitude OR Dyspnea OR “Shortness of Breath” OR “Breath Shortness” OR Breathlessness OR Orthopnea OR “Recumbent Dyspnea” OR “Dyspnea, Recumbent” OR “Platypnea” OR Trepopnea OR “Rest Dyspnea” OR “Dyspnea, Rest” OR “Dyspneas, Rest”) | 222(2) |
| EBSCO * | (“Post-Acute COVID-19 Syndrome” OR “COVID-19 Syndrome, Post-Acute” OR “Post-Acute COVID-19 Syndromes” OR “Long Haul COVID-19” OR “COVID-19, Long Haul” OR “Long Haul COVID 19” OR “Long Haul COVID-19s” OR “Post Acute COVID-19 Syndrome” OR “Post Acute COVID 19 Syndrome” OR “Long COVID” OR “Post-Acute Sequelae of SARS-CoV-2 Infection” OR “Post Acute Sequelae of SARS-CoV 2 Infection” OR “Post-COVID Conditions” OR “Post COVID Conditions” OR “Post-COVID Condition” OR “Long-Haul COVID” OR “COVID, Long-Haul” OR “Long Haul COVID” OR “Long-Haul COVIDs”) AND (Exercise OR Exercises OR “Physical Activity” OR “Activities, Physical” OR “Activity, Physical” OR “Exercise, Physical” OR “Exercises, Physical” OR “Physical Exercise” OR “Physical Exercises” OR “Acute Exercise” OR “Acute Exercises” OR “Exercise, Acute” OR “Exercises, Acute” OR “Exercise, Isometric” OR “Exercises, Isometric” OR “Isometric Exercises” OR “Isometric Exercise” OR “Exercise, Aerobic” OR “Aerobic Exercise” OR “Aerobic Exercises” OR “Exercises, Aerobic” OR “Exercise Training” OR “Exercise Trainings” OR “Training, Exercise” OR “Trainings, Exercise”) AND (Fatigue OR Lassitude OR Dyspnea OR “Shortness of Breath” OR “Breath Shortness” OR Breathlessness OR Orthopnea OR “Recumbent Dyspnea” OR “Dyspnea, Recumbent” OR “Platypnea” OR Trepopnea OR “Rest Dyspnea” OR “Dyspnea, Rest” OR “Dyspneas, Rest”) | 478 |
| Google scholar | (Post-Acute COVID-19 Syndrome) AND (exercise) AND (fatigue OR dyspnea) | 100 |
| medRxiv | (Post-Acute COVID-19 Syndrome) AND (exercise) AND (fatigue OR dyspnea) | 584 |
| References | Objective | Types of Intervention | Effects on Fatigue | Effects on Dyspnea |
|---|---|---|---|---|
| Vieira Da Costa et al., 2023. Brazil [11] | To evaluate the effectiveness of a rehabilitation protocol on pulmonary and respiratory muscles and the thickness of the quadriceps femoris and diaphragm in patients with post-COVID-19 syndrome. | RMT + Strength Training + Aerobic 6 weeks. RMT: 3 × 10 at 40% inspiratory pressure load; Strength training 2× per week; Anterior Elevation 3 × 1 min pause 1 min. Aerobic: Treadmill at 60–70% and 70–80% of max HR. | ↔ | NA |
| Dumitrescu et al., 2023. Romania [12] | To assess the impact of COVID-19 on cardiopulmonary health and the effectiveness of various rehabilitation interventions. This study hypothesizes that post-COVID-19 patients present distinct characteristics and recovery dynamics that significantly influence their response to specific rehabilitation interventions. | Aerobic + RMT + Strength Training 3 months. Aerobic: starting with a bike at 40–50% max effort 3× per week, gradually adding walking; frequency increased to 5× and intensity varied based on individual responses, such as HIIT application. RMT: guided coughing exercises and drainage posture (airway clearance and mucus removal). Strength training: 2× per week with 1–2 kg weights and low elasticity resistance bands (increasing gradually to 3–4× per week). Flexibility 2–3× per week. | NA | ↔ |
| Elhamrawy et al., 2023. Egypt [13] | To understand the impact of Tai Chi versus aerobic training on fatigue and functional performance in elderly post-COVID. | Tai Chi (TC) or Aerobic 3 months. TC: 4× per week for 60 min; 10′ warm-up; 40′ main session; 10′ relaxation: 7 TC movements: controlled weight shifting, ankle swings, and forward-backward and lateral steps (4–6 Borg Scale). Aerobic: 4× per week for 60 min; warm-up: 10′ static stretches targeting the trunk and limbs; 20′ general muscle strengthening with 5 kg; Treadmill walking for 15–20 min at moderate effort of 12–26 km/h; 10′ relaxation. | ↑ ↑ | NA |
| Espinoza-Bravo et al., 2023. Spain [14] | To compare the clinical effects of two tele-rehabilitation programs on long COVID symptoms. | Functional + RMT or Aerobic + RMT 3× per week for 8 weeks. App: https://fisiotrack.com/ (accessed on 5 January 2025) Functional: Squats, lateral squats, hip lifts, bench press, and rowing; 2–3× 10 reps. 1′ pause; 4–6 exercises, increasing difficulty every 2 weeks. Aerobic: progressive walking with weekly load adjustments from 25′ to 45′ (25′ in week 1 to 45′ in week 8). Walking pace allowed maintaining a fluid conversation. RMT: diaphragmatic and pursed-lip breathing 5× per week, 3 × 15 reps. | ↑ ↑ | NA |
| Hasenoehrl et al., 2023. Áustria [15] | To assess the effects of physical exercise on post-COVID-19 symptoms on physical/mental abilities and work capacity within a workplace health promotion project among healthcare workers. | Strength Training + Aerobic Strength training: 2× training sessions over 8 weeks supervised, circuit training with body weight and resistance bands, including 8 full-body exercises. Squats, glute bridges, hip walks, back extensions at 45°, push-ups, low row, planks, and shoulder external rotations with varying difficulty levels based on fitness. Starting with 30″ exercise and 30″ pause, progressing every 2 weeks by adding 10″ until reaching 1′/1′. Initial PSE 7–8 and from week 3 PSE 9–10. Aerobic: unsupervised aerobic exercises—recommendations: at least 3× 20′ of moderate exercise per week at LV1. Note: Severe cases showed better levels of improvement compared to mild cases. Note 2: PCFS corrected by Bonferroni method shows strong association between relative VO2 peak, 30-s STS, and 6MWT. | ↑ | NA |
| Ogonowska-Slodownik et al., 2023. Poland [16] | To analyze the effectiveness of water- and land-based training programs on exercise capacity, fatigue, and secondary outcomes on health-related quality of life in children with post-COVID-19 condition. | Aerobic or Aquatic 2× for 8 weeks, 45′. Warm-up: 8′ and relaxation at the end for 5′. Aquatic: Punch, kick, stationary running, and breath control. Aerobic: 2 circuit stations, each with 5 stations with different resistance exercises for upper and lower limbs, 1′ exercise and 15″ pause. Intensity 6–8 on the Pictorial scale. Aquatic and land exercises were combined as closely as possible in terms of intensity, duration, and muscle groups trained. (No significant differences were found in total fatigue level and individual fatigue symptoms). | ↔ ↔ | NA |
| De La Plaza San Frutos et al., 2023. Spain [17] | To evaluate the outcomes of a tele-respiratory rehabilitation program in post-COVID-19 patients ranging from mild to critical COVID-19 without vaccination. | RMT + Stretching RMT: 10 online sessions with diaphragmatic breathing: costal expansion, flexion, and abduction of upper limbs; active respiratory cycle; yoga-based breathing exercises and progressive muscle relaxation. Stretching: specific for neck and thoracic muscles. | NA | ↑ |
| Smith et al., 2023. Europe, África e Ásia [18] | To evaluate the clinical efficacy of a new 12-week combined community rehabilitation program for individuals with long COVID. | Programa Nuffield Health: www.nuffieldhealth.com/covid-rehab (accessed on 5 January 2025) Nuffield Health Program: Participants used a diary to record exercises and progress. Exercises: 12 weeks (6 weeks remote and 6 weeks in-person in a community setting), 3 × 45 min per week (36 total) including a combination of cardiovascular, strength, and mobility exercises. Exercise intensity, volume, movement complexity, range of motion, and stability were prescribed according to participants’ functional capacity and fitness. Weekly distribution: Week 1 cardio; Week 7 cardio; Week 2 mobility; Week 8 mobility; Week 3 strength; Week 9 strength; Week 4 mobility; Week 10 mobility; Week 5 cardio; Week 11 strength; Week 6 strength; Week 12 cardio. | NA | ↑ |
| Torres et al., 2023. South Africa [19] | To help standardize exercise for post-COVID (applying the CERT by describing the 16 essential items). | Multicomponent Aerobic: 3× per week for 7–10′. Progression: increase by 1–2′ each week and PSE 6–11 (gradually). Strength Training: 1× 4–8 reps on equipment (add 2 reps every week, and when reaching 10 reps, add 1 exercise and 1 set each week until 3 × 10 reps). Balance exercises; flexibility exercises (2–4 exercises based on HR, dyspnea level, technique, symptoms for sedentary/beginners). | ↔ | ↔ |
| Wahyuni et al., 2023. Indonesia [20] | To analyze the effect of educational videos on therapeutic exercises on the functional status of subjects after hospitalization for COVID-19. | Strength Training Basic Strength and Balance Exercises: 2–3 times per day with 5–10 reps for each movement. Phase 1: seated: Strengthening and balance. Phase 2: Squat (sit-to-stand and gait alignment or assistance). | ↔ | NA |
| Araújo et al., 2022. Brazil [21] | To verify the effects of a cardiopulmonary rehabilitation program consisting of continuous moderate-intensity aerobic and resistance training on pulmonary function, respiratory muscle strength, maximal and submaximal exercise tolerance, fatigue, and quality of life in post-COVID-19 patients. | Aerobic + Strength Training Aerobic: 40′ on treadmill, 5′ warm-up; 30′ conditioning; 5′ relaxation. Strength Training: 2× per week, 3× 8–12 reps. Biceps, triceps, shoulder abductors; quadriceps, hip abductors, and calf muscles. 60% of 1RM with progression at the 6th session. A total of 12 sessions. | ↔ | NA |
| Binetti et al., 2022. Spain [22] | To analyze the impact of a supervised exercise program on the clinical evolution of long COVID patients with persistent fatigue as the main symptom and to identify whether specific blood biomarkers could predict rehabilitation response in a cohort from a high-prevalence area. | Aerobic + Strength Training (Upper Limbs) 3 months with 12–20 supervised physiotherapy sessions; Warm-up: 5–10′ stretching and light exercises; Main: aerobic on bike starting at 10′ progressing to 30′. Intensity according to effort and tolerance based on HR. 1× per week upper limb muscle strengthening exercises. | ↔ | ↔ |
| Calvo-Paniagua et al., 2022. Spain [23] | To analyze whether a tele-rehabilitation program can improve self-perception of physical exertion in patients with post-COVID fatigue and dyspnea. | Aerobic + Active Mobilizations and Motor Control + Respiratory Muscle Training (RMT) RMT: airway clearance exercises and respiratory exercises (in all sessions). 3 months with 18 sessions, 3× per week, 40′ on alternate days via videoconference (Zoom). Session 1: Postural Ergonomics; Session 2–5 RMT: diaphragmatic breathing, costal breathing, pursed-lip breathing, and airway clearance; Session 6–8: Physical conditioning with increasing intensity: active mobilizations of the cervical, dorsal, and lumbar spine, active mobilizations of lower and upper limbs + core training with motor control exercises; Session 9: Balance + Dynamic control seated exercises + gait exercises; Session 10–11: functional exercises and plyometric exercises + occupational therapy for daily activities; Session 12–18: functional exercises + occupational therapy + aerobic training: walking at a tolerable speed. | NA | ↑ |
| Campos et al., 2022. Brazil [24] | To evaluate the effects of an 8-week in-person rehabilitation program for COVID-19 on fatigue and dyspnea, exercise capacity, pulmonary function, cognitive function, anxiety and depression symptoms, and peripheral muscle strength compared to a remote monitoring group. | RMT + Aerobic + Strength Training + Stretching 8 weeks, 2× per week, 80′. RMT: respiratory exercises, energy conservation techniques. Aerobic: Treadmill at 75% Borg speed of 4–6. Warm-up: 5′ and 30′ at target intensity (moderate). Strength Training: 80% of 1RM with 3 × 10 reps, 1–2′ pause for upper and lower limbs. Stretching: muscles trained were stretched. | ↑ | ↑ |
| Chikina et al., 2022. Russia [25] | To investigate the effectiveness of physical rehabilitation in treating post-COVID syndrome in patients with lung injuries caused by coronavirus infection. | RMT + Strength Training + Aerobic RMT: Loaded breathing and positive expiratory pressure breathing (respiratory simulators). Strength Training: Exercises with a gym stick, elastic bands, and 0.5–2 kg dumbbells. Aerobic: Stepper (walking simulator). | NA | ↑ |
| Colas et al., 2022. France [26] | To evaluate fatigue in patients with prolonged symptoms after COVID-19 infection who received a mixed program of adapted physical activity remotely and therapeutic education. The secondary aim was to assess the efficacy and safety of this training method through aerobic and anaerobic parameters. | Aerobic + Strength Training or RMT Aerobic: 12 sessions; 3× per week; 45′ with the first week in-person and subsequent sessions online (training at ventilatory threshold 1 (VT1) with progression to VT2 on a cycle ergometer from week 4 interval training. Strength Training: 15′ full-body circuit with body weight, with light to moderate intensity according to the Borg scale. Note: Exercise was stopped if the heart rate was >80% max HR (vigorous exercise) and/or if the perceived effort was >6/10 on the Borg scale. RMT: Traditional community physical rehabilitation 3× per week for 4 weeks. | ↑ ↑ | NA |
| Compagno et al., 2022. Italy [27] | To evaluate the efficacy, safety, and feasibility of an out-of-hospital multidisciplinary rehabilitation program (MDR) based on physical and psychological reconditioning to reduce symptoms and improve fitness and psychological parameters in long COVID patients. | ACSM Program + RMT based on meditation Training 3× per week for 90′ (10′ mixed warm-up + 45′ main session (strength training + 35′ aerobic and 5′ relaxation). RMT: muscle relaxation techniques, breath control, and guided relaxation. Aerobic: cycle ergometer and continuous treadmill moderate (60–80% VO2 peak). Strength Training: performed with variable loads of 30 to 50% of 1RM (pectoral, lumbar, leg press, leg extension, adductor machine, and deltoids). Stretching: at the end as relaxation. | ↑ | ↑ |
| Jimeno-Almazán et al., 2022 Spain [28] | Determine the effectiveness of physical exercise, respiratory muscle training, and the World Health Organization (WHO) self-management recommendation leaflet on recovery of physical fitness, quality of life, and symptoms. | Concurrent Training (CT)—Strength Training + Aerobic or RMT or Concurrent Training + RMT or WHO Guidelines CT: 8 weeks, 3 sessions per week, 2× Strength training: 3 × 8 repetitions, 4 exercises squats, bench press, deadlifts and bench pulls. 50% RM constant programming model—intra-set intensity and volume kept constant throughout the training plan. Strength training was combined with moderate-intensity variable aerobic training (MIVT: 4–6 × 3–5 min at 70–80% heart rate reserve [HRR]/2–3 min at 55–65% of FCR) TMR: Inspiratory muscle training with PowerBreath Classic Heath Series Mechanical Threshold Devices 1 set of 30 repetitions [62.5 ± 4.6% of IMP (Maximum Inspiratory Pressure)], preceded by a warm-up set twice daily, all the days of the week TC + TMR: the combination of the previous protocols. WHO: Controlled breathing, light walking, stretching and balance exercises (Borg 0–1). Phase 2: Add light daily household chores (Borg 2–3). Phase 3: brisk walking, going up and down stairs and running for up to 30′ adding 15′ strength exercises (Borg 4–5). Phase 4: moderate intensity exercises with coordination and skill in running, cycling, swimming and dancing (Borg 5–7). Phase 5: the participant returned to their usual routine (Borg 8–10). | ↑ ↔ ↑ ↔ | ↑ ↔ ↑ ↓ |
| Jimeno-Almazán et al., 2022 Spain [29] | Compare the outcomes of patients with post-COVID-19 condition undergoing supervised therapeutic exercise intervention or following the WHO (World Health Organization) self-management rehabilitation leaflet. | Concurrent Training (CT)—Strength Training + Aerobic or WHO Guidelines post-COVID CT: 8 weeks, 3 sessions per week, 2× Strength training: 3 × 8 repetitions, 4 exercises squats, bench press, deadlifts and bench pulls. 50% RM constant programming model—intra-set intensity and volume kept constant throughout the training plan. Strength training was combined with moderate-intensity variable aerobic training (MIVT: 4–6 × 3–5 min at 70–80% heart rate reserve [HRR]/2–3 min at 55–65% of FCR). Isolated aerobic: 1 day of continuous light intensity training (LICT: 30–60min, 65–70% HRR) WHO: 30′, 5× week at an intensity that allows breathless speech plus strength exercises in 3 weekly sessions (3 × 10 repetitions of the 7 recommended exercises). Note: adapted and supervised multicomponent exercise program from the ACSM guidelines for chronic obstructive pulmonary disease and cardiovascular disease. | ↔ ↔ | ↑ ↔ |
| Longobardi et al. 2022. Brazil [30] | Recovery of general physical condition in post-COVID patients. | Aerobic + Strength Training + Stretching—HBET: home training 3× a week, aerobic exercises for strengthening and flexibility. 1 supervised session (online) and 2 unsupervised sessions. Aerobic: 2 sets of 10 min/day of walking at “very light” to “reasonably light” intensity (Borg scale 9–11) following week, progression with a single 45-min walking session at “somewhat difficult” to “strong” (Borg scale 14–16) Strength training: 6 strengthening exercises of 3 to 4 sets per exercise of 10 to 15 repetitions, with a self-suggested recovery interval between sets. Stretching: Active stretching exercises for major muscle groups were prescribed as relaxation. | ↑ | ↑ |
| Márquez-Silva et al., 2022. Mexico [31] | Generate an exercise program to improve the physical condition of patients with the syndrome Post-COVID-19. | Strength training + Aerobic + Balance + RMT 10 sessions 4× per week, 60–90′ per session based on RPE. The session was divided into: warm-up; central phase where strength and muscular endurance exercises were worked on; aerobic training; balance exercises and breathing exercises. Strength training: bench press; military bench press; squat; deadlift. Aerobic: walking. Balance: - TMR: - Note: Own preparation. | ↔ | ↔ |
| Sari et al., 2022. Turkey [32] | To investigate the effectiveness of inspiratory muscle training on exercise capacity, lower muscle strength, dyspnea, anxiety-depression, quality of life, physical activity and fatigue in coronavirus disease 2019 (COVID-19) patients with respiratory diseases. | Strength training + RMT or RMT (inspiratory) TMR: diaphragmatic breathing; chest expansion; exercises to increase chest compliance with respiratory control with an exercise band. 5–10 repetitions of 5 to 10 min, 3 sets/day. Strength training: squats and clinical bridge exercises (based on pilates), for 6 weeks every day 3 × 10 repetitions/day. TMR (inspiratory): 30 min, 3 times, 7 days for 6 weeks, deep diaphragmatic breathing for 8 to 10 breaths. Loading resistance was increased every week. | ↑ ↑ | ↑ ↔ |
| Takekawa et al., 2022. Japan [33] | Determine the impact of Unsupervised Pulmonary Rehabilitation. We describe here a nephrectomized patient with severe COVID-19 infection who required extracorporeal membrane oxygenation (ECMO) during admission to the intensive care unit (ICU), but made a full recovery and returned to society after rehabilitation therapy. | RMT + Strength training + Aerobic 3× a day, 30′ total with 3 sets each time, 6 days a week. Self-training focused on strengthening the muscles of the trunk, upper and lower limbs and expiratory muscles. TMR: trunk stretching, shoulder girdle and neck exercises and deep breathing. Strength training: joint range of motion and muscle strengthening exercises. Non-equipment-based resistance training. 8–12 reps. Aerobic: in “easy” PSE; walking exercise and going up and down stairs. | ↑ | NA |
| Mayer et al., 2021. USA [34] | Provide the clinical presentation and physical therapy management of a patient with post-COVID syndrome. | Aerobic + Strength training + RMT Fortnightly sessions for 8 weeks totaling 16 training sessions (15 sessions were held) from 40–80′. The first 4 were supervised with education to be carried out at home. Aerobic: Upper limb exercise bike, treadmill, running and dancing. 60–80% of HR max. in test with at least 15′. Strength training: ‘10–20’ of 10–15 repetitions focused on multi-joint or compound exercises. Based on PSEm when <4/10 with increased load and/or number of repetitions. Start with dumbbells (1.3kg) and leg weights sitting and standing. Progressing to functional movements with squats and weight gain. TMR: controlled diaphragmatic breathing techniques with relaxation and mindfulness. Diaphragmatic breathing combined with general core and trunk exercises (sitting lumbar extension and flexion with core activation, cat-cow exercise, child’s pose and bird-dog exercises). Note: post-exertion malaise. | ↓ | ↓ |
| Stavrou et al., 2021. Greece [35] | Determine the impact of Unsupervised Pulmonary Rehabilitation (uns-PR) on patients recovering from COVID-19, and determine their anthropometric and biological characteristics. | Multicomponent + Breathing Exercises based on Yoga 8 weeks, 3 weekly sessions, around 100 min. Flexibility and mobility: Warm-up/recovery: Child’s Pose-Prayer Stretch, Doorway Stretch, Quadriceps Stretch. Aerobic: walking on a hard, flat surface marking the distance covered (50′). Yoga: for breathing and proprioception (20′). Strength training: multi-joint exercises; lateral raise with dumbbells; squats with dumbbells, chair lunges, seated leg raises, elbow flexion-extension on the chest with medicine ball. | ↔ | ↑ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mazzonetto, L.F.; Cordeiro, J.F.C.; Correia, I.M.; Oliveira, A.d.S.; Moraes, C.; Brilhadori, J.; Gomide, E.B.G.; Kudlacek, M.; Machado, D.R.L.; Anjos, J.R.C.d.; et al. Physical Training Protocols for Improving Dyspnea and Fatigue in Long COVID: A Systematic Review with Meta-Analysis. Healthcare 2025, 13, 1897. https://doi.org/10.3390/healthcare13151897
Mazzonetto LF, Cordeiro JFC, Correia IM, Oliveira AdS, Moraes C, Brilhadori J, Gomide EBG, Kudlacek M, Machado DRL, Anjos JRCd, et al. Physical Training Protocols for Improving Dyspnea and Fatigue in Long COVID: A Systematic Review with Meta-Analysis. Healthcare. 2025; 13(15):1897. https://doi.org/10.3390/healthcare13151897
Chicago/Turabian StyleMazzonetto, Lisa Fernanda, Jéssica Fernanda Correa Cordeiro, Igor Massari Correia, Alcivandro de Sousa Oliveira, Chimenny Moraes, Joana Brilhadori, Eurípedes Barsanulfo Gonçalves Gomide, Michal Kudlacek, Dalmo Roberto Lopes Machado, Jeferson Roberto Collevatti dos Anjos, and et al. 2025. "Physical Training Protocols for Improving Dyspnea and Fatigue in Long COVID: A Systematic Review with Meta-Analysis" Healthcare 13, no. 15: 1897. https://doi.org/10.3390/healthcare13151897
APA StyleMazzonetto, L. F., Cordeiro, J. F. C., Correia, I. M., Oliveira, A. d. S., Moraes, C., Brilhadori, J., Gomide, E. B. G., Kudlacek, M., Machado, D. R. L., Anjos, J. R. C. d., & Santos, A. P. d. (2025). Physical Training Protocols for Improving Dyspnea and Fatigue in Long COVID: A Systematic Review with Meta-Analysis. Healthcare, 13(15), 1897. https://doi.org/10.3390/healthcare13151897





