Evaluating Maturity Models in Healthcare Information Systems: A Comprehensive Review
Abstract
1. Introduction
2. HIS Implementation Challenges
- Technical skills—encompassing a broad spectrum of expertise, including technical knowledge, practical experience, and functional capabilities;
- Project management skills—involving the knowledge, methodologies, and competencies required to effectively manage Health Information System (HIS) projects;
- People and organizational skills—referring to the interpersonal and organizational abilities needed to engage and collaborate effectively with the diverse stakeholders involved in HIS initiatives.
- Lack of senior management commitment, which is frequently incomplete or entirely absent [46];
- Challenges in engaging healthcare professionals and insufficient attention to end-user needs [47];
- Inaccurate specification of requirements, leading to system misalignment with clinical needs [48];
- An absent or poorly managed change process, which undermines adoption efforts [49];
- Limited understanding of the complexity of healthcare systems, resulting in ineffective implementation strategies [46];
- Insufficient investment in human resources, which hampers the capacity to support and sustain digital initiatives [50];
- Inadequate training, a critical factor influencing health professionals’ willingness and ability to adopt and integrate information systems into clinical practice [51].
3. Maturity Models for HISs
4. Methodology
- Definition of search terms, keywords, and their combinations to guide the review criteria.
- Identification of relevant publications containing the specified keywords.
- Evaluation of the identified literature and selection of works that met the inclusion criteria.
- Extraction of relevant information from the selected studies.
- Synthesis and analysis of the extracted data.
4.1. Inclusion and Exclusion Criteria
- Peer-reviewed journal articles or conference papers.
- Published between 2000 and 2025.
- Written in English.
- Explicit focus on Maturity Models within the context of healthcare, digital health, or Health Information Systems (HISs).
- Articles addressing the development, application, or evaluation of Maturity Models.
- Studies presenting practical, empirical, or theoretical contributions related to HIS maturity.
- Articles not related to Maturity Models or not applied in healthcare settings.
- Conceptual work lacks empirical grounding or practical application.
- Studies focused on general IT or other sectors (e.g., manufacturing, education) without healthcare-specific adaptation.
- Non-peer-reviewed publications, editorials, theses, or opinion papers.
- Non-English language sources.
- Duplicate records.
4.2. Search Strategy and Criteria
5. Classification of Maturity Models
- Technology-Focused Models: These assess the maturity of technological infrastructure, IT services, and system adoption levels. They provide guidance on infrastructure development, IT governance, and digital capability. Notable examples include the Healthcare IT Maturity Model (HIT-MM) and the Infrastructure Adoption Model (INFRAM).
- Specialized Domain Models: These target specific healthcare functions or domains, such as telemedicine, usability, interoperability, or public health coordination. They are typically designed for tailored applications, such as the Telemedicine Service Maturity Model (TMSMM) or the Interoperability Maturity Model (IMM).
- Data and Analytics Models: These models address the organization’s capacity to manage, analyze, and utilize healthcare data effectively. They focus on data quality, analytics maturity, and decision support capabilities. Prominent examples include the Healthcare Analytics Adoption Model (HAAM) and the Business Intelligence Maturity Model (BIMM).
- Policy-Oriented Models: These models address the development, implementation, and institutional maturity of health-related public policies, especially in intersectoral and government settings. They are primarily intended for use by policymakers, administrators, and public institutions aiming to improve population health through systemic governance, for example, the Maturity Model for Health in All Policies (MMHiAP).
5.1. Process-Oriented Models
- Culture—Encompasses organizational practices related to communication, leadership, and the overall receptiveness to change and collaboration.
- Strategy—Refers to the guiding principles and strategic alignment necessary for the effective implementation and evolution of process management within healthcare institutions.
- Structure—Includes the organizational architecture, governance mechanisms, and role definitions that support process-based approaches.
- Practices—Represents the operational methodologies and standardized procedures that are central to consistent and effective process management.
- Information Technology (IT)—Captures the extent to which hospital IT systems facilitate the seamless integration and continuity of end-to-end patient care processes.
- Measure performance against the Victorian Government’s IM standards.
- Assess an organization’s alignment with information management best practices.
- Maturity level ratings for each IMMAP participant.
- Average maturity levels across key IM areas.
- Recommendations for future IM improvement initiatives.
5.2. Technology-Focused Models
- Assess their current mobility capabilities and maturity;
- Establish a baseline to define short- and long-term goals and improvement plans;
- Prioritize investments in mobility-related technologies, staff, and infrastructure;
- PACS maturity, defining PACS and its components;
- Alignment of PACS, focusing on how PACS integrates with the hospital’s organizational structures;
- PACS performance, reflecting the added value PACS brings to healthcare delivery.
- Identify their current maturity stage;
- Determine the next achievable stage of maturity;
- Recognize the attributes required to advance to the next level.
- Phase 1: Patient records are primarily paper-based or image-based. Most healthcare providers operate at this stage, where patient information management is viewed largely as a content- or records-management challenge.
- Phase 2: Access to standalone electronic repositories improves. Providers at this stage store more patient data within Electronic Medical Record (EMR) systems and reduce their reliance on paper records.
- Phase 3: Role-based access to a fully digital medical record is achieved. Providers exchange electronic data with other healthcare organizations, patients, and administrative systems. At this level, content is structured to support results-driven analysis.
- Governing all types of information—regardless of format or location—in a consistent and coordinated way;
- Securing information throughout its lifecycle and across the organization’s ecosystem, covering both data and IT governance;
- Addressing data privacy and integrity requirements, ensuring compliance while maximizing the value derived from information.
- This enterprise-wide framework enables organizations to treat information as a strategic asset, supporting a wide range of needs, including strategic planning, regulatory compliance, legal obligations, risk management, and environmental responsibility.
- IG Structure
- Strategic Alignment
- Enterprise Information Management
- Privacy and Security
- Legal and Regulatory Compliance
- Data Governance
- IT Governance
- Analytics
- IG Performance
- Awareness and Adherence
- A conceptual model of smart city services;
- Clearly defined IT dimensions and indicators;
- Distinct IT maturity levels.
- Level 1: Integrated—Information is collected, stored, and integrated, making it readily available for smart services.
- Level 2: Analytically Managed—Advanced analytics (descriptive, predictive, prescriptive) are applied, enabling the generation of smart dashboards for decision-making.
- Level 3: Optimized Automated—Beyond integration and analytics, this level incorporates artificial intelligence to automate processes, enhancing decision-making, operational efficiency, and system performance.
- A tabular view showing results across individual security domains along with the overall maturity score.
- A Maturity Model with defined domains and progression pathways for HIS interoperability.
- An assessment tool that enables structured national or sub-national evaluations.
- A users’ guide to support implementation and interpretation.
- Benchmark interoperability maturity;
- Advocate for investment and policy change;
- Build roadmaps for digital transformation.
- Co-creating the Digital Health Profile (DHP);
- Defining both quantitative and qualitative country-specific indicators;
- Co-developing the Digital Health Maturity Assessment Tool (DHMAT);
- Aligning DHP indicators with the maturity of essential digital health foundations as assessed by the DHMAT;
- Iteratively refining and validating indicators and the DHP with input from key informants;
- Developing localized maturity assessment criteria;
- Finalizing the DHPMAT framework;
- Conducting multiple iterations of the DHPMAT to refine its content and structure;
- Testing the initial version with key informants, followed by further evaluation at a PHIN workshop.
- Digital health foundations;
- Maturity assessment;
- Quality improvement.
- Acts as a conceptual bridge between guiding principles for health information systems and the strategic objectives of public health organizations. It ensures alignment between health information practices and broader public health goals.
- Supports planning, risk identification, and prioritization of activities related to IS4H adoption. It addresses operational and cultural challenges, helping to balance local engagement and organizational support for health information systems.
- Functions as a roadmap guiding health organizations toward their strategic goals within the IS4H program, outlining the vision, priorities, and actions needed for long-term success.
- Defines key concepts within the health information systems domain and promotes shared understanding among health professionals. It also describes the processes necessary to deliver services and the benefits that they produce, providing a foundation for developing actionable plans based on IS4H best practices.
- Provides tools and guidance for applying the IS4H Maturity Model Level Assessment, allowing organizations to appraise their current maturity level. Trust is positioned as a foundational element, supporting transparency and continuous improvement.
- Focuses on building capacity and fostering continuous learning within the IS4H environment. This component outlines learning objectives, processes, and tools to help health organizations and professionals adapt and evolve alongside advancements in Health Information Systems.
- Security—Ensuring protection of patient data and system integrity.
- Mobility—Supporting clinicians’ access to systems and information anywhere, anytime.
- Collaboration—Enabling communication and integration across systems and care teams.
- Transport—Assessing the capacity and speed of networks and connectivity.
- Data Center—Evaluating the resiliency and scalability of core IT systems.
5.3. Specialized Domain Models
- eReadiness Categories;
- Stages of the Telemedicine Process;
- Maturity Levels.
- Technology and Maintenance: Availability and reliability of ICT infrastructure, user training, and system usability.
- Policy and Legislation: The presence of supportive government and institutional policies, standardization efforts, and security measures.
- Individual Users: The trust and willingness of healthcare providers and decision-makers, evidence generation, and openness to process changes.
- Organizational Processes: Effective decision-making structures and streamlined work procedures.
- Planning and Financial Sustainability: Viable business models that ensure the long-term continuity of telemedicine services.
- Community Interaction and Involvement: Engagement with and involvement of the local community in telemedicine initiatives.
- EMR Functionality: Supports longitudinal patient tracking, referral processes, and comprehensive discharge summaries.
- Interoperability Standards: Implements open standards such as HL7, FHIR, and SNOMED CT to enable structured data exchange.
- Data Governance: Ensures role-based access controls, consent management, and audit trails to safeguard patient data.
- Care Pathway Alignment: Enables multidisciplinary, team-based care pathways within the EMR.
- System Integration: Achieves seamless communication and synchronization between core Health Information System (HIS) modules, such as laboratory, radiology, and pharmacy.
- Patient Engagement: Facilitates patient access to health records, digital follow-ups, and automated reminders to promote active participation in their care.
- The CCMM serves as both an assessment and a strategic planning tool, helping healthcare organizations benchmark their current capabilities and define the necessary steps toward integrated, patient-centered care delivery [129].
- Governance and policy alignment;
- Use of open standards (e.g., HL7, FHIR, CDA, SNOMED CT);
- Technical infrastructure readiness;
- Organizational workflows and data lifecycle management;
- Security, privacy, and consent mechanisms;
- Monitoring and performance metrics.
- Vision and Engagement
- Governance
- Policy and Legislation
- Skills and Resources
- Funding
- Model Practice
- Success Metrics
- Clinical Use Cases
- Technology and Applications
- Security and Privacy
- Initial
- Anticipate
- Interoperate
- Collaborate
- Optimize
- Unrecognized—Lack of awareness or understanding of usability principles.
- Preliminary—Sporadic inclusion of usability practices, often inconsistent.
- Implemented—Usability is recognized as valuable and systematically considered.
- Integrated—Usability practices are embedded across all relevant workflows and departments.
- Strategic—Usability is treated as a strategic asset with allocated budgets and resources; outcomes are measured and used to drive organizational strategy.
- Opportunity: HCMM responds to the growing need for enhanced cooperation in healthcare, focusing on optimizing collaborative structures and workflows in hospital environments. It is a newly developed model rooted in contemporary healthcare challenges.
- Scope: The model is targeted, concentrating on strategic, organizational, and technical dimensions that influence cooperative efficiency. Its primary users are hospital decision-makers seeking to assess and improve collaboration.
- Maturity Concept: HCMM employs a multidimensional measurement framework. It evaluates both “as-is” (current state) and “to-be” (desired future state) maturity levels across strategic, organizational, and technical capabilities.
- Design Decisions: The model combines theory-based constructs with practical insights gathered from hospital environments. It aims to diagnose challenges and offer a roadmap for improvement across multiple dimensions of cooperation.
- Evaluation: The HCMM was evaluated using both ex-ante methods (e.g., structured questionnaires) and naturalistic settings involving real-world user feedback to validate both content and usability.
- Strategic Layer—Assesses the hospital’s capacity to establish and manage collaborations with external healthcare partners.
- Organizational Layer—Focuses on internal cooperation across departments and units within the hospital.
- Information Layer—Measures the adequacy and effectiveness of the hospital’s IT infrastructure to support internal and external collaboration.
- Initial (Level 1): Processes are ad hoc, chaotic, or reactive; success depends on individual effort and a lack of standardization.
- Managed (Level 2): Basic project and process management is in place; repeatable procedures exist for specific areas and more consistent outcomes.
- Defined (Level 3): Organization-wide standards and policies are established; processes are documented and integrated and staff are trained in standardized procedures.
- Quantitatively Managed (Level 4): Performance metrics are collected and analyzed; data-driven decision making is emphasized and continuous monitoring and control.
- Optimizing (Level 5): Focus on continuous improvement and innovation; lessons learned are systematically incorporated with proactive problem prevention and process optimization.
- Stakeholders working on standards, guidelines, and supporting resources to improve the integration of devices and systems, and
- Anyone seeking a deeper understanding of interoperability dimensions and the detailed structure of the Maturity Model.
- Health software focus in low-resource settings: GGMM emphasizes solutions intended for use in resource-constrained environments, aligning with SORMAS’s operational context.
- Aligned objectives: The goals of the GGMM closely match SORMAS’s mission of improving health surveillance and outbreak responses.
- Comparable scope: Many of the tools assessed through the GGMM framework share similar functionalities and use cases with SORMAS.
- Global Utility;
- Community Support;
- Software Maturity.
- Governance—This axis addresses the decision-making and command structure of field hospitals throughout their entire mission lifecycle, including situation assessment, deployment, operational phases, and withdrawal.
- Logistics—Encompasses the provision, storage, transport, and post-use collection of all resources (both medical and non-medical) necessary for field hospital functioning. These logistic operations may be internally managed or supported by external entities.
- Care—Refers to the clinical and medical services delivered during the field hospital’s operation phase.
- Unconsidered/Unknown—The axis is either poorly addressed or entirely neglected.
- Initial—The axis is recognized but addressed in an unstructured or ad hoc manner.
- Practiced—Formal processes are in place, but there is no consistent monitoring or assessment.
- Managed—The axis is governed by international standards and established procedures, with appropriate monitoring and management mechanisms.
- Improved—Processes are continuously optimized, with the systematic incorporation of changes and updates to standards and procedures.
- Differentiation of Maturity Levels: Each semantic interoperability attribute distinguishes between at least two levels of maturity.
- Gradual Improvement Guidance: Recommendations are provided using improvement tables that guide services incrementally through maturity stages.
- Targeted Recommendations: If a service has not yet reached the highest maturity level for an attribute, IMAPS offers specific advice to reach the next level.
- No Redundant Advice: If the highest maturity level has already been achieved, no further recommendation is given for that attribute.
- Sliding Scale for Generic Improvements: Where maturity is measured on a continuous scale rather than discrete levels, general advice is provided to promote further improvement.
- It provides a systematic measurement framework to describe and evaluate HIS components;
- It helps users and stakeholders set strategic goals for HIS advancement;
- It guides the development of improvement plans, enabling systems to move progressively toward higher levels of maturity.
- Readiness to Change—Organizational willingness and leadership support.
- Structure and Governance—Policies and partnerships to support integration.
- Information and eHealth Services—Use of digital tools for communication and data sharing.
- Standardization and Simplification—Use of common protocols and processes.
- Funding Models—Sustainable financing mechanisms for integrated care.
- Incentives and Motivation—Professional and system-level incentives.
- Process Coordination—Alignment of care pathways across providers.
- Population Approach—Stratification and targeting based on patient needs.
- Citizen Empowerment—Involving patients in care decisions and self-management.
- Evaluation Methods—Measurement of outcomes and performance.
- Breadth of Ambition—Scope of integration (local vs. system-wide).
- Innovation Management—Capacity to adopt and scale new models.
- Process Integration—The extent to which collaboration is embedded in formal business workflows.
- Governance and Roles—Definition of responsibilities, facilitation structures, and leadership mechanisms that support collaborative work.
- Supporting Tools—The use and integration of digital platforms and technologies (e.g., communication tools, shared documentation systems) that enable effective collaboration.
- Measurement and Improvement—The presence of metrics and feedback loops to assess collaborative performance and guide continuous enhancement.
- Visibility and Clarity: CollabMM transforms informal collaboration into a formalized, measurable process. This visibility supports better alignment with strategic objectives.
- Benchmarking: The model facilitates both internal and external benchmarking of collaborative practices, providing a reference point for organizational development.
- Targeted Improvements: By highlighting maturity gaps, CollabMM offers a roadmap for systematic improvement across tools, communication practices, governance, and team culture.
- Sector Versatility: CollabMM is applicable across a wide range of sectors, including healthcare, education, software development, and public administration, making it a flexible and scalable tool for organizational development.
5.4. Data and Analytics Models
- The Informatics Capability Maturity Model (ICMM) is a framework designed to assess an organization’s ability to effectively collect, manage, and share health data, implement ICT solutions, ensure robust data governance, and leverage health business intelligence for integrated, multidisciplinary care delivery [151]. The ICMM aligns with broader informatics maturity frameworks and has been shown, in integrated primary care settings, to correlate with improved care coordination and health outcomes.
- Basic: Health IT systems are fragmented, unreliable, and lack coordination.
- Controlled: Systems provide consistent functionality, but data and expertise remain siloed.
- Standardized: Common standards and protocols enable broader data sharing and collaboration.
- Optimized: Processes are streamlined, efficient, and governed by formal policies.
- Innovative: Informatics capabilities drive continuous innovation and are embedded across the enterprise.
- ICM1: Data collection, integration, and management (including HIS and EHR systems).
- ICM2: Information sharing and interoperability across healthcare districts and networks.
- ICM3: ICT-implementation practices and change management strategies.
- ICM4: Data quality management and governance frameworks for secure and reliable data handling.
- ICM5: Use of health business intelligence to drive improvements in population health outcomes.
- Recognize informatics as a strategic asset that supports broader business and care-delivery objectives.
- Align IT investments with organizational goals and care-delivery strategies.
- View IT not merely as a support function but as a key driver of healthcare transformation.
- Implement IT-enabled change management practices that enhance organizational efficiency and clinical outcomes.
- The need to integrate both clinical and financial data, which traditionally exist in siloed systems;
- The heterogeneity of data formats required to support high-level analytical functions;
- Increasing expectations from external stakeholders for reliable clinical and financial decision support.
- A conceptual framework for managing BI deployment in healthcare environments;
- A focus on both operational/financial and clinical information requirements;
- Inclusion of key BI processes that are specific to healthcare, such as patient care pathways, regulatory compliance, and cost control;
- Integration of the people–process–technology triad to ensure a holistic maturity evaluation;
- Emphasis on quality dimensions, including system quality, information quality, and service quality;
- Clarity on the interrelationship between maturity levels and critical BI processes, grounded in theoretical and empirical foundations [154].
- Maturity Levels—defining the stages of advancement in data quality practices.
- Practices—standardized methods for improving data quality.
- Process Areas—aligned with phases of the data lifecycle (collection, storage, processing, analysis, and reporting).
- Value Creation—focusing on how data quality improvements contribute to better health outcomes and decision-making.
- Stage 1. Conceptual: clinical processes capture data primarily in verbose documents, not as data; lack of organizational awareness of data utility, no effort to systematically manage healthcare data, lack of consistent or centralized governance, policies, and/or resources, data not organized centrally.
- Stage 2. Reactive: the enterprise can react to requests for analysis and respond to research requests but mostly accomplished by manual chart review and abstraction; data management inefficient and expensive, with only sporadic recognition of data utility beyond immediate use.
- Stage 3. Structured: clinical systems manage transactional data types (e.g., orders, transactions, laboratory results, medication prescriptions) as discrete data; support from leadership for centralized data governance and management of these data types at the enterprise level.
- Stage 4. Complete: granular and complete clinical data based on standardized clinical common data elements captured in the processes of care, integrated into those care processes; health systems data routinely and systematically represent data externally via various CDMs, including efficient queries, support for large number of research projects.
- Stage 5. Advanced: data linkage and aggregation across systems enabled and open to external queries; interoperability of clinical data enabled; multiple sources of sustainable funding support for research; engagement of regulatory and industry enterprises with enterprise data.
5.5. Policy-Oriented Models
- Benchmark digital health maturity and improve the quality of digital health systems at the national level.
- Track progress toward comprehensive and integrated digital health ecosystems.
- Identify gaps in funding and technical assistance, both within individual countries and across regions.
- Promote alignment among policymakers, donors, and implementers, following the Principles for Digital Development and the Donor Alignment for Digital Health framework.
- Highlight investment risks at the country level, providing greater transparency for funders and stakeholders.
6. Discussion
6.1. Definitions and Characteristics of Maturity Models
6.2. Applications in Healthcare Domains
6.3. Contextualization in Healthcare Environments
6.3.1. Public vs. Private Hospitals
6.3.2. Developed vs. Emerging Economies
6.3.3. Primary vs. Tertiary Care Settings
6.3.4. Limitations of Adapted Models from Other Sectors
- The criticality of timely clinical decision-making;
- The ethical and regulatory sensitivities surrounding personal health data;
- The highly interdisciplinary nature of healthcare teams.
6.4. Practical Implications and Model Selection Guidance
6.5. Limitations of the Review
6.5.1. Scope of the Literature Search
6.5.2. Heterogeneity of Model Definitions
6.5.3. Limited Empirical Validation
6.5.4. Geographical and Sectoral Bias
6.5.5. Focus on Model Characteristics over Outcomes
6.5.6. Limited Coverage of Commercial Benchmarking Models
6.6. Recommendations for Future Research
6.6.1. Empirical Validation in Diverse Healthcare Settings
6.6.2. Development of Healthcare-Specific Models
6.6.3. Comparative Studies of Model Effectiveness
6.6.4. Integration Across Domains
6.6.5. Adaptation for Emerging Technologies and Challenges
6.6.6. Tools and Automated Assessments
6.7. Summary of Identified Maturity Models
7. Conclusions
Compliance with Ethical Standards
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Drury, P. The eHealth agenda for developing countries. World Hosp. Health Serv. 2005, 41, 38–40. [Google Scholar]
- Bukachi, F.; Pakenham-Walsh, N. Information technology for health in developing countries. Chest 2007, 132, 1624–1630. [Google Scholar] [CrossRef]
- Bajwa, J.; Munir, U.; Nori, A.; Williams, B. Artificial intelligence in healthcare: Transforming the practice of medicine. Future Healthc. J. 2021, 8, e188–e194. [Google Scholar] [CrossRef]
- Gomes, J.; Romão, M. Improving the success of IS/IT projects in healthcare: Benefits and project management approaches. In New Advances in Information Systems and Technologies, Part II; Rocha, A., Correia, A.M., Adeli, H., Reis, L.P., Costanzo, S., Eds.; Springer: Berlin/Heidelberg, Germany, 2016; Volume 444, pp. 547–556. [Google Scholar] [CrossRef]
- Savoy, M.; Hazlett-O’Brien, C.; Rapacciuolo, J. The role of primary care physicians in managing chronic disease. Del. J. Public Health 2017, 3, 86–93. [Google Scholar] [CrossRef]
- WHO (World Health Organization). World Report on Ageing and Health; World Health Organization: Geneva, Switzerland, 2015; Available online: http://apps.who.int/iris/bitstream/10665/186463/1/9789240694811_eng.pdf?ua=1 (accessed on 1 July 2025).
- EC (European Commission). Ageing Report: Economic and Budgetary Projections for the EU-27 Member States (2008–2060); Directorate General for Economic and Financial Affairs—DG ECFIN, European Commission: Brussels, Belgium, 2009; Available online: http://ec.europa.eu/economy_finance/publications/pages/publication14992_en.pdf (accessed on 1 July 2025).
- Jones, C.H.; Dolsten, M. Healthcare on the brink: Navigating the challenges of an aging society in the United States. NPJ Aging 2024, 10, 22. [Google Scholar] [CrossRef] [PubMed]
- Lymberis, A.; Dittmar, A. Advanced wearable health systems and applications: Research and development efforts in the European Union. IEEE Eng. Med. Biol. Mag. 2007, 26, 29–33. [Google Scholar] [CrossRef]
- OECD (Organisation for Economic Co-operation and Development). Projecting OECD Health and Long-Term Care Expenditures: What Are the Main Drivers? (OECD Economics Department Working Papers No. 477, ECO/WKP(2006)5); OECD Publishing: Paris, France, 2006; Available online: https://www.oecd.org/en/publications/projecting-oecd-health-and-long-term-care-expenditures_736341548748.html (accessed on 22 July 2025).
- Javaid, M.; Haleem, A.; Singh, R.P. Health informatics to enhance the healthcare industry’s culture: An extensive analysis of its features, contributions, applications and limitations. Inform. Health 2024, 1, 123–148. [Google Scholar] [CrossRef]
- Kirilov, N. Capture of real-time data from electronic health records: Scenarios and solutions. mHealth 2024, 10, 14. [Google Scholar] [CrossRef]
- Mäenpää, T.; Suominen, T.; Asikainen, P.; Maass, M.; Rostila, I. The outcomes of regional healthcare information systems in health care: A review of the research literature. Int. J. Med. Inform. 2009, 78, 757–771. [Google Scholar] [CrossRef] [PubMed]
- Beuscart-Zéphir, M.C.; Anceaux, F.; Crinquette, V.; Renard, J.M. Integrating users’ activity modeling in the design and assessment of hospital electronic patient records: The example of anesthesia. Int. J. Med. Inform. 2001, 64, 157–171. [Google Scholar] [CrossRef]
- Gruber, D.; Cummings, G.G.; Leblanc, L.; Smith, D.L. Factors influencing outcomes of clinical information systems implementation: A systematic review. Comput. Inform. Nurs. 2009, 27, 151–163. [Google Scholar] [CrossRef]
- Sutton, R.T.; Pincock, D.; Baumgart, D.C.; Sadowski, D.C.; Fedorak, R.N.; Kroeker, K.I. An overview of clinical decision support systems: Benefits, risks, and strategies for success. NPJ Digit. Med. 2020, 3, 17. [Google Scholar] [CrossRef]
- Bindakheel, A.; Rosnah, N. Adoption of ICT at hospital: A case study of UMMC. In Proceedings of the 2nd International Conference on Electronic Computer Technology (ICET 2010), IEEE, Kuala Lumpur, Malaysia, 7–10 May 2010; pp. 157–167. [Google Scholar]
- Sinnaiah, T.; Adam, S.; Mahadi, B. A strategic management process: The role of decision-making style and organisational performance. J. Work-Appl. Manag. 2023, 15, 37–50. [Google Scholar] [CrossRef]
- Aiwerioghene, E.M.; Lewis, J.; Rea, D. Maturity models for hospital management: A literature review. Int. J. Healthc. Manag. 2024. ahead of print. [Google Scholar] [CrossRef]
- Albrecht, J.C.; Spang, K. Linking the benefits of project management maturity to project complexity: Insights from a multiple case study. Int. J. Manag. Proj. Bus. 2014, 7, 285–301. [Google Scholar] [CrossRef]
- Becker, J.; Knackstedt, R.; Pöppelbuß, J. Developing maturity models for IT management: A procedure model and its application. Bus. Inf. Syst. Eng. 2009, 1, 213–222. [Google Scholar] [CrossRef]
- Carvalho, J.V.; Rocha, Á. Towards an encompassing maturity model for the management of hospital information systems. J. Med. Syst. 2015, 39, 119. [Google Scholar] [CrossRef]
- Shi, Q. Rethinking the implementation of project management: A value adding path map approach. Int. J. Proj. Manag. 2011, 29, 295–302. [Google Scholar] [CrossRef]
- Sopko, J.A.; Strausser, G. The value of organizational project management (OPM) maturity—Understanding, measuring, and delivering benefits. In Proceedings of the PMI Global Congress 2010—North America, Project Management Institute, Washington, DC, USA, 12 October 2010. [Google Scholar]
- Alshabragi, A.M.; Almohsen, A.S.; Bin Mahmoud, A.A. Developing a Maturity Rating System for Project Management Offices. Systems 2024, 12, 367. [Google Scholar] [CrossRef]
- Crawford, L. Senior management perceptions of project management competence. Int. J. Proj. Manag. 2005, 23, 7–16. [Google Scholar] [CrossRef]
- Kruk, M.E.; Gage, A.D.; Arsenault, C.; Jordan, K.; Leslie, H.H.; Roder-DeWan, S.; Adeyi, O.; Barker, P.; Daelmans, B.; Doubova, S.V.; et al. High-quality health systems in the Sustainable Development Goals era: Time for a revolution. Lancet Glob. Health 2018, 6, e1196–e1252. [Google Scholar] [CrossRef]
- Cleven, A.; Winter, R.; Wortmann, F.; Mettler, T. Process management in hospitals: An empirically grounded maturity model. Bus. Res. 2014, 7, 191–216. [Google Scholar] [CrossRef]
- van Wijngaarden, J.D.H.; Braam, A.; Buljac-Samardžić, M.; Hilders, C.G.J.M. Towards process-oriented hospital structures: Drivers behind the development of hospital designs. Int. J. Environ. Res. Public Health 2023, 20, 1993. [Google Scholar] [CrossRef]
- Gomes, J.; Romão, M. Information system maturity models in healthcare. J. Med. Syst. 2018, 42, 235. [Google Scholar] [CrossRef]
- Rohner, P. Achieving impact with clinical process management in hospitals: An inspiring case. Bus. Process Manag. J. 2012, 18, 600–624. [Google Scholar] [CrossRef]
- Cleven, A.; Mettler, T.; Rohner, P.; Winter, R. Healthcare quality innovation and performance through process orientation: Evidence from general hospitals in Switzerland. Technol. Forecast. Soc. Change 2016, 113 Pt B, 386–395. [Google Scholar] [CrossRef]
- Kaplan, B.; Harris-Salamone, K.D. Health IT success and failure: Recommendations from literature and an AMIA workshop. J. Am. Med. Inform. Assoc. 2009, 16, 291–299. [Google Scholar] [CrossRef] [PubMed]
- Sadoughi, F.; Kimiafar, K.; Ahmadi, M.; Shakeri, M.T. Determining the factors influencing the success and failure of hospital information systems and their evaluation methods: A systematic review. Iran. Red. Crescent Med. J. 2013, 15, e11716. [Google Scholar] [CrossRef] [PubMed]
- Kahouli, B.; Omri, A.; Afi, H. Technological innovations and health performance: Effects and transmission channels. Technol. Forecast. Soc. Change 2024, 204, 123450. [Google Scholar] [CrossRef]
- Schultz, J.R. Measuring service industry performance: Some basic concepts. Perform. Improv. 2006, 45, 13–19. [Google Scholar] [CrossRef]
- Bagherian, H.; Sattari, M. Health information system in developing countries: A review on the challenges and causes of success and failure. Med. J. Islam. Repub. Iran 2022, 36, 111. [Google Scholar] [CrossRef] [PubMed]
- Heeks, R.B. Success and failure rates of e-government in developing/transitional countries: Overview. In Building Digital Opportunities Programme, Information Exchange, University of Manchester’s Institute for Development Policy and Management; UK Department for International Development: London, UK, 2008; Available online: http://www.egov4dev.org/success/sfrates.shtml#overall (accessed on 1 July 2025).
- Heeks, R.B. Health information systems: Failure, success and improvisation. Int. J. Med. Inform. 2006, 75, 125–137. [Google Scholar] [CrossRef] [PubMed]
- Ștefan, A.-M.; Rusu, N.-R.; Ovreiu, E.; Ciuc, M. Empowering Healthcare: A Comprehensive Guide to Implementing a Robust Medical Information System—Components, Benefits, Objectives, Evaluation Criteria, and Seamless Deployment Strategies. Appl. Syst. Innov. 2024, 7, 51. [Google Scholar] [CrossRef]
- Aerts, H.; Kalra, D.; Sáez, C.; Ramírez-Anguita, J.M.; Mayer, M.A.; Garcia-Gomez, J.M.; Durà-Hernández, M.; Thienpont, G.; Coorevits, P. Quality of hospital electronic health record (EHR) data based on the International Consortium for Health Outcomes Measurement (ICHOM) in heart failure: Pilot data quality assessment study. JMIR Med. Inform. 2021, 9, e27842. [Google Scholar] [CrossRef]
- Alharbi, T.A.F.; Rababa, M.; Alsuwayl, H.; Alsubail, A.; Alenizi, W.S. Diagnostic challenges and patient safety: The critical role of accuracy—A systematic review. J. Multidiscip. Healthc. 2025, 18, 3051–3064. [Google Scholar] [CrossRef] [PubMed]
- Jokanović Đajić, M.; Ciric Lalic, D.; Vujičić, M.D.; Stankov, U.; Petrovic, M.; Đurić, Ž. Development and validation of the Project Manager Skills Scale (PMSS): An empirical approach. Heliyon 2024, 10, e25055. [Google Scholar] [CrossRef]
- Lorenzi, M.M.; Riley, R.T. Organizational issues = change. Int. J. Med. Inform. 2003, 69, 197–203. [Google Scholar] [CrossRef]
- Lewis, D.; Hodge, N.; Gamage, D.; Whittaker, M. Understanding the role of technology in health information systems. Pac. Health Dialog 2011, 18, 144–154. [Google Scholar]
- Bayat, M.; Kashkalani, T.; Khodadost, M.; Shokri, A.; Fattahi, H.; Ghasemi Seproo, F.; Younesi, F.; Khalilnezhad, R. Factors associated with failure of health system reform: A systematic review and meta-synthesis. J. Prev. Med. Public Health 2023, 56, 128–144. [Google Scholar] [CrossRef]
- Woodward, E.N.; Castillo, A.I.M.; True, G.; Willging, C.; Kirchner, J.E. Challenges and promising solutions to engaging patients in healthcare implementation in the United States: An environmental scan. BMC Health Serv. Res. 2024, 24, 29. [Google Scholar] [CrossRef]
- Holmes, J.H.; Beinlich, J.; Boland, M.R.; Bowles, K.H.; Chen, Y.; Cook, T.S.; Demiris, G.; Draugelis, M.; Fluharty, L.; Gabriel, P.E.; et al. Why is the electronic health record so challenging for research and clinical care? Methods Inf. Med. 2021, 60, 32–48. [Google Scholar] [CrossRef]
- Borges do Nascimento, I.J.; Abdulazeem, H.; Vasanthan, L.T.; Martinez, E.Z.; Zucoloto, M.L.; Østengaard, L.; Azzopardi-Muscat, N.; Zapata, T.; Novillo-Ortiz, D. Barriers and facilitators to utilizing digital health technologies by healthcare professionals. NPJ Digit. Med. 2023, 6, 161. [Google Scholar] [CrossRef]
- Berry, L.L.; Yadav, M.S.; Hole, M.K. Reclaiming healthcare’s healing mission for a sustainable future. J. Serv. Res. 2023, 27, 6–27. [Google Scholar] [CrossRef]
- Khan, R.; Khan, S.; Almohaimeed, H.M.; Almars, A.I.; Pari, B. Utilization, challenges, and training needs of digital health technologies: Perspectives from healthcare professionals. Int. J. Med. Inform. 2025, 197, 105833. [Google Scholar] [CrossRef]
- Paredes-Saavedra, M.; Vallejos, M.; Huancahuire-Vega, S.; Morales-García, W.C.; Geraldo-Campos, L.A. Work Team Effectiveness: Importance of Organizational Culture, Work Climate, Leadership, Creative Synergy, and Emotional Intelligence in University Employees. Adm. Sci. 2024, 14, 280. [Google Scholar] [CrossRef]
- Pereira, G.S.; Novaski, O.; dos Santos Neto, N.F. Study on the state of the art of critical success factors and project management performance. Gestão Produção 2022, 29, e4722. [Google Scholar] [CrossRef]
- Liaw, S.T.; Godinho, M.A. Digital health and capability maturity models—A critical thematic review and conceptual synthesis of the literature. J. Am. Med. Inform. Assoc. 2023, 30, 393–406. [Google Scholar] [CrossRef] [PubMed]
- Smajli, E.; Feldman, G.; Cox, S. Exploring the limitations of business process maturity models: A systematic literature review. Inf. Syst. Manag. 2024, 42, 2–21. [Google Scholar] [CrossRef]
- Poeppelbuss, J.; Roeglinger, M. What makes a useful maturity model? A framework of general design principles for maturity models and its demonstration in business process management. In Proceedings of the 19th European Conference on Information Systems (ECIS), Helsinki, Finland, 9–11 June 2011. [Google Scholar]
- Mullaly, M. If maturity is the answer, then exactly what was the question? Int. J. Manag. Proj. Bus. 2014, 7, 169–185. [Google Scholar] [CrossRef]
- Domingues, L.; Ribeiro, P. Project management maturity models: Proposal of a framework for models comparison. In Proceedings of the CENTERIS, ProjMAN & HCist 2022 Conferences, Porto, Portugal, 8–10 November 2023; Procedia Computer Science. Volume 219, pp. 2011–2018. [Google Scholar] [CrossRef]
- Friedman, C.P.; Flynn, A.J. A maturity grid assessment tool for learning networks. Learn. Health Syst. 2020, 4, e10203. [Google Scholar] [CrossRef]
- Dong, H.; Dacre, N.; Baxter, D.; Ceylan, S. What is Agile Project Management? Developing a New Definition Following a Systematic Literature Review. Proj. Manag. J. 2024, 55, 668–688. [Google Scholar] [CrossRef]
- Colli, M.; Berger, U.; Bockholt, M.; Madsen, O.; Møller, C.; Wæhrens, B.V. A maturity assessment approach for conceiving context-specific roadmaps in the Industry 4.0 era. Annu. Rev. Control 2019, 48, 165–177. [Google Scholar] [CrossRef]
- Odważny, F.; Wojtkowiak, D.; Cyplik, P.; Adamczak, M. Concept for measuring organizational maturity supporting Sustainable Development Goals. Logforum 2022, 15, 237–247. [Google Scholar] [CrossRef]
- Mauro, M.; Noto, G.; Prenestini, A.; Sarto, F. Digital transformation in healthcare: Assessing the role of digital technologies for managerial support processes. Technol. Forecast. Soc. Change 2024, 209, 123781. [Google Scholar] [CrossRef]
- Epizitone, A.; Moyane, S.P.; Agbehadji, I.E. A systematic literature review of health information systems for healthcare. Healthcare 2023, 11, 959. [Google Scholar] [CrossRef]
- Stoumpos, A.I.; Kitsios, F.; Talias, M.A. Digital transformation in healthcare: Technology acceptance and its applications. Int. J. Environ. Res. Public Health 2023, 20, 3407. [Google Scholar] [CrossRef]
- Paulk, M.C.; Curtis, B.; Chrissis, M.B.; Weber, C.V. The Capability Maturity Model for Software (Version 1.1) (Technical Report CMU/SEI-93-TR-024); Software Engineering Institute, Carnegie Mellon University: Pittsburgh, PA, USA, 1993; Available online: https://resources.sei.cmu.edu/asset_files/technicalreport/1993_005_001_16211.pdf (accessed on 22 July 2025).
- Gomes, J.; Romão, M. Information Systems and Technology Projects in Healthcare Organisations. In Encyclopedia of Information Science and Technology, 4th ed.; Khosrow-Pour, D.B.A.M., Ed.; IGI Global Scientific Publishing: New York, NY, USA, 2018; pp. 3756–3766. [Google Scholar] [CrossRef]
- Chiawah, T.; Dzekashu, W.G.; McCollum, W.R.; Fomuso, E.E.K. Local governments: Outcomes of enterprise resource planning system on organizational productivity. Int. J. Appl. Manag. Technol. 2022, 21, 14–30. [Google Scholar] [CrossRef]
- Stelzl, K.; Röglinger, M.; Wyrtki, K. Building an ambidextrous organization: A maturity model for organizational ambidexterity. Bus. Res. 2020, 13, 1203–1230. [Google Scholar] [CrossRef]
- Modrák, V.; Šoltysová, Z. Development of an organizational maturity model in terms of mass customization. In Industry 4.0 for SMEs; Matt, D., Modrák, V., Zsifkovits, H., Eds.; Palgrave Macmillan: London, UK, 2020; pp. 137–154. [Google Scholar] [CrossRef]
- Blondiau, A.; Mettler, T.; Winter, R. Designing and implementing maturity models in hospitals: An experience report from 5 years of research. Health Inform. J. 2016, 22, 758–767. [Google Scholar] [CrossRef]
- Moreira, A.; Hak, F.; Santos, M.F. A maturity model for omnichannel adoption in health care institutions. Heliyon 2024, 10, e38526. [Google Scholar] [CrossRef] [PubMed]
- Hasselbring, W. Information system integration. Commun. ACM 2000, 43, 32–38. [Google Scholar] [CrossRef]
- Levina, A.; Ilin, I.; Gugutishvili, D.; Kochetkova, K.; Tick, A. Towards a smart hospital: Smart infrastructure integration. J. Open Innov. Technol. Mark. Complex. 2024, 10, 100339. [Google Scholar] [CrossRef]
- Paré, G.; Sicotte, C. Information technology sophistication in health care: An instrument validation study among Canadian hospitals. Int. J. Med. Inform. 2001, 63, 205–223. [Google Scholar] [CrossRef]
- Tahran, A.; Garousi, V.; Turetken, O.; Söylemez, M.; Garossi, S. Maturity assessment and maturity models in health care: A multivocal literature review. Digit. Health 2020, 6, 2055207620914772. [Google Scholar] [CrossRef]
- Torab-Miandoab, A.; Samad-Soltani, T.; Jodati, A.; Rezaei-Hachesu, P. Interoperability of heterogeneous health information systems: A systematic literature review. BMC Med. Inform. Decis. Mak. 2023, 23, 18. [Google Scholar] [CrossRef] [PubMed]
- Cimini, C.; Lagorio, A.; Cavalieri, S. Development and application of a maturity model for Industrial Agile Working. Comput. Ind. Eng. 2024, 188, 109877. [Google Scholar] [CrossRef]
- Paré, G.; Kitsiou, S. Methods for literature reviews. In Handbook of eHealth Evaluation: An Evidence-Based Approach (Chapter 9); Lau, F., Kuziemsky, C., Eds.; University of Victoria: Victoria, BC, Canada, 2017. Available online: https://www.ncbi.nlm.nih.gov/books/NBK481583/ (accessed on 22 July 2025).
- Tranfield, D.; Denyer, D.; Smart, P. Towards a methodology for developing evidence-informed management knowledge by means of systematic review. Br. J. Manag. 2003, 14, 207–222. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Straus, S.E.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- CMMI. CMMI® for Services, Version 1.3: Improving Processes for Providing Better Services; (Technical Report No. CMU/SEI-2010-TR-034, ESC-TR-2010-034); Software Engineering Institute, Carnegie Mellon University: Pittsburgh, PA, USA, 2010. [Google Scholar]
- Gemmel, P.; Vandaele, D.; Tambeur, W. Hospital process orientation (HPO): The development of a measurement tool. Total Qual. Manag. Bus. Excell. 2008, 19, 1207–1217. [Google Scholar] [CrossRef]
- Škrinjar, R.; Štemberger, M.; Hernaus, T. The impact of business process orientation on organizational performance. In Proceedings of the 2007 Informing Science and IT Education Joint Conference, Ljubljana, Slovenia, 22–25 June 2007; Available online: https://www.informingscience.org/Publications/3150 (accessed on 22 July 2025).
- Türetken, O.; Van Looy, A. Capability and maturity models in business process management. In Handbook on Business Process Management and Digital Transformation: Research Handbooks in Information Systems; Grefen, P., Vanderfeesten, I., Eds.; Edward Elgar Publishing: Cheltenham, UK, 2024; pp. 303–331. [Google Scholar] [CrossRef]
- Idogawa, J.; Bizarrias, F.S.; Camara, R. Critical success factors for change management in business process management. Bus. Process Manag. J. 2023, 29, 2009–2033. [Google Scholar] [CrossRef]
- Hein-Pensel, F.; Winkler, H.; Brückner, A.; Wölke, M.; Jabs, I.; Mayan, I.J.; Kirschenbaum, A.; Friedrich, J.; Zinke-Wehlmann, C. Maturity assessment for Industry 5.0: A review of existing maturity models. J. Manuf. Syst. 2023, 66, 200–210. [Google Scholar] [CrossRef]
- Gomes, J.V.; Romão, M.B.; Bento, I. Project Management Maturity: OPM3 Study. In Intersecting Environmental Social Governance and AI for Business Sustainability; Popescu, C., Yu, P., Eds.; IGI Global Scientific Publishing: New York, NY, USA, 2024; pp. 220–245. [Google Scholar] [CrossRef]
- PROV (Public Record Office Victoria). Information Management Maturity Measurement Tool (IM3). 11 July 2021. Available online: https://prov.vic.gov.au/recordkeeping-government/learning-resources-tools/information-management-maturity-measurement-tool-im3 (accessed on 22 July 2025).
- Fitterer, R.; Rohner, P. Towards assessing the networkability of health care providers: A maturity model approach. Inf. Syst. e-Bus. Manag. 2010, 8, 223–244. [Google Scholar] [CrossRef]
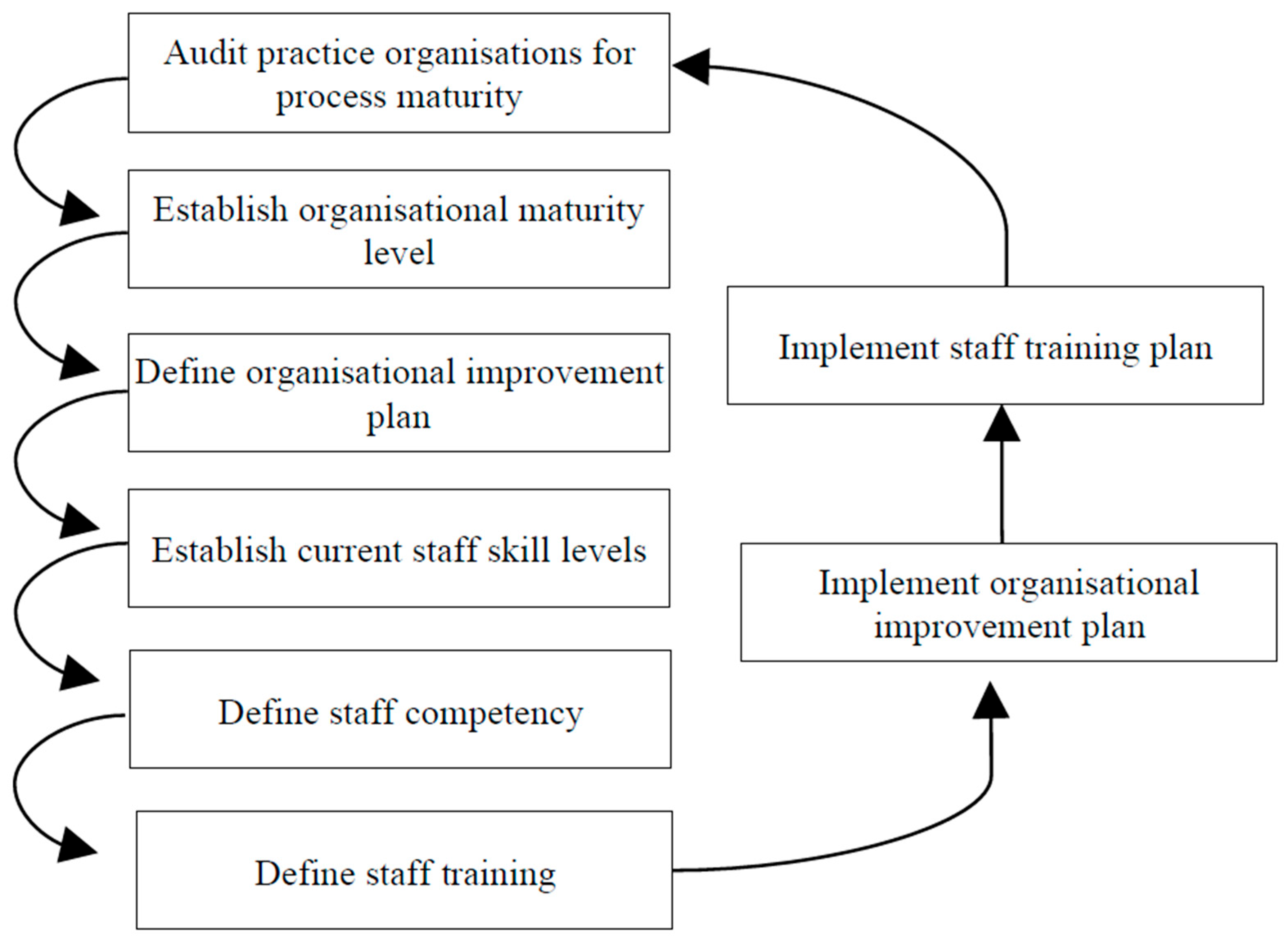
- Gillies, A.; Howard, J. Managing change in process and people: Combining a maturity model with a competency-based approach. Total Qual. Manag. Bus. Excell. 2003, 14, 779–787. [Google Scholar] [CrossRef]
- HIMSS. Community Care Outcomes Maturity Model (C-COMM); Healthcare Information and Management Systems Society: Chicago, IL, USA, 2023; Available online: https://www.himss.org/maturity-models/ccomm/ (accessed on 22 July 2025).
- Garets, D.; Davis, M. Electronic Medical Records Versus Electronic Health Records: Yes, There Is a Difference; HIMSS Analytics: Chicago, IL, USA, 2006; Available online: http://sirroteinfo.ezyro.com/wp-content/uploads/2020/06/WP_EMR_EHR.pdf?i=1 (accessed on 12 August 2022).
- Smith, L.S.; Bradley, R.V.; Bichescu, B.C.; Tremblay, M.C. IT governance characteristics, electronic medical records sophistication, and financial performance in U.S. hospitals: An empirical investigation. Decis. Sci. J. 2013, 44, 483–516. [Google Scholar] [CrossRef]
- Tekerek, B.; Işık, O. Exploring the digitalization of hospitals upon the EMRAM model: The case of Türkiye. İşletme Bilim. Derg. 2025, 13, 20–27. [Google Scholar] [CrossRef]
- Sharma, B. Electronic Healthcare Maturity Model (eHMM): A White Paper; Quintegra Solutions Limited: Teynampet, Chennai, 2008; Available online: https://www.quintegrasolutions.com (accessed on 22 July 2025).
- Guédria, W.; Bouzid, H.; Bosh, G.; Naudet, Y.; Chen, D. eHealth interoperability evaluation using a maturity model. Stud. Health Technol. Inform. 2012, 180, 333–337. [Google Scholar] [PubMed]
- IDC. IDC MaturityScape Benchmark: Big Data and Analytics 2021; IDC: Singapore, 2021; Available online: https://my.idc.com/getdoc.jsp?containerId=TEA003965&pageNumber=32&pageSize=10 (accessed on 22 July 2025).
- Anderson, C.; Kolding, M.; Sundblad, M. IDC MaturityScape: Technology Skill Development 2.0 (IDC #US47596821). IDC. April 2021. Available online: https://my.idc.com/getdoc.jsp?containerId=US47596821 (accessed on 22 July 2025).
- Bhavnani, S.P.; Narula, J.; Sengupta, P.P. Mobile technology and the digitization of healthcare. Eur. Heart J. 2016, 37, 1428–1438. [Google Scholar] [CrossRef] [PubMed]
- Slabodkin, G. IDC Issues Mobility Maturity Model for Healthcare Organizations. FierceMobileHealthcare. 5 August 2013. Available online: https://www.fiercehealthcare.com/mobile/idc-issues-mobility-maturity-model-for-healthcare-organizations (accessed on 22 July 2025).
- van Dyk, L.; Schutte, C. The Telemedicine Service Maturity Model: A framework for the measurement and improvement of telemedicine services. In Telemedicine; Madhavan, R., Khalid, S., Eds.; IntechOpen: London, UK, 2013. [Google Scholar] [CrossRef]
- Duffy, J. Healthcare Transformation: The Role of IT; Health Industry Insights: New York, NY, USA, 2006; Available online: https://docplayer.net/5588134-Jan-duffy-research-manager-health-industry-insights-emea.html (accessed on 12 August 2022).
- Liu, C.-F.; Hwang, H.-G.; Chang, H.-C. E-healthcare maturity in Taiwan. Telemed. E-Health 2011, 17, 569–573. [Google Scholar] [CrossRef]
- Kenneally, J.; Curley, M.; Wilson, B.; Porter, M. Using design science research: Presenting a unified application of the IT Capability Maturity Framework and the Electronic Medical Record Adoption Model. In Design Science: Perspectives from Europe. EDSS 2012; Helfert, M., Donnellan, B., Eds.; Communications in Computer and Information Science; Springer: Cham, Switzerland, 2013; Volume 388, pp. 124–143. [Google Scholar] [CrossRef]
- NHS Digital. National Infrastructure Maturity Model (NIMM) Handbook: A Guide for Assessing and Improving IT Infrastructure in NHS Organizations; NHS Digital: Leeds, UK; London, UK, 2019; Available online: https://digital.nhs.uk (accessed on 22 July 2025).
- Huang, H.K. PACS is only in the beginning of being used as a clinical research tool. In Proceedings of the 24th International EuroPACS Conference, Trondheim, Norway, 15–17 July 2006; pp. 1–10. [Google Scholar]
- van de Wetering, R.; Batenburg, R. A PACS maturity model: A systematic meta-analytic review on maturation and evolvability of PACS in the hospital enterprise. Int. J. Med. Inform. 2009, 78, 127–140. [Google Scholar] [CrossRef] [PubMed]
- van de Wetering, R.; Batenburg, R. Towards a theory of PACS deployment: An integrative PACS maturity framework. J. Digit. Imaging 2014, 27, 337–350. [Google Scholar] [CrossRef]
- Carvalho, J.V.; Rocha, Á.; Abreu, A. Maturity Models of Healthcare Information Systems and Technologies: A Literature Review. J. Med. Syst. 2016, 40, 131. [Google Scholar] [CrossRef]
- Page, B.J. Information Security Maturity Model for Healthcare Organizations in the United States. Ph.D. Thesis, Portland State University, Portland, OR, USA, 2021; p. 5758. [Google Scholar] [CrossRef]
- Le Clair, C. Electronic Medical Records Need More to Support “Meaningful Use”: ECM and BPM Anchor the Portfolio of Technologies That Will Improve Hospitals’ Processes [Do Trend Report]; Forrester Research: Cambridge, MA, USA, 2010; Available online: https://www.forrester.com/report/Electronic-Medical-Records-Need-More-To-Support-Meaningful-Use/RES55554 (accessed on 20 May 2010).
- Iron Mountain. Measuring Enterprise Information Governance Maturity with IGHealthRate™ [White paper]; Iron Mountain: Singapore. Available online: https://edge.sitecorecloud.io/ironmountain-c8dd68e9/media/project/iron-mountain/iron-mountain/files/resources/whitepapers/m/measuring-enterprise-information-governance-maturity-with-ighealthrate.pdf?sc_lang=en (accessed on 18 February 2025).
- Crowley, K.; Gold, R.S.; Bandi, S.; Agarwal, R. The Public Health Information Technology Maturity Index: An approach to evaluating the adoption and use of public health information technology. Front. Public Health Serv. Syst. Res. 2016, 5, 26–33. [Google Scholar] [CrossRef]
- Wijayarathne, H.; Rajapaksha, T.G.; Perera, M.; Pathirage, R. Modification and Validation of a Maturity Assessment Tool for Public Health Information System Implementations in Sri Lanka. In Studies in Health Technology and Informatics; Lovis, C., Séroussi, B., Hasman, A., Ferreira, L.R.L., Romano, M.F.F., Eds.; IOS Press: Amsterdam, The Netherlands, 2022; Volume 294, pp. 62–66. [Google Scholar] [CrossRef]
- Bernal, W.; Espitaleta, K. Framework for developing an information technology maturity model for smart city services in emerging economies (FSCE2). Appl. Sci. 2021, 11, 10712. [Google Scholar] [CrossRef]
- Akinsanya, O.; Papadaki, M.; Sun, L. Current cybersecurity maturity models: How effective in healthcare cloud? In Proceedings of the 1st International Workshop on Cybersecurity and Data Privacy (CERC 2019), CEUR Workshop Proceedings, New Delhi, India, 15 March 2019; Volume 2348, pp. 127–138. Available online: http://ceur-ws.org/Vol-2348/paper16.pdf (accessed on 22 July 2025).
- Le, N.; Hoang, D. Capability maturity model and metrics framework for cyber cloud security. Scalable Comput. Pract. Exp. 2017, 18, 277–290. [Google Scholar] [CrossRef]
- CSA. Healthcare Cloud Security Metrics and Assessment Framework (HCSMAF); Cloud Security Alliance: Berlin, Germany, 2020; Available online: https://cloudsecurityalliance.org (accessed on 22 July 2025).
- Google Cloud. Security Best Practices for Compute Engine. 2020. Available online: https://cloud.google.com/security (accessed on 22 July 2025).
- CSA (Cloud Security Alliance). Cloud Controls Matrix (CCM); CSA (Cloud Security Alliance): Berlin, Germany, 2020. [Google Scholar]
- Novais, T. Healthcare Cloud Security Maturity Assessment Framework. Master’s Thesis, Faculty of Sciences of the University of Porto, Porto, Portugal, 2021. Available online: https://repositorio-aberto.up.pt/bitstream/10216/139046/2/524041.pdf (accessed on 22 July 2025).
- MEASURE Evaluation. Health Information Systems Interoperability Maturity Toolkit: Assessment Tool (Version 0.5) [PDF]; University of North Carolina at Chapel Hill: Chapel Hill, NC, USA, 2017; Available online: https://www.measureevaluation.org/resources/publications/tl-17-03b.html (accessed on 22 July 2025).
- MEASURE Evaluation. Health Information Systems Interoperability Maturity Toolkit: User Guide, Maturity Model, and Assessment Tool (Version 1.0); University of North Carolina at Chapel Hill: Chapel Hill, NC, USA, 2019; Available online: https://www.measureevaluation.org/tools/health-information-systems-interoperability-toolkit.html (accessed on 22 July 2025).
- Liaw, S.; Zhou, R.; Ansari, S.; Gao, J. A digital health profile & maturity assessment toolkit: Cocreation and testing in the Pacific Islands. J. Am. Med. Inform. Assoc. 2021, 28, 494–503. [Google Scholar] [CrossRef]
- PAHO/WHO (Pan American Health Organization/World Health Organization). Information Systems for Health: Standard Assessment Method IS4H-MM 1.0; PAHO/WHO: Washington, DC, UAS, 2008; Available online: https://www3.paho.org/ish/docs/maturity.pdf (accessed on 10 July 2025).
- HIMSS. Infrastructure Adoption Model (INFRAM): Driving Healthcare Infrastructure Transformation; Healthcare Information and Management Systems Society: Chicago, IL, USA, 2018; Available online: https://www.himss.org/maturity-models/infram/ (accessed on 22 July 2025).
- van Dyk, L.; Schutte, C.; Fortuin, J. A maturity model for telemedicine implementation. In Proceedings of the Fourth International Conference on eHealth, Telemedicine, and Social Medicine (eTELEMED 2012), Valencia, Spain, 30 January–4 February 2012; International Academy, Research, and Industry Association (IARIA): Wilmington, DE, USA, 2012; pp. 98–105. [Google Scholar]
- HIMSS. Continuity of Care Maturity Model (CCMM): A Framework for Advancing Coordinated Care; Healthcare Information and Management Systems Society: Chicago, IL, USA, 2022; Available online: https://www.himss.org/maturity-models/ccmm/ (accessed on 22 July 2025).
- Kim, G.J.; Namkoong, K. Developing the Digital Health Communication Maturity Model: Systematic review. J. Med. Internet Res. 2025, 27, e68344. [Google Scholar] [CrossRef]
- NEHTA. Interoperability Maturity Model Version 2.0; National eHealth Transition Authority: Sydney, Australia, 2007. Available online: https://developer.digitalhealth.gov.au/resources/interoperability-framework-v2-0 (accessed on 22 July 2025).
- Knight, M.R.; Kolln, J.T.; Widergren, S.E.; Narang, D.; Khandekar, A.; Nordman, B. Interoperability Maturity Model: A Qualitative and Quantitative Approach for Measuring Interoperability; Grid Modernization Laboratory Consortium, U.S. Department of Energy: Denver, CO, USA, 2020. Available online: https://www.pnnl.gov/main/publications/external/technical_reports/PNNL-29683.pdf (accessed on 22 July 2025).
- HIN Advisory Group. Health Information Network (HIN) Maturity Model: A Discussion Paper; Canada Health Infoway: Montreal, QC, Canada, 2015; Available online: https://www.infoway-inforoute.ca/en/component/edocman/resources/reports/2834-health-information-network-hin-maturity-model?Itemid=103 (accessed on 22 July 2025).
- Staggers, N.; Rodney, M. Promoting usability in organizations with a new Health Usability Model: Implications for nursing informatics. In Proceedings of the 11th International Congress on Nursing Informatics, Montreal, QC, Canada, 23–27 June 2012. [Google Scholar]
- Nielsen, J. Corporate Usability Maturity Stages: 1–4 and 5–8; Nielsen Norman Group: Fremont, CA, USA, 2006; Available online: https://www.nngroup.com/articles/usability-maturity-stages-1-4/ (accessed on 22 July 2025).
- Schaffer, E. Institutionalization of Usability: A Step-by-Step Guide; Addison-Wesley: Boston, MA, USA, 2004. [Google Scholar]
- ISO/TC159/SC4/WG6; Usability Maturity Model: Human Centredness Scale. ISO (International Organization for Standardization): Geneva, Switzerland, 1998.
- Mettler, T.; Blondiau, A. HCMM—A maturity model for measuring and assessing the quality of cooperation between and within hospitals. In Proceedings of the 25th IEEE International Symposium on Computer-Based Medical Systems (CBMS), IEEE, Rome, Italy, 20–22 June 2012; pp. 1–6. [Google Scholar] [CrossRef]
- Boer, J.; van Houwelingen, J.; Adriani, P.; Geerts, A. Game Maturity Model for Healthcare: How Games Will Change Healthcare. Compact Magazine. 2013. Available online: https://www.compact.nl/articles/game-maturity-model-for-healthcare/ (accessed on 22 July 2025).
- Furukubo, M.; Ohuchi, A.; Morimoto, N. Maturity Model of Hospital (MMH) for Continuous Improvement. In Proceedings of the 2nd International Conference on Information Technology for Application (ICITA 2004), Harbin, China, 9–11 January 2004. [Google Scholar]
- Chassin, M.R.; Loeb, J.M. High-reliability health care: Getting there from here. Milbank Q. 2013, 91, 459–490. [Google Scholar] [CrossRef]
- Sullivan, J.; Rivard, P.; Shin, M.; Rosen, A. Applying the High Reliability Health Care Maturity Model to assess hospital performance: A VA case study. Jt. Comm. J. Qual. Patient Saf. 2016, 42, 389–AP12. [Google Scholar] [CrossRef]
- Digital Square. Digital Square Global Goods Guidebook, 3rd ed.; PATH: Seattle, WA, USA, 2022; Available online: https://static1.squarespace.com/static/59bc3457ccc5c5890fe7cacd/t/62a46059642f3b5127550bfe/1654939756182/Global+Goods+Guidebook+V3-Update-10-June-2022.pdf (accessed on 22 July 2025).
- Tom-Aba, D.; Silenou, B.; Doerrbecker, J.; Fourie, C.; Leitner, C.; Wahnschaffe, M.; Strysewske, M.; Arinze, C.; Krause, G. The Surveillance Outbreak Response Management and Analysis System (SORMAS): Digital Health Global Goods Maturity Assessment. JMIR Public Health Surveill. 2020, 6, e15860. [Google Scholar] [CrossRef] [PubMed]
- Daclin, N.; Dusserre, G.; Mailhac, L.; L’Héritier, B.; Blanchard, J.; Picard, A. Towards a maturity model to assess field hospitals’ rollout. Int. J. Emerg. Manag. 2018, 14, 139–158. [Google Scholar] [CrossRef]
- EC (European Commission). Interoperability Maturity Tools (IMTs) for Digital Public Services; Interoperable Europe: Brussels, Belgium, 2022; Available online: https://interoperable-europe.ec.europa.eu/collection/interoperability-maturity-tools-imts-digital-public-services (accessed on 22 July 2025).
- MEASURE Evaluation. Standards and Tools for Health Information Systems Strengthening (SOCI) Toolkit; MEASURE Evaluation, University of North Carolina at Chapel Hill: Chapel Hill, NC, USA, 2016; Available online: https://www.measureevaluation.org/resources/publications/ms-15-99.html (accessed on 22 July 2025).
- HIMSS. Electronic Medical Record Adoption Model (EMRAM); Healthcare Information and Management Systems Society (HIMSS): Chicago, IL, USA, 2023; Available online: https://www.himss.org/maturity-models/emram/ (accessed on 22 July 2025).
- EC (European Commission). Maturity Assessment Model for Integrated Care (IC-MM). Blueprint on Digital Transformation of Health and Care. 2019. Available online: https://digital-strategy.ec.europa.eu/en/library/blueprint-digital-transformation-health-and-care-ageing-society (accessed on 22 July 2025).
- Magdaleno, A.M.; Araujo, R.; Werner, C.M.L. A roadmap to the Collaboration Maturity Model (CollabMM) evolution. In Proceedings of the 2011 15th International Conference on Computer Supported Cooperative Work in Design (CSCWD), IEEE, Laussane, Switzerland, 8–10 June 2011; pp. 305–312. [Google Scholar] [CrossRef]
- Mettler, T. Maturity assessment models: A design science research approach. Int. J. Soc. Syst. Sci. 2011, 3, 81–98. [Google Scholar] [CrossRef]
- Sanders, D.; Burton, D.A.; Protti, D. The Healthcare Analytics Adoption Model: A Framework and Roadmap [White Paper]; Health Catalyst: South Jordan, UT, USA, 2013; Available online: https://www.healthcatalyst.com/learn/white-papers/the-healthcare-analytics-adoption-model-a-roadmap-to-analytic-maturity (accessed on 22 July 2025).
- Mettler, T.; Vimarlund, V. Understanding business intelligence in the context of healthcare. Health Inform. J. 2009, 15, 254–264. [Google Scholar] [CrossRef]
- Brooks, P.; El-Gayar, O.; Sarnikar, S. Towards a business intelligence maturity model for healthcare. In Proceedings of the 2013 46th Hawaii International Conference on System Sciences, Wailea, HI, USA, 7–10 January 2013; pp. 3807–3816. [Google Scholar] [CrossRef]
- Gastaldi, L.; Pietrosi, A.; Lessanibahri, S.; Paparella, M.; Scaccianoce, A.; Provenzale, G.; Corso, M.; Gridelli, B. Measuring the maturity of business intelligence in healthcare: Supporting the development of a roadmap toward precision medicine within ISMETT hospital. Technol. Forecast. Soc. Change 2018, 128, 84–103. [Google Scholar] [CrossRef]
- Pinto-Valverde, J.M.; Pérez-Guardado, M.Á.; Gomez-Martinez, L.; Corrales-Estrada, M.; Lavariega-Jarquín, J.C. HDQM2: Healthcare Data Quality Maturity Model. In Proceedings of the Transactions of the International Conference on Health Information Technology Advancement, Philadelphia, PA, USA, 9–11 September 2013; p. 37. Available online: https://scholarworks.wmich.edu/ichita_transactions/37 (accessed on 22 July 2025).
- Tcheng, J.E.; Fleurence, R.; Sedrakyan, A. Electronic health data quality maturity model for medical device evaluations. BMJ Surg. Interv. Health Technol. 2020, 2, e000043. [Google Scholar] [CrossRef] [PubMed]
- HIMSS. Promoting Usability in Health Organizations: Initial Steps and Progress Toward a Healthcare Usability Maturity Model; Health Information Management Systems Society: Chicago, IL, USA, 2011. [Google Scholar]
- Storm, I.; Harting, J.; Stronks, K.; Schuit, A. Measuring stages of Health in All Policies on a local level: The applicability of a maturity model. Health Policy 2014, 114, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Andersen, J.B.; Gulis, G. Community maturity to implement Health in All Policies. Int. J. Public Health 2017, 62, 605–612. [Google Scholar] [CrossRef]
- Global Digital Health Index. The State of Digital Health. 2019. Available online: https://static1.squarespace.com/static/5ace2d0c5cfd792078a05e5f/t/5d4dcb80a9b3640001183a34/1565379490219/State+of+Digital+Health+2019.pdf (accessed on 1 July 2025).
- WHO (World Health Organization). National eHealth Strategy Toolkit; WHO and ITU: Geneva, Switzerland, 2012; Available online: https://www.who.int/publications/i/item/national-ehealth-strategy-toolkit (accessed on 22 July 2025).
- HIMSS. HIMSS Dictionary of Healthcare Information Technology Terms, Acronyms and Organizations, 3rd ed.; Healthcare Information and Management Systems Society (HIMSS): Chicago, IL, USA, 2016. [Google Scholar]
| Search Criteria |
|---|
| Maturity Model AND Health |
| Maturity Model AND Healthcare |
| Maturity Model AND Hospital |
| Maturity Model AND eHealth |
| Maturity Model AND HIS |
| Maturity Model AND Health Information System |
| Components | Factors |
|---|---|
| Strategic alignment | Communication, partnership, strategy governance |
| IT management | IT governance, IT organization, IT performance, IT scope, IT strategy |
| Process management | BPM (business process management) alignment, BPM methods, BPM governance people |
| Organizational project management | OPM governance, OPM assessment, OPM communication, People cooperation |
| Cooperation management | Collaboration engineering, committee work, cooperation strategy, partner selection |
| Systems architecture | IT architecture, IT applications, IT integration |
| Functional | Technological | Diffusional | Organizational |
|---|---|---|---|
| F1—Goal definition | T1—BI architecture | D1—Accessing users | O1—BI strategy |
| F2—Measurement | T2—Reporting | D2—System users | O2—BI budget |
| F3—Gap analysis | T3—Interface | D3—Process coverage | O3—Organization coverage |
| F4—Data quality | T4—User profiling | O4—Key-user capabilities | |
| F5—Functional integration | T5—Technological integration | O5—User capabilities | |
| T6—Standards | O6—Competence improvement | ||
| T7—Data provisioning | O7—Partner/supplier coordination | ||
| Model Type | Primary Focus | Typical Dimensions | Example Models |
|---|---|---|---|
| Process-oriented | Workflows, culture, process quality | Process areas, structure, IT alignment | CMMI, BPOMM, PMMM |
| Technology-focused | Systems, infrastructure, security | IT systems, EMR adoption, cybersecurity | EMRAM, INFRAM, HCSMAF |
| Specialized domain | Specific health services | Domain-specific practices and processes | PACS MM, TMSMM, UMM |
| Data and Analytics | Data management and use | Data quality, analytics, governance | ICMM, HAAM, HDQM2 |
| Policy-oriented | Governance and public health policy | Strategy, legislation, national programs | MMHiAP, GDHI, IMAPS |
| Process-Oriented Models | ||||
|---|---|---|---|---|
| Model Name | Health Focus | Dimensions/Factors | Author | |
| 1 | Capability Maturity Model Integration for Services (CMMI) | Health care services | 24 process areas | [82] |
| 2 | Business Process Orientation Maturity Model (BPOMM) | Process orientation | Seven dimensions subdivided into two parts: the BPO-Components and the BPO-Impacts | [83] |
| 3 | Process management Maturity Model (PMMM) | Process management | Culture: strategy; structures; practices; IT | [71] |
| 4 | Information Management Maturity Assessment Program (IMMAP) | Information management | Measure performance against the whole of Victorian government IM standards. Assess an organization’s ability to meet information management best practice | [89] |
| 5 | Networkability maturity Model (NMM) | Networkability | Strategic alignment, IT management, process management, organizational project management, corporation management, system architecture | [90] |
| 6 | General Practice Information Maturity Model (GPIMM) | General practice information | Paper-based, computerized, computerized PHCT, coded, bespoke, paperless | [91] |
| Technology-Focused Models | ||||
| 7 | HIMSS Analytics Electronic Medical Record Adoption Model (EMRAM) | HIS application | Clinical quality; efficiency; patient safety; analytics; interoperability | [92] |
| 8 | Electronic Healthcare Maturity Model (eHMM) | Standardizing, integrating, and optimizing electronic processes | Timeliness of process; data access and accuracy of data; process effort; cost-effectiveness; quality of process results; utility or value to stakeholders. The eHMM proposes a 7-level Maturity Model | [96] |
| 9 | IDC Maturity Scapes (IDC-MS) | 3rd Platform technologies | Intent; data; technology; people; processes | [98] |
| 10 | IDC Mobility Maturity Model (IDC-Mobility) | Mobility | Strategic intent; technology; people; processes | [100] |
| 11 | IDC healthcare IT Maturity Model (IDC-HIT) | Integrated Health Information Systems | Improved clinical outcomes; patient safety; operational efficiency; continuity and coordination of care; access and equity; data-driven health governance | [103,104] |
| 12 | Healthcare Information Technology Maturity Model (HIT-MM) | Digitization and integration of systems | Clinical quality; patient safety; operational efficiency; data-driven governance; patient engagement; health equity and access | [105] |
| 13 | NHS Infrastructure Maturity Model (NIMM) | Evaluating and advancing NHS IT infrastructure | People and organization; technology; security and information governance; alignment and value | [106] |
| 14 | PACS Maturity Model (PMM) | PACS | Strategy and policy; organization and processes. Monitoring and control; IT; people and culture | [108] |
| 15 | Hospital Information System Maturity Model (HISMM) | Assess and guide the evolution of HIS | Data analysis; strategy; people, electronic medical record; information security; systems and IT infrastructure | [110] |
| 16 | Forrester “Meaningful Use” Model | EMR | Access; interoperability; content features; planning and strategy | [112] |
| 17 | IGHealthRate™ | Information governance | (1) IG structure; (2) strategic alignment; (3) enterprise information management; (4) privacy and security; (5) legal and regulatory;(6) data governance; (7) IT governance; (8) analytics; (9) IG performance; (10) awareness and adherence. | [113] |
| 18 | Public Health Information Technology (PHIT) | Information technology | Scale and scope of use PHIT, PHIT quality, PHIT human capital, policy and resources, PHIT community infrastructure | [114] |
| 19 | IT Maturity Model for Smart City Services in Emerging Economies (FSCE2) | Smart city services | A conceptual model of smart cities services, IT dimensions and indicators, IT maturity levels Integrated (level 1), analytically managed (level 2, optimized automated (level 3) | [116] |
| 20 | Cloud Security Capability Maturity Model (CSCMM) | Cloud security | Domain and maturity level 12 security domains and 4 levels of maturity | [118] |
| 21 | Healthcare Cloud Security Maturity Assessment Framework (HCSMAF) | Cloud security | Identity and access management, data privacy and management, risk management, asset management, cryptography and key management, infrastructure and network security, compliance and audit management, incident response management, business continuity management. Initial (level 1): managed (level 2), quantitatively managed (level 3): optimizing (level 4) | [119] |
| 22 | Health Information Systems Interoperability Maturity Toolkit (HISAMT) | Information systems interoperability | Nascent, emerging, established, institutionalized and optimized | [123] |
| 23 | Digital Health Profile and Maturity Assessment Toolkit (DHPMAT) | Support national health priorities | Level 1: basic, Level 2: controlled, Level 3: standardized, Level 4: optimized, Level 5: innovative | [54] |
| 24 | Information Systems for Health Standard Assessment Method (IS4HMM) | Information systems for health | Conceptual framework; tactical framework; strategic framework; concepts, process, services and products; trust-based model; learning framework | [126] |
| 25 | Infrastructure Adoption Model (INFRAM) | Align IT capability | Cybersecurity; IT management and performance; adoption; outcomes; sustainability. Each of these dimensions is assessed across a maturity scale (Levels 0–7) to determine how well the infrastructure contributes to overall healthcare goals | [127] |
| Specialized Domain Models | ||||
| 26 | The Telemedicine Service Maturity Model (TMSMM) | Telemedicine | Man; machine; material; method; money | [128] |
| 27 | Continuity of Care Maturity Model (CCMM) | EMR | HIS application | [129] |
| 28 | Interoperability Maturity Model (IMM) | Interoperability | Organization, information, technical | [131] |
| 29 | Health Information Network Maturity Model (HIN) | Health information exchange | Vision and engagement; governance, policy and legislation; skills and resources; financing; model practice; success metrics; clinical use cases; technology and apps; security and privacy | [133] |
| 30 | Healthcare Usability Maturity Model (UMM) | Usability | Focus on users; management; process and infrastructure; resources; education | [158] |
| 31 | Hospital Cooperation Maturity Model (HCMM) | Networking/cooperation | Strategic; organizational, information | [138] |
| 32 | Health Game Maturity Model (HGMM) | Gamification | Value; process; coverage; types | [139] |
| 33 | Maturity Model for Hospital (MMH) | Medical service improvement | Learning and growth; hospital’s process; patients; citizen | [140] |
| 34 | High Reliability Health Care Maturity Model (HRHCM) | High reliability health care | Leadership, safety culture; robust process improvement | [142] |
| 35 | GRID Interoperability Maturity Model (G-IMM) | Interoperability | Organizational, informational, and technical | [143] |
| 36 | Global Goods Maturity Model (GGMM) | Open-source mobile and web application software | Global utility, community support, and software maturity global indicators | [143] |
| 37 | The Field Hospital Maturity Model (FHMM) | Field hospitals | Governance, logistics, and care Unconsidered, initial, practiced, managed, and improved | [145] |
| 38 | Interoperability Maturity Assessment of a Public Service (IMAPS) | Interoperability | Service delivery, service consumption, service management. Ad hoc (level 1): opportunistic (level 2): essential (level 3): sustainable (level 4): seamless (level 5) | [146] |
| 39 | Health Information System Stages of Continuous Improvement Toolkit (SOCI) | System stages of continuous improvement | Emerging/ad hoc, repeatable, defined, managed, and optimized | [147] |
| 40 | Community Care Outcomes Maturity Model (C-COMM) | Integration | Digital care coordination; access and equity; patient and caregiver engagement; outcomes and performance measurement; community partnerships and ecosystem integration; digital maturity and infrastructure readiness | [148] |
| 41 | Integrated Care Maturity Model (IC-MM) | Infrastructure IT | Managing IS; using BI; using IT; (4) aligning business and informatics; managing change. Five levels of maturity: basic, controlled, standardized, optimized, and innovative | [149] |
| 42 | Collaboration Maturity Model (CollabMM) | Coordination | Process integration; governance and roles; supporting tools; measurement and improvement. Similar to other Maturity Models, uses five progressive levels | [150] |
| Data and Analytics Models | ||||
| 43 | Informatics Capability Maturity Model (ICMM) | eHealth | The dimensions considered are as follows: ICM1. Collection, integration, and management of data in HIS/HER; ICM2. Sharing information in the health district; ICM3. Manage the implementation and change of information and communication technology in health; ICM4. Data quality management and information governance; ICM5. Using healthcare business intelligence to improve population care and health | [136,151] |
| 44 | The Healthcare Analytics Adoption Model (HAAM) | Data warehouse and analysis | New data sources; complexity; data literacy; data timeliness | [152] |
| 45 | Business Intelligence Maturity Model (BIMM) | Business intelligence | Collaboration; knowledge; trust; institutions; governance | [153] |
| 46 | Healthcare Data Quality Maturity Model (HDQM2) | Data quality | Accuracy/correctness; completeness; uniqueness; duplicates | [156] |
| 47 | Data Quality Maturity Model (DDMM) | Data quality | Conceptual, reactive, structured, complete, and advanced | [157] |
| 48 | Adoption Model for Analytics Maturity (AMAM) | Predictive analytics and governance | The AMAM is an international eight-stage (0–7) model measuring the capabilities that organizations have gained from technology and surrounding processes | [163] |
| Policy-Oriented Models | ||||
| 49 | The Maturity Model for Health in All Policies (MMHiAP) | Health in all policies at local government | Unrecognized, recognized, considered, implemented, integrated, institutionalized | [159,160] |
| 50 | Global Digital Health Index (GDHI) | Global maturity assessment in digital health and benchmark against other countries | Leadership and governance; strategy and investment; legislation, policy, and compliance; workforce; standards and interoperability; infrastructure; services and applications | [161] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gomes, J.; Romão, M. Evaluating Maturity Models in Healthcare Information Systems: A Comprehensive Review. Healthcare 2025, 13, 1847. https://doi.org/10.3390/healthcare13151847
Gomes J, Romão M. Evaluating Maturity Models in Healthcare Information Systems: A Comprehensive Review. Healthcare. 2025; 13(15):1847. https://doi.org/10.3390/healthcare13151847
Chicago/Turabian StyleGomes, Jorge, and Mário Romão. 2025. "Evaluating Maturity Models in Healthcare Information Systems: A Comprehensive Review" Healthcare 13, no. 15: 1847. https://doi.org/10.3390/healthcare13151847
APA StyleGomes, J., & Romão, M. (2025). Evaluating Maturity Models in Healthcare Information Systems: A Comprehensive Review. Healthcare, 13(15), 1847. https://doi.org/10.3390/healthcare13151847







